Abstract
Background:
Active patients with musculoskeletal pain are not immune to psychological or psychiatric disease. Observations suggest that patients undergoing hip arthroscopic surgery may have an increased prevalence of comorbid psychiatric conditions.
Hypothesis:
Patients undergoing hip arthroscopic surgery have an increased prevalence of concomitant psychiatric diagnoses compared with the general population as well as those undergoing anterior cruciate ligament (ACL) reconstruction.
Study Design:
Case-control study; Level of evidence, 3.
Methods:
A retrospective review of a medical claims database spanning from 2007 to 2016 was utilized to identify patients with a Current Procedural Terminology (CPT) code indicating that they had undergone hip arthroscopic surgery. This group was then dichotomized to those with or without an International Classification of Diseases, 9th Revision (ICD-9) and 10th Revision (ICD-10) diagnosis code indicating a psychological or psychiatric condition at any time before hip arthroscopic surgery or up to 2 years after hip arthrscopic surgery. As a control, ICD-9 and ICD-10 diagnosis codes for psychological or psychiatric conditions were determined in patients without a CPT code for hip arthroscopic surgery (general population) as well as for 2 surgical groups: those undergoing ACL reconstruction and those undergoing shoulder stabilization surgery. Prevalence was determined in all groups and compared using chi-square analysis.
Results:
There were 22,676,069 patients in the database, with 2428 undergoing hip arthroscopic surgery. Those undergoing hip arthroscopic surgery had a 3-fold increased prevalence of concomitant psychiatric diagnoses compared with the general population (52% vs 17%, respectively; P < .0001). There was a significant difference in the prevalence of psychiatric diagnoses in the hip arthroscopic surgery group between male and female patients (46% vs 56%, respectively; P = .0061), with depression and anxiety being the 2 most common comorbid conditions. Those undergoing hip arthroscopic surgery also had a significantly increased prevalence of concomitant psychiatric diagnoses versus those undergoing ACL reconstruction (52% vs 28%, respectively; P < .0001) as well as those undergoing shoulder stabilization surgery (52% vs 42%, respectively; P < .0001).
Conclusion:
Patients undergoing hip arthroscopic surgery had an increased prevalence of comorbid psychiatric conditions compared with the general population as well as those undergoing ACL reconstruction or shoulder stabilization surgery. Depression and anxiety were the most prevalent concomitant psychiatric diagnoses.
Keywords: hip, arthroscopic surgery, psychiatric, psychological, psych, anxiety, depression
Hip pain is common in the general population.4,6 Although other diagnoses are possible, one of the main causes of hip pain in active patients is femoroacetabular impingement (FAI).6 FAI can lead to cartilage and labral damage due to abnormal contact of the acetabular rim and proximal femur during movement.6 Although FAI can be treated using open surgical techniques, arthroscopic surgery is now the primary method of treatment for symptomatic FAI.4,6,9
There has been an increased recognition of psychiatric disorders in athletically active populations, with prevalence rates ranging from 15% to 21%.3,16 The prevalence of psychiatric disease in the general population is reported to be lower than this, with 7% of all United States adults diagnosed with a psychiatric disorder at some point during a 1-year period.16 Given this difference, it has been hypothesized that more athletically inclined patients may be more prone to develop and experience psychiatric disorders, possibly because of the demands of sporting activity as well as a variety of behavioral characteristics.10,16
This increased prevalence of mental health issues presents a concern for patients undergoing surgery, as there is a correlation between psychological symptoms and inferior postoperative outcomes.1,8,12,13 In those undergoing hip replacement, patients who have psychological symptoms before surgery have inferior clinical outcomes after surgery, even if their prior physical state was comparable with that of other nondistressed patients.8 In patients undergoing rotator cuff repair, it has been noted that higher levels of self-reported pain are more related to higher baseline psychological distress (as measured using a specific questionnaire) than to the severity of their rotator cuff injury.14,17 For those undergoing hip arthroscopic surgery, it has been reported that higher levels of baseline psychological distress are related to increased difficulty in controlling postoperative pain.13 In addition, symptom severity has been significantly more related to mental health status than the size of the labral tear or FAI deformity.5
To our knowledge, no study has examined the prevalence of concomitant psychological or psychiatric comorbidities in patients undergoing hip arthroscopic surgery. We sought to determine if there was an increased prevalence of psychiatric disorders in patients undergoing hip arthroscopic surgery versus the general population as well as those undergoing anterior cruciate ligament (ACL) reconstruction or shoulder stabilization surgery. We hypothesized that patients undergoing hip arthroscopic surgery would have an increased prevalence of psychiatric diagnoses compared with the other populations.
Methods
To conduct this study, we performed a review of a large medical records database, (PearlDiver). PearlDiver offers access to several databases including the Medicare Standard Analytic Files (SAFs), which contain approximately 50 million patient records from 2007 to 2014, and the Humana claims database, which contains approximately 21 million patient records from 2007 to 2016. All claims data are deidentified for the purpose of compliance with the Health Insurance Portability and Accountability Act of 1996 (HIPAA). For this study, we restricted our search to the Humana database, as the SAF data set includes almost exclusively Medicare patients older than 65 years and is less representative of the population that we sought to study.
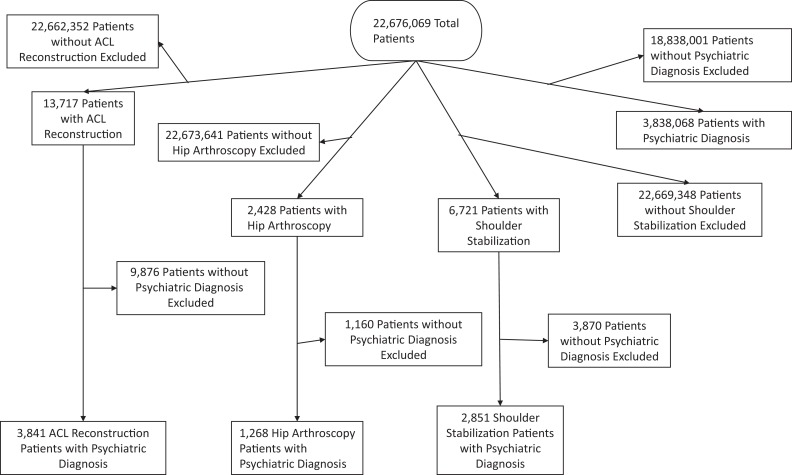
The search query comprised all patients with a record of a psychiatric diagnosis denoted by an International Classification of Diseases, 9th Revision (ICD-9) and 10th Revision (ICD-10) code. Within the ICD-9 and ICD-10, all psychological and psychiatric diagnoses are listed sequentially and include ICD-9 codes from 290.0 (senile dementia, uncomplicated) to 319 (unspecified mental retardation) and ICD-10 codes between F01 (vascular dementia) and F99 (mental disorder, not otherwise specified). The first appearance of these ICD-9 and ICD-10 codes within each patient in the data set (if present) was recorded. Next, the number of patients having a record of Current Procedural Terminology (CPT) codes denoting arthroscopic procedures of the hip (Table 1) was recorded. The database was then queried to denote any patients who had undergone hip arthroscopic surgery and had a record of any psychiatric diagnosis occurring before hip arthroscopic surgery or within 2 years postoperatively. Prevalence rates for psychiatric diagnoses were then noted for the entire database and for patients who had undergone hip arthroscopic surgery (Figure 1). Data were stratified by age and sex as well as by the most common psychiatric diagnoses.
TABLE 1.
CPT Codes Used to Denote Patients Undergoing Hip Arthroscopic Surgerya
| 29860 | Arthroscopy, hip, diagnostic with or without synovial biopsy |
| 29861 | Arthroscopy, hip, surgical; with removal of loose body or foreign body |
| 29862 | Arthroscopy, hip, surgical; with removal of loose body or foreign body with debridement/shaving of articular cartilage (chondroplasty), abrasion arthroplasty, and/or resection of labrum |
| 29863 | Arthroscopy, hip, surgical; with removal of loose body or foreign body with synovectomy |
| 29914 | Arthroscopy, hip, surgical; with removal of loose body or foreign body with femoroplasty (ie, treatment of cam lesion) |
| 29915 | Arthroscopy, hip, surgical; with removal of loose body or foreign body with acetabuloplasty (ie, treatment of pincer lesion) |
| 29916 | Arthroscopy, hip, surgical; with removal of loose body or foreign body with labral repair |
aCPT, Current Procedural Terminology.
Figure 1.
Flowchart detailing how patients of interest were isolated from the general population. ACL, anterior cruciate ligament.
As a further control group and to investigate whether undergoing any surgical procedure (not just hip arthroscopic surgery) increased the prevalene of a psychiatric diagnosis, the prevalence of psychiatric comorbid conditions in those undergoing ACL reconstruction (CPT 29888) and those undergoing shoulder stabilization surgery (Appendix Table A1) were also examined. Similar to the hip arthroscopic surgery group, the database was searched for the presence of ICD-9 codes from 290.0 to 319 and ICD-10 codes between F01 and F99 either before or within 2 years after ACL reconstruction.
Age prevalence is presented as the median and mode (patient-level data not available), while sex and disease prevalence are provided as raw values. Prevalence was calculated as the number of patients with psychiatric diagnoses and undergoing the related procedure divided by the number of patients available in the database or who underwent the surgical procedure. Additional analysis excluding patients who had a diagnosis of a “tobacco use disorder” was performed. Comparisons between prevalence rates were made with the chi-square test using the Yates correction, with an alpha value of .05 set as significant.
Results
Among the 22,676,069 patients within the database (median age, 55-59 years; 56.2% female) (Appendix Table A2), 2428 patients underwent hip arthroscopic surgery, with 1268 (52%) of these patients (median age, 45-49 years; 404 male, 864 female) having a psychiatric or psychological diagnosis within the defined period (Figure 1 and Table 2). Female patients made up 68% of the patient population that had undergone hip arthroscopic surgery and had concomitant psychiatric diagnoses. Depression and anxiety were the most common concomitant psychiatric diagnoses within the hip arthroscopic surgery group (Table 2). Patients undergoing hip arthroscopic surgery displayed a 3-fold higher prevalence of psychiatric diagnoses compared with the general population, with a significantly higher prevalence of psychiatric diagnoses in female versus male patients (Table 3).
TABLE 2.
Top 20 ICD-9 Psychiatric Diagnoses of Patients Undergoing Hip Arthroscopic Surgerya
| Code | Diagnosis | n (%) | |
|---|---|---|---|
| 1 | 311 | Depressive disorder, not elsewhere classified | 240 (18.93) |
| 2 | 300.00 | Anxiety state, unspecified | 206 (16.25) |
| 3 | 305.1 | Tobacco use disorder | 171 (13.49) |
| 4 | 300.02 | Generalized anxiety disorder | 47 (3.71) |
| 5 | 300.4 | Dysthymic disorder | 47 (3.71) |
| 6 | 314.00 | Attention deficit disorder without mention of hyperactivity | 44 (3.47) |
| 7 | 307.81 | Tension headache | 25 (1.97) |
| 8 | 296.32 | Major depressive affective disorder, recurrent episode, moderate | 23 (1.81) |
| 9 | 309.28 | Adjustment disorder with mixed anxiety and depressed mood | 22 (1.74) |
| 10 | 314.01 | Attention deficit disorder with hyperactivity | 21 (1.66) |
| 11 | 309.0 | Adjustment disorder with depressed mood | 16 (1.26) |
| 12 | 296.20 | Major depressive affective disorder, single episode, unspecified | 15 (1.18) |
| 13 | 296.33 | Major depressive affective disorder, recurrent episode, severe, without mention of psychotic behavior | 14 (1.10) |
| 14 | 307.42 | Persistent disorder of initiating or maintaining sleep | 13 (1.03) |
| 15 | 309.24 | Adjustment disorder with anxiety | 13 (1.03) |
| 16 | 300.01 | Panic disorder without agoraphobia | 12 (0.95) |
| 17 | 310.2 | Postconcussion syndrome | 12 (0.95) |
| 18 | 296.80 | Bipolar disorder, unspecified | 11 (0.87) |
| 19 | 290.21 | Senile dementia with depressive features | <11 (<0.87) |
| 20 | 292.81 | Drug-induced delirium | <11 (<0.87) |
aICD-9, International Classification of Diseases, 9th Revision.
TABLE 3.
Prevalence of Psychiatric Diagnoses in the General Population Versus Patients Undergoing Hip Arthroscopic Surgery
| General Population, % | Hip Arthroscopic Surgery, % | Difference | P Value | |
|---|---|---|---|---|
| All patients | 17 | 52 | 3.06 times | <.0001 |
| Male | 16 | 46 | 2.88 times | — |
| Female | 18 | 56 | 3.11 times | .0061 (vs male) |
Comparatively, 13,717 patients underwent ACL reconstruction, with 3841 (28%) having a psychiatric or psychological diagnosis (median age, 30-34 years; 2002 male, 1839 female) within the defined period (Figure 1 and Appendix Table A3). Among those undergoing ACL reconstruction, there was a 65% increased prevalence of concomitant psychiatric diagnoses versus the general population (Table 4), and there was also significantly less prevalence when compared with those undergoing hip arthroscopic surgery (P < .0001). Regarding shoulder stabilization surgery, 6721 patients underwent this procedure, with 2851 (42%) patients having concomitant psychiatric diagnoses (median age, 35-59 years; 1738 male, 1113 female) (Table 5 and Appendix Table A4). The overall prevalence of psychiatric and psychological diagnoses within the shoulder stabilization group was significantly higher than that in the general population, and again, female patients demonstrated a higher prevalence than male patients. However, the rate of concomitant psychiatric or psychological diagnoses remained significantly below that in the hip arthroscopic surgery group (P < .0001) (Table 5).
TABLE 4.
Prevalence of Psychiatric Diagnoses in the General Population Versus Patients Undergoing ACL Reconstructiona
| General Population, % | ACL Reconstruction, % | Difference | P Value | |
|---|---|---|---|---|
| All patients | 17 | 28 | 1.65 times | <.0001 and <.0001 (vs hips) |
| Male | 16 | 25 | 1.56 times | — |
| Female | 18 | 32 | 1.78 times | <.0001 (vs male) |
aACL, anterior cruciate ligament.
TABLE 5.
Prevalence of Psychiatric Diagnoses in the General Population Versus Patients Undergoing Shoulder Stabilization Surgery
| General Population, % | Shoulder Stabilization, % | Difference | P Value | |
|---|---|---|---|---|
| All patients | 17 | 42 | 2.47 times | <.0001 and <.0001 (vs hips) |
| Male | 16 | 37 | 2.31 times | — |
| Female | 18 | 54 | 3.00 times | <.0001 (vs male) |
A separate analysis was performed to exclude patients with a “tobacco use disorder” from inclusion in the cohort with a psychological/psychiatric diagnosis (Table 6). When comparing all groups, and excluding this disorder from the analysis, the hip arthroscopic surgery group was still found to have a 3.5 times increased prevalence of concomitant psychiatric or psychological diagnoses, which was significantly greater than both the ACL reconstruction and shoulder stabilization groups (Table 6).
TABLE 6.
Prevalence of Psychiatric Diagnoses in the General Population Versus Patients Undergoing Surgery, With Those With a “Tobacco Use Disorder” Excluded
| General Population, % | Surgical Population, % | Difference | P Value | |
|---|---|---|---|---|
| Hip arthroscopic surgery | 14 | 49 | 3.50 times | — |
| Anterior cruciate ligament reconstruction | 14 | 25 | 1.78 times | <.0001 (vs hips) |
| Shoulder stabilization | 14 | 38 | 2.70 times | <.0001 (vs hips) |
Discussion
This investigation reports a significantly higher prevalence of concomitant psychiatric diagnoses in patients undergoing hip arthroscopic surgery compared with the general population and compared with those undergoing ACL reconstruction or shoulder stabilization surgery. These findings support our hypothesis that patients undergoing hip arthroscopic surgery have an increased prevalence of concomitant psychiatric diagnoses.
Those with musculoskeletal pain, potentially from athletic activities, are not immune from mental health disorders and psychological distress. Gouttebarge et al3 investigated the prevalence of mental health disorders in elite athletes. In a prospective cohort study of Dutch athletes with a 12-month follow-up period, the authors noted that up to 57% of athletes included in their investigation experienced mental health disorders. By increasing awareness that athletes are also susceptible to psychiatric disorders, preventive mental health measures for athletes have become more available.3 Other studies have demonstrated that athletic populations actually face higher rates of psychiatric diagnoses, especially when considering issues related to performance anxiety and coping mechanisms, such as drinking behaviors.10,16 Wolanin et al16 examined research related to mental health in athletic populations and found that in cases of sports-related injuries and decreased athletic performance, rates of psychiatric disorders increased. Mastroleo et al10 investigated a potential correlation between athletes’ personality and engagement in heavy drinking behaviors. Using a mixed study population of collegiate athletes and nonathletes, the researchers concluded that athletes were more likely to engage in risky drinking behaviors and may be at a higher risk for experiencing alcohol-related issues.10
Mental health status and psychological distress have been shown to have a close relationship with postoperative outcomes after orthopaedic surgery. Petrie et al12 reported that total hip arthroplasty can significantly improve psychological well-being. Using preoperative, immediate postoperative, and 2-month postoperative questionnaires of 51 patients undergoing hip arthroplasty, the authors found that pain reduction from surgery helped to decrease psychological distress.12 However, Lavernia et al8 found that mentally distressed patients undergoing total hip and total knee arthroplasty had worse preoperative and postoperative outcome scores. In their retrospective study of 563 patients, patients with inferior preoperative 36-Item Short Form Health Survey (SF-36) Mental Component Summary scores reported inferior outcomes after surgery.8 Similarly, patients undergoing rotator cuff repair who have increased psychological distress preoperatively experience inferior postoperative outcomes. In a prospective study of 85 patients with full-thickness rotator cuff tears, Potter et al14 found that patients with higher mental distress reported worse shoulder pain. It was also noted that these patients reported worse outcomes on the Simple Shoulder Test and the American Shoulder and Elbow Surgeons score. Furthermore, in a prospective study of 196 patients with full-thickness rotator cuff tears, Wylie et al17 found that tear size, measured by magnetic resonance imaging, did not correlate with worse functional scores. Instead, they reported that inferior SF-36 scores had the strongest associations with pain level and shoulder function.17
Mental health issues have also been shown to negatively correlate with pain and function, specifically in patients undergoing hip arthroscopic surgery. Potter et al13 sought to determine if patients with higher levels of preoperative psychological distress were more likely to request a postoperative block and if this form of pain control was more effective for postoperative pain control than multimodal and intravenous analgesia. Using preoperative Distress and Risk Assessment Method questionnaires and postoperative visual analog scale pain scores, these authors determined that patients with higher levels of preoperative psychological distress had higher postoperative visual analog scale scores and were more likely to request a nerve block. Jacobs et al5 examined 64 patients with FAI undergoing surgery and reported that an increased severity of FAI symptoms was more closely correlated with mental health distress than the severity of their physical injury and anatomic findings during arthroscopic surgery. The severity of injury was determined by the size of the labral tear, the presence of chondral deformities, the magnitude of the FAI deformity, and preoperative subjective outcomes.5
Although we found that patients undergoing hip arthroscopic surgery had a significantly increased prevalence of concomitant psychiatric diagnoses, we were concerned that this effect may simply be caused by the surgical procedure itself, that is, that those choosing to undergo an elective procedure, or any surgical procedure in general, are more likely to have psychiatric comorbidities. We therefore examined the prevalence of psychiatric diagnoses for those undergoing ACL reconstruction as well as for those undergoing shoulder stabilization surgery. These procedures were chosen because they represent elective procedures, similar to nearly all hip arthroscopic procedures, performed in a similar population. The current finding of significantly increased psychiatric diagnoses in patients undergoing hip arthroscopic surgery as compared with both the general population and these surgical populations confirms that the increased prevalence is not simply caused by the presence of the surgical procedure itself.
One of the possible reasons for the increased prevalence of psychiatric diagnoses in the hip arthroscopic surgery population may relate to the close interplay between hip and back pain15 and the subsequent relationship between back pain and psychiatric comorbid conditions.2,7,18 Although some patients will undergo a diagnostic hip intra-articular injection before hip arthroscopic surgery for pain relief, this cannot definitively rule out operative procedures on some patients with at least some perceived hip symptoms originating from back abnormalities. Given the relationship between back pain and psychological comorbidities, this may lead to an increased prevalence of psychiatric conditions in the hip arthroscopic surgery population. The increased prevalence of psychiatric conditions in the ACL reconstruction and shoulder stabilization groups as compared with the general population may relate to the higher rate of participation in demanding sporting activities and subsequent baseline personality characteristics of athletes.10,16
This study has several limitations. As with all investigations using claims data, our results are dependent on the accuracy of the coding contained within the database. Furthermore, because of HIPAA reporting requirements, individual patient-level data are not available in the database, making more granular comparisons in which small patient numbers exist impossible. The database utilized in this investigation, however, is a well-known and vetted database and has been used in a number of peer-reviewed studies.1,10,14 The exclusion of Medicare patients also limited our available claims data pool available for analysis. However, the Medicare patient population is older in age, more likely to have comorbid medical conditions, not representative of the typical patient undergoing hip arthroscopic surgery.11 Despite this, the average patient age may have been older than the typical patient included in prospective studies. Because of the limitations of working with claims data, however, we are able to only report the median age (vs mean).
The hip arthroscopic surgery group also had a higher percentage of female patients versus the ACL reconstruction and shoulder stabilization groups, potentially biasing our results. Furthermore, our results may be confounded by the possibility that patients with psychiatric diagnoses are more likely to undergo surgery in general and not specifically hip arthroscopic surgery. This possibility is mitigated, however, with the inclusion of other surgical groups (ACL reconstruction and shoulder stabilization) for comparison. The significantly decreased prevalence of psychiatric disease in those undergoing ACL reconstruction as well as shoulder stabilization surgery supports the findings of this study.
In addition, it may be that hip abnormalities captured in the hip arthroscopic surgery group are intrinisically different than those in the ACL reconstruction and shoulder stabilization groups. Patients undergoing hip arthroscopic surgery typically present with pain, while those undergoing ACL reconstruction and shoulder stabilization surgery report instability symptoms. Some of our findings may be the result of hip patients experiencing more pain, which in turn may lead to an increased risk of psychiatric conditions. Last, the diagnosis of a “tobacco use disorder” as a psychiatric diagnosis was initially included, and this may have artificially elevated our prevalence rate. Even after this disorder was excluded from all groups, however, the prevalence of concomitant psychiatric diagnoses in the hip arthroscopic surgery group remained significantly higher than all other groups.
Conclusion
Patients undergoing hip arthroscopic surgery had an increased prevalence of psychiatric diagnoses compared with the general population as well as the control groups of patients undergoing ACL reconstruction or undergoing shoulder stabilization surgery. This finding should be considered in surgical indications for hip arthroscopic surgery and when caring for patients with FAI to properly counsel patients regarding surgical outcomes.
Appendix
TABLE A1.
CPT Codes Used to Denote Patients Undergoing Shoulder Stabilization Surgerya
| Code | |
|---|---|
| 23450 | Capsulorrhaphy, anterior; Putti-Platt procedure or Magnuson type operation |
| 23455 | Capsulorrhaphy, anterior; Putti-Platt procedure or Magnuson type operation with labral repair |
| 23460 | Capsulorrhaphy, anterior, any type; with bone block |
| 23462 | Capsulorrhaphy, anterior, any type; with bone block with coracoid process transfer |
| 23465 | Capsulorrhaphy, glenohumeral joint, posterior, with or without bone block |
| 23466 | Capsulorrhaphy, glenohumeral joint, any type multidirectional instability |
| 29806 | Arthroscopy, shoulder, surgical; capsulorrhaphy |
aCPT, Current Procedural Terminology.
TABLE A2.
Top 20 ICD-9 Psychiatric Diagnoses of the General Populationa
| Code | Diagnosis | n (%) | |
|---|---|---|---|
| 1 | 305.1 | Tobacco use disorder | 667,755 (17.40) |
| 2 | 311 | Depressive disorder, not elsewhere classified | 615,942 (16.05) |
| 3 | 300.00 | Anxiety state, unspecified | 574,550 (14.97) |
| 4 | 300.02 | Generalized anxiety disorder | 120,146 (3.13) |
| 5 | 300.4 | Dysthymic disorder | 116,484 (3.03) |
| 6 | 294.8 | Other persistent mental disorders due to conditions classified elsewhere | 73,822 (1.92) |
| 7 | 296.20 | Major depressive affective disorder, single episode, unspecified | 69,070 (1.80) |
| 8 | 298.9 | Unspecified psychosis | 67,789 (1.77) |
| 9 | 294.20 | Dementia, unspecified, without behavioral disturbance | 53,095 (1.38) |
| 10 | 302.72 | Psychosexual dysfunction with inhibited sexual excitement | 46,430 (1.21) |
| 11 | 307.81 | Tension headache | 44,399 (1.16) |
| 12 | 309.28 | Adjustment disorder with mixed anxiety and depressed mood | 41,663 (1.09) |
| 13 | 314.00 | Attention deficit disorder without mention of hyperactivity | 41,538 (1.08) |
| 14 | 314.01 | Attention deficit disorder with hyperactivity | 37,275 (0.97) |
| 15 | 309.0 | Adjustment disorder with depressed mood | 35,919 (0.94) |
| 16 | 305.00 | Alcohol abuse, unspecified | 35,444 (0.92) |
| 17 | 296.30 | Major depressive affective disorder, recurrent episode, unspecified | 35,200 (0.92) |
| 18 | 296.32 | Major depressive affective disorder, recurrent episode, moderate | 32,945 (0.86) |
| 19 | 294.10 | Dementia in conditions classified elsewhere without behavioral disturbance | 31,408 (0.82) |
| 20 | 296.80 | Bipolar disorder, unspecified | 26,582 (0.69) |
aICD-9, International Classification of Diseases, 9th Revision.
TABLE A3.
Top 20 ICD-9 Psychiatric Diagnoses of Patients Undergoing ACL Reconstructiona
| Code | Diagnosis | n (%) | |
|---|---|---|---|
| 1 | 300.00 | Anxiety state, unspecified | 565 (14.71) |
| 2 | 305.1 | Tobacco use disorder | 525 (13.67) |
| 3 | 311 | Depressive disorder, not elsewhere classified | 366 (9.53) |
| 4 | 314.00 | Attention deficit disorder without mention of hyperactivity | 262 (6.82) |
| 5 | 314.01 | Attention deficit disorder with hyperactivity | 170 (4.43) |
| 6 | 309.28 | Adjustment disorder with mixed anxiety and depressed mood | 138 (3.59) |
| 7 | 300.02 | Generalized anxiety disorder | 135 (3.51) |
| 8 | 300.4 | Dysthymic disorder | 94 (2.45) |
| 9 | 305.00 | Alcohol abuse, unspecified | 86 (2.24) |
| 10 | 307.81 | Tension headache | 84 (2.19) |
| 11 | 309.0 | Adjustment disorder with depressed mood | 60 (1.56) |
| 12 | 300.01 | Panic disorder without agoraphobia | 58 (1.51) |
| 13 | 309.9 | Unspecified adjustment reaction | 56 (1.46) |
| 14 | 296.20 | Major depressive affective disorder, single episode, unspecified | 46 (1.20) |
| 15 | 309.24 | Adjustment disorder with anxiety | 41 (1.07) |
| 16 | 310.2 | Postconcussion syndrome | 36 (0.94) |
| 17 | 296.30 | Major depressive affective disorder, recurrent episode, unspecified | 33 (0.86) |
| 18 | 296.80 | Bipolar disorder, unspecified | 32 (0.83) |
| 19 | 296.32 | Major depressive affective disorder, recurrent episode, moderate | 29 (0.76) |
| 20 | 296.90 | Unspecified episodic mood disorder | 29 (0.76) |
aACL, anterior cruciate ligament; ICD-9, International Classification of Diseases, 9th Revision.
TABLE A4.
Top 20 ICD-9 Psychiatric Diagnoses of Patients Undergoing Shoulder Stabilization Surgerya
| Code | Diagnosis | n (%) | |
|---|---|---|---|
| 1 | 305.1 | Tobacco use disorder | 430 (15.08) |
| 2 | 311 | Depressive disorder, not elsewhere classified | 411 (14.42) |
| 3 | 300.00 | Anxiety state, unspecified | 389 (13.64) |
| 4 | 314.00 | Attention deficit disorder without mention of hyperactivity | 140 (4.91) |
| 5 | 300.02 | Generalized anxiety disorder | 98 (3.44) |
| 6 | 300.4 | Dysthymic disorder | 98 (3.44) |
| 7 | 314.01 | Attention deficit disorder with hyperactivity | 97 (3.40) |
| 8 | 309.28 | Adjustment disorder with mixed anxiety and depressed mood | 74 (2.60) |
| 9 | 305.00 | Alcohol abuse, unspecified | 52 (1.82) |
| 10 | 307.81 | Tension headache | 51 (1.79) |
| 11 | 310.2 | Postconcussion syndrome | 42 (1.47) |
| 12 | 296.32 | Major depressive affective disorder, recurrent episode, moderate | 41 (1.44) |
| 13 | 296.80 | Bipolar disorder, unspecified | 40 (1.40) |
| 14 | 300.01 | Panic disorder without agoraphobia | 36 (1.26) |
| 15 | 296.20 | Major depressive affective disorder, single episode, unspecified | 35 (1.23) |
| 16 | 302.72 | Psychosexual dysfunction with inhibited sexual excitement | 34 (1.19) |
| 17 | 309.0 | Adjustment disorder with depressed mood | 31 (1.09) |
| 18 | 309.9 | Unspecified adjustment reaction | 31 (1.09) |
| 19 | 296.90 | Unspecified episodic mood disorder | 23 (0.81) |
| 20 | 296.30 | Major depressive affective disorder, recurrent episode, unspecified | 20 (0.70) |
aICD-9, International Classification of Diseases, 9th Revision.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: M.R.S. has received consulting fees from Biomet, Ferring Pharmaceuticals, Linvatec, Medacta, and Smith & Nephew. G.D.A. has received educational support from Pacific Medical. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Cho CH, Song KS, Hwang I, Warner JJ. Does rotator cuff repair improve psychologic status and quality of life in patients with rotator cuff tear? Clin Orthop Relat Res. 2015;473(11):3494–3500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ciaramella A, Poli P. Chronic low back pain: perception and coping with pain in the presence of psychiatric comorbidity. J Nerv Ment Dis. 2015;203(8):632–640. [DOI] [PubMed] [Google Scholar]
- 3. Gouttebarge V, Jonkers R, Moen M, Verhagen E, Wylleman P, Kerkhoffs G. A prospective cohort study on symptoms of common mental disorders among Dutch elite athletes. Phys Sportsmed. 2017;45(4):426–432. [DOI] [PubMed] [Google Scholar]
- 4. Griffiths EJ, Khanduja V. Hip arthroscopy: evolution, current practice and future developments. Int Orthop. 2012;36(6):1115–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jacobs CA, Burnham JM, Jochimsen KN, Molina D, 4th, Hamilton DA, Duncan ST. Preoperative symptoms in femoroacetabular impingement patients are more related to mental health scores than the severity of labral tear or magnitude of bony deformity. J Arthroplasty. 2017;32(12):3603–3606. [DOI] [PubMed] [Google Scholar]
- 6. Jamil M, Dandachli W, Noordin S, Witt J. Hip arthroscopy: indications, outcomes and complications. Int J Surg. 2018;54(pt B):341–344. [DOI] [PubMed] [Google Scholar]
- 7. Konnopka A, Lobner M, Luppa M, et al. Psychiatric comorbidity as predictor of costs in back pain patients undergoing disc surgery: a longitudinal observational study. BMC Musculoskelet Disord. 2012;13:165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lavernia CJ, Alcerro JC, Brooks LG, Rossi MD. Mental health and outcomes in primary total joint arthroplasty. J Arthroplasty. 2012;27(7):1276–1282. [DOI] [PubMed] [Google Scholar]
- 9. Magrill ACL, Nakano N, Khanduja V. Historical review of arthroscopic surgery of the hip. Int Orthop. 2017;41(10):1983–1994. [DOI] [PubMed] [Google Scholar]
- 10. Mastroleo NR, Scaglione N, Mallett KA, Turrisi R. Can personality account for differences in drinking between college athletes and non-athletes? Explaining the role of sensation seeking, risk-taking, and impulsivity. J Drug Educ. 2013;43(1):81–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Parker JL, Regan JF, Petroski J. Beneficiary activation in the Medicare population. Medicare & Medicaid Research Review. 2014;4(4):e1–e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Petrie K, Chamberlain K, Azariah R. The psychological impact of hip arthroplasty. Aust N Z J Surg. 1994;64(2):115–117. [DOI] [PubMed] [Google Scholar]
- 13. Potter MQ, Sun GS, Fraser JA, et al. Psychological distress in hip arthroscopy patients affects postoperative pain control. Arthroscopy. 2014;30(2):195–201. [DOI] [PubMed] [Google Scholar]
- 14. Potter MQ, Wylie JD, Greis PE, Burks RT, Tashjian RZ. Psychological distress negatively affects self-assessment of shoulder function in patients with rotator cuff tears. Clin Orthop Relat Res. 2014;472(12):3926–3932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Redmond JM, Gupta A, Hammarstedt JE, Stake CE, Domb BG. The hip-spine syndrome: how does back pain impact the indications and outcomes of hip arthroscopy? Arthroscopy. 2014;30(7):872–881. [DOI] [PubMed] [Google Scholar]
- 16. Wolanin A, Gross M, Hong E. Depression in athletes: prevalence and risk factors. Curr Sports Med Rep. 2015;14(1):56–60. [DOI] [PubMed] [Google Scholar]
- 17. Wylie JD, Suter T, Potter MQ, Granger EK, Tashjian RZ. Mental health has a stronger association with patient-reported shoulder pain and function than tear size in patients with full-thickness rotator cuff tears. J Bone Joint Surg Am. 2016;98(4):251–256. [DOI] [PubMed] [Google Scholar]
- 18. Yoshida K, Sekiguchi M, Otani K, et al. Computational psychological study of the Brief Scale for Psychiatric Problems in Orthopaedic Patients (BS-POP) for patients with chronic low back pain: verification of responsiveness. J Orthop Sci. 2015;20(3):469–474. [DOI] [PubMed] [Google Scholar]