Abstract
Purpose
The aim of this report was to describe a case of myopic foveoschisis and a macular hole with retinal detachment that resolved spontaneously.
Observations
A 62-year-old woman with bilateral blurred vision was referred to our department. Her best-corrected visual acuity (BCVA) was 0.4 bilaterally; the standard equivalent refractive error was −17.0 diopters in the right eye and −18.75 diopters in the left eye. The axial length was 31.4 mm and 31.2 mm, respectively. After cataract surgery was performed, the BCVA of the right and left eye was 0.6 and 1.0, respectively. Four years later, slight macular traction, foveoschisis, and the macular hole had progressed in the left eye and the BCVA had decreased to 0.7. However, the macular hole had closed, the foveoschisis had resolved, and retinal detachment had mostly resolved three weeks later. The BCVA improved to 0.8. The macular hole did not reoccur and retinal detachment resolved completely after six more months.
Conclusions and Importance
This case demonstrated that myopic foveoschisis and a macular hole with retinal detachment could improve spontaneously. It is necessary to decide carefully whether surgery is required or whether the patient should be observed.
Keywords: Macular hole, Myopic foveoschisis, Retinal detachment, High myopia
1. Introduction
Vitreous macular traction and myopic foveoschisis are commonly observed in highly myopic eyes,1 and are referred to as myopic traction maculopathy (MTM). Previous reports show that 9–34% of highly myopic eyes with posterior staphyloma have MTM.1,2 The macular hole is also recognized as a complication of highly myopic eyes and can progress to retinal detachment, which impairs visual acuity. Although macular holes with retinal detachment are usually treated with vitreous surgery to release vitreous traction or with a gas tamponade, their prognosis is poor.3 Spontaneous improvement of MTM without surgery has been reported, but spontaneous resolution of a macular hole with MTM is rare.4, 5, 6, 7, 8, 9, 10 Here, we observed a case of myopic foveoschisis and a macular hole with retinal detachment that resolved spontaneously, as demonstrated on spectral-domain optical coherence tomography (SD-OCT).
2. Case report
A 62-year-old woman was referred to our hospital in October 2012. She had visited a local ophthalmologist with the chief complaint of bilateral blurred vision. A cataract was diagnosed and she was referred to our hospital for a consultation. She had a medical history of hypertension. At the initial presentation, her best-corrected visual acuity (BCVA) was 0.4 bilaterally. The standard equivalent refractive error was −17.0 diopters in the right eye and −18.75 diopters in the left eye. The axial length was 31.4 mm and 31.2 mm, while the intraocular pressure (IOP) was 14 mmHg and 15 mmHg in the right and left eyes, respectively. The anterior chamber was deep and no inflammation was observed. Moderate cataract was bilaterally observed and the fundus was obscured.
Phacoemulsification, aspiration, and intraocular lens implantations were performed without complications. Myopic choroidal neovascularization was observed on the right fundus, and the BCVA was 0.6 after cataract surgery. There was no exudative change but scar with pigmentation was observed in the right eye. The BCVA of the left eye improved to 1.0. There was no abnormality of the macula but the optic disc was tilted and peripapillary atrophy was observed in the left eye (Fig. 1a).
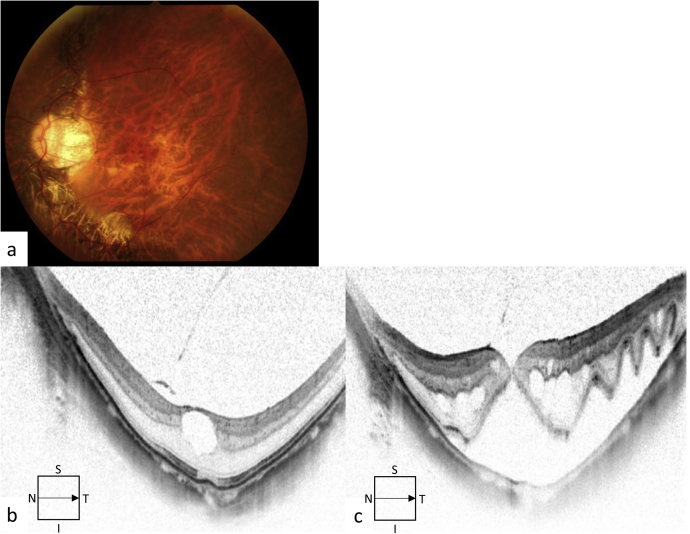
Fig. 1.
The color fundus and spectral-domain optical coherence tomography (SD-OCT) images of the left eye of a 62-year-old female patient. a. The color fundus image of the left eye showed that tilted optic disc and peripapillary atrophy. b. The SD-OCT image showed macular traction with partial posterior vitreous detachment (PVD). A macular hole was observed. c. The SD-OCT image showed that foveoschisis and the small macular hole had progressed after six months. The retinal outer layer was wavy above the subretinal fluid. (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
After observation for four years, SD-OCT showed slight macular traction with partial posterior vitreous detachment (PVD), retinal schisis, and a macular hole in the left eye that was classified into stage 1A according to Gass's classification (Fig. 1b). The BCVA remained at 1.0. However, foveoschisis and the macular hole with retinal detachment progressed and the BCVA deteriorated to 0.7 after 6 months (Fig. 1c). The macular hole was stage 4 and the IOP was 17 mmHg. Therefore, we planned vitreous surgery according to the patient's schedule.
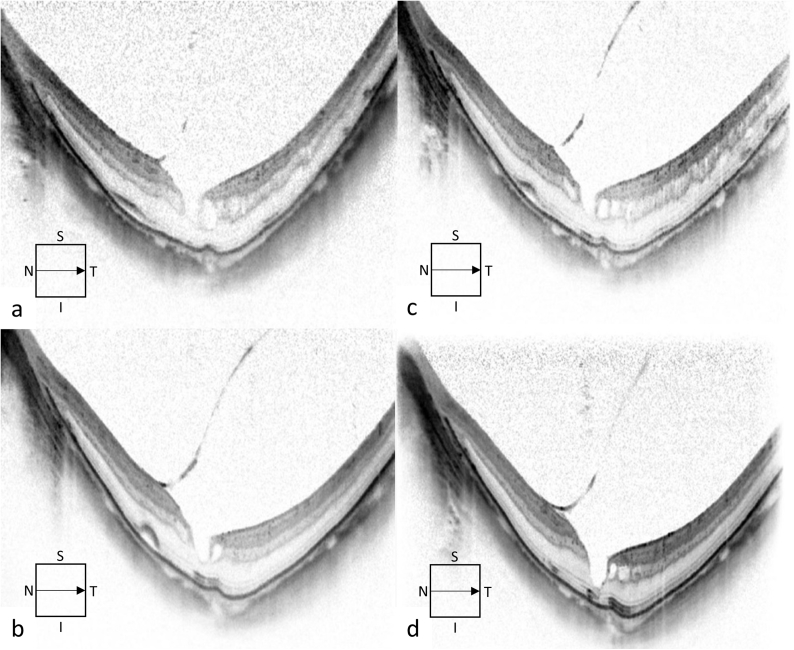
However, when the patient was admitted for vitreous surgery three weeks later, it was found that the macular hole had closed, foveoschisis had resolved, and retinal detachment had mostly resolved (Fig. 2a). An inner lamellar macular hole and slight retinal detachment remained. The BCVA had improved to 0.8 and the IOP was 16 mmHg. After consultation with the patient, the surgery was cancelled and observation was continued. The macular hole did not recur after two or after four months (Fig. 2b and c). Furthermore, the retinal detachment resolved completely after six months (Fig. 2d). The BCVA was 0.7 and the IOP was 15 mmHg. SD-OCT images showed that partial PVD progressed slowly but was not complete during observation; there was no change in the internal limiting membrane.
Fig. 2.
The natural course of spectral-domain optical coherence tomography (SD-OCT) images of the left eye of a 62-year-old female patient. a. On admission, the macular hole of the left eye was closed but slight retinal detachment and foveoschisis remained. Posterior vitreous detachment (PVD) was not completed. b. After two months, foveoschisis improved with partial PVD. Retinal detachment remained. c. The SD-OCT image showed that the subretinal fluid decreased after four months. d. The retinal detachment resolved completely without reemergence of the macular hole after six months. Slight foveoschisis remained.
3. Discussion
Shimada et al. reported that although 3.9% of MTMs improved over three years of observation, 11.6% of them progressed.11 If traction progresses and causes a macular hole or retinal detachment, surgical repair is necessary. However, 27.3% of macular hole occurred after vitreous surgery for MTM although the surgery was effective for treating MTM.12 It is difficult to determine whether surgical intervention is necessary and to determine the correct timing of the surgery because exacerbation and natural resolution are both possible. A highly myopic macular hole with foveoschisis was reported to have a worse outcome than without foveoschisis.13 Our case was an example of the former type but foveoschisis and a macular hole with retinal detachment improved spontaneously with good visual acuity. This result strongly suggested that it was necessary to decide carefully whether surgery or observation was appropriate.
In the current case, slight retinal schisis and an inner lamellar macular hole were observed after cataract surgery. Retinal schisis progressed due to foveal traction. Furthermore, the macular hole opened and the subretinal fluid increased. Subsequently, the retinal detachment, macular hole, and foveoschisis spontaneously resolved. We hypothesized the possible mechanism of this resolution. SD-OCT images showed that the PVD was not complete and it slowly progressed. The site of attachment of the vitreous membrane to the macula also changed. Therefore, vitreous macula traction could be relieved as the PVD progressed. In fact, Lee et al. reported that a large macular hole closed completely with no retinal schisis10; they described that the spontaneous release of vitreoretinal traction was important. Additionally, spontaneous closure of macular hole with retinal detachment was rare.10 Although it is not necessary to close a macular hole to resolve retinal detachment, closure of the macular hole may lead to reattachment of the retina through the natural absorption of subretinal fluid. In our case, the size of the macular hole was small, which may have contributed to spontaneous closure. SD-OCT showed that the detached retina was wavy above the subretinal fluid and it was distant from the scleral curve with posterior staphyloma. The detached and easily-moved retina may have contributed to spontaneous closure of the macular hole.
Changes in the radius of posterior staphyloma are suggested to be another cause of spontaneous resolution of retinal detachment of myopic eyes. Baba et al. reported that scleral imbrication combined with vitrectomy was effective for myopic schisis.14 Hoang et al. reported that changes of radius of curvature of posterior staphyloma were related to spontaneous improvement of myopic schisis.15 In this case, minor morphologic changes that altered the tractional force to the internal limiting membrane may have occurred during observation, but the change was not apparent on the OCT images. It is necessary to accumulate more cases with high myopia to examine long-term changes in the radius of curvature of posterior staphyloma.
Based on the classification of the MTM according to the size of the macular retinoschisis as proposed by Shimada et al., the case was classified as S4, the most severe retinal schisis.11 This type is unstable and may easily progress or improve. The progress of MTM is related to axial length, chorioretinal atrophy, PVD, and tears of the internal limiting membrane. The PVD could change the traction of the macula, resulting in improvement of the macular hole and retinal detachment or in worsening of them. However, Lai et al. reported that foveal detachment in cases of high myopia improved naturally, unrelated to PVD.4 Our case suggested that even severe retinal schisis and macular detachment might resolve spontaneously.
SD-OCT is widely used to evaluate the interface between the retina and the vitreous body currently. Our case suggested that frequent observations with SD-OCT were useful at short intervals to observe the occurrence or exacerbation of retinal detachment and to decide when to operate. When retinal detachment occurs and does not improve, surgical intervention is necessary. If foveal traction improves during follow-up, it may be possible to only observe retinal detachment; surgery may not be necessary. On contrary, vitreous surgery may be required at an early stage for cases with severe chorioretinal atrophy that could not absorb subretinal fluid. The use of gas tamponade could be another option. It is less invasive and is reported to be an effective approach for the treatment of myopic foveoschisis.16
4. Conclusions
This report showed that myopic foveoschisis and a macular hole with retinal detachment improved spontaneously. Additional long-term studies including more cases are needed to determine the mechanisms and the treatment.
Patient consent
Written informed consent was obtained from the subject prior to the collection of any data.
Acknowledgements and disclosure
Conflicts of interest
None of the authors have any financial disclosures related to this submission.
Authorship
All authors attest that they meet the current ICMJE criteria for authorship.
Funding
No funding or grant support.
Acknowledgements
None.
References
- 1.Takano M., Kishi S. Foveal retinoschisis and retinal detachment in severely myopic eyes with posterior staphyloma. Am J Ophthalmol. 1999;128(4):472–476. doi: 10.1016/s0002-9394(99)00186-5. [DOI] [PubMed] [Google Scholar]
- 2.Baba T., Hirose A., Kawazoe Y., Mochizuki M. Optical coherence tomography for retinal detachment with a macular hole in a highly myopic eye. Ophthalmic Surg Laser Imag. 2003;34(6):483–484. [PubMed] [Google Scholar]
- 3.Gaucher D., Haouchine B., Tadayoni R. Long-term follow-up of high myopic foveoschisis: natural course and surgical outcome. Am J Ophthalmol. 2007;143(3):455–462. doi: 10.1016/j.ajo.2006.10.053. [DOI] [PubMed] [Google Scholar]
- 4.Lai T.T., Ho T.C., Yang C.M. Spontaneous resolution of foveal detachment in traction maculopathy in high myopia unrelated to posterior vitreous detachment. BMC Ophthalmol. 2016;16:18. doi: 10.1186/s12886-016-0195-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hirota K., Hirakata A., Inoue M. Dehiscence of detached internal limiting membrane in eyes with myopic traction maculopathy with spontaneous resolution. BMC Ophthalmol. 2014;14:39. doi: 10.1186/1471-2415-14-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Polito A., Lanzetta P., Del Borrello M., Bandello F. Spontaneous resolution of a shallow detachment of the macula in a highly myopic eye. Am J Ophthalmol. 2003;135(4):546–547. doi: 10.1016/s0002-9394(02)02080-9. [DOI] [PubMed] [Google Scholar]
- 7.Yu J., Jiang C., Xu G. Spontaneous closure of a myopic macular hole with retinal reattachment in an eye with high myopia and staphyloma: a case report. BMC Ophthalmol. 2014;14:111. doi: 10.1186/1471-2415-14-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brue C., Rossiello I., Guidotti J.M., Mariotti C. Spontaneous closure of a fully developed macular hole in a severely myopic eye. Case Rep Ophthalmol Med. 2014;2014:182892. doi: 10.1155/2014/182892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li Y., Jonas J.B., Lu L. Spontaneous closure of highly myopic macular hole associated with retinal detachment. Acta Ophthalmol. 2014;92(5):e408–410. doi: 10.1111/aos.12338. [DOI] [PubMed] [Google Scholar]
- 10.Lee S.J., Kim Y.C. Spontaneous resolution of macular hole with retinal detachment in a highly myopic eye. Kor J Ophthalmol. 2017;31(6):572–573. doi: 10.3341/kjo.2017.0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shimada N., Tanaka Y., Tokoro T., Ohno-Matsui K. Natural course of myopic traction maculopathy and factors associated with progression or resolution. Am J Ophthalmol. 2013;156(5):948–957 e941. doi: 10.1016/j.ajo.2013.06.031. [DOI] [PubMed] [Google Scholar]
- 12.Fujimoto M., Hangai M., Suda K., Yoshimura N. Features associated with foveal retinal detachment in myopic macular retinoschisis. Am J Ophthalmol. 2010;150(6):863–870. doi: 10.1016/j.ajo.2010.06.023. [DOI] [PubMed] [Google Scholar]
- 13.Alkabes M., Pichi F., Nucci P. Anatomical and visual outcomes in high myopic macular hole (HM-MH) without retinal detachment: a review. Graefes Arch Clin Exp Ophthalmol. 2014;252(2):191–199. doi: 10.1007/s00417-013-2555-5. [DOI] [PubMed] [Google Scholar]
- 14.Baba T., Tanaka S., Nizawa T., Oshitari T., Yamamoto S. Scleral imbrication combined with pars plana vitrectomy without internal limiting membrane peeling for myopic schisis. Retina. 2016;36(10):1927–1934. doi: 10.1097/IAE.0000000000001023. [DOI] [PubMed] [Google Scholar]
- 15.Hoang Q.V., Chen C.L., Garcia-Arumi J., Sherwood P.R., Chang S. Radius of curvature changes in spontaneous improvement of foveoschisis in highly myopic eyes. Br J Ophthalmol. 2016;100(2):222–226. doi: 10.1136/bjophthalmol-2015-306628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu T.Y., Yang C.H., Yang C.M. Gas tamponade for myopic foveoschisis with foveal detachment. Graefes Arch Clin Exp Ophthalmol. 2013;251(5):1319–1324. doi: 10.1007/s00417-012-2192-4. [DOI] [PubMed] [Google Scholar]