Abstract
Erectile dysfunction (ED) is important to a man’s well-being and health, since it not only affects the individual but also causes strain on a couple’s lifestyle and relationship. There are multiple non-invasive treatments that exist for ED including lifestyle changes, oral medications (phosphodiesterase type 5 inhibitors), vacuum-assisted erectile devices, and intraurethral suppositories. While lifestyle changes and oral medications are typically first-line treatments for ED, more-invasive treatments including intracavernosal injections and surgically implanted prosthetic devices may be required for the management of complex cases. Additionally, novel therapies are currently being developed, and future treatment options may include shock-wave therapy, external prosthetic devices, and injection of stem cells or platelet-rich plasma. The current manuscript seeks to highlight advances in management and may eventually alter the treatment paradigm to allow more-inclusive care pathways.
Keywords: medical therapy, penile injections, belted prosthesis, external penile prosthesis
Introduction
Erectile dysfunction (ED), one of the most frequently reported medical conditions in men, is defined as the chronic inability to achieve or sustain a penile erection. Indeed, regular and chronic ED increases with age from ~35% of men aged 60 to ~50% of men older than 70 being affected 1. Primary care physicians identify and diagnose the majority of ED in the United States and Canada and, as such, are on the ground floor of helping patients navigate the multitude of treatment options that exist 2.
Many risk factors for ED exist including age, coronary artery disease, obesity, smoking, depression, hypertension, prior pelvic surgery, and spinal cord injuries as well as other psychological variables 3. Sexual health and erectile quality are key components to not only an individual’s quality of life but also their partner’s mental, emotional, and physical well-being 4. Along those lines, many seek support as they navigate their way through the multiple treatment options. As erectile function is a complex interplay between psychological and physiological factors, the American Urological Association (AUA) guidelines suggest referral to a mental health professional as adjunctive therapy for the treatment of ED 5. This has been shown to improve adherence to treatment plans and improve erectile function when used as a primary therapy and may enhance the effects of additional treatment options 6. A partner’s willingness to try different options has been shown to increase the likelihood of recovery of sexual function 7. These treatments vary from non-invasive to invasive. While non-invasive treatment options may be preferred for many patients, all management options should be thoroughly discussed. The AUA guidelines acknowledge that any treatment option may be used as a first-line therapy 5. Treatment options include lifestyle changes, oral medications, penile injections, and surgically implantable penile prostheses as well as more novel approaches such as belted external penile prostheses. Additional novel approaches to the management of ED are still considered experimental and include penile shockwave therapy and the injection of stem cells or platelet-rich plasma (PRP). These therapies have shown promising initial results and may become part of the ED treatment algorithm in the future. The current manuscript details these treatments with the goal being to help patients understand their options and thus improve their overall sexual recovery and experiences.
Treatment options
Lifestyle changes
Improvements in lifestyle and the proper management of medical comorbidities are arguably the most beneficial and safest treatment. This first-line approach is, without a doubt, the most difficult to execute. Patient education detailing the risk factors for ED is a logical first step. While the risks for developing future ED are sometimes out of an individual’s control, understanding them can help to change current behaviors. Lack of physical activity, obesity, unhealthy diets, and cigarette smoking have all been shown to contribute to ED 8. Other contributing factors include diabetes, cardiovascular disease, hypertension, hyperlipidemia, metabolic syndrome, and hypogonadism as well as psychiatric and psychological disorders 8. Lifestyle changes can thus prevent progression or improve regression in early manifestations of ED 8.
Data have found that physical activity is associated with a lower risk of ED while simultaneously both preventing and improving ED 9. In a large study of 31,724 men who were free of ED at baseline, a 40% increased risk of ED was noted with the development of obesity 10. Weight loss was also beneficial on quality of sexual life 11 while a healthy diet and reduced caloric intake have been associated with improvements in erectile function 8. Smoking has a negative relationship with erectile function, with cumulative smoking history being correlated to significantly increased ED risk 12.
Aside from altering risk factors, some lifestyle adaptations may also play a role in erectile function management. For example, some couples may serve to eroticize some treatments to make them more successful. Kukula et al. 7 strategized that by taking an erectile aid and incorporating it into the sexual experience in a positive way, the aid itself could become viewed as erotic and stimulating.
Oral medications
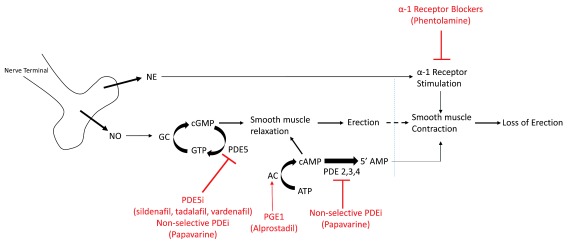
An erection starts with nerve stimulation, which releases nitric oxide (NO). NO stimulates guanylate cyclase (GC), which converts guanosine triphosphate (GTP) into cyclic guanosine monophosphate (cGMP). cGMP subsequently induces smooth muscle relaxation, which allows for influx of blood into the penis with resultant erection. The molecule phosphodiesterase type 5 (PDE5) breaks down cGMP and allows the penis to return to the flaccid state. This is the site of action of the most common oral medications used to treat ED ( Figure 1).
Figure 1. Molecular pathway of erections (black) and location of action of medications for erectile dysfunction (red).
AC, adenylyl cyclase; ATP, adenosine triphosphate; cAMP, cyclic adenosine monophosphate; cGMP, cyclic guanosine monophosphate; GC, guanylate cyclase; GTP, guanosine triphosphate; NE, norepinephrine; NO, nitric oxide; PDE5, phosphodiesterase type 5; PDE5i, phosphodiesterase type 5 inhibitor; PDE, phosphodiesterase; PDEi, phosphodiesterase inhibitor; PGE1, prostaglandin E1.
Taken by mouth prior to intercourse, oral medications are the first line of treatment for ED refractory to lifestyle modifications. These medications inhibit PDE5, which keeps the level of cGMP high and promotes erections. The most well-known of these PDE5 inhibitors is sildenafil (Viagra®, Pfizer Inc., FDA approved 1998). Additional PDE5 inhibitors include tadalafil (Cialis®, Lilly, FDA approved 2003), vardenafil (Levitra®, Bayer Healthcare, FDA approved 2003), and avanafil (Stendra®, Metuchen Pharmaceutical, FDA approved 2012).
Sildenafil and vardenafil are similar in action, with a peak absorption of 30–60 minutes and a half-life of 3–5 hours. These medications should be taken on an empty stomach to maximize absorption 13, 14. Avanafil is absorbed in 20–30 minutes with a half-life of 6 hours 15. Tadalafil is different from the other medications in that it takes longer to absorb (2–4 hours) and has a longer half-life (17.5 hours), so it lasts longer in the body. Additionally, it is not affected by food, so it does not have to be taken on an empty stomach. Currently, tadalafil is the only oral ED medication approved for daily use, rather than on an as-needed basis 16. Additionally, it has been shown to improve lower urinary tract symptoms in patients with benign prostatic hyperplasia 17.
For these medications to work, the nervous system pathways must be intact and a patient must have some sexual stimulation in order to increase the NO and cGMP in the penile tissues. Therefore, in patients who have severe diabetes with peripheral neuropathy or have undergone radical prostatectomy for prostate cancer, in whom the nerves for erections may be damaged, these medications may not be as effective 18, 19. Additionally, oral medications cannot be taken by patients who are taking nitrates for the treatment of chest pain, and care should be taken when combining PDE5 inhibitors with alpha-receptor-blocking medications, which may be prescribed for hypertension and lower urinary tract symptoms 20.
Even if a patient has tried oral medications in the past with poor response, he may have a good response with an alternative oral medication 21. A recent review of the literature and meta-analysis showed that sildenafil and tadalafil had similar efficacy and side effect profiles, but tadalafil had improved psychological outcomes including satisfaction with ED treatment 22, suggesting that this should be considered when deciding which oral medication to prescribe. Some evidence suggests that combining daily tadalafil with on-demand sildenafil may result in improved erectile function, particularly in men with severe ED 23. Additionally, for men who have difficulty timing an on-demand PDE5 inhibitor with sexual intercourse or for men experiencing bothersome side effects on higher-dose on-demand medications, the once-daily formulation of tadalafil may allow for better medication compliance, fewer side effects, and therefore better outcomes on the medication 24. There has been some recent controversy as to whether these medications can cause melanoma skin cancer or prostate cancer, but there is currently no evidence to support this, and PDE5 inhibitors remain common and recommended first-line treatments for ED 25.
Some patients may find PDE5 inhibitors cost-prohibitive for use in treating their ED. Urology offices often work with compounding pharmacies that may be able to provide these medications at a fraction of the cost. Additionally, several of the name-brand PDE5 inhibitors have recently come off, or soon will be coming off, patent, which will allow the generic versions of these medications to be more affordable. Generic sildenafil became available in 2016, and a generic version of tadalafil was FDA approved in May 2018.
Intracavernosal injections
Intracavernosal injections (ICIs) are an alternative to oral medications in the treatment of ED. With this treatment, medication is injected directly into the penile corpora at the lateral base of the penis, with care taken to avoid the neurovascular bundles dorsally and the urethra ventrally. The most commonly injected medication is prostaglandin E1 (PGE1), which stimulates cyclic adenosine monophosphate (cAMP) to induce smooth muscle relaxation and promote erections ( Figure 1). PGE1, also known as alprostadil (Edex®, Caverject®) is FDA approved for monotherapy injection. This medication is also commonly combined with one or two other medications, papaverine and phentolamine, as “bimix” or “trimix” in variable formulations for injection to treat ED ( Figure 1).
While slightly more invasive, ICI may be preferred to oral medications for the treatment of ED in certain patients in whom oral medications may be contraindicated (for example, patients who have had a recent heart attack) or who have not been able to tolerate oral medications in the past because of side effects. Additionally, since these medications act directly on the molecules that induce erections, they may work better in patients who have damage to the nerves that stimulate erections (see section on oral medications, and Figure 1) 26. The main barrier to the use of this therapy is patient anxiety centered around penile injections 27. Conflicting evidence exists as to whether patients have higher satisfaction with the use of ICI or oral PDE5i, but it is known that patients who use ICI consistently have high satisfaction rates 26.
According to the AUA guidelines, an in-office injection test dose should be administered to all men considering ICI for the management of ED to optimize the dose and to ensure the patient does not develop priapism or systemic side effects 26. The use of this medication is contraindicated in patients with a history of recurrent priapism, Peyronie’s disease, and bleeding disorders 26.
Intraurethral suppositories
Similar to alprostadil ICI, alprostadil is also available as an intraurethral suppository. This route of administration may be preferred by some patients who wish to avoid oral or injectable medications. While intraurethral alprostadil improves erectile function over placebo, it is less effective than ICI 26.
It is recommended that a test dose of intraurethral alprostadil be administered in clinic, similar to ICI 26. The most common side effect is penile or urethral pain 28. This medication should be used with caution in patients with increased risk for priapism or in patients with urethral disease. A condom should be used during sexual activity with a pregnant female partner to minimize her potential risk of exposure to prostaglandin.
Vacuum-assisted erectile devices
The vacuum-assisted erectile device (VED) is a device that is placed over the penis and pumped to create a vacuum, which pulls blood into the penis to cause engorgement and erection. A band is then placed around the base of the penis to maintain the erection and is removed to allow the penis to return to the flaccid state. The device may be challenging to use for patients with decreased dexterity or a large amount of lower abdominal fat and buried penis. VEDs may be effective in generating an erection in 90% of patients, though long-term use decreases, as many patients feel the devices are inconvenient to use and may have pain and temporary changes to penile sensation with the use of the constricting ring 24. Caution should be used in patients on blood thinners, given the theoretical increased risk of penile bruising with the device.
Though penile rehabilitation following radical prostatectomy for prostate cancer remains controversial, a VED may be prescribed as part of a rehabilitation program to minimize the risk of corporal fibrosis and has been shown to assist with erectile function during treatments 29.
Penile prostheses
The penile prosthesis is a surgically implanted device that has been used as a treatment for ED since the 1970s 30. The device and the technical aspects of surgical implantation have undergone multiple revisions over the years to optimize device function, minimize device failure, and maximize patient and partner satisfaction. Currently, patients who have undergone placement of a penile prosthesis report the highest satisfaction rate compared to patients who have received oral medications or ICI 31, 32.
The penile prosthesis comes in a variety of forms, including a malleable or inflatable device. The inflatable devices may be two- or three-piece devices. The malleable device consists of two rigid cylinders that are implanted within the penile corpora. This device remains rigid and may be simply positioned to allow for intercourse. This device is good for patients with limited dexterity. The inflatable devices consist of two fluid-filled cylinders that are implanted within the penis, along with a pump that is placed within the scrotum, and typically a fluid reservoir which is placed in the abdomen. To induce an erection, the patient squeezes the pump within the scrotum, which pulls fluid from the reservoir to inflate the penile cylinders. To return to the flaccid state, the patient pushes a button on the pump and the fluid leaves the cylinders and returns to the reservoir. The inflatable device results in a more physiologic-appearing erection than the malleable prosthesis.
The penile prosthesis is typically reserved for patients who have not responded to less-invasive ED treatments, though it may be considered as a first-line therapy. Preoperative patient counselling is important to manage postoperative outcomes and expectations 33.
Novel therapies
As many patients fail to respond to traditional therapies for ED, research is ongoing into the development of novel treatment approaches. These treatment options are still considered experimental and, per the AUA guidelines and the Sexual Medicine Society of North America Position Statement on Restorative Therapies for ED, should not be administered outside of a research setting in compliance with Institutional Review Board approval 5, 34.
Penile shockwave therapy
Low-intensity extracorporeal shockwave therapy (LI-ESWT) has been investigated as a therapy that may improve blood vessel function and promote the growth of new blood vessels in the setting of cardiovascular disease. Based on this, groups have begun investigating LI-ESWT as a potential treatment option for ED caused by vascular disease 35. A protocol for this therapy was first developed by Vardi et al. in 2010, and this group was able to show that LI-ESWT for ED is well tolerated and results in significant improvement in penile blood flow, which was correlated with improvement in erectile function six months following treatment 35. While still experimental, LI-ESWT has more recently been shown to improve patient response to oral PDE5 inhibitors and may allow patients who previously did not respond to these drugs to have erections sufficient for penetration using them following LI-ESWT 36. Short-term outcomes are promising, but, as this is a new therapy, data regarding long-term outcomes are lacking. Kitrey et al. recently evaluated 156 patients who had undergone 12 treatment sessions over a nine-week period, with 5 treatment points along the penis and a total of 1,500 shockwaves administered at a frequency of 120 shocks per minute. These patients were followed for two years post-treatment. During the follow up period, the clinically effective response decreased over time, from 64% response rate one month following treatment to a 34% response rate at two years. This group hypothesized that a higher rate of treatment failure may be related to more-severe ED and more medical comorbidities at baseline prior to the start of treatment 37. Though preliminary results with LI-ESWT are promising, additional research needs to be done to determine long-term efficacy and side effects, and currently this treatment modality is offered only as part of a clinical trial.
Stem cell therapy
There has been recent interest in the use of stem cells to treat ED. In animal studies, the injection of stem cells following prostate radiation has shown restoration of erectile function via the regeneration of cavernosal nerves 38. Small phase 1 studies in humans have shown promising results in terms of tolerability, safety, and efficacy of use of intracavernosal stem cell transplant for the treatment of ED 39. Interestingly, a recent study has suggested that the combination of LI-ESWT and stem cell therapy may promote the growth of new blood vessels and decrease the destruction of cells within the penile corpora, more than either therapy alone 40. Much more work needs to be done in this field to understand the long-term efficacy and safety of this therapy, which remains investigational at this time.
Platelet-rich plasma
Platelets produce growth factors which are important in wound healing and the growth of new blood vessels. Intracavernosal injection of PRP in animal models has shown improvement in erectile function in cases of neurogenic ED 41. This has been translated into human studies, and a recent study of four patients with ED treated with PRP resulted in improvement in erectile function, with no serious adverse events 42. Additional studies need to be done to determine if this is reproducible on a larger scale.
External penile prosthesis
Despite advances in medical and surgical treatments for ED, many patients may have an incomplete or unsatisfactory result to treatment or may not be able to afford more-invasive surgical treatments 43. Over-the-counter sexual aids may be a more affordable, minimally invasive, and effective alternative to traditional ED treatments. The challenge with the use of these devices may be twofold: physicians may be less knowledgeable about the variety and cost of these options, and patients may find the notion of sexual aids to be stigmatized with a vulgar or embarrassing connotation 26. It has been suggested that describing sexual aids as external penile prostheses may “medicalize” these tools and may increase the physician’s comfort in prescribing these devices and increase patient willingness to use them 43, 44.
A variety of external devices exist as sexual aids, including penile sleeves, extenders, support devices, and the banded prosthetic phallus 26. These devices allow for the preservation of penetrative intercourse in the setting of ED and may be combined with various physical shapes or vibratory stimulation technology to enhance intercourse.
The external penile prosthesis is a prosthetic phallus that is strapped around the patient’s waist. While it may seem difficult to conceive that a prosthetic phallus could result in rewarding penetrative intercourse for the patient, the neurophysiology surrounding the perception of appendages is complex, and it has been suggested that the incorporation of other senses can allow for a sensation that the prosthetic phallus is the patient’s own phallus, and orgasm may still be achieved by the patient and partner with the use of an external penile prosthesis 26.
Satisfaction with these treatment options depends on both the patient and the partner, so extensive counselling should be provided in the office to maximize success rates 26. Little research exists regarding the effectiveness and variety of external prosthetic devices and alternative treatments for ED, but these treatment options may be more accessible, less invasive, and more cost effective for the appropriate group of patients. More work needs to be done to understand patient and partner outcomes following treatment with these prosthetic devices.
Conclusion
There have been many developments in treatments for ED. Traditional therapies including lifestyle modifications, oral medications, injections, and penile prostheses have shown great efficacy in the management of ED. However, research on novel approaches remains sparse, and alternative treatment modalities including external penile prostheses have been slow to gain acceptance in the scientific community. External penile prostheses and LI-ESWT have shown promise as treatment options for men with ED, with few side effects and high cost-effectiveness. More research needs to be done to fully appreciate the role these options may play in the management of ED.
Abbreviations
AUA, American Urological Association; cGMP, cyclic guanosine monophosphate; ED, erectile dysfunction; GTP, guanosine triphosphate; ICI, intracavernosal injection; LI-ESWT, low-intensity extracorporeal shockwave therapy; NO, nitric oxide; PDE5, phosphodiesterase type 5; PGE1, prostaglandin E1; PRP, platelet-rich plasma; VED, vacuum-assisted erectile device.
Editorial Note on the Review Process
F1000 Faculty Reviews are commissioned from members of the prestigious F1000 Faculty and are edited as a service to readers. In order to make these reviews as comprehensive and accessible as possible, the referees provide input before publication and only the final, revised version is published. The referees who approved the final version are listed with their names and affiliations but without their reports on earlier versions (any comments will already have been addressed in the published version).
The referees who approved this article are:
Wayne Hellstrom, Department of Urology, Tulane University School of Medicine, New Orleans, USA
Arthur L Burnett, Department of Urology, The James Buchanan Brady Urological Institute, The Johns Hopkins Medical Institutions, Baltimore, USA
Funding Statement
The author(s) declared that no grants were involved in supporting this work.
[version 1; referees: 2 approved]
References
- 1. Sánchez-Cruz JJ, Cabrera-León A, Martín-Morales A, et al. : Male erectile dysfunction and health-related quality of life. Eur Urol. 2003;44(2):245–53. 10.1016/S0302-2838(03)00215-X [DOI] [PubMed] [Google Scholar]
- 2. Kovac JR: A critical analysis of the 2014 CUA guidelines for erectile dysfunction: Is there more that can be done? Can Urol Assoc J. 2015;9(1–2):30–1. 10.5489/cuaj.2731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McCabe MP, Sharlip ID, Lewis R, et al. : Risk Factors for Sexual Dysfunction Among Women and Men: A Consensus Statement From the Fourth International Consultation on Sexual Medicine 2015. J Sex Med. 2016;13(2):153–67. 10.1016/j.jsxm.2015.12.015 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 4. Wassersug R, Wibowo E: Non-pharmacological and non-surgical strategies to promote sexual recovery for men with erectile dysfunction. Transl Androl Urol. 2017;6(Suppl 5):S776–S794. 10.21037/tau.2017.04.09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Burnett AL, Nehra A, Breau RH, et al. : Erectile Dysfunction: AUA Guideline. J Urol. 2018;200(3):633–41. 10.1016/j.juro.2018.05.004 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 6. Melnik T, Soares BG, Nasello AG: Psychosocial interventions for erectile dysfunction. Cochrane Database Syst Rev. 2007;128(3):CD004825. 10.1002/14651858.CD004825.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kukula KC, Jackowich RA, Wassersug RJ: Eroticization as a factor influencing erectile dysfunction treatment effectiveness. Int J Impot Res. 2014;26(1):1–6. 10.1038/ijir.2013.29 [DOI] [PubMed] [Google Scholar]
- 8. Maiorino MI, Bellastella G, Esposito K: Lifestyle modifications and erectile dysfunction: what can be expected? Asian J Androl. 2015;17(1):5–10. 10.4103/1008-682X.137687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cheng JY, Ng EM, Ko JS, et al. : Physical activity and erectile dysfunction: meta-analysis of population-based studies. Int J Impot Res. 2007;19(3):245–52. 10.1038/sj.ijir.3901521 [DOI] [PubMed] [Google Scholar]
- 10. Bacon CG, Mittleman MA, Kawachi I, et al. : Sexual function in men older than 50 years of age: results from the health professionals follow-up study. Ann Intern Med. 2003;139(3):161–8. 10.7326/0003-4819-139-3-200308050-00005 [DOI] [PubMed] [Google Scholar]
- 11. Kolotkin RL, Head S, Hamilton M, et al. : Assessing Impact of Weight on Quality of Life. Obes Res. 1995;3(1):49–56. 10.1002/j.1550-8528.1995.tb00120.x [DOI] [PubMed] [Google Scholar]
- 12. Kovac JR, Labbate C, Ramasamy R, et al. : Effects of cigarette smoking on erectile dysfunction. Andrologia. 2015;47(10):1087–92. 10.1111/and.12393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Health Risk, Safety and Side Effects | LEVITRA. (accessed 26 September 2018). Reference Source [Google Scholar]
- 14. Nichols DJ, Muirhead GJ, Harness JA: Pharmacokinetics of sildenafil after single oral doses in healthy male subjects: absolute bioavailability, food effects and dose proportionality. Br J Clin Pharmacol. 2002;53 Suppl 1:5S–12S. 10.1046/j.0306-5251.2001.00027.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jung J, Choi S, Cho SH, et al. : Tolerability and pharmacokinetics of avanafil, a phosphodiesterase type 5 inhibitor: a single- and multiple-dose, double-blind, randomized, placebo-controlled, dose-escalation study in healthy Korean male volunteers. Clin Ther. 2010;32(6):1178–87. 10.1016/j.clinthera.2010.06.011 [DOI] [PubMed] [Google Scholar]
- 16. Wrishko R, Sorsaburu S, Wong D, et al. : Safety, efficacy, and pharmacokinetic overview of low-dose daily administration of tadalafil. J Sex Med. 2009;6(7):2039–48. 10.1111/j.1743-6109.2009.01301.x [DOI] [PubMed] [Google Scholar]
- 17. Porst H, Kim ED, Casabé AR, et al. : Efficacy and safety of tadalafil once daily in the treatment of men with lower urinary tract symptoms suggestive of benign prostatic hyperplasia: results of an international randomized, double-blind, placebo-controlled trial. Eur Urol. 2011;60(5):1105–13. 10.1016/j.eururo.2011.08.005 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 18. Montorsi F, McCullough A: Efficacy of sildenafil citrate in men with erectile dysfunction following radical prostatectomy: a systematic review of clinical data. J Sex Med. 2005;2(5):658–67. 10.1111/j.1743-6109.2005.00117.x [DOI] [PubMed] [Google Scholar]
- 19. Porst H, Burnett A, Brock G, et al. : SOP conservative (medical and mechanical) treatment of erectile dysfunction. J Sex Med. 2013;10(1):130–71. 10.1111/jsm.12023 [DOI] [PubMed] [Google Scholar]
- 20. Corona G, Razzoli E, Forti G, et al. : The use of phosphodiesterase 5 inhibitors with concomitant medications. J Endocrinol Invest. 2008;31(9):799–808. 10.1007/BF03349261 [DOI] [PubMed] [Google Scholar]
- 21. Ströberg P, Hedelin H, Ljunggren C: Prescribing all phosphodiesterase 5 inhibitors to a patient with erectile dysfunction--a realistic and feasible option in everyday clinical practice--outcomes of a simple treatment regime. Eur Urol. 2006;49(5):900–7. 10.1016/j.eururo.2006.02.032 [DOI] [PubMed] [Google Scholar]
- 22. Gong B, Ma M, Xie W, et al. : Direct comparison of tadalafil with sildenafil for the treatment of erectile dysfunction: a systematic review and meta-analysis. Int Urol Nephrol. 2017;49(10):1731–40. 10.1007/s11255-017-1644-5 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 23. Cui H, Liu B, Song Z, et al. : Efficacy and safety of long-term tadalafil 5 mg once daily combined with sildenafil 50 mg as needed at the early stage of treatment for patients with erectile dysfunction. Andrologia. 2015;47(1):20–4. 10.1111/and.12216 [DOI] [PubMed] [Google Scholar]
- 24. Lee M, Sharifi R: Non-invasive Management Options for Erectile Dysfunction When a Phosphodiesterase Type 5 Inhibitor Fails. Drugs Aging. 2018;35(3):175–87. 10.1007/s40266-018-0528-4 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 25. Yafi FA, Sharlip ID, Becher EF: Update on the Safety of Phosphodiesterase Type 5 Inhibitors for the Treatment of Erectile Dysfunction. Sex Med Rev. 2018;6(2):242–52. 10.1016/j.sxmr.2017.08.001 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 26. Belew D, Klaassen Z, Lewis RW: Intracavernosal Injection for the Diagnosis, Evaluation, and Treatment of Erectile Dysfunction: A Review. Sex Med Rev. 2015;3(1):11–23. 10.1002/smrj.35 [DOI] [PubMed] [Google Scholar]
- 27. Nelson CJ, Hsiao W, Balk E, et al. : Injection anxiety and pain in men using intracavernosal injection therapy after radical pelvic surgery. J Sex Med. 2013;10(10):2559–65. 10.1111/jsm.12271 [DOI] [PubMed] [Google Scholar]
- 28. Costa P, Potempa AJ: Intraurethral alprostadil for erectile dysfunction: a review of the literature. Drugs. 2012;72(17):2243–54. 10.2165/11641380-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 29. Liu C, Lopez DS, Chen M, et al. : Penile Rehabilitation Therapy Following Radical Prostatectomy: A Meta-Analysis. J Sex Med. 2017;14(12):1496–503. 10.1016/j.jsxm.2017.09.020 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 30. Scott FB, Bradley WE, Timm GW: Management of erectile impotence. Use of implantable inflatable prosthesis. Urology. 1973;2(1):80–2. 10.1016/0090-4295(73)90224-0 [DOI] [PubMed] [Google Scholar]
- 31. Bernal RM, Henry GD: Contemporary patient satisfaction rates for three-piece inflatable penile prostheses. Adv Urol. 2012;2012:707321. 10.1155/2012/707321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Rajpurkar A, Dhabuwala CB: Comparison of satisfaction rates and erectile function in patients treated with sildenafil, intracavernous prostaglandin E1 and penile implant surgery for erectile dysfunction in urology practice. J Urol. 2003;170(1):159–63. 10.1097/01.ju.0000072524.82345.6d [DOI] [PubMed] [Google Scholar]
- 33. Trost LW, Baum N, Hellstrom WJ: Managing the difficult penile prosthesis patient. J Sex Med. 2013;10(4):893–906; quiz 907. 10.1111/jsm.12115 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 34. SMSNA - SMSNA Position Statement on Restorative Therapies for ED.(accessed 14 November 2018). Reference Source [Google Scholar]
- 35. Vardi Y, Appel B, Jacob G, et al. : Can low-intensity extracorporeal shockwave therapy improve erectile function? A 6-month follow-up pilot study in patients with organic erectile dysfunction. Eur Urol. 2010;58(2):243–8. 10.1016/j.eururo.2010.04.004 [DOI] [PubMed] [Google Scholar]
- 36. Kitrey ND, Gruenwald I, Appel B, et al. : Penile Low Intensity Shock Wave Treatment is Able to Shift PDE5i Nonresponders to Responders: A Double-Blind, Sham Controlled Study. J Urol. 2016;195(5):1550–5. 10.1016/j.juro.2015.12.049 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 37. Kitrey ND, Vardi Y, Appel B, et al. : Low Intensity Shock Wave Treatment for Erectile Dysfunction-How Long Does the Effect Last? J Urol. 2018;200(1):167–70. 10.1016/j.juro.2018.02.070 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 38. Qiu X, Villalta J, Ferretti L, et al. : Effects of intravenous injection of adipose-derived stem cells in a rat model of radiation therapy-induced erectile dysfunction. J Sex Med. 2012;9(7):1834–41. 10.1111/j.1743-6109.2012.02753.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Al Demour S, Jafar H, Adwan S, et al. : Safety and Potential Therapeutic Effect of Two Intracavernous Autologous Bone Marrow Derived Mesenchymal Stem Cells injections in Diabetic Patients with Erectile Dysfunction: An Open Label Phase I Clinical Trial. Urol Int. 2018;101(3):358–65. 10.1159/000492120 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 40. Zhu GQ, Jeon SH, Bae WJ, et al. : Efficient Promotion of Autophagy and Angiogenesis Using Mesenchymal Stem Cell Therapy Enhanced by the Low-Energy Shock Waves in the Treatment of Erectile Dysfunction. Stem Cells Int. 2018;2018:1302672. 10.1155/2018/1302672 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 41. Wu YN, Wu CC, Sheu MT, et al. : Optimization of platelet-rich plasma and its effects on the recovery of erectile function after bilateral cavernous nerve injury in a rat model. J Tissue Eng Regen Med. 2016;10(10):E294–E304. 10.1002/term.1806 [DOI] [PubMed] [Google Scholar]; F1000 Recommendation
- 42. Matz EL, Pearlman AM, Terlecki RP: Safety and feasibility of platelet rich fibrin matrix injections for treatment of common urologic conditions. Investig Clin Urol. 2018;59(1):61–5. 10.4111/icu.2018.59.1.61 [DOI] [PMC free article] [PubMed] [Google Scholar]; F1000 Recommendation
- 43. Tatem A, Kovac JR: External penile prosthesis as a novel approach to the treatment of erectile dysfunction. Transl Androl Urol. 2017;6(Suppl 5):S795–S796. 10.21037/tau.2017.11.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Gray RE, Klotz LH: Restoring sexual function in prostate cancer patients: an innovative approach. Can J Urol. 2004;11(3):2285–9. [PubMed] [Google Scholar]