Abstract
Caregivers of technology-dependent children face considerable responsibilities. This study examined the association of 2 child-related stressors—functional status and use of mechanical ventilator—with 2 domains of family caregiver well-being—depressive symptoms (Center for Epidemiologic Studies Depression Scale [CES-D]) and health-related quality of life (HRQOL) and family function (PedsQL Family Impact Module). The secondary objective was to determine whether these associations were moderated by caregiver-perceived social support. Structured interviews were conducted with 88 primary family caregivers of technology-dependent children in Singapore. Hierarchical multiple regression was used to assess the primary and secondary objectives. A total of 44.3% of caregivers were at high risk of clinical depression. Moderately poor child functional status was associated with more caregiver depressive symptoms. Perceived social support moderated this association. Family caregivers of technology-dependent children have high levels of depressive symptoms and relatively poor HRQOL and family functioning. Enhancing caregivers’ social support is important for their well-being.
Keywords: pediatric, home care, caregiver health
Introduction
Medical advances have resulted in improvements in the survival of children with life-threatening conditions, such as preterm birth, congenital abnormalities, and chronic diseases, leading to a growing number of children who are technology-dependent.1,2 A technology-dependent child is one who needs both a medical device to compensate for the loss of a vital body function and substantial and ongoing nursing care to avert further disability or even death.3 As a result, pediatric home care has become a significant and necessary component of health care.4 Caregivers, often the parents,5 play a central role in provision of home health care. However, the process of caregiving can be daunting,6 and caregivers experience a significant impact on their psychological well-being.7,8 Fatigue, poor physical health, and social isolation are also common.9
Singapore is a cosmopolitan, developed country in Southeast Asia, with a population of 5.54 million and about 600 000 under the age of 15 years.10 Like many developed and developing countries,1,2,11,12 Singapore has an increasing population of children with medical complexity who require medical technology at home. KK Women’s and Children’s Hospital (KKH) is the largest tertiary pediatric hospital in Singapore with about 28 000 acute pediatric admissions annually. The lack of community hospital and home nursing program for children prompted the start of the KKH Pediatric Home Care program in 2001. The model centers on training to caregivers delivered by 4 KKH nurses with 4 follow-up home visits per year for ventilated children and up to 3 visits annually for non-ventilated patients (eg, tracheostomy only, enteral feeding tubes). Much of the caregiving is provided by the parents, grandparents, or employed foreign domestic workers (FDWs). The lack of universal home health care funding also poses a challenge for the families. From inception till January 2016, the program has enrolled more than 1560 technology-dependent children, approximately 90% of whom had left the program over the years due to improvement in clinical status, transfer to another medical center, or demise.
Much of the current literature on child caregiver health and burden are exploratory and descriptive in nature, and centered on disease-specific conditions. Medical conditions that lead to the need for technology support at home are heterogeneous, and caregiving requires huge commitment of time and resources by the caregivers. Caregivers of children with perinatal stroke, chronic disabilities, and reliance on medical technology are at risk of depression,8,13 and the severity of the child’s condition affect family function.14 Adult and pediatric studies have both reported high prevalence of caregiver depression in caring for patients with long-term mechanical ventilation at home.7,15,16 However, caregiver social support has been found to be a moderator or directly associated with caregiver depression and family function.17,18 A study of caregivers of adults in a single center also suggested that perceived social support may be more important than actual enacted support.19
In examining the factors that influence child caregiver well-being, our conceptual framework (Figure 1) was built on the moderating stress buffering model.20 The study primarily examined the association of 2 child-related stressors—(1) functional status and (2) use of mechanical ventilator—with 2 domains of family caregiver well-being—(1) depressive symptoms (measured by Center for Epidemiologic Studies Depression Scale [CES-D] score) and (2) health-related quality of life (HRQOL) and family function (measured by PedsQL Family Impact Module total summary score). We hypothesized that poorer child functional status and the child’s need for mechanical ventilation at home are associated with greater caregiver depressive symptoms and lower caregiver HRQOL and family functioning. The secondary objective was to determine if these associations are moderated by caregiver-perceived social support with the hypothesis that perceived social support moderates or buffers the effects of child-related stressors on caregiver well-being.
Figure 1.
Conceptual model.
aAge, gender, ethnicity, religion, marital status, educational status, relationship to child, housing type, monthly household income, perceived financial adequacy, and household size.
bAge, gender, and ethnicity.
Methods
Study Design and Participants
This was a cross-sectional study including primary caregivers who were (1) aged 21 years or older; (2) caring for a child aged 18 years or younger, lived at home in Singapore, and required one or more medical technology daily; and (3) able to speak and understand English or Standard Chinese. Primary caregiver was defined as a family member who was directly involved in the caregiving of the child and who made important financial and clinical decisions pertaining to the care of the child. Of 180 caregivers in the home care database who were found to be eligible, 65 (36.1%) refused participation and 27 (15%) could not schedule a time for interview, leaving 88 (48.9%) primary family caregivers of technology-dependent children for inclusion into the study. Participant recruitment and interviews were carried out between March 2015 and January 2016.
Ethical Approval and Informed Consent
The study was approved by the SingHealth Centralised Institutional Review Board (CIRB Ref: 2014/2000). Written informed consent was obtained from the participants prior to the interviews.
Data Collection and Instruments
Interviews, lasting 30 to 90 minutes, were conducted with the caregivers at a location of their choice (home, workplace, or hospital), using a structured questionnaire. Interviews were conducted mostly in English (n = 78, 88.6%). The English and Chinese versions of the questionnaires had been pilot tested on a few caregivers who were not part of the study sample. The Chinese version was developed in accordance with the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) translation guidelines.21
Child-Related Stressors (Predictors)
Functional Status
The Pediatrics Functional Status Score (FSS) was administered to the caregiver.22 The FSS has 6 domains (mental status, sensory function, communication, motor function, feeding, and respiratory status), each scored from normal (1) to very severe dysfunction (5). A higher total FSS (range = 6-30) indicates poorer functional status. The FSS has been reported to have good interrater reliability and high reproducibility in a study with a subpopulation of technology-dependent children.22
Use of Mechanical Ventilator
Type of medical technology (mechanical ventilation, tracheostomy, oxygen therapy, oropharyngeal suctioning, enteral feeding [nasogastric, nasojejunal, or gastrojejunal], and urinary catheterization) that the child required daily was assessed from the caregiver. Children were classified into 2 groups (Yes vs No) based on mechanical ventilator status.
Caregiver Well-Being (Outcomes)
Depressive Symptoms
The 20-item CES-D was used.23 It appraises the frequency of depressive symptoms over the past week (rarely or none of the time [0] to most or all of the time [3]). A higher total score (range = 0-60) indicates more depressive symptoms; scoring 16 or greater indicates high risk for clinical depression.23 The CES-D has demonstrated good internal consistency in adults with diabetes mellitus in multiethnic Singapore.24
HRQOL and Family Functioning
The 36-item PedsQL Family Impact Module,25 which measures the impact of pediatric chronic health conditions on parents and family, was utilized. Items are scored from never a problem (0) to always a problem (4), then reverse-coded and transformed to a 0 to 100 composite scale HRQOL and family function (PedsQL Total Summary Score [PedsQLTSS]); higher scores indicate better HRQOL and family functioning. The total summary score (PedsQLTSS) has reported good internal consistency reliability of 0.97 in families with children with chronic complex medical conditions.25
Social Support (Moderators)
Caregiver-Perceived Social Support
The modified 8-item Medical Outcomes Study: Social Support Survey Instrument (mMOS-SSS) was used.26 An overall score, based on individual item scores (none of the time [1] to all of the time [5]), is calculated and transformed to a 0 to 100 scale. Higher scores indicate greater social support. The mMOS-SSS has a reported internal consistency reliability of 0.88 to 0.93, with excellent psychometric properties similar to the original 19-item instrument.26
Sociodemographics
Information on caregiver’s age, gender, ethnicity, religion, marital status, employment, education, monthly household income, housing type and household size, and the child’s age, gender, and ethnicity was collected, as was the average weekly hours of caregiving help received from others (including FDWs, visiting nurses, family members, and relatives). While the CES-D, PedsQL Family Impact Module, and mMOS-SSS were self-administered, the rest of the questionnaire was interviewer-administered.
Data Analysis
Descriptive data on caregiving situation and caregiver condition were summarized as mean and standard deviation, median and range, or frequency and percentage, as applicable. For each of the 2 caregiver outcomes, CES-D and PedsQLTSS, separate 3-stage hierarchical regression models were estimated. To facilitate interpretation, continuous independent variables were standardized. For dichotomous variables, effects coding was applied. In the first stage, both child stressors, namely, child FSS and use of mechanical ventilation (Vent), were entered. In the second stage, the moderator, mMOS-SSS, was entered; and in the third stage, 2 interaction terms representing the interaction between the child stressors and the moderator were entered (FSS × mMOS-SSS and Vent × mMOS-SSS). Recognizing differences in caregiver or child sociodemographic and instrumental support attributes, a stepwise regression procedure was performed to select at most 3 characteristics (in keeping with the parsimony principle in modelling) to adjust for. The characteristics selected by stepwise regression, caregiver perception of financial adequacy (adequate/nonadequate), religion (Islam/non-Islam), and secondary education (Yes/No), were entered in the first stage along with the child stressor variables. Assumptions of normality, linearity, and homoscedasticity were verified using residual plots, including presence of outliers. A 10% significance level was used in tests of hypotheses. All analyses were performed using IBM Statistics version 21.0.
Results
The characteristics of the family caregivers and children are presented in Table 1. The mean age of caregivers was 39.9 years, and most were female (90.9%), mothers of the child (87.5%), of Chinese ethnicity (72.7%), Singapore citizens (85.2%), and married (92.0%). The median household monthly income was S$4500, less than the national median income of S$8500.27 About half (53.4%) the technology-dependent children were male, with mean age of 7.1 (SD = 5.3) years.
Table 1.
Sociodemographic Characteristics of Primary Informal Caregivers and Care Recipients.
| Primary Informal Caregivers (N = 88) | n | % |
|---|---|---|
| Gender | ||
| Male | 8 | 9 |
| Female | 80 | 91 |
| Age (in years)a, mean ± SD | 39.9 ± 7.5 | |
| Relationship to child | ||
| Father | 7 | 8 |
| Mother | 77 | 88 |
| Grandmother | 3 | 3 |
| Uncle | 1 | 1 |
| Race | ||
| Chinese | 64 | 73 |
| Malay | 16 | 18 |
| Indian | 5 | 6 |
| Others | 3 | 3 |
| Nationality | ||
| Singapore citizen | 75 | 85 |
| Singapore PR | 11 | 13 |
| Others | 2 | 2 |
| Religion | ||
| Christianity | 25 | 29 |
| Buddhism/Taoism | 31 | 35 |
| Islam | 22 | 25 |
| Hinduism | 2 | 2 |
| No religion | 8 | 9 |
| Marital status | ||
| Married | 81 | 92 |
| Not married/divorced/separated | 7 | 8 |
| Level of education | ||
| Primary/secondary school | 30 | 34 |
| Postsecondary/polytechnic diploma | 29 | 33 |
| University/postgraduate degree | 29 | 33 |
| Total monthly household income | ||
| <S$1999 | 19 | 22 |
| S$2000-4999 | 30 | 34 |
| ≥S$5000 | 36 | 41 |
| Do not know/refuse to answer | 3 | 3 |
| Care Recipients (N = 88) | n | % |
| Gender | ||
| Male | 47 | 53 |
| Female | 41 | 47 |
| Age (in years), mean ± SD | 7.1 ± 5.3 | |
| 1-4 | 37 | 42 |
| 5-8 | 22 | 25 |
| 9-12 | 13 | 15 |
| 13-18 | 16 | 18 |
| Race | ||
| Chinese | 65 | 74 |
| Malay | 18 | 20.5 |
| Indian | 4 | 5 |
| Others | 1 | 1 |
Abbreviation: PR, permanent resident.
Primary caregiver’s age ranges from 29 to 62.
The caregiving situation and types of technological assistance received by the children are summarized in Table 2. Almost half of the children were ventilated (40.9%). Prevalence of formal (paid) caregiving from a FDW was 57.4%. Considering all sources of support, caregivers received a mean of 74.2 (SD = 49.0) hours per week of help in the care of the technology-dependent child. Six (6.8%) were found to be the sole caregivers of the child. The mean caregiver mMOS-SSS score was 26.5 (SD = 8.3). The mean FSS score was 13.9 (SD = 4.4). Relatively greater impairments were seen in domains of motor function and feeding. Mean CES-D of the caregivers was 16.4 (SD = 10.2), and almost half (44.5%) had CES-D score of ≥16, indicating a risk for clinical depression. The mean PedsQLTSS score was 57.3 (SD = 17.0). In our sample, both CES-D and PedsQLTSS had good internal consistency (Cronbach’s α = .90 and .95, respectively).
Table 2.
Distribution of Child-Related Stressors and Moderators, and Mean Value of Caregiver Outcomes by Child-Related Stressors and Moderators, N = 88.
| n (%) or Mean ± SD | CES-D, Mean ± SD | PedsQLTSS, Mean ± SD | |
|---|---|---|---|
| Child-related stressors | |||
| Functional Status Score (FSS)a of child | |||
| Total score | 13.9 ± 4.4 | ||
| Mental status | 1.5 ± 0.9 | ||
| Sensory function | 1.7 ± 0.9 | ||
| Communication | 2.1 ± 1.1 | ||
| Motor function | 3.0 ± 1.4 | ||
| Feeding | 3.0 ± 1.1 | ||
| Respiratory status | 2.6 ± 1.5 | ||
| Total score | |||
| 6-12 | 30 | 16.6 ± 9.0 | 59.5 ± 15.7 |
| 13-16 | 32 | 18.2 ± 12.7 | 54.6 ± 20.1 |
| 17-25 | 26 | 13.9 ± 7.5 | 58.0 ± 14.3 |
| Type of medical technologyb | |||
| Ventilator-assisted child | 36 (40.9%) | 14.0 ± 9.4 | 61.0 ± 16.8 |
| Only ventilator | 5 | ||
| Tracheostomy | 17 | ||
| Oropharyngeal suctioning | 26 | ||
| Oxygen therapy | 13 | ||
| Enteral tube feeding | 25 | ||
| Urinary catheter | 0 | ||
| Non-ventilator–assisted child | 52 (59.2%) | 18.1 ± 10.4 | 54.7 ± 16.8 |
| Tracheostomy | 10 | ||
| Oropharyngeal suctioning | 14 | ||
| Oxygen therapy | 7 | ||
| Enteral tube feeding | 42 | ||
| Urinary catheter | 6 | ||
| Moderators | |||
| Perceived Social Support (mMOS-SSS) Scorec | |||
| Total score | 57.9 ± 26.0 | ||
| Caregiving help received from others (hours per week) | |||
| 0 hours (no help) | 6 (6.8%) | 20.0 ± 16.3 | 59.0 ± 28.7 |
| 1-42 hours | 25 (28.4%) | 16.9 ± 10.1 | 53.9 ± 15.1 |
| 43-84 hours | 27 (30.7%) | 14.2 ± 10.2 | 61.6 ± 17.0 |
| More than 85 hours | 30 (34.1%) | 15.1 ± 9.2 | 57.9 ± 16.1 |
| Overall mean hours/week | 74.2 ± 49.0 | ||
| Presence of FDW | |||
| No | 37 (42.0%) | 18.0 ± 11.2 | 53.6 ± 18.1 |
| Yes | 51 (58.0%) | 15.2 ± 9.2 | 59.9 ± 15.8 |
| 1 FDW | 36 (40.9%) | 14.8 ± 8.5 | 60.1 ± 15.4 |
| 2 FDWs | 15 (17.0%) | 16.2 ± 11.2 | 57.9 ± 17.3 |
| Overall mean hours/day | 8.1 ± 4.7 | ||
| Caregiver outcomes (overall)d,e | 16.4 ± 10.2 | 57.3 ± 17.0 | |
Abbreviations: CES-D, Center for Epidemiologic Studies Depression Scale; PedsQLTSS, PedsQL Total Summary Score; mMOS-SSS, Medical Outcomes Study: Social Support Survey Instrument; FDW, foreign domestic worker.
FSS ranged from 6 (normal) to 25. A higher score indicates more severe dysfunction.
Some children were on multiple medical technologies concurrently.
mMOS-SSS total score ranged from 0 to 100. A higher score indicates more social support.
CES-D measures caregiver depressive symptoms. Score ranged from 0 to 44. A higher score indicates more negative outcome.
PedsQLTSS measures the health-related quality of life and family functioning of caregiver. Score ranged from 58.4 to 97.2. A higher score indicates more positive outcome.
The relationship between child FSS and caregiver CES-D score was nonlinear, resembling a concave (inverse U) shape: caregivers with children with the highest and lowest FSS had the lowest CES-D scores (Figure 2). To achieve linearity, we transformed the FSS by taking the absolute values of the mean-centered FSS. This had the effect of “folding” the inverted U-relationship at the point of the mean. In the stepwise regression for selection of covariates, caregiver perception of financial adequacy and religion were associated with caregiver CES-D and thus adjusted for in the 3-step hierarchical regression model (Table 3). The final stage of the hierarchical regression model was significant, R2 = 0.33, P < .001 (Table 3). In the first step, of the 2 child stressors, (folded) FSS but not ventilation was associated with CES-D. Every unit (1 SD) increase in the (folded) FSS was associated with a decrease of 2.2 points in the expected CES-D score, holding other variables constant. An increase in the (folded) FSS had the effect of moving toward either extreme of the FSS, away from the average. mMOS-SSS was entered in the second step; every unit (1 SD) increase in mMOS-SSS was associated with a decrease of 2.0 points in the expected CES-D score, holding other variables constant. In the final step, interaction terms (folded FSS × mMOS-SSS) and (Vent × mMOS-SSS) were entered; only the interaction of child function with caregiver-perceived social support was significant. The significant interaction term indicates that the negative relationship between (folded) FSS and caregiver CES-D is attenuated by an increase in mMOS-SSS: higher the caregiver social support, the weaker is the negative relationship between (folded) FSS and CES-D (Figure 3).
Figure 2.
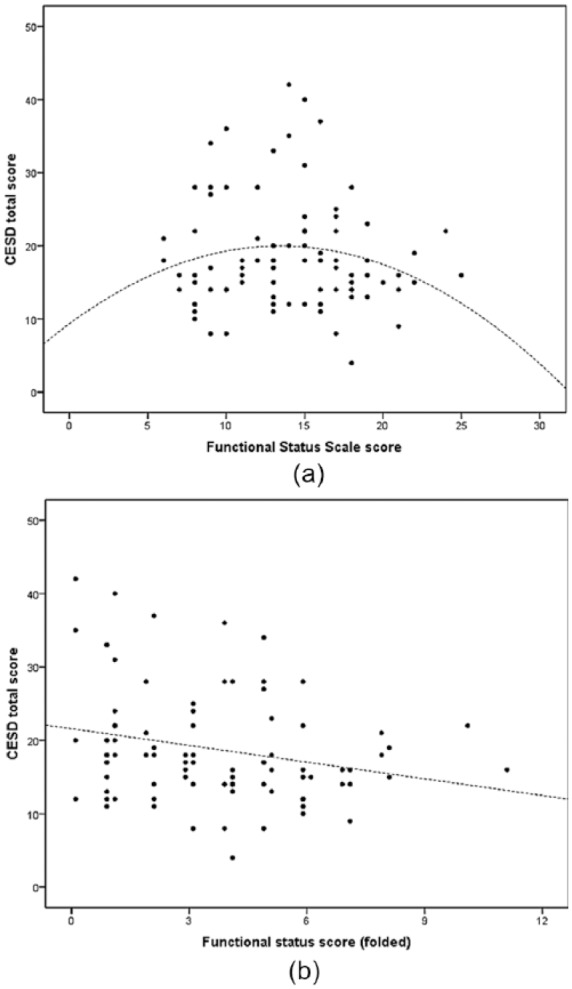
Relationship between functional status (Functional Status Score [FSS]) and depression (Center for Epidemiologic Studies Depression Scale [CES-D]). (a) The nonlinear (concave) relationship between FSS and CES-D. (b) The linearized relationship by folding the centered FSS scores.
Table 3.
Hierarchical Regression of CES-D on Child Stressors and Perceived Social Support, Adjusting for Caregiver Differences at Baseline.
| Unstandardized Coefficients |
Standardized Coefficients |
95% Confidence Interval for B |
|||||
|---|---|---|---|---|---|---|---|
| B | Standard Error | β | t | Sig. | Lower Bound | Upper Bound | |
| Step 1: Child-related stressors (X1, X2) + caregiver covariates (R2 = .242, P < .001) | |||||||
| (Constant) | 18.8 | 1.06 | 17.691 | .00 | 17.053 | 20.593 | |
| Perception of adequacy | −3.7 | 1.55 | −0.23 | −2.374 | .020 | −6.239 | −1.097 |
| Religion (Islam vs non-Islam) | 5.1 | 1.74 | 0.29 | 2.955 | .004 | 2.245 | 8.028 |
| X1: z-ca-FSSa | −2.2 | 0.74 | −0.29 | −2.913 | .005** | −3.405 | −0.930 |
| X2: mechanical ventilationb | −0.8 | 0.76 | −0.11 | −1.124 | .264 | −2.114 | 0.410 |
| Step 2: Child-related stressors (X1, X2) + perceived social support (M) + caregiver covariates (R2 = .305; P = .008) | |||||||
| (Constant) | 18.7 | 1.03 | 18.241 | .000 | 17.008 | 20.422 | |
| Perception of adequacy | −3.1 | 1.50 | −0.20 | −2.073 | .041 | −5.616 | −0.615 |
| Religion (Islam vs non-Islam) | 4.9 | 1.68 | 0.28 | 2.950 | .004 | 2.156 | 7.734 |
| X1: z-ca-FSSa | −2.2 | 0.72 | −0.29 | −3.105 | .003** | −3.421 | −1.034 |
| X2: mechanical ventilationb | −0.4 | 0.75 | −0.06 | −0.577 | .566 | −1.675 | 0.812 |
| M: perceived social supportc | −2.0 | 0.74 | −0.26 | −2.704 | .008** | −3.218 | −0.767 |
| Step 3: (X1, X2) + (M) + interaction terms (X1, M), (X2, M) + caregiver covariates (R2 = .33; P = .218) | |||||||
| (Constant) | 19.0 | 1.04 | 18.338 | .000 | 17.266 | 20.713 | |
| Perception of adequacy | −3.1 | 1.51 | −0.20 | −2.029 | .046 | −5.583 | −0.551 |
| Religion (Islam vs non-Islam) | 3.9 | 1.77 | 0.22 | 2.219 | .029 | 0.979 | 6.853 |
| X1: z-ca-FSSa | −2.1 | 0.72 | −0.27 | −2.836 | .006** | −3.253 | −0.847 |
| X2: mechanical ventilationb | −0.4 | 0.74 | −0.05 | −0.472 | .638 | −1.590 | 0.887 |
| M: perceived social supportc | −2.0 | 0.75 | −0.26 | −2.636 | .010** | −3.222 | −0.728 |
| Interaction (X1 × M) | 1.3 | 0.74 | 0.18 | 1.748 | .084* | 0.061 | 2.521 |
| Interaction (X2 × M) | 0.2 | 0.78 | 0.03 | 0.287 | .775 | −1.078 | 1.526 |
Abbreviations: CES-D, Center for Epidemiologic Studies Depression Scale; FSS, Functional Status Score; mMOS-SSS, Medical Outcomes Study: Social Support Survey Instrument.
Z-score FSS (ca-FSS is the centered mean of FSS score).
Effect coding (users coded 1, nonusers coded 1).
Z-score mMOS-SSS.
P < .10. **P < .05.
Figure 3.

Perceived social support moderates relationship between (folded) Functional Status Score (FSS) and Center for Epidemiologic Studies Depression Scale (CES-D).
The negative relationship between (folded) FSS and CES-D scores is attenuated by level of perceived social support: solid straight line with steepest downward slope represents relationship in caregivers with lower than average (mean = 1 SD) social support; fine broken line with moderate downward slope represents relationship in caregivers with average social support (mean); broad broken line with mildest downward slope represents relationship in caregivers with higher than average (mean + 1 SD) social support.
Among caregiver baseline characteristics, perception of financial adequacy and caregiver completion of secondary education were associated with higher and lower PedsQL scores, respectively, and were consequently adjusted for. The final step of the hierarchical regression model was significant, R2 = .34, P < .001 (Table 4). In the first step, perception of adequacy, education, mMOS-SSS, and ventilation accounted for a significant amount of variance in PedsQLTSS, R2 = .21. mMOS-SSS was not associated with PedsQL but ventilation was. The expected PedsQLTSS score of caregivers of children on mechanical ventilation was 3.8 points higher than the mean of all caregivers, holding other variables constant. The entry of perceived social support (mMOS-SSS) in the second step significantly added to the amount of variance in the criterion accounted for, ΔR2 = .180. With mMOS-SSS (P < .001) in the model, use of mechanical ventilation was no longer associated with PedsQLTSS. Every unit increase (1 SD) in mMOS-SSS was associated with an increase of 6.4 points in the expected PedsQLTSS, holding other variables constant. There being no association between PedsQLTSS and child stressors, we no longer tested for the moderation hypothesis. In the presence of caregiver-perceived social support, neither of the child stressor variables was found to be significantly associated with caregiver HRQOL and family function.
Table 4.
Hierarchical Regression of PedsQLTSS on Child Stressors and Perceived Social Support, Adjusting for Caregiver Differences at Baseline.
| Unstandardized Coefficients |
Standardized Coefficients |
95% Confidence Interval for B |
|||||
|---|---|---|---|---|---|---|---|
| B | Standard Error | β | t | Sig. | Lower Bound | Upper Bound | |
| Step 1: Child-related stressors (X1, X2) + caregiver covariates (R2 = .21, P = .001) | |||||||
| (Constant) | 58.5 | 1.81 | 32.389 | .000 | 55.526 | 61.542 | |
| Perception of adequacy | 5.9 | 2.18 | 0.28 | 2.698 | .009 | 2.252 | 9.510 |
| Secondary education (Yes/No) | −5.9 | 1.80 | −0.33 | −3.262 | .002 | −8.863 | −2.875 |
| X1: z-ca-FSSa | −1.7 | 1.79 | −0.10 | −0.951 | .345 | −4.691 | 1.280 |
| X2: mechanical ventilationb | 3.8 | 1.84 | 0.22 | 2.065 | .042** | 0.738 | 6.869 |
| Step 2: Child-related stressors (X1, X2) + perceived social support (M) + caregiver covariates (R2 = .39; P < .001) | |||||||
| (Constant) | 58.4 | 1.66 | 35.117 | .000 | 55.660 | 61.199 | |
| Perception of adequacy | 4.8 | 2.03 | 0.23 | 2.380 | .020 | 1.450 | 8.192 |
| Secondary education (Yes/No) | −5.7 | 1.66 | −0.32 | −3.431 | .001 | −8.442 | −2.926 |
| X1: z-ca-FSSa | −1.2 | 1.66 | −0.07 | −0.738 | .463 | −3.978 | 1.535 |
| X2: mechanical ventilationb | 2.2 | 1.75 | 0.127 | 1.255 | .213 | −0.716 | 0.5094 |
| M: perceived social supportc | 6.4 | 1.63 | 0.38 | 3.902 | .000** | 3.647 | 9.075 |
| Step 3: (X1, X2) + (M) + interaction terms (X1, M), (X2, M) + caregiver covariates (R2 = .34; P < .001) | |||||||
| (Constant) | 58.0 | 1.74 | 33.367 | .000 | 55.135 | 60.927 | |
| Perception of adequacy | 4.6 | 2.07 | 0.22 | 2.220 | .029 | 1.145 | 8.021 |
| Secondary education (Yes/No) | −5.5 | 1.69 | −0.31 | −3.225 | .002 | −8.264 | −2.636 |
| X1: z-ca-FSSa | −1.3 | 1.69 | −0.08 | −0.758 | .451 | −4.089 | 1.532 |
| X2: mechanical ventilationb | 2.1 | 1.77 | 0.12 | 1.183 | .240 | −0.853 | 5.042 |
| M: perceived social supportc | 6.7 | 1.69 | 0.40 | 3.971 | .000** | 3.902 | 9.538 |
| Interaction (X1 × M) | 0.1 | 1.7 | 0.01 | 0.046 | .963 | −2.684 | 2.837 |
| Interaction (X2 × M) | 1.5 | 1.78 | 0.09 | 0.837 | .405 | −1.476 | 4.457 |
Abbreviations: PedsQLTSS, PedsQL Total Summary Score; FSS, Functional Status Score; mMOS-SSS, Medical Outcomes Study Social: Support Survey Instrument.
Z-score FSS (ca-FSS is the centered mean of FSS score).
Effect coding (users coded 1, nonusers coded 1).
Z-score mMOS-SSS.
P < .10. **P < .05.
Discussion
This study highlights that caregivers of technology-dependent children not only experience more sleep deprivation, daytime sleepiness, and fatigue but also high mental health burden.28 Importantly, the caregivers in our study had higher mean CES-D scores than in those found in other studies of caregivers for children dependent on medical technology and in adult Chinese Singaporeans with chronic disease.7,29 The lower income of this sample compared with the general Singapore population may also explain the higher mental health burden since perception of financial adequacy was associated with both risk of depression and QOL in the analysis.
Our hypothesis that child’s need for mechanical ventilation at home was associated with more caregiver symptoms, however, was not supported. Caring for children requiring other forms of technology support was associated with similarly high mental health burden. Parents of children requiring home ventilation could have better perception of the child’s QOL compared with those parents with children on enterostomy tube feeding if the latter group had more functional limitations.30 In our study, we found that caregivers of children with extremes of function had fewer symptoms of depression. Various studies had shown that caregiving for children with more serious impairments and technological needs was more demanding and perceived as greater source of stress.31,32 In this cohort, we included a population that already had high medical needs. While the child’s dependence on increasingly high-risk technologies was not associated with more caregiver depressive symptoms, moderate functional disability was. One can postulate that at extremes of functions, when the child is either normal or least functional in the various domains of measure, caregiving demands may be lower compared with a child of moderate dysfunction. Higher caregiving demands for children with cerebral palsy has been shown to be associated with worse caregiver psychological health.33 Our findings that perceived social support was both a direct predictor of caregiver depressive symptoms and also a moderator on the relationship between child’s functional status and caregiver depressive symptoms highlight the importance of social support in caregiving. The predictor and moderator effects of social support are in line with findings from studies of mothers caring for children with ventilator dependence7 and cerebral palsy,34 respectively. It is likely that social restriction as a result of caregiving for a technology-dependent child leads to social isolation and potentiates depressive symptoms. It is possible that in caregivers with moderate dysfunction and high caregiving demands, perception of social support helps buffer their mental stress. We did not find correlation of perceived social support with actual hours of help received.
HRQOL and family function in the caregivers was comparable if not lower than in parents of children with chronic conditions cared for at home and lower than in parents of children with chronic conditions in a care facility.25 Perceived social support was also a direct predictor of the caregiver HRQOL and family function. Although need for mechanical ventilation at home was associated with better HRQOL and family function, this effect was negated when social support was added into the model. Although not measured in this study, ventilated patients in this program generally received more home visits and attention by the home care nurses. This, combined with the stronger network of parent support for ventilated children in Singapore, could have accounted for this improved perception. Caregivers with perception of good social support not only had better mental health but also better QOL in cognitive, social, and family functions. This has important implications for future intervention strategies, where targeting social support programs may be more beneficial than just providing formal caregiving help. This study was limited by the relatively modest sample size and participation rate, which posed the potential for selection bias. It also did not account for the heterogeneity and prognoses of the diseases, which can affect caregiver’s perception and stress. Furthermore, child functional status and dependence on high-risk medical technology was measured at one time as a correlate to caregiver health and family outcomes. However, both the predictors and the outcomes are often dynamic and may change with the progression of the child’s condition or any acute change in the clinical status of the child. With time and experience, caregivers could also become more accustomed to home care responsibilities and cope better with the impact of the child’s illness. It would be useful to examine caregiver health and its predictors at various stages of the child’s illness trajectory in a longitudinal study.
Pediatric home care is not well developed in Asia, unlike many Western countries where home care agencies provide formal home health care on a frequent basis, and funding is delivered through government or health care insurance. Asia is undergoing rapid urbanization, and health care expenditure is growing rapidly. The number of technology-dependent children is likely to grow, and provision of home care seems inevitable. Singapore, like many countries in Asia, has a scarcity of such community health care resources for children. Home care depends largely on family members for caregiving, the majority being mothers. Unique to the Asian context, many families also employ FDW for formal caregiving, although this was not found to help alleviate mental stress of caregiving in this study, unlike what was observed in an earlier adult study.20
Singapore is culturally similar to many other parts of Asia. Individuals tend to somatize mental health issues and adopt passive coping strategies such as avoidance and withdrawal rather than to seek help.35
Recommendations
Clinicians managing technology-dependent children should also assess and manage the mental health and QOL of parental caregivers. This study also highlights the need to plan for strong social support networks as well as a robust mental health screening and intervention program for these caregivers. Further studies into factors that influence perceived social support in these caregivers are needed to inform strategies to improve mental health outcomes.
Acknowledgments
We thank Bernadette Sook Han Teoh for organizing the interviews and Rina Nianlin Han for the Chinese translation of the questionnaires.
Footnotes
Author Contributions: YHC: Contributed to conception and design; contributed to acquisition, analysis, and interpretation; drafted the manuscript; critically revised the manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
CZRL: Contributed to design; contributed to acquisition, analysis, and interpretation; drafted the manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
DB: Contributed to analysis and interpretation; critically revised the manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
RM: Contributed to conception and design; contributed to analysis and interpretation; critically revised the manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
TØ: Contributed to conception and design; contributed to analysis and interpretation; critically revised the manuscript; gave final approval; agrees to be accountable for all aspects of work ensuring integrity and accuracy.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The authors received financial support from the Duke-NUS Academic Medicine Philanthropic Fund for the research.
ORCID iD: Yoke Hwee Chan  https://orcid.org/0000-0002-7612-6414
https://orcid.org/0000-0002-7612-6414
References
- 1. Cohen E, Kuo DZ, Agrawal R, et al. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics. 2011;127:529-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wise PH. Emerging technologies and their impact on disability. Future Child. 2012;22:169-191. [DOI] [PubMed] [Google Scholar]
- 3. US Congress Office of Technology Assessment. Technology-Dependent Children: Hospital vs Home Care—A Technical Memorandum. Washington, DC: US Government Printing Office; 1987. [Google Scholar]
- 4. American Academy of Pediatrics Council on Children With Disabilities; Duby JC. Role of the medical home in family-centered early intervention services. Pediatrics. 2007;120:1153-1158. [DOI] [PubMed] [Google Scholar]
- 5. Caicedo C. Families with special needs children: family health, functioning, and care burden. J Am Psychiatr Nurses Assoc. 2014;20:398-407. [DOI] [PubMed] [Google Scholar]
- 6. Kirk S. Families’ experiences of caring at home for a technology-dependent child: a review of the literature. Child Care Health Dev. 1998;24:101-114. [DOI] [PubMed] [Google Scholar]
- 7. Kuster PA, Badr LK. Mental health of mothers caring for ventilator-assisted children at home. Issues Mental Health Nurs. 2006;27:817-835. [DOI] [PubMed] [Google Scholar]
- 8. Toly VB, Musil CM, Carl JC. Families with children who are technology dependent: normalization and family functioning. West J Nurs Res. 2012;34:52-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cousino MK, Hazen RA. Parenting stress among caregivers of children with chronic illness: a systematic review. J Pediatr Psychol. 2013;38:809-828. [DOI] [PubMed] [Google Scholar]
- 10. Department of Statistics, Ministry of Trade and Industry, Republic of Singapore. Population Trends, 2016. Singapore: Department of Statistics; 2016. [Google Scholar]
- 11. Glendinning C, Kirk S, Guiffrida A, Lawton D. Technology-dependent children in the community: definitions, numbers and costs. Child Care Health Dev. 2001;27:321-334. [DOI] [PubMed] [Google Scholar]
- 12. Wang KW, Barnard A. Technology-dependent children and their families: a review. J Adv Nurs. 2004;45:36-46. [DOI] [PubMed] [Google Scholar]
- 13. Murphy NA, Christian B, Caplin DA, Young PC. The health of caregivers for children with disabilities: caregiver perspectives. Child Care Health Dev. 2007;33:180-187. [DOI] [PubMed] [Google Scholar]
- 14. Bemister TB, Brooks BL, Dyck RH, Kirton A. Predictors of caregiver depression and family functioning after perinatal stroke. BMC Pediatr. 2015;15:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Douglas SL, Daly BJ. Caregivers of long-term ventilator patients: physical and psychological outcomes. Chest. 2003;123:1073-1081. [DOI] [PubMed] [Google Scholar]
- 16. Carnevale FA, Alexander E, Davis M, Rennick J, Troini R. Daily living with distress and enrichment: the moral experience of families with ventilator-assisted children at home. Pediatrics. 2006;117:e48-e60. [DOI] [PubMed] [Google Scholar]
- 17. Rodakowski J, Skidmore ER, Rogers JC, Schulz R. Does social support impact depression in caregivers of adults ageing with spinal cord injuries? Clin Rehabil. 2013;27:565-575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ergh TC, Rapport LJ, Coleman RD, Hanks RA. Predictors of caregiver and family functioning following traumatic brain injury: social support moderates caregiver distress. J Head Trauma Rehabil. 2002;17:155-174. [DOI] [PubMed] [Google Scholar]
- 19. Sander AM, High WM, Jr, Hannay HJ, Sherer M. Predictors of psychological health in caregivers of patients with closed head injury. Brain Inj. 1997;11:235-249. [DOI] [PubMed] [Google Scholar]
- 20. Østbye T, Malhotra R, Malhotra C, Arambepola C, Chan A. Does support from foreign domestic workers decrease the negative impact of informal caregiving? Results from Singapore survey on informal caregiving. J Gerontol B Psychol Sci Soc Sci. 2013;68:609-621. [DOI] [PubMed] [Google Scholar]
- 21. Wild D, Grove A, Martin M, et al. ; ISPOR Task Force for Translation and Cultural Adaptation. Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health. 2005;8:94-104. [DOI] [PubMed] [Google Scholar]
- 22. Pollack MM, Holubkov R, Glass P, et al. ; Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network. Functional Status Scale: new pediatric outcome measure. Pediatrics. 2009;124:e18-e28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385-401. [Google Scholar]
- 24. Stahl D, Sum CF, Lum SS, et al. Screening for depressive symptoms: validation of the Center for Epidemiologic Studies Depression Scale (CES-D) in a multiethnic group of patients with diabetes in Singapore. Diabetes Care. 2008;31:1118-1119. [DOI] [PubMed] [Google Scholar]
- 25. Varni JW, Sherman SA, Burwinkle TM, Dickinson PE, Dixon P. The PedsQL Family Impact Module: preliminary reliability and validity. Health Qual Life Outcomes. 2004;2:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Moser A, Stuck AE, Silliman RA, Ganz PA, Clough-Gorr KM. The eight-item modified Medical Outcomes Study Social Support Survey: psychometric evaluation showed excellent performance. J Clin Epidemiol. 2012;65:1107-1116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Singapore Department of Statistics. Key household income trends. http://www.nas.gov.sg/archivesonline/data/pdfdoc/20170216002/Key%20Household%20Income%20Trends%202016%20Press%20Release.pdf. Published February 16, 2017. Accessed December 19, 2018.
- 28. Keilty K, Cohen E, Spalding K, Pullenayegum E, Stremler R. Sleep in family caregivers of children who depend on medical technology. Arch Dis Child. 2018;103:137-142. [DOI] [PubMed] [Google Scholar]
- 29. Zhang Y, Ting RZ, Lam MH, et al. Measuring depression with CES-D in Chinese patients with type 2 diabetes: the validity and its comparison to PHQ-9. BMC Psychiatry. 2015;15:198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Redouane B, Cohen E, Stephens D, et al. Parental perceptions of quality of life in children on long-term ventilation at home as compared to enterostomy tubes. PLoS One. 2016;11:e0149999.26914939 [Google Scholar]
- 31. Plant KM, Sanders MR. Predictors of care-giver stress in families of preschool-aged children with developmental disabilities. J Intellect Disabil Res. 2007;51(pt 2):109-124. [DOI] [PubMed] [Google Scholar]
- 32. Kirk S, Glendinning C, Callery P. Parent or nurse? The experience of being the parent of a technology-dependent child. J Adv Nurs. 2005;51:456-464. [DOI] [PubMed] [Google Scholar]
- 33. Raina P, O’Donnell M, Rosenbaum P, et al. The health and well-being of caregivers of children with cerebral palsy. Pediatrics. 2005;115:e626-e636. [DOI] [PubMed] [Google Scholar]
- 34. Manuel J, Naughton MJ, Balkrishnan R, Smith BP, Koman LA. Stress and adaptation in mothers of children with cerebral palsy. J Pediatr Psychol. 2003;28:197-201. [DOI] [PubMed] [Google Scholar]
- 35. Kung WW. Cultural and practical barriers to seeking mental health treatment for Chinese Americans. J Community Psychol. 2004;32:27-43. [Google Scholar]



