Abstract
Objective:
To compare five-year outcomes and changes over time of a client-centred activities of daily living (ADL) intervention versus usual ADL interventions for people with stroke and their significant others.
Design:
Five-year follow-up of a cluster-randomized controlled trial where a client-centred ADL intervention (n = 129) or usual ADL interventions (n = 151) were delivered to people with stroke.
Setting:
Multicentre study including 16 inpatient or home-based rehabilitation units.
Participants:
People with stroke and significant others.
Intervention:
The client-centred ADL intervention aimed at enabling agency in daily activities and participation in everyday life and at reducing caregiver burden.
Main measures:
For people with stroke, perceived participation (Stroke Impact Scale), independence in ADL, life satisfaction, and use of formal/informal care were measured. For significant others, caregiver burden, life satisfaction, and mood (Hospital Anxiety and Depression Scale) were assessed.
Results:
Five years post-intervention, data were collected from 145 people with stroke (intervention group: n = 71/control group: n = 74) and 75 significant others (intervention group: n = 36/control group: n = 39). For those with stroke, the Participation domain of the Stroke Impact Scale showed no group differences at year five (68.9 vs 75.4, P = 0.062) or in changes over time. At year five, the control group had better outcomes regarding Other help/supervision. Significant others in the control group were more likely to show signs of depression at year five (odds ratio = 22.3; P < 0.001).
Conclusion:
The client-centred ADL intervention appears to render similar long-term effects as usual ADL interventions for people with stroke, but for significant others signs of depression might be reduced.
Keywords: Stroke rehabilitation, rehabilitation, occupational therapy, follow-up studies, evaluation studies, longitudinal studies, caregivers
Introduction
Stroke often has long-lasting consequences, both for people with stroke themselves1–4 and for their significant others.5–8 It is, therefore, important to continue developing rehabilitation interventions that target needs of both these groups and to monitor their effectiveness over time. However, despite the large number of people who undergo rehabilitation after stroke each year, long-term follow-up studies are still rare. This prospective five-year follow-up study of people who have had a stroke and their significant others is addressing this gap.
There is evidence that client-centred activities of daily living (ADL) interventions, that is, interventions based on the client’s ability, perceived needs, and lived experiences, are efficient and therefore preferable in stroke rehabilitation.9 A client-centred ADL intervention for people with stroke was developed,10 which took the person’s unique lived experiences as the point of departure for collaboration and goal-setting during the rehabilitation process in order to enable people with stroke to assume responsibility for their own rehabilitation, ADL, and participation in daily life. However, neither the three-month nor the one-year follow-up showed any differences in the primary outcome perceived participation between the intervention group and the control group, which had received usual ADL interventions. This was true both for those with stroke10,11 and for their significant others.10,12
However, unlike for the significant others in the control group, the caregiver burden factor ‘General strain’ improved significantly between 3 and 12 months for the significant others in the intervention group.12 In addition, the qualitative findings revealed that in the context of the client-centred ADL intervention, participants with stroke experienced a sense of responsibility and ownership of their rehabilitation13 and significant others reported that they were encouraged by the person with stroke to create space for their own needs again.14 Taken together, these aspects might in a longer perspective alleviate caregiver burden.
Longer than one-year follow-ups are vital in order to capture outcomes of complex rehabilitation processes and interventions that might appear gradually and to investigate their sustainability. The client-centred ADL intervention provided a structure for how to discover and solve problems in daily activities after stroke15 and the use of goal-directed problem-solving strategies.16 When these strategies are incorporated into everyday life, the expected behavioural changes likely occur gradually over a prolonged period of time. Consequently, differences in outcomes between interventions may take time to emerge.
Accordingly, the objective of this study was to compare the long-term outcomes of a client-centred ADL intervention with outcomes from usual ADL interventions in people with stroke and their significant others. The hypothesis was that those who received the client-centred ADL intervention after stroke would have better outcomes five years later compared to those who received the usual ADL interventions regarding perceived participation in daily life, independence in ADL, use of formal and informal care, self-efficacy, life satisfaction, reintegration into normal living, and mood state. An additional hypothesis was that their significant others would have better outcomes concerning caregiver burden, informal care given, mood state, life satisfaction, and participation.
Methods
This is a five-year follow-up of a multicentre, cluster-randomized trial (stratified into inpatient <65 years; inpatient ⩾65 years; home rehabilitation), based on the Consolidated Standards Of Reporting Trials (CONSORT) guidelines for non-pharmacological trials.17 Ethical approvals for the original trial (ClinicalTrials.gov NCT01417585) and the five-year follow-up were obtained from the Ethical Committee in Stockholm, reference numbers 2009/727-31/1 and 2014/996-32. Details of the methodology and the results of the original trial are available in previous works.10,11,18 In short, 16 rehabilitation units in three Swedish county councils were included and randomized so as to provide either client-centred ADL intervention (intervention group) or usual ADL interventions (control group). Participants were recruited among people with stroke admitted to these units between 6 October 2009 and 7 September 2011. Between 21 January 2010 and 5 September 2012, significant others were also included and invited to take part in the rehabilitation process.
Recruitment to the present five-year follow-up study took place between 2014 and 2016. All those people with stroke from the original trial who were still alive were contacted by telephone, or, if there was no response, by letter with a prepaid reply envelope. Information on addresses, and whether the individuals were alive, was collected from the Swedish population register. Information about the study was given and, for those who were willing to participate, a date for data collection in the participant’s home was agreed upon. Informed consent was obtained when meeting the participant, before initiating data collection. The procedure was similar for the significant others. If possible, they were interviewed on the same occasion as the person with stroke. If this was impossible, written information about the study was left in the home of the person with stroke for their significant other, together with a consent form, the questionnaire, and a prepaid reply envelope.
Data collection
At the five-year follow-up, the data collectors were the same as in the previous data collection and still blinded. The instruments and points of data collection used in this study are outlined in Supplemental Table S1. Mostly, the same instruments as in the original trial were used and, as previously, perceived participation for those with stroke was the primary outcome. At the five-year follow-up, instruments were added to assess both the people with stroke and their significant others regarding mood state and for those with stroke regarding fatigue, self-efficacy, and reintegration into normal living.
The following outcomes were used for people with stroke:
The primary outcome of perceived participation was assessed with the Participation domain of the Stroke Impact Scale 2.0,19 where a higher score reflects fewer problems after stroke. The proxy version20 was used when the person with stroke was unable to self-report. The perceived Recovery after stroke was assessed with a visual analogue scale, where 0 reflects ‘no recovery’ and 100 indicates ‘full recovery’.
A secondary outcome measure for perceived participation, more specifically focused on identifying restrictions (gaps) in participation in everyday occupations, was the 30-item version of the Occupational Gaps Questionnaire.21 For each activity item, discrepancies between what the person actually does and what he or she wishes to do are registered as occupational gaps, with a larger number of gaps indicating more restrictions in participation.
To assess frequency of participation in social and complex everyday activities pre- and post-stroke, the Frenchay Activities Index22,23 was used. Higher scores indicate a more active lifestyle in recent months.
The Katz Extended Scale24 was used to assess the self-reported use of assistance (yes/no) in six personal and four instrumental ADL both pre- and post-stroke.
At inclusion, the Barthel Index25,26 was used to determine stroke severity. Higher total score from the 10 personal ADL and mobility items reflects less dependency in ADL. Scores of <15 were classified as severe stroke, 15–49 as moderate stroke, and 50–100 as mild stroke.27
People with stroke self-reported whether or not they received formal care in terms of Home-help service or Personal assistance. Presence, or not, of informal care defined as Other regular help or supervision was also self-reported.
To assess perceived self-efficacy in performing everyday activities, a Self-Efficacy Scale28,29 was adapted for people with stroke. Confidence in performing 18 common everyday activities was rated, where higher scores indicate better self-efficacy.
The global question ‘My life as a whole’ in the 11-item Life Satisfaction Scale (LiSat-11)30,31 was used to assess the participants’ overall satisfaction with life.
The Swedish version of the Reintegration to Normal Living Index32,33 was used to globally assess perceived quality of life by evaluating satisfaction within 11 daily activities and family roles post-stroke. Higher scores reflect better reintegration to a premorbid pattern of living.
The Hospital Anxiety and Depression Scale34 was used to assess mood. Higher scores on the Anxiety and Depressions subscales indicate lower mood, that is, more anxiety or depressive symptoms.
Fatigue severity was assessed using the Fatigue Severity Scale.35 All original nine statement items were scored, but as recommended36 the first two items were removed. Higher scores indicate more severe fatigue.
The following outcomes were used for significant others:
The Caregiver’s Burden Scale8,37 was used to assess the burden of care as perceived by the significant others. A higher score reflects greater burden of care. The significant others reported whether they assisted the person with stroke in Personal ADL (yes/no), Instrumental ADL (yes/no), and in Other activities that before the stroke were performed independently or that had been added due to the stroke (yes/no).
Informal care was assessed by the use of the question ‘To what extent do you assist your significant other?’ which was reported on a visual analogue scale where 0 reflects ‘not at all’ and 100 reflects ‘to a great extent’. Assessment of mood, that is, anxiety and depression, was performed by use of the Hospital Anxiety and Depression Scale.38 The recommended cut-off of ⩾8 was used for identifying signs of anxiety and depression in the general population.
The ‘My life as a whole’ item in LiSat-11 was used to assess the overall satisfaction with life.30,39
Restrictions (gaps) in participation in everyday occupations were identified by use of the 30-item version of the Occupational Gaps Questionnaire,21 with a larger number of gaps indicating greater restriction in participation.
Statistical methods
Descriptive statistics were used to report baseline participant characteristics. Per protocol analysis was used, that is, only people with stroke and significant others who contributed data at the five-year follow-up were included in the analyses. Dropout analysis was performed for those with stroke by testing the relation between attrition at five years and categorical variables (intervention group, stroke severity, rehabilitation cluster, Katz Extended Scale pre-stroke, sex, marital status, and educational level) with chi-square or Fisher’s exact. The Mann Whitney U test was used to test differences between those who dropped out and those who provided data at year five on continuous variables (age at stroke onset, Frenchay Activitites Index pre-stroke, and Stroke Impact Scale Recovery at baseline).
In all analysis, scores from the Katz Extended Scale were trichotomized into ‘dependent in both Personal ADL and Instrumental ADL’, ‘dependent in either Personal ADL or Instrumental ADL’, and ‘independent in both Personal ADL and Instrumental ADL’. Scores on the ‘My life as a whole’ item in LiSat-11 were dichotomized into ‘not satisfied’ (scores 1–4) and ‘satisfied’ (scores 5–6), a validated scale reduction.39
Outcomes at year five were compared cross-sectionally between the intervention group and control group using analysis of covariance (ANCOVA) for continuous variables, that is, Stroke Impact Scale, Occupational Gaps Questionnaire, Frenchay Activities Index, Hospital Anxiety and Depression Scale, Self-Efficacy Scale, Reintegration to Normal Living Index, and Fatigue Severity Scale for the persons with stroke, and Caregiver’s Burden Scale, ‘To what extent do you assist?’, Hospital Anxiety and Depression Scale, and Occupational Gaps Questionnaire for the significant others. After fitting the general linear model, the residuals were examined and extreme cases which could have a major impact on the model were identified by means of Cook’s distance. Such cases were excluded and the model reanalysed.
For categorical variables, that is, LiSat-11, formal/informal care, and Katz Extended Scale (for the people with stroke) and informal care, clinical cut-offs of Hospital Anxiety and Depression Scale, and LiSat-11 (for the significant others), binary or multinomial logistic regression analyses were performed. In cases when the cells in the cross-tabulation of the outcome variable and the independent variables were zero, exact tests of the parameters for the specified effects were computed. Results were presented as odds ratios with 95% confidence intervals (CIs).
For analyses of differences in change between baseline/3 months and five years, and 12 months and five years, respectively, in the intervention and control groups, linear mixed-effects models were used for the continuous outcomes Stroke Impact Scale Participation and Frenchay Activities Index for those with stroke and for Caregiver’s Burden Scale for the significant others. For categorical outcomes, generalized estimating equations were applied using the same time points regarding Katz Extended Scale, and LiSat-11 for those with stroke, and for the significant others regarding provision of informal care in Personal ADL, Instrumental ADL and Other activities, and LiSat-11.
Covariates included in all statistical analyses of people with stroke were age at stroke onset, sex, marital status, educational level, Frenchay Activities Index at baseline (i.e. pre-stroke situation), Katz Extended Scale at baseline (i.e. pre-stroke situation), and stroke severity. In the cross-sectional analysis, Mini-Mental State Examination year 5 was also included. For the significant others, sex of the significant other, age at stroke onset for the person with stroke, cohabiting, Katz Extended Scale for the person with stroke pre-stroke, and stroke severity were included as covariates in all statistical analysis.
A statistician blinded to which group had received which intervention performed the analyses, using SAS and SPSS software, and the significance level was set to ⩽0.05. The original trial was powered for a one-year follow-up with an expected attrition of 20%.10 Even though it was underpowered for a five-year comparison of the primary outcome perceived participation, the lack and importance of long-term studies following rehabilitation after stroke guided the decision to carry out this five-year follow-up.
Results
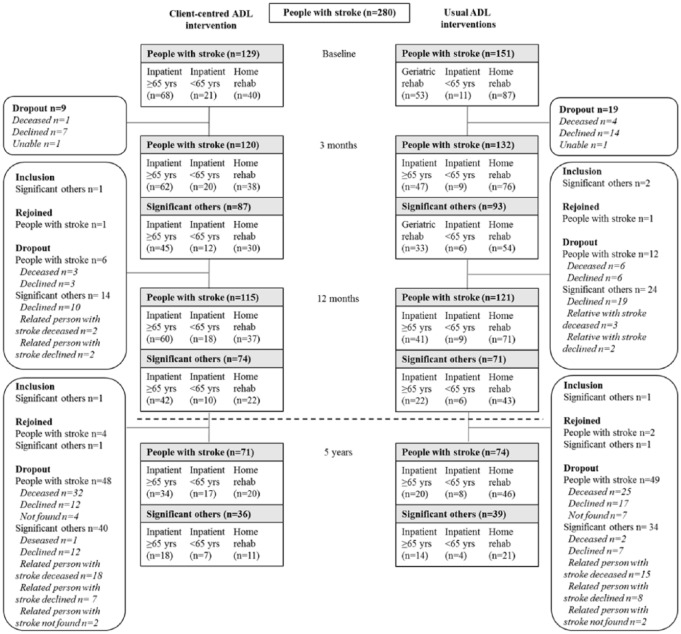
Between 5 August 2014 and 16 June 2016, 145 people with stroke (52% of those included in the original trial) and 75 significant others (41% of those included in the original trial) participated in the present five-year follow-up study. Participant flow from baseline to follow-up at five years is illustrated in Figure 1. At year five, in total, 71 people with stroke (25%) originally included had deceased, which means that 209 people with stroke were eligible. Also, those with stroke who had declined participation at the 12-month follow-up were approached. Of the 209 eligible persons with stroke, 29 (14%) declined participation in the five-year follow-up and 11 (5%) could not be found.
Figure 1.
Participant flow from baseline to follow-up at five years.
Baseline data for those with stroke and significant others participating in the five-year follow-up are presented in Table 1. People with stroke who did not participate in the five-year follow-up were older (P < 0.001), less active before stroke onset (P < 0.001), more often suffered a moderate or severe stroke (P = 0.009), and more often lived alone (P = 0.010), compared to those with stroke who participated. There was a trend towards being more dependent as regards ADL before stroke onset in the attrition group (P = 0.052). There were no differences between those with stroke who contributed with data at the five-year follow-up and those who did not regarding intervention group allocation (P = 0.314), sex (P = 0.625), educational level (P = 0.205), or Stroke Impact Scale Recovery at inclusion (P = 0.866).
Table 1.
Baseline characteristics of people with stroke and of significant others followed up at year five.
| Characteristic | Client-centred ADL | Usual ADL |
|---|---|---|
| People with stroke | n = 71 | n = 74 |
| Age, mean years (SD) | 71 (9) | 68 (9) |
| Men/women, n (%) | 41/30 (58/42) | 48/26 (65/35) |
| Cohabiting, n (%) | 44 (62) | 49 (66) |
| Educational level, n (%) | ||
| Elementary school | 32 (45) | 30 (41) |
| High school | 17 (24) | 23 (31) |
| University | 22 (31) | 21 (28) |
| Pre-stroke | ||
| Frenchay Activities Index (0–45), mean (SD) | 32 (7) | 33 (6) |
| Katz Extended Scale, n (%) yes | ||
| Dependent in Personal ADL and Instrumental ADL | 4 (6) | 2 (3) |
| Dependent in either Personal ADL or Instrumental ADL | 18 (25) | 21 (28) |
| Independent in Personal ADL and Instrumental ADL | 49 (69) | 51 (69) |
| Post-stroke | ||
| Hemisphere, n (%) | ||
| Left | 33 (46) | 32 (43) |
| Right | 36 (51) | 39 (53) |
| Unspecified | 2 (3) | 3 (4) |
| Haemorrhage, n (%) | 11 (15) | 12 (16) |
| Infarct, n (%) | 52 (73) | 53 (72) |
| Unspecified stroke, n (%) | 8 (11) | 9 (12) |
| Stroke severity, n (%) | ||
| Mild (Barthel Index = 50–100) | 55 (78) | 70 (95) |
| Moderate (Barthel Index = 15–49) | 15 (21) | 4 (5) |
| Severe (Barthel Index ⩽15) | 1 (1) | 0 (0) |
| Mini-Mental State Examination (0–30), mean (SD) | 25 (6) | 26 (4) |
| Barthel Index (0–100), mean (SD) | 66 (23) | 78 (18) |
| Stroke Impact Scale: recovery (0–100), mean (SD) | 33 (22) | 41 (23) |
| Significant others | n = 36 | n = 39 |
| Age, mean years (SD) | 65 (17) | 69 (10) |
| Men/women, n (%) | 11/25 (31/69) | 8/31 (20/80) |
| Cohabiting, n (%) | 23 (66) | 30 (77) |
| Relation to the person with stroke, n (%) | ||
| Partner | 23 (64) | 31 (80) |
| Child | 10 (28) | 4 (10) |
| Other relationship | 3 (8) | 4 (10) |
| Caregiver’s Burden Scale (22–88), mean (SD) | 41 (12) | 45 (16) |
| Assists in Personal ADL, % yes | 41 | 53 |
| Assists in Instrumental ADL, % yes | 78 | 71 |
| Assists in Other activities, % yes | 83 | 80 |
ADL, activities of daily living.
Comparisons of outcomes at five years for people with stroke in the intervention and control groups are presented in Table 2. At the five-year follow-up, there were no differences between the groups in the primary outcome perceived participation. The odds of receiving ‘Other regular help or supervision’ five years after stroke were significantly lower for those in the control group. There were no other group differences regarding the secondary outcomes at year five for the people with stroke.
Table 2.
Comparison of outcomes at the five-year follow-up for people with stroke.a
| Measure (range) | Client-centred ADL (n = 71) | (n) | Usual ADL (n = 74) | (n) | Mean difference Client-centred ADL–usual ADL (95% CI) |
Odds ratio Usual ADL versus client-centred ADL (95% CI) |
P-value |
|---|---|---|---|---|---|---|---|
| Stroke Impact Scale (0–100) | |||||||
| Participation, mean (SD) | 68.9 (20.6) | (67) | 75.4 (20.9) | (72) | –6.5 (–13.3 to 0.3) | 0.062 | |
| Recovery, mean (SD) | 58.7 (24.3) | (67) | 63.5 (27.1) | (71) | –4.8 (–13.4 to 3.8) | 0.270 | |
| Occupational Gaps Questionnaire (0–30), mean (SD) | 4.9 (4.1) | (67) | 4.2 (3.4) | (69) | 0.7 (–0.6 to 2.0) | 0.293 | |
| Frenchay Activities Index (0–45), mean (SD) | 22.7 (10.5) | (68) | 22.9 (11.1) | (72) | –0.2 (–3.2 to 2.7) | 0.885 | |
| Hospital Anxiety and Depression Scale: Anxiety (0–21), mean (SD) |
4.5 (3.6) | (67) | 4.8 (3.7) | (70) | –0.3 (–1.6 to 1.0) | 0.611 | |
| Hospital Anxiety and Depression Scale: Depression (0–21), mean (SD) |
4.3 (3.5) | (67) | 4.7 (3.5) | (70) | –0.4 (–1.6 to 0.7) | 0.474 | |
| Self-Efficacy Scale (18–180), mean (SD) | 141.3 (34.4) | (67) | 138.6 (40.4) | (71) | 2.7 (–8.2 to 13.6) | 0.621 | |
| Reintegration to Normal Living Index (11–44), mean (SD) | 35.5 (6.9) | (67) | 36.1 (7.2) | (70) | –0.6 (–3.0 to 1.8) | 0.617 | |
| Fatigue Severity Scale (7–49), mean (SD) | 26.6 (11.9) | (67) | 29.1 (12.7) | (69) | –2.6 (–6.9 to 1.8) | 0.245 | |
| LiSat-11 (Satisfied with life = no/yes), n (%) yes | 32 (45) | (70) | 28 (38) | (71) | 0.6 (0.2 to 1.3) | 0.219 | |
| Home-help service (no/yes), n (%) yes | 23 (32) | (71) | 15 (20) | (72) | 1.1 (0.4 to 2.9) | 0.821 | |
| Personal assistancea (no/yes), n (%) yes | 2 (3) | (66) | 1 (1) | (65) | |||
| Other regular help or supervision (no/yes), n (%) yes | 41 (58) | (69) | 22 (30) | (67) | 0.4 (0.2 to 0.8) | 0.012 | |
| Katz Extended Scale | |||||||
| 0 = dependent in Personal ADL and Instrumental ADL, n (%), versus 2 | 27 (38) | (71) | 23 (31) | (73) | 1.2 (0.4 to 3.5) | 0.717 | |
| 1 = dependent in Personal ADL or Instrumental ADL, n (%),versus 2 | 25 (35) | (71) | 24 (32) | (73) | 0.9 (0.4 to 2.2) | 0.795 | |
| 2 = independent in Personal ADL and Instrumental ADL, n (%) | 19 (27) | (71) | 26 (35) | (73) | – | – | |
Statistical comparison was not possible due to too few participants with this type of formal help.
ADL, activities of daily living; CI, confidence interval.
In Table 3, outcomes at five years are presented for significant others of those with stroke in the intervention and control groups. There were no differences between the significant other groups as regards caregiver burden or in their provision of informal help in Personal ADL, Instrumental ADL or Other activities, signs of anxiety, or life satisfaction. There was a trend towards higher odds of the significant others assisting in Personal ADL in the control group. At year five, significant others of people with stroke who had received client-centred ADL intervention scored significantly lower on the Depression domain of the Hospital Anxiety and Depression Scale compared to significant others of people with stroke who had received usual ADL interventions. The odds of showing signs of depression according to the ⩾8 cut-off on the Hospital Anxiety and Depression Scale were significantly higher for significant others in control group.
Table 3.
Comparison of outcomes at the five-year follow-up for significant others.
| Measure (range) | Client-centred ADL | (n) | Usual ADL | (n) | Mean difference Client-centred ADL–usual ADL (95% CI) |
Odds ratio Usual ADL versus client-centred ADL (95% CI) |
P-value |
|---|---|---|---|---|---|---|---|
| Caregiver’s Burden Scale (22–88), mean (SD) | 39.8 (12.5) | (35) | 44.5 (17.5) | (38) | −4.7 (−12.0 to 2.5) | 0.196 | |
| To what extent do you assist? (0–100), mean (SD) | 39.1 (26.3) | (34) | 45.1 (30.9) | (36) | −6.0 (−20.1 to 8.1) | 0.402 | |
| Assists in Personal ADL (yes/no), n (%) yes | 4 (11) | (36) | 11 (28) | (39) | 4.6 (0.96 to 22.0) | 0.056 | |
| Assists in Instrumental ADL (yes/no), n (%) yes | 18 (50) | (36) | 19 (49) | (39) | 1.0 (0.4 to 3.0) | 0.939 | |
| Assists in Other activities (yes/no), n (%) yes | 26 (72) | (36) | 28 (74) | (38) | 1.7 (0.5 to 5.6) | 0.380 | |
| Hospital Anxiety and Depression Scale: Anxiety (0–21), mean (SD) | 4.0 (3.9) | (34) | 5.6 (3.9) | (38) | −1.6 (−3.3 to 0.1) | 0.069 | |
| Hospital Anxiety and Depression Scale: Signs of anxiety according to ⩾8 cut-off (yes/no), n (%) yes | 7 (19) | (34) | 14 (36) | (38) | 2.8 (0.9 to 9.1) | 0.086 | |
| Hospital Anxiety and Depression Scale: Depression (0–21), mean (SD) | 2.3 (1.8) | (35) | 4.0 (3.9) | (38) | −1.7 (–3.0 to −0.5) | 0.005 | |
| Hospital Anxiety and Depression Scale: Signs of depression according to ⩾8 cut-off (yes/no), n (%) yes | 0 (0) | (35) | 8 (21) | (38) | 22.3 (3.8 to infinity) | <0.001 | |
| LiSat-11 (Satisfied with life = no/yes), n (%) yes | 17 (49) | (35) | 18 (46) | (39) | 1.1 (0.4 to 2.8) | 0.922 | |
| Occupational Gaps Questionnaire (0–30), mean (SD) | 2.3 (3.3) | (30) | 2.9 (3.4) | (36) | −0.6 (−2.0 to 0.7) | 0.329 |
ADL, activities of daily living; CI, confidence interval.
P-value in bold are statistically significant.
For those with stroke, changes over the five-year study time were not related to which intervention they had received regarding the primary outcome perceived participation as assessed with the Stroke Impact Scale (P = 0.488) or the secondary outcomes Frenchay Activities Index (P = 0.526), Katz Extended Scale (P = 0.795), and LiSat-11 (P = 0.451). The outcomes for those with stroke at 3 months, 12 months, and five years on the above variables are presented in Table 4.
Table 4.
Outcomes at three months and one and five years for people with stroke and significant others in the client-centred ADL intervention and usual ADL intervention groups.
| Measurement (range) | People with stroke (client-centred ADL (n = 71), usual ADL (n = 74)) |
Significant others (client-centred ADL (n = 36), usual ADL (n = 39)) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 3 months | 12 months | 5 years | 12 months | 5 years | ||||||
| Client-centred ADL | Usual ADL | Client-centred ADL | Usual ADL | Client-centred ADL | Usual ADL | Client-centred ADL | Usual ADL | Client-centred ADL | Usual ADL | |
| Katz Extended Scale | ||||||||||
| Dependent in Personal ADL and Instrumental ADL, % | 40.6 | 36.5 | 41.8 | 27.8 | 38.0 | 31.5 | – | – | – | – |
| Dependent in Personal ADL or Instrumental ADL, % | 42.0 | 33.8 | 32.8 | 38.9 | 35.2 | 32.9 | – | – | – | – |
| Independent in Personal ADL and Instrumental ADL, % | 17.4 | 29.7 | 25.4 | 33.3 | 26.8 | 35.6 | – | – | – | – |
| Stroke Impact Scale: Participation (0–100), mean (SD) | 53.5 (21.2) | 62.4 (21.2) | 66.5 (20.5) | 71.0 (20.8) | 67.5 (20.6) | 73.1 (20.9) | – | – | – | – |
| Frenchay Activities Index (0–45), mean (SD) | – | – | 21.9 (9.2) | 24.8 (10.1) | 21.3 (10.5) | 24.0 (11.1) | – | – | – | – |
| LiSat-11 (satisfied: yes/no), % yes | 40.6 | 40.5 | 35.8 | 42.3 | 45.7 | 39.4 | 60.6 | 53.3 | 48.6 | 46.2 |
| Caregiver’s Burden Scale (22–88), mean (SD) | – | – | – | – | – | – | 39.2 (11.3) | 42.2 (13.9) | 39.7 (12.5) | 45.1 (17.5) |
| Assists in Personal ADL (yes/no), % yes | – | – | – | – | – | – | 40.6 | 46.4 | 11.1 | 28.2 |
| Assists in Instrumental ADL (yes/no), % yes | – | – | – | – | – | – | 75.0 | 67.9 | 50.0 | 48.7 |
| Assists in Other activities (yes/no), % yes | – | – | – | – | – | – | 66.7 | 75.9 | 72.2 | 73.7 |
ADL, activities of daily living; CI, confidence interval.
P-value in bold are statistically significant.
For the sample as a whole, after adjusting for the covariates, the Stroke Impact Scale domain Participation improved over time (P < 0.001), indicating less stroke-related restrictions in participation at five years than at three months, while the Frenchay Activities Index indicated less frequent participation in social and complex activities at five years than pre-stroke (P < 0.001). Regarding Katz Extended Scale, the odds of being more independent were significantly higher at year five than at three months for the sample as a whole (odds ratio = 1.45, P = 0.025). For LiSat-11, no significant difference in log odds (P = 0.690) were found between three months and year five regarding the odds of being satisfied with life as a whole.
For the significant others, five-year changes regarding the Caregiver’s Burden Scale (P = 0.515), their provision of informal care in Personal ADL (P = 0.512), Instrumental ADL (P = 0.849) or Other activities (P = 0.565), for example, administrating economy, and LiSat-11 (p = 0.460), were not related to which intervention those with stroke had received. The outcomes for significant others at 12 months and five years on the above variables are displayed in Table 4.
Overall, after adjusting for the covariates, no indication of change in caregiver burden was found between inclusion of the significant others three months after stroke onset and five years (P = 0.530). Regarding informal care, the odds of assisting in Personal ADL were significantly lower at year five than at three months for the sample as a whole (odds ratio = 0.21, P < 0.001). The odds of assisting in Instrumental ADL were significantly lower at year five than at three months for the sample as a whole (odds ratio = 0.30, P < 0.001). For informal care in Other activities, no overall significant difference in log odds (P = 0.304) were found between year five and three months, and the same was true for LiSat-11, regarding the odds of being satisfied with life as a whole (P = 0.857).
Discussion
For the people with stroke, this five-year follow-up – as well as previous 3- and 12-month follow-ups10,11 – could detect no better or worse effects of the client-centred ADL intervention compared to usual ADL interventions, neither for the primary outcome perceived participation nor for secondary outcomes such as independence in ADL and life satisfaction. This was the case both for group comparisons at year five and for the comparison of changes between three months and five years.
Both groups improved significantly between three months and five years regarding perceived participation and independence in ADL, but neither group had at year five reached the same frequency of participating in everyday activities as before stroke. The assumption that adaptive behavioural changes as a result of the client-centred ADL intervention would occur with delay – and eventually lead to a more favourable outcome regarding participation in everyday life – could not be verified.
For the significant others, no changes over time were found that favoured the client-centred ADL intervention. In both groups, a smaller share of the significant others assisted in Personal ADL and Instrumental ADL at five years compared to at three months. However, at year five, better outcomes were found for significant others of those with stroke who received the client-centred ADL intervention regarding mean depression score, as well as the proportion with signs of depression according to the ⩾8 cut-off on the Hospital Anxiety and Depression Scale. A reflection on this last somewhat unexpected finding will initiate the discussion.
At year five, significant others in the client-centred ADL intervention group had significantly lower depression scores, and a smaller proportion of them showed signs of depression based on the recommended clinical cut-off38 compared to significant others in the usual ADL interventions group. In fact, no significant others in the client-centred ADL intervention group showed signs of depression based on this cut-off at year five, while more than one-fifth of the significant others in the usual ADL interventions group did. This is an interesting finding, as the client-centred ADL intervention was not specifically designed to meet the needs of the significant others.
Qualitative findings from the first year of the same trial suggested that the client-centred ADL intervention seemed to enable the significant others gradually to find ways to meet their own needs.14 Furthermore, a significant within-group change regarding the caregiver burden factor ‘General strain’ was observed in the 12-month follow-up among the significant others in the client-centred ADL intervention group.12 Thus, the group differences regarding signs of depression identified in the present five-year follow-up study may relate to a development that started already during the first year among the significant others of those with stroke who received client-centred ADL intervention.
Overall, the people with stroke were significantly more likely to be independent in Personal ADL and Instrumental ADL at year five compared to at three months, which is consistent with the finding that, overall, a smaller proportion of the significant others provided support in Personal ADL and Instrumental ADL year five. Nevertheless, the perceived caregiver burden remained unchanged among the significant others as a whole, and the estimates of life satisfaction of both the significant others and the people with stroke were not changed between three months and five years. The odds of significant others assisting the people with stroke in ‘Other activities’ did not decrease over time for the sample as a whole; about 75% of the significant others in both groups still provided such assistance five years after stroke, which might have contributed to unrelieved caregiver burden.
Although these are encouraging findings, the lower degree and proportion of depression signs among the significant others in the client-centred ADL intervention group year five were not reflected in a lower perceived caregiver burden or better life satisfaction in that group. Sustained caregiver burden for significant others several years after stroke, despite improved ADL abilities for their relative with stroke, has also been found in earlier research,8 as have long-term lower levels of life satisfaction.5 Both caregiver burden and quality of life are complex phenomena, obviously including more aspects than the effects of dependence/independence in Personal ADL and Instrumental ADL and mood state. This challenges healthcare professionals to continued efforts in developing long-term supportive interventions with a broad scope for the significant others of persons with stroke.
This five-year follow-up found no significant group differences at year five on the primary outcome perceived participation. One explanation might be that the considerable attrition among those with stroke resulted in lack of power to detect a potential group difference. Another possibility is that the selected instrument was not sensitive enough to capture changes in this outcome. However, the fact that significant improvements over time were detected for people with stroke in both groups regarding perceived participation to some extent contradicts this scenario.
Given that no group differences were detected in previous follow-ups either regarding perceived participation,10,11 a plausible explanation is that the control and experimental interventions might have been too similar. The usual ADL interventions might well have included client-centred elements of practice, because this perspective has in past decades been embraced by many occupational therapists.40 Thus, experiences in the context of receiving the client-centred ADL intervention identified in earlier qualitative studies, for example, responsibility and ownership of the rehabilitation process among those with stroke13 and the possibility to create space for one’s own needs as a significant other,14 could also have been present in the usual ADL interventions.
A major limitation in this study is the lack of power. The dropout analysis suggests that more vulnerable people with stroke tended to drop out. Those who left the study had a poorer position both before and after their stroke and were more likely to be living alone. However, this situation is probably evenly distributed across the groups, as group allocation was not significantly related to attrition. Thus, the attrition does not seem to affect the conclusions regarding the group comparisons for the people with stroke. Another limitation is that baseline data regarding the Hospital Anxiety and Depression Scale was not available. Therefore, it is not certain that the significant others in the client-centred ADL intervention and usual ADL interventions groups had a similar mood state before the intervention started, which means that the finding of fewer signs of depression among significant others in the client-centred ADL intervention group needs to be interpreted with caution.
Finally, this study did not include all the information that might affect how the participants perceived outcomes such as participation, dependence/independence, and life satisfaction. For example, information on potential new strokes or other major life events were not controlled for. However, the study offers a unique long-term follow-up of a rigorous cluster-randomized controlled trial comparing several relevant outcomes of client-centred and usual ADL interventions after stroke, covering both the perspective of those with stroke and their significant others. Given the finding of fewer signs of depression among significant others in the client-centred ADL intervention group, it is worth investigating further the indirect influence on the significant others when people with stroke are enabled to take responsibility for their own rehabilitation and continue to apply a problem-solving strategy over time.
Clinical messages.
For people with stroke, the client-centred ADL intervention does not appear to render better or worse long-term effects than the usual ADL interventions regarding participation and independence in activities of daily living.
At year five, significant others of people with stroke who had received client-centred ADL intervention less often showed signs of depression.
Supplemental Material
Supplemental material, Supplemental_Material for Five-year follow-up of a cluster-randomized controlled trial of a client-centred activities of daily living intervention for people with stroke by Annicka Hedman, Gunilla Eriksson, Lena von Koch and Susanne Guidetti in Clinical Rehabilitation
Acknowledgments
The authors thank the people with stroke and their significant others who participated for over the years repeatedly sharing experiences of life post-stroke with us and the occupational therapists who helped with recruitment and data collection.
Footnotes
Author contributions: All authors formulated the research questions in consensus and contributed to the quality review of data. Hedman compiled the results from the statistical analyses performed by a statistician and drafted the manuscript. Eriksson supervised the data collection, gave advice regarding the statistical analyses, and provided input to the draft. Von Koch gave advice regarding the statistical analyses and provided input to the draft. Guidetti was responsible for the design of the study, supervised the data collection, and provided input to the draft.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The following funders made the project possible: The Swedish Research Council (VR), the Swedish Stroke Association, and the Uppsala-Örebro Regional Research Council.
Supplemental material: Supplemental material for this article is available online.
ORCID iDs: Annicka Hedman  https://orcid.org/0000-0001-5082-8998
https://orcid.org/0000-0001-5082-8998
Susanne Guidetti  https://orcid.org/0000-0001-6878-6394
https://orcid.org/0000-0001-6878-6394
References
- 1. Achten D, Visser-Meily JMA, Post MWM, et al. Life satisfaction of couples 3 years after stroke. Disabil Rehabil 2012; 34(17): 1468–1472. [DOI] [PubMed] [Google Scholar]
- 2. Bergstrom A, Guidetti S, Tham K, et al. Association between satisfaction and participation in everyday occupations after stroke. Scand J Occup Ther 2017; 24(5): 339–348. [DOI] [PubMed] [Google Scholar]
- 3. Elf M, Eriksson G, Johansson S, et al. Self-reported fatigue and associated factors six years after stroke. PLoS ONE 2016; 11(8): e0161942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ytterberg C, Dyback M, Bergstrom A, et al. Perceived impact of stroke six years after onset, and changes in impact between one and six years. J Rehabil Med 2017; 49(8): 637–643. [DOI] [PubMed] [Google Scholar]
- 5. Abzhandadze T, Forsberg-Wärleby G, Holmegaard L, et al. Life satisfaction in spouses of stroke survivors and control subjects: a 7-year follow-up of participants in the Sahlgrenska Academy study on ischaemic stroke. J Rehabil Med 2017; 49(7): 550–557. [DOI] [PubMed] [Google Scholar]
- 6. Berg A, Palomäki H, Lönnqvist J, et al. Depression among caregivers of stroke survivors. Stroke 2005; 36(3): 639–643. [DOI] [PubMed] [Google Scholar]
- 7. Bergström AL, Eriksson G, von Koch L, et al. Combined life satisfaction of persons with stroke and their caregivers: associations with caregiver burden and the impact of stroke. Health Qual Life Outcomes 2011; 9(1): 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Elmståhl S, Malmberg B, Annerstedt L. Caregiver’s burden of patients 3 years after stroke assessed by a novel caregiver burden scale. Arch Phys Med Rehabil 1996; 77(2): 177–182. [DOI] [PubMed] [Google Scholar]
- 9. Kristensen HK, Persson D, Nygren C, et al. Evaluation of evidence within occupational therapy in stroke rehabilitation. Scand J Occupat Ther 2011; 18(1): 11–25. [DOI] [PubMed] [Google Scholar]
- 10. Bertilsson A-S, Ranner M, von Koch L, et al. A client-centred ADL intervention: three-month follow-up of a randomized controlled trial. Scand J Occupat Ther 2014; 21(5): 377–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Guidetti S, Ranner M, Tham K, et al. A ‘client-centred activities of daily living’ intervention for persons with stroke: one-year follow-up of a randomized controlled trial. J Rehabil Med 2015; 47(7): 605–611. [DOI] [PubMed] [Google Scholar]
- 12. Bertilsson A-S, Eriksson G, Ekstam L, et al. A cluster randomized controlled trial of a client-centred, activities of daily living intervention for people with stroke: one year follow-up of caregivers. Clin Rehabil 2016; 30(8): 765–775. [DOI] [PubMed] [Google Scholar]
- 13. Ranner M. Evaluation and experiences of a client-centred ADL intervention after stroke. Stockholm: Karolinska Institutet, 2016. [Google Scholar]
- 14. Bertilsson A-S, von Koch L, Tham K, et al. Client-centred ADL intervention after stroke: significant others’ experiences. Scand J Occupat Ther 2015; 22(5): 377–386. [DOI] [PubMed] [Google Scholar]
- 15. Tham K, Borell L, Gustavsson A. The discovery of disability: a phenomenological study of unilateral neglect. Am J Occupat Ther 2000; 54(4): 398–406. [DOI] [PubMed] [Google Scholar]
- 16. Polatajko HJ, Mandich AD, Missiuna C, et al. Cognitive Orientation to Daily Occupational Performance (CO-OP). Phys Occupat Ther Pediatr 2001; 20(2–3): 107–123. [PubMed] [Google Scholar]
- 17. Boutron I, Altman DG, Moher D, et al. Consort statement for randomized trials of nonpharmacologic treatments: a 2017 update and a consort extension for nonpharmacologic trial abstracts. Ann Intern Med 2017; 167(1): 40–47. [DOI] [PubMed] [Google Scholar]
- 18. Flink M, Bertilsson A-S, Johansson U, et al. Training in client-centeredness enhances occupational therapist documentation on goal setting and client participation in goal setting in the medical records of people with stroke. Clin Rehabil 2016; 30(12): 1200–1210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Duncan PW, Wallace D, Lai SM, et al. The Stroke Impact Scale Version 2.0. Evaluation of reliability, validity, and sensitivity to change. Stroke 1999; 30(10): 2131–2140. [DOI] [PubMed] [Google Scholar]
- 20. Duncan PW, Lai SM, Tyler D, et al. Evaluation of proxy responses to the Stroke Impact Scale. Stroke 2002; 33(11): 2593–2599. [DOI] [PubMed] [Google Scholar]
- 21. Eriksson G, Tham K, Kottorp A. A cross-diagnostic validation of an instrument measuring participation in everyday occupations: the Occupational Gaps Questionnaire (OGQ). Scand J Occupat Ther 2013; 20(2): 152–160. [DOI] [PubMed] [Google Scholar]
- 22. Holbrook M, Skilbeck CE. An activities index for use with stroke patients. Age Ageing 1983; 12(2): 166–170. [DOI] [PubMed] [Google Scholar]
- 23. Post MW, de Witte LP. Good inter-rater reliability of the Frenchay Activities Index in stroke patients. Clin Rehabil 2003; 17(5): 548–552. [DOI] [PubMed] [Google Scholar]
- 24. Asberg KH, Sonn U. The cumulative structure of personal and instrumental ADL. A study of elderly people in a health service district. Scand J Rehabil Med 1989; 21(4): 171–177. [PubMed] [Google Scholar]
- 25. Mahoney F, Barthel D. Functional evaluation: the Barthel Index. Maryland State Med J 1965; 14: 61–65. [PubMed] [Google Scholar]
- 26. Quinn TJ, Langhorne P, Stott DJ. Barthel index for stroke trials: development, properties, and application. Stroke 2011; 42(4): 1146–1151. [DOI] [PubMed] [Google Scholar]
- 27. Govan L, Langhorne P, Weir CJ. Categorizing stroke prognosis using different stroke scales. Stroke 2009; 40(10): 3396–3399. [DOI] [PubMed] [Google Scholar]
- 28. Bandura A. The nature and structure of self-efficacy. In: Bandura A. (ed.) Self-efficacy: the exercise of control. Basingstoke: W. H. Freeman, 1997, pp.3–5. [Google Scholar]
- 29. Denison E, Asenlöf P, Lindberg P. Self-efficacy, fear avoidance, and pain intensity as predictors of disability in subacute and chronic musculoskeletal pain patients in primary health care. Pain 2004; 111(3): 245–252. [DOI] [PubMed] [Google Scholar]
- 30. Fugl-Meyer AR, Melin R, Fugl-Meyer KS. Life satisfaction in 18- to 64-year-old Swedes: in relation to gender, age, partner and immigrant status. J Rehabil Med 2002; 34(5): 239–246. [DOI] [PubMed] [Google Scholar]
- 31. Jacobsson L, Lexell J. Life satisfaction after traumatic brain injury: comparison of ratings with the Life Satisfaction Questionnaire (LiSat-11) and the Satisfaction With Life Scale (SWLS). Health Qual Life Outcomes 2016; 14(1): 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Merz ZC, Van Patten R, Mulhauser K, et al. Exploratory factor analysis of the reintegration to normal living index in a stroke population. Top Stroke Rehabil 2017; 24(2): 158–162. [DOI] [PubMed] [Google Scholar]
- 33. Wood-Dauphinee SL, Opzoomer MA, Williams JI, et al. Assessment of global function: the reintegration to Normal Living Index. Arch Phys Med Rehabil 1988; 69(8): 583–590. [PubMed] [Google Scholar]
- 34. Sagen U, Vik TG, Moum T, et al. Screening for anxiety and depression after stroke: comparison of the Hospital Anxiety and Depression Scale and the Montgomery and Åsberg Depression Rating Scale. J Psychosom Res 2009; 67(4): 325–332. [DOI] [PubMed] [Google Scholar]
- 35. Krupp LB, LaRocca NG, Muir-Nash J, et al. The fatigue severity scale: application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol 1989; 46(10): 1121–1123. [DOI] [PubMed] [Google Scholar]
- 36. Lerdal A, Kottorp A. Psychometric properties of the Fatigue Severity Scale – Rasch analyses of individual responses in a Norwegian stroke cohort. Int J Nurs Stud 2011; 48(10): 1258–1265. [DOI] [PubMed] [Google Scholar]
- 37. Visser-Meily JMA, Post MWM, Riphagen II, et al. Measures used to assess burden among caregivers of stroke patients: a review. Clin Rehabil 2004; 18(6): 601–623. [DOI] [PubMed] [Google Scholar]
- 38. Bjelland I, Dahl AA, Haug TT, et al. The validity of the Hospital Anxiety and Depression Scale. J Psychosom Res 2002; 52(2): 69–77. [DOI] [PubMed] [Google Scholar]
- 39. Melin R, Fugl-Meyer K, Fugl-Meyer A. Life satisfaction in 18- to 64-year-old Swedes: in relation to education, employment situation, health and physical activity. J Rehabil Med 2003; 35(2): 84–90. [DOI] [PubMed] [Google Scholar]
- 40. Whalley Hammell KR. Client-centred practice in occupational therapy: critical reflections. Scand J Occupat Ther 2013; 20(3): 174–181. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplemental_Material for Five-year follow-up of a cluster-randomized controlled trial of a client-centred activities of daily living intervention for people with stroke by Annicka Hedman, Gunilla Eriksson, Lena von Koch and Susanne Guidetti in Clinical Rehabilitation