Abstract
[Purpose] The minimal clinically important difference (MCID) in grip strength is critical to interpreting changes in hand strength over time. This review was undertaken to summarize extant descriptions of the MCID for grip strength. [Methods] A search of 3 bibliographic databases as well as a hand search were completed to identify articles reporting the MCID for grip forces obtained by dynamometry. [Results] Of 38 unique articles identified as potentially relevant, 4 met the inclusion and exclusion criteria of this review. The MCIDs ranged from 0.04 kg to 6.5 kg. However, only a single study used receiver operating characteristic curve analysis and had an associated area under the curve exceeding 0.70. That study reported an MCID of 6.5 kg, which was similar to the MCIDs of another included study and minimal detectable changes reported elsewhere. [Conclusion] Additional, more rigorous, studies are needed to identify MCIDs for grip strength. In the meantime changes of 5.0 to 6.5 kg may be reasonable estimates of meaningful changes in grip strength.
Key words: Hand, Muscle strength, Dynamometry
INTRODUCTION
Measurements of grip strength are widely used as an indicator of overall muscle strength and of present and future health status- particularly among older individuals1). The reliability of grip strength measurements is well established2). That noted, the interpretability of the measurements depends on the availability of normative reference values and indicators of real change. Papers providing normative reference values for grip strength are abundant3, 4), but little information has been published that identifies standards for real changes in grip strength over time. Real changes are typically indicated by the distribution-based minimal detectable change (MDC) or the anchor-based minimal clinically important difference (MCID). The latter, which represents a change perceived to be beneficial and sufficiently large to warrant an alteration in a patient’s management5), has been described as preferable to the MDC as an indicator of responsiveness6). The purpose of this systematic review, therefore, was to determine and summarize what is known about the MCID of grip strength measurements obtained from adults.
METHODS
A search of the PubMed (since 1950), Scopus (since 1950), and CINAHL (since 1986) databases was conducted on April 14, 2018 and again on August 24, 2018. The search string used was: grip strength AND (“minimal clinically important difference” OR “minimum clinically important difference” OR “MCID” OR “minimal important difference” OR “minimal important change”). A hand search was also conducted.
To be considered for inclusion a study had to report an MCID for grip strength or provide information from which an MCID could be determined. Studies were excluded if they were not in English, reported an MCID between groups rather than over time, or if a clear anchor was not indicated. Articles were also excluded if they quantified grip strength using pneumatic devices that measure pressure7) or focused on children. The authors of articles deemed relevant but lacking requisite data were contacted for specifics.
Included articles were examined for information on the sample tested, measurement procedures (eg dynamometer used, measurement times, and anchor criteria) and findings. Findings related to differences in grip strength over time and descriptions of MCIDs. A 20 point quality checklist adapted from another article focused on MCIDs for gait speed was used for this review8).
RESULTS
Figure 1 is a PRISMA diagram showing how the final set of relevant studies was derived. The 3 databases yielded 36 unique, possibly relevant articles. Two additional articles were uncovered by hand searches. Of these 38 articles, 27 were judged to be inappropriate following review of their titles and abstracts. Of the 11 remaining articles, 4 provided acceptable information relevant to the MCID of grip strength9,10,11,12).
Fig. 1.
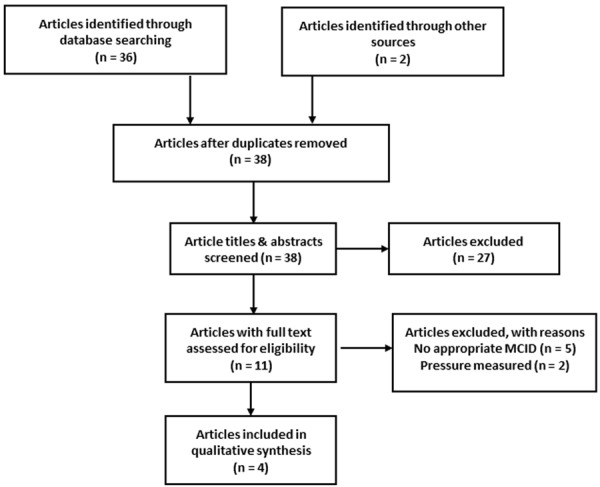
Flowchart illustrating search results and article selection for systematic review.
The specifics of the included studies are summarized in Table 1. Three involved samples of participants from different countries10,11,12) with the other involving a multinational sample9). Each sample incorporated adults with a different pathology or disorder, but 3 could be considered neuromuscular9, 10, 12). All included studies used a Jamar dynamometer with the hiatus between test and retest measures ranging from a mean 16 days (stroke)12) to 9 years (myotonic dystrophy)10). Each article reported using a different anchor. Two focused on participants’ judgments of strength or weakness10, 11) whereas 1 focused on health9) and another focused on global rating of change11). The difference of interest in 2 articles was a decrease in strength10, 11) whereas the difference of interest in 2 studies was an increase in strength9, 12). The MCIDs ranged from 0.04 kg to 6.9 kg. As a percentage the MCIDs ranged from 0.8% to 19.5%.
Table 1. Summary of studies included in systematic review.
| Study | Sample | Procedure | Findings |
|---|---|---|---|
| Draak et al. | International adults (n=163) with immune mediated neuropathies undergoing intra-venous immunoglobulin & other medical interventions | Dynamometer: Jamar in second handle position. Grip measurement times: baseline & retests 1, 3, 6, 12 mo post-baseline Anchor: General rating of health “compared to one year ago” (5 category from SF-36). Criterion: “somewhat better” |
Mean difference (increase) at 6 mo: about 67% MCID: 2.7 kg |
| Kierkegaard et al. | Canadian adults (n=108) with myotonic dystrophy | Dynamometer: Jamar Grip measurement times: baseline and retest (9 yrs). Anchor: Patient rating of hand weakness (5 category). Criterion: “worse” |
Median difference (decrease) at 9 yrs: 1 kg, 13.3%. MCID: 0.04 kg (AUC 0.51), 0.8% (AUC 0.58) |
| Kim et al. | Korean adults (n=50) undergoing surgical repair of distal radius fracture | Dynamometer: Jamar Grip measurement time: 1 yr post surgery Anchor: Rating of strength compared to before injury (4 category) Criterion = “weakened” |
Mean difference (decresase) injured vs. calculated
preinjury: 5.0 kg, 17.9%. MCID: 6.5 kg (AUC 0.76), 19.5% (AUC 0.77) |
| Lang et al. | American adults with recent stroke (n=52) | Dynamometer: Jamar in 3rd handle position. Grip measurement times: baseline (9.5 d) and retest (25.9 d) post-stroke Anchor: Global rating of change (7 category). Criterion = “a little better, meaningful.” |
Mean difference (increase) over time (affected side):
6.9 kg, 71.9%. MCID: 5.0 kg (dominant side affected), 6.2 kg (nondominant side affected) |
The quality scores of the articles included in this systematic review ranged from 14 to 16 out of a maximum possible 20 points. Most lacking were descriptions of interventions between tests, the determination of cutpoints by procedures other than receiver operating characteristic curve (ROC) analysis, and the reliance upon a single anchor (Table 2).
Table 2. Quality checklist scores for four studies.
| Criteria | Draak et al. | Kierkegaard et al. | Kim et al. | Lang et al. |
|---|---|---|---|---|
| 1. Participant inclusion/exclusion criteria explicit | 1 | 2 | 2 | 2 |
| 2. Participants enrolled consecutively or systematically | 2 | 2 | 2 | 2 |
| 3. Attrition addressed | 2 | 1 | 2 | 2 |
| 4. Grip strength measure described | 4 | 3 | 4 | 5 |
| 5. Measurement bias | 1 | 2 | 1 | 2 |
| 6. Measurement hiatus | 2 | 2 | 2 | 2 |
| 7. Intervention or inter-test activity described | 2 | 0 | 0 | 0 |
| 8. ROC with AUC for cut-point | 0 | 1 | 2 | 0 |
| 9. MCID anchors | 1 | 1 | 1 | 1 |
| Total | 15 | 14 | 16 | 16 |
1. Both (2), one (1), neither (0); 2. Yes (2), unclear (1), no (0); 3. No attrition or yes & <25%, reasons given (2), yes but >25%, reasons given (1), no or>25%, no reasons given; 4. Instrument, adjustment, position, trials, criterion measurement described (5); 4/5 (4), 3/5 (3), 2/5 (2), 1/5 (1), 0/5 (0); 5. Blind, duplicate, or independent observer (2), unclear (1), investigator or treating clinician (0); 6. Specifically (2), vaguely (1), no (0); 7. Specifically (2), vaguely (1), no (0); 8. Cut point from ROC noted & AUC≥0.70 reported (2), cut point from ROC noted but AUC<0.70 (1), cut point not determined by ROC (0); 9. More than one anchor (2), one anchor (1), anchor not designated (0).
DISCUSSION
Given the widespread use of hand dynamometry to quantify grip strength, it is surprising that only 4 studies reporting MCIDs for grip strength were found that met this review’s inclusion and exclusion criteria. Only 2 of the 4 used ROC analysis as recommended by Terwee et al. to identify MCID cutpoints and only 1 of the 2 that did so met the 0.70 area under the curve criterion recommended by Terwee et al13). As a consequence, a specific MCID value for grip strength cannot be recommended. However, Kim et al.’s report of a MCID of 6.5 kg based on ROC analysis and an area under the curve greater than 0.70 can be highlighted11). Their MCID is close to those of 5.0 and 6.2 kg reported by Lang et al.12) and in line with the 6.0 kg Nitschke et al. described as “necessary to detect a genuine change in grip strength”14). Kim et al.’s MCID is also similar to the minimal detectable changes (95%) of 5.1 kg and 5.2 kg described for the left and right hands by Puthoff and Saskowski15).
Based the limited availability of rigorously determined MCIDs and their value in interpreting changes in grip strength over time, further research needs to be undertaken to identify MCIDs for grip strength. The research should focus on individuals with pathologies or conditions whose grip strength can be expected to either increase substantially over a short time (eg, soon after stroke or following discharge from intensive care) or decrease substantially over a short time (eg, amyotrophic lateral sclerosis or after the initiation of chemo therapy). The research should use ROC analysis to select a MCID that maximizes sensitivity and specificity. Anchors used to determine MCIDs should be specific to grip strength or activities limited by impairments in grip strength rather than general ratings of health. Among specific anchors could be self-ratings of grip strength such as described in the Stroke Impact Scale16) or self-rating of difficulty with specific activities personally identified by patients as problematic17). Anchors should be based on repeated testing rather than recall of previous status10). Finally, we suggest the use of more than 1 anchor as doing so can help to validate MCIDs.
This review has 2 notable limitations. The first is its limitation to only 4 studies. This was determined by the paucity of relevant studies. I used 3 databases and sought to expand inclusion by seeking further information from authors. The second limitation is reliance upon a single individual to select, abstract, and quality score the articles. The use of 2 independent reviewers is typically recommended.
In conclusion, the literature does not identify a clear MCID for grip strength. Until some consensus is reached, however, changes of 5.0 to 6.5 kg may provide a rough estimate of meaningful changes in grip strength.
Conflict of Interest
None.
REFERENCES
- 1.Bohannon RW: Muscle strength: clinical and prognostic value of hand-grip dynamometry. Curr Opin Clin Nutr Metab Care, 2015, 18: 465–470. [DOI] [PubMed] [Google Scholar]
- 2.Bohannon RW: Test-retest reliability of measurements of hand-grip strength obtained by dynamometry from older adults: a systematic review of research in the PubMed database. J Frailty Aging, 2017, 6: 83–87. [DOI] [PubMed] [Google Scholar]
- 3.Bohannon RW, Peollson A, Massy-Westropp N, et al. : Reference values for adult grip strength measured with a Jamar dynamometer: a descriptive meta-analysis. Physiotherapy, 2006, 92: 11–15. [Google Scholar]
- 4.Dodds RM, Syddall HE, Cooper R, et al. : Global variation in grip strength: a systematic review and meta-analysis of normative data. Age Ageing, 2016, 45: 209–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jaeschke R, Singer J, Guyatt GH: Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials, 1989, 10: 407–415. [DOI] [PubMed] [Google Scholar]
- 6.Turner D, Schünemann HJ, Griffith LE, et al. : The minimal detectable change cannot reliably replace the minimal important difference. J Clin Epidemiol, 2010, 63: 28–36. [DOI] [PubMed] [Google Scholar]
- 7.Roberts HC, Denison HJ, Martin HJ, et al. : A review of the measurement of grip strength in clinical and epidemiological studies: towards a standardised approach. Age Ageing, 2011, 40: 423–429. [DOI] [PubMed] [Google Scholar]
- 8.Bohannon RW, Glenney SS: Minimal clinically important difference for change in comfortable gait speed of adults with pathology: a systematic review. J Eval Clin Pract, 2014, 20: 295–300. [DOI] [PubMed] [Google Scholar]
- 9.Draak TH, Pruppers MH, van Nes SI, et al. PeriNomS study group: Grip strength comparison in immune-mediated neuropathies: Vigorimeter vs. Jamar. J Peripher Nerv Syst, 2015, 20: 269–276. [DOI] [PubMed] [Google Scholar]
- 10.Kierkegaard M, Petitclerc É, Hébert LJ, et al. : Responsiveness of performance-based outcome measures for mobility, balance, muscle strength and manual dexterity in adults with myotonic dystrophy type 1. J Rehabil Med, 2018, 50: 269–277. [DOI] [PubMed] [Google Scholar]
- 11.Kim JK, Park MG, Shin SJ: What is the minimum clinically important difference in grip strength? Clin Orthop Relat Res, 2014, 472: 2536–2541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lang CE, Edwards DF, Birkenmeier RL, et al. : Estimating minimal clinically important differences of upper-extremity measures early after stroke. Arch Phys Med Rehabil, 2008, 89: 1693–1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Terwee CB, Bot SD, de Boer MR, et al. : Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol, 2007, 60: 34–42. [DOI] [PubMed] [Google Scholar]
- 14.Nitschke JE, McMeeken JM, Burry HC, et al. : When is a change a genuine change? A clinically meaningful interpretation of grip strength measurements in healthy and disabled women. J Hand Ther, 1999, 12: 25–30. [PubMed] [Google Scholar]
- 15.Puthoff ML, Saskowski D: Reliability and responsiveness of gait speed, five times sit to stand, and hand grip strength for patients in cardiac rehabilitation. Cardiopulm Phys Ther J, 2013, 24: 31–37. [PMC free article] [PubMed] [Google Scholar]
- 16.Duncan PW, Wallace D, Lai SM, et al. : The stroke impact scale version 2.0. Evaluation of reliability, validity, and sensitivity to change. Stroke, 1999, 30: 2131–2140. [DOI] [PubMed] [Google Scholar]
- 17.Stratford P, Gill C, Westway M, et al. : Assessing disability and change on individual patient: a report of a patient specific measure. Physiother Can, 1995, 47: 258–263. [Google Scholar]


