Abstract
Background:
A Rapid Response Team can respond to critically ill patients in hospital to prevent further deterioration and unexpected deaths. However, approximately one-third of reviews involve a patient approaching the end-of-life. It is not well understood whether patients have pre-existing advance care plans at the time of significant clinical deterioration requiring Rapid Response Team review. Nor is it understood whether such critical events prompt patients, their families and treating teams to discuss advance care planning and consider referral to specialist palliative care services.
Aim and design:
This systematic review examined advance care planning with patients who experience significant clinical deterioration in hospital and require Rapid Response Team review. The prevalence of pre-existing advance directives, whether this event prompts end-of-life discussions, the provision of broader advance care planning and referral to specialist palliative care services was examined.
Data sources:
Three electronic databases up to August 2017 were searched, and a manual review of article reference lists conducted. Quality of studies was appraised by the first and fourth authors.
Results:
Of the 324 articles identified through database searching, 31 met the inclusion criteria, generating data from 47,850 patients. There was a low prevalence of resuscitation orders and formal advance directives prior to Rapid Response Team review, with subsequent increases in resuscitation and limitations of medical treatment orders, but not advance directives. There was high short- and long-term mortality following review, and low rates of palliative care referral.
Conclusions:
The failure of patients, their families and medical teams to engage in advance care planning may result in inappropriate Rapid Response Team review that is not in line with patient and family priorities and preferences. Earlier engagement in advance care planning may result in improved person-centred care and referral to specialist palliative care services for ongoing management.
Keywords: advance care planning, advance directives, hospital Rapid Response Team, palliative care
Introduction
Advance care planning is the process of determining future health care needs for a time when a person may be unable to speak for themselves due to illness or impaired cognition.1,2 It involves multiple steps: discussing options for future care, appointing a substitute decision maker, discussing care options, priorities and preferences, and documenting those preferences for future consideration.1 It can be a complex process that may need to take place over time.3
An advance care plan that balances clinical realities with patients’ values and priorities1 may reduce unwanted, burdensome or intensive treatments at the end-of-life in line with patients’ care preferences.4,5 It may give greater control over psychological and physical symptoms3–5 and reduce stress, anxiety and depression in surviving relatives.1,6,7 There is also the potential to reduce health care spending at the end-of-life on resource-intensive, inappropriate or futile interventions that may contribute to increased suffering for patients, their families and carers.7,8 It may also facilitate better access to palliative care or hospice services.3,9
Rapid Response Systems have been established in many hospitals in Australia and internationally10,11 to provide a prompt response to critical patients to prevent further deterioration, unexpected deaths, cardiac arrest or the need to transfer patients to an Intensive Care Unit (ICU).12,13 Staff activate a Rapid Response Team (RRT) review according to established criteria which may indicate physiological instability,12,14 or concern about a patient’s condition. A person in the process of dying can also trigger activation due to meeting one or more of the calling criteria.15 Over time, the RRT has taken on secondary functions: the diagnosis of dying, initiating end-of-life discussions and establishing limitations of medical treatment.13,15–20 However, the RRT may not always adequately address the needs of patients at the end-of-life due to limited access to comprehensive information about current illness, disease trajectory, and treatment and care preferences. This may be better addressed as part of an advance care planning process.21
A systematic review of the role of the RRT in end-of-life care by Jones and colleagues15 reported up to one-third of RRT reviews may involve a patient approaching the end-of-life. These teams had a role in establishing limitations of medical treatment or not for resuscitation orders, conducting patient and family meetings, documentation of comfort care orders and initiating chaplain visits. Similarly, Tan and Delaney22 found the RRT had a vital role in providing end-of-life interventions which included establishing limitations of medical treatment. These reviews provide a greater understanding of the role of the RRT with patients at the end-of-life.
Little is known about the influence of RRT reviews on the broader provision of advance care planning that integrates patient values, preferences and priorities. This includes the prevalence of pre-existing written advance directives, and whether the RRT review prompts discussing and documenting care preferences and priorities and establishing a legal substitute decision maker. This represents a current gap in the literature. Further understanding of how advance care planning may impact the care provided at the time of a clinical deterioration in hospital is needed. With up to one-third of patients requiring RRT review approaching the end-of-life, this is a critical event that should prompt health professionals to initiate an advance care planning discussion for many patients.
Aim
In response to the aforementioned knowledge and practice gaps, this systematic review aims to examine the current research evidence by considering observational and experimental studies that can contribute further knowledge of the provision of advance care planning. This is in relation to the clinical deterioration of patients in hospital requiring RRT review. It examines trends in discussions between medical teams and patients, families or substitute decision makers and how formal, pre-existing advance directives are documented and influence care planning. Prompts for further establishment of patient goals, priorities and preferences for medical care and treatment, and referral for specialist palliative care management is examined.
Method
This systematic literature review was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) approach.23
Eligibility criteria
A systematic search was conducted to identify studies that described the deployment of an RRT, related to end-of-life decision making with human participants, described aspects of advance care planning and described an experimental or observational study. Studies addressing paediatric or mental health RRT calls were not within the scope of this study as the focus was on patients who are likely to benefit from the provision of advance care planning due to their current medical condition or illness trajectory with a particular focus on end-of-life care. Papers not published in English were also excluded if no translation was readily available. There is debate as to whether the establishment of Not for Resuscitation and Limitations of Medical Treatment orders form part of the advance care planning process.21 For the purposes of this review, articles that only focussed on these medical orders without reporting on broader aspects of advance care planning were excluded.
Search
An electronic Title/Abstract/Keyword search of relevant literature was performed using Scopus®, PubMed and PsycNet. Search terms were Medical Subject Heading (MeSH) keyword searches for ‘Advance Care Planning’, ‘Advance Directive’, AND ‘Hospital Rapid Response Team’ and METeOR term ‘Rapid Response Team’. Searches were performed to identify peer-reviewed manuscripts up to August 2017. Searches of reference lists in published manuscripts were also conducted to ensure other relevant studies were captured.
Study selection
Articles returned from the electronic database searches were imported into Endnote (version X7), and the titles and abstracts of all papers were examined by the first author to ascertain whether they met the inclusion criteria.
Data collection and items
Data were compiled into table format in Microsoft Word. Items included the publication year; hospital type; bed numbers; country; study design; main findings (Table 1); total patient numbers; total RRT reviews; not for resuscitation and limitations of medical treatment before and after clinical deterioration requiring RRT review; pre-existing advance care planning documents; discussions with the patient, family or proxy decision maker; palliative care consultation; escalation to higher level care; and in-hospital mortality (Table 2). Numbers were expressed as a percentage of RRT reviews or number of patients where RRT review figures was not available.
Table 1.
Study type, methods and main findings.
| Study first author | Year | Hospital type (beds) | Country | Study design | Main findings |
|---|---|---|---|---|---|
| Austin24 | 2014 | Academic (800+) with specialist cancer centre (50) | The United States | Retrospective cohort | NFR orders created before, during and after the RRT review were low, at 9.6%, 3% and 13.3%, respectively. RRT activations were higher for oncology patients than general medical patients (37.34 v 20.86 per 1000 patient discharges) |
| Boniatti25 | 2010 | Academic (794) | Brazil | Retrospective observational | RRT review is associated with a high 30-day mortality, with NFR orders before and after the RRT review 5.1% and 3.3%, respectively |
| Calzavacca26 | 2010 | Tertiary (400) | Australia | Retrospective observational | 22.7% of patients had an NFR order prior to RRT review and an additional 8.5% after. Patients with multiple RRT reviews have increased risk of mortality |
| Calzavacca27 | 2010 | Tertiary (400) | Australia | Retrospective observational | 15% of patients had an NFR order prior to RRT review and further 9.5% after |
| Calzavacca28 | 2008 | Tertiary (NS) | Australia | Prospective observational | Presence of NFR orders was independently associated with mortality |
| Cardona-Morrell29 | 2016 | Teaching (NS) | Australia | Retrospective case-control analysis | Older patients requiring RRT with pre-existing LOMT or multiple indicators of chronic illness, cognitive impairment and frailty had a higher risk of death |
| Casamento30 | 2008 | General (NS) | Australia | Prospective audit and chart review | High in-hospital mortality following RRT review (32%) |
| Chen20 | 2008 | 23 hospitals | Australia | Cluster randomized control trial | NFR orders were uncommon for people receiving RRT review for cardiac arrest or unplanned ICU admission, due to limited time in which to discuss end-of-life wishes |
| Dargin31 | 2014 | Tertiary (350) | The United States | Retrospective | High in-hospital mortality for patients following RRT review. End-of-life care may be improved with better coordination between medical teams and palliative care |
| Downar32 | 2013 | 3 academic (NS) | Canada | Retrospective | In-hospital mortality for patients with an NFR order was high. RRTs frequently facilitate end-of-life discussions and decision making |
| Gouda and Alqahtani33 | 2016 | Tertiary (1200) | Saudi Arabia | Retrospective chart review | RRTs have a key role in addressing and initiating NFR orders |
| Jäderling34 | 2013 | Teaching (650) | Sweden | Observational cohort | In-hospital mortality for patients with NFR orders was high in the short- and long-term. Decisions about limitations of treatment are often made close to the time of the RRT review and did not preclude further RRT reviews |
| Jäderling35 | 2011 | 2 Teaching (650)/(400) | Sweden Australia |
Two-centre prospective observational study | Similarities in pre-existing LOMT (34.2% and 30.8%) and those implemented after RRT review (14.4% and 12.6%) were found between two different centres in Sweden and Australia, respectively |
| Jones11 | 2012 | 7 Academic | Australia (5) Canada (1) Sweden (1) |
Prospective audit | Approximately one-third of RRT reviews involved end-of-life and LOMT issues, highlighting a need for improved advance care planning |
| Medical Emergency Team End-of-Life Care investigators14 | 2013 | 7 Academic | Australia (5) Canada (1) Sweden (1) |
Prospective audit | Patients who required RRT review later in the admission (after day 7) were more likely to have a LOMT than patients receiving review on day 0 or 1 |
| Knott17 | 2011 | Tertiary teaching (450) | New Zealand | Retrospective cohort | LOMT and NFR documentation rates doubled after RRT review |
| O’Horo36 | 2015 | Tertiary (NS) | The United States | Retrospective chart review and prospective survey | Involvement of the primary treating team in RRT reviews was associated with significantly higher transfers to higher level care and discussion about code status |
| Parr37 | 2001 | Tertiary (580) | Australia | Retrospective cohort | The RRT can identify patient for whom an NFR should be considered |
| Psirides38 | 2016 | 11 (including 6 tertiary, 1 paediatric) | New Zealand | Prospective multicentre observational | RRT reviews resulted in new NFR orders (22.5%), altered early warning system calling criteria (10.8%) and other treatment limitations (8.8%) |
| Schneider39 | 2011 | Teaching (400) | Australia | Retrospective cohort | Atrial fibrillation was a trigger for approximately 10% of RRT activations |
| Silva40 | 2016 | Tertiary academic (600) | Portugal | Retrospective cohort | Prior to RRT activation, 5.1% of patients had an NFR order and 2.5% had a withhold therapy decision. An additional 24.1% had end-of-life decisions as part of the RRT actions |
| Smith41 | 2014 | Tertiary (300) | The United States | Retrospective audit (non-cardiac arrest events only) | NFR orders were in place before the RRT review for 11.01% of patients, with an additional 5.5% created at the time of the RRT review |
| Smith42 | 2015 | Academic teaching (400) | Australia | Retrospective cohort | NFR implemented by RRT during early reviews (<48 h of admission) in 3.91% of cases, 5.45% for intermediate cases (48<168 h after admission) and 8.39% in late cases (⩾168 h after admission) |
| Smith13 | 2014 | Tertiary (NS) | Australia | Retrospective, quasi-experimental | 28% of RRT reviews were associated with an NFR order. In 11.5% of instances, NFR was placed prior to the review |
| Stelfox21 | 2015 | 2 tertiary, 2 community (2883) | Canada | Retrospective database review | 2% of patients <50 years and 15% of patients >80 years had goals of care changed to exclude resuscitation following RRT review |
| Sulistio19 | 2015 | 3 hospitals (NS) | Australia | Retrospective cohort | 36.2% of patients had documented LOMT, 77.2% of these were instituted following the RRT review. Goals were changed to a more palliative intent in 28.5% of patients following RRT review |
| Sundararajan43 | 2014 | Tertiary (650) | Australia | Prospective study | Pre-existing LOMT orders were more likely to have been made in consultation with the patient or NOK (patient 50%, NOK 90%) compared with LOMT associated with an RRT review (patient 18%, NOK 58%) |
| Tam44 | 2014 | Tertiary (458) | Canada | Retrospective chart review | 6% of patients had their resuscitation status initiated or revisited by the RRT. Of these, 27% of patients had their status changed to NFR following the consultation |
| Tirkkonen45 | 2016 | University (NS) | Finland | Prospective observational | New LOMT were issued for 9.2% patients following RRT review following discussion with the patient in 19% or cases and discussion with relatives in 69% of cases |
| Tirkkonen46 | 2013 | Tertiary (769) | Finland | Prospective observational | NFR orders were associated with increased hospital mortality |
| Visser47 | 2014 | Sub-acute (NS) | Australia | Retrospective observational | LOMT were documented for 79.4% patients on admission. For 22.7% of the RRT reviews, there was an increase in LOMT following review by the RRT |
| White48 | 2016 | University teaching (780) | Australia | Prospective cohort | Few RRT activations were associated with a resuscitation order, with high mortality and transfers to ICU following RRT reviews |
LOMT, limitations of medical treatment; NFR, not for resuscitation; NOK, next of kin; RRT, Rapid Response Team.
Table 2.
Care and treatment planning characteristics.
| Study first author | Total patient numbers | Total RRT reviews | NFR/LOMT before RRT review | NFR/LOMT during or after RRT review | Escalation to higher level care, e.g. ICU | In-hospital mortality | Formal advance care planning | Discussion with patient, family or proxy decision maker | Palliative care consultation |
|---|---|---|---|---|---|---|---|---|---|
| Austin24 | Ca centre: 135 Gen med: 422 Total: 557 |
NS | 9.6%* | 1.5% D*
13.3% A* |
34.8% | 21.5% | NS | NS | 1.5% B*
4.4% A* |
| Boniatti25 | 901 | 1051 | 5.1% | 3.3% A | 55.4% | 46.9% at 30 days | NS | NS | NS |
| Calzavacca26 | 1664 | 2237 | 22.7% | 8.5% A | 16% | 34.3% | NS | NS | NS |
| Calzavacca27 | 200 | 200 | 15% | 9.5% | 17.5% | 27% | NS | NS | NS |
| Calzavacca28 | 228 | 251 | 14.5% | 9.2% | 16.7% | 40% | NS | NS | NS |
| Cardona-Morrell29 | 2353 | 328# | 12.5% | 32.5% D | NS | 7.8% of patients aged 60+ | 5% | NS | NS |
| Casamento30 | NS | 195 | 20% | 15% | 28% | 34% | NS | NS | NS |
| Chen20 | NS | 4161^ | 45.4% | 3.85% | 19.1% | 47.2% | NS | NS | NS |
| Dargin31 | 998 | 1156 | 8.65% | 5% D | 39.7% | 17% | NS | 44%@ | 2.68% |
| Downar32 | NS | 291 | 8.9% | NS | 33% | 24.7% | NS | 16.5% within 48 h | 0% B 13% within 48 h^^ 17% after 48 h^^ |
| Gouda and Alqahtani33 | NS | 5904 | 6.66% D 1.27% A |
34.5% | NS | NS | NS | NS | |
| Jäderling34 | 1818 | 2189 | 4.7% | 16.3% D 14.4% A |
31.5% | 25.6% | NS | NS | NS |
| Jäderling35 | NS | 3063 | 34.2% Sweden 30.8% Australia |
14.4% Sweden 12.6% Australia |
18.7% Sweden 9.9% Australia |
27.7% Sweden 29.4% Australia |
NS | NS | NS |
| Jones11 | 518 | 652 | 20.3% | 10.8% | NS | NS | NS | NS | |
| Medical Emergency Team End-of-Life Care investigators14 | 518 | 652 | Early/late reviews 16.9%/26.3% |
Early/late reviews 25.4%/35.9% |
NS | Early/late review 12.8%/32.3% |
NS | NS | NS |
| Knott17 | 71 | NS | 32% | 62% | NS | 42% | NS | NS | NS |
| O’Horo36 | NS | Retrospective 4408 Prospective 135 |
Retrospective/prospective study 13.5%/16.3% |
Retrospective/prospective study 7.2% D /5.9% D |
Retrospective study: 58.6% Prospective study: 62.2% |
NS | NS | NS | NS |
| Parr37 | 559 | 713 | 0% | 4.8% A | 45% | 6.9% D | NS | NS | NS |
| Psirides38 | 313 | 351 | NS | 31.3% (22.5% NFR, 8.8% other LOMT) | 13.1% | 2.8% at time of RRT 19.8% at 30 days |
NS | NS | NS |
| Schneider39 | 458 | 557 | 19.7% | 7% D | 11.4% | 20.1% | NS | NS | NS |
| Silva40 | 389 | 389 | 7.7% B | 24.1% D | 39.3% | 18.7% D 52.8% overall |
NS | NS | NS |
| Smith41 | 1117 | NS | 11.01% B | 5.55% D | 17.91% | 18.8%: deterioration group 62.64%: cardiac arrest group |
NS | NS | NS |
| Smith42 | 2843 | 3860 | 15.2% | 5.7% D | 15.5% | 12.8% early RRT review 16.7% intermediate RRT review 30.6% for late RRT review 59.4% for patients who had cardiac arrest |
NS | NS | NS |
| Smith13 | NS | 390 | 11.5% | 16.4% A | 54% | NS | NS | NS | NS |
| Stelfox21 | 5103 | NS | 3.8% 4910/5103 | 8.05% D | 24.83% | 32.6% | NS | NS | NS |
| Sulistio19 | 351 | 456 | 17.9% NFR 1.42% LOMT |
21.7% | 24.5% | NS | NS | 15.1% | |
| Sundararajan43 | NS | 994 | Group 1 LOMT not associated with RRT team review 100% |
Group 2: Limitations of Medical Treatment at time of RRT review 5% | NS | NS | NS | Group 1 50% with patient 90% with next of kin Group 2: 18% with patient 58% with next of kin |
NS |
| Tam44 | 5320 | NS | 58% | 17% D | 8.4% of ‘end-of-life’ group 17% of ‘non-end-of-life’ group |
25% of ‘end-of-life’ group 8% of ‘non-end-of-life’ group |
NS | NS | 34% of ‘end-of-life’ group 5.3% of ‘non-end-of-life’ group |
| Tirkkonen45 | 640 | 774 | 0% | 9.22% | 26% (no LOMT) 3.4% (LOMT) |
14% (no LOMT) 44% (LOMT) |
NS | 76% for new LOMT (7% of total patients) | NS |
| Tirkkonen46 | 458 | 569 | 6.3% | 7.4% D | 27.2% | 26% | NS | NS | NS |
| Visser47 | 132 | 141 | 79.4% | 24.2% D | 10.6% | 28% | NS | NS | NS |
| White48 | 800 | 1151 | 22.2% | 2% D 5% A |
17.2% | 12.6% | NS | NS | NS |
A, after; B, before; D, During; ICU, intensive care unit; LOMT, limitations of medical treatment; NFR, not for resuscitation; NS, not stated; RRT, Rapid Response Team.
Cancer centre patients.
Included 184 cases where patient died following RRT review; 144 controls who lived.
Hospitals with an RRT (control hospitals without RRT were excluded).
Resuscitation status at admission.
Subset of patients who had a change in NFR status following the RRT review.
Study selection
The electronic search yielded 312 references and an additional 12 were identified via manual reference searching. A total of 149 duplicate references were excluded, related to studies conducted in the paediatric or mental health setting, or no English language version was available. Potentially relevant titles and abstracts for 175 articles were reviewed. Of these, 124 were excluded as they did not describe an observational or interventional study or did not relate to advance care planning or clinical deterioration requiring the RRT review. A total of 51 were selected for full-text review based on their title and abstract. Studies were excluded that included only one measure of not for resuscitation orders or limitations of medical treatment, with no comparison of how the RRT review impacted the implementation of such orders. Other studies with limited scope such as those that considered only patients who died in hospital or were transferred to an ICU were excluded. A total of 31 articles met the review selection criteria and were included. The study selection process is shown in Figure 1.
Figure 1.
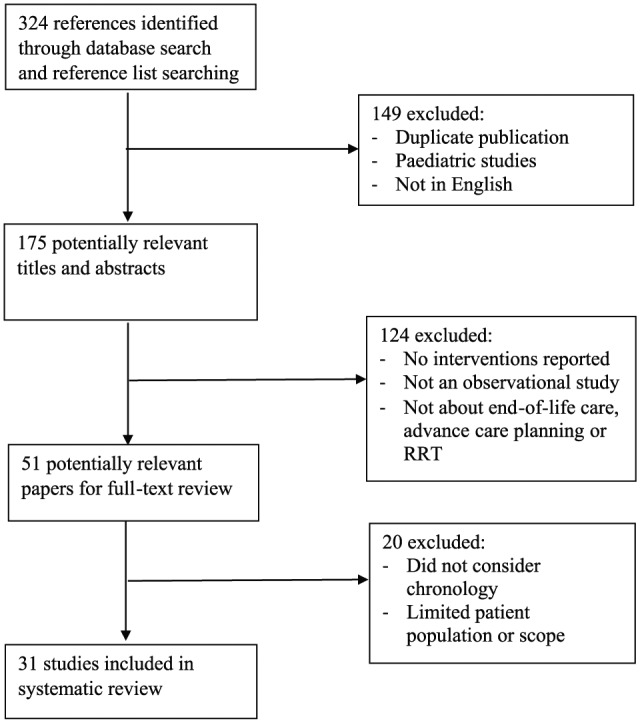
Flow diagram of systematic review process.
RRT, Rapid Response Team.
Results
Study characteristics
Study location
Single-site studies were conducted in Australia (14), Brazil (1), Canada (1), Finland (2), New Zealand (1), Saudi Arabia (1), Sweden (1) and the United States (4). Multisite studies were conducted in Australia (2), Canada (2) and New Zealand (1), and three multisite international studies were conducted. Psirides and colleagues38 reported a multicentre study which included 11 hospitals, of which 6 were tertiary and 1 paediatric. Although paediatric RRT reviews were beyond the scope of this review, this study was still included as only 7.1% of the total patients receiving an RRT review call were paediatric, forming only a minor aspect of the data set for this study (A. Psirides, personal communication, 15 July 2017).
Study design
All studies as listed in Table 1 used quantitative methods of data collection. One study used a cluster randomized control study design, one a case-control analysis and all other studies using a retrospective or prospective cohort design. Two studies in this review described quasi-experimental studies.13,29
Sample characteristics
Studies were conducted at a range of hospital types, including large tertiary hospitals, university-affiliated academic hospitals, community and sub-acute hospitals and one with a specialist cancer-care centre.
The sample sizes ranged from 71 patients receiving an unspecified number of RRT reviews,17 to 5904 reviews carried out with an unspecified number of patients.33 Total patient numbers were 47,850.
Several studies reported a defined patient cohort as part of their overall data collections, including patients at a cancer-care centre,24 or where the RRT review occurred early, compared with late in an admission.14
Advance care planning characteristics
A summary of the advance care planning characteristics described in the study is included in Table 2. Most studies focussed on reporting the institution of not for resuscitation or limitations of medical treatment orders before, during and after the RRT review. These ranged from 0%37 to 79.4%47 before the RRT review, 1.5%24 to 32.5%29 at the time of the RRT review and 1.27%33 to 62%17 after the RRT review.
The incidence of formal advance care planning documents such as an Advance Directive was reported in only one study,29 with only 5% of patients having a directive in place.
Four studies reported the involvement of a patient, family member or formal Substitute Decision Maker in discussions about limitations of medical treatment or goals of care planning at the time or following a clinical deterioration requiring RRT review. Downar and colleagues32 reported that a family and/or patient conference was held for 16.5% of patients who were for full resuscitation at the time of the RRT review. Sundararajan and colleagues43 found that only 18% of patients were involved in discussions relating to limitations of medical treatment instituted by the RRT, with families or substitute decision makers involved in 58% of cases. This was less than for patients with pre-existing limitations of medical treatment, when patients and their family or substitute decision maker were involved 50% and 90% of the time, respectively. Tirkkonen and colleagues45 reported that families or next of kin were involved in discussions about new limitations of medical treatment (7% of total patients), in 76% of cases.
Palliative care consultation varied greatly among the three articles that reported figures24,32,44 from 1.5% of patients before the clinical deterioration requiring RRT review,24 up to 34% of patients identified as being at the end-of-life after review.44 Escalation of care to a critical care unit ranged from a low of 3.4% of patients following clinical deterioration,45 to a high of 62.2%.36 Downar and colleagues32 reported referral for spiritual care consultation for 12% patients following RRT review; no other studies reported this parameter.
Mortality
Mortality was reported in most studies as having occurred at the time of the RRT review, at 30 days post-review, for a subgroup of patients, such as those over 60 years, or in hospital. Mortality ranged from 2.8% at the time of the clinical deterioration38 to 62.6% of patients following in-hospital cardiac arrest.39
Discussion
The study setting, research methods, differences in patient cohorts and, not surprisingly, outcomes were highly variable. Most outcomes focussed on the establishment of medical orders relating to end-of-life care, with data on advance care planning discussions establishing patient values, priorities and preferences largely missing. Studies were conducted in a wide variety of countries, where policies relating to end-of-life care and advance care planning differ. In the United States, for example, the Patient Self-Determination Act49 requires all Medicaid and Medicare funded facilities to ask patients about pre-existing advance directives. Australia has no such requirement, although recent national policy developed by the Australian Commission on Safety and Quality in Health Care states that all health professionals should identify existing advance care plans and invite patients to participate in advance care planning.50 The heterogeneity of the methods did not allow the direct comparison of studies or meta-analysis of results.
RRTs have a critical role in hospitals, but approximately one-third of patients reviewed by the RRT are approaching the end-of-life,11,51 such as frail, elderly patients,52 and those with high incidence of co-morbidity.41,42 The aim of this review was to examine the provision of advance care planning in patients who deteriorated in hospital and required RRT review. This builds upon previous reviews conducted by Jones and colleagues15 and Tan and Delaney22 to further understand the role of the RRT with patients approaching the end-of-life.
This review confirmed that a patient’s clinical deterioration requiring RRT review led to a focus on end-of-life decision making and establishing ceilings of care by the RRT team, which is entirely appropriate given the role of such teams. However, relying on RRT to service the needs of patients with irreversible and persistent symptomatology is filled with inherent difficulties. These teams have limited knowledge of patients’ complex medical history, trajectory of illness and long-term care needs, and a finite window of time in which to appropriately address those needs before further deterioration.19
Goals of care discussions should be separate to RRT review so they are more likely to involve patients and their families in care discussions that consider values, treatment priorities and preferences.43 The primary team is likely to have greater access to the comprehensive medical history, information about current illness, and recent illness trajectory, and it should be their role to guide such conversations. Short timeframes between admission and RRT activation may preclude the provision of advance care planning with the patient, their families and substitute decision maker, and the patient’s clinical deterioration itself could be the catalyst to do so.19 Failure to involve patient and their families in care discussions may result in inappropriate activation of the RRT team and the provision of treatments that are not aligned with patient’s priorities and preferences.
There may be variability in the quality of end-of-life discussions in acute hospitals following an acute event due to time constraints, skill of staff and a patient’s need for urgent care. Some patients may not be ready to consider existential and end-of-life issues; however, they and their family members should be given the opportunity to do so. This may start with providing patients with educational materials and advance care planning forms. Patient and family involvement in advance care planning may lead to greater satisfaction with the end-of-life experience and reduced bereavement risk.7 Few studies in this review included discussion of family member involvement in decision making31,32,45 and further research that considers the provision of advance care planning in the context of clinical deterioration is warranted.
Implications for practice
Advance care planning is an ongoing process, sometimes involving multiple discussions to maximise efficacy, and should be introduced early in a hospital admission to patients at risk of serious deterioration or death. Evidence from the available literature indicated low prevalence of resuscitation orders and formal advance care planning documents, high short- and long-term mortality following clinical deterioration requiring RRT review and a proportion of patients who then require intensive care. Early discussion of goals of care, patient values and preferences as part of an advance care planning process has the potential to reduce the need for RRT intervention and may allow the redistribution of resources to patients whose deterioration is reversible.
Failure to provide care in line with a patient’s wishes as they approach may result in unnecessary burden for patients and families, poorer quality of life or increased suffering for patients, and the additional psychological pressures relating to caring for a family member suffering from reduced quality of life.53 Health services may also experience increased burden of care due to unwanted or even futile interventions that have both monetary implications, and psychological implications for staff caring for those patients.54
RRT reviews can be distressing for patients, carers and staff, and may preclude patients from being allowed a natural death. Factors such as effective communication and decision making, respectful and compassionate care, maintenance of self-identity and appropriate surroundings have been identified as important to patients and families.55 In contrast, patients, family members or caregivers may be required to make decisions in a crisis, where patient preferences and priorities for ongoing treatment may be unknown, and responses such as shock, grief, guilt and anxiety may impact clear decision making.56,57
For staff caring for patients at the end-of-life, establishing medical orders such as not for resuscitation or limitations of medical treatment that are clearly identifiable and easily accessed in the context of sudden deterioration are very important. However, they do not replace other aspect of advance care planning.58 Such orders may be less time-intensive and therefore complementary to the RRT.59 This may indicate that patients are afforded decision-making processes that are service-driven at the time of the review out of necessity, rather than patient-driven. Further research is required to define this issue.
Low rates of referral for palliative care management following RRT management may be due to a failure of the studies to capture this or could also be due to the fact that patients died despite all attempts. It may also reveal a lost opportunity to improve end-of-life care through specialist palliative care team management. Evaluation of palliative care referral could be a good outcome measure to assess for as part of patient outcomes measures. Further research examining the role of specialist palliative care services following sudden clinical deterioration is warranted.
Limitations and strengths
From a methodological point of view, this review has several limitations. It is possible some relevant references were not identified. Importantly, the studies were all quantitative and did not consider issues such as quality of life for patients or families. Some studies included small participant numbers and there was a range of hospital settings included, making it difficult to make conclusions about a specific health care setting. Inclusion of studies from a range of countries may influence the interpretation of the results due to policy influences or cultural factors impacting how deterioration, dying and death can be discussed in a clinical setting. Some studies limited their scope to specific disease types or a limited view of the patient journey within the acute care setting. Therefore, meta-analysis of results was not possible. No experimental or qualitative studies were identified, suggesting a gap in the current literature.
This systematic review considered literature published over a wide time frame and included studies that discussed aspects of advance care planning. It has identified several gaps in the literature and highlighted the need to enhance person-centred care to patients at the end-of-life. To our knowledge, it is the first systematic review to examine the provision of advance care planning in the context of sudden clinical deterioration requiring review by an RRT.
Conclusion
To support the growing evidence base, further research is required that seeks to better describe the provision of advance care planning in relation to clinical deterioration in hospital. This includes further research about decision making at the end-of-life, the availability of advance directives, establishment of goals of care, and how patient, families and other substitute decision makers are included in decisions. How RRT review impacts future care, including referral for specialist palliative care, is warranted. This may guide the development of strategies to improve end-of-life care planning, identify those patients who will or will not benefit from aggressive treatment15 and ensure services provided to patients at the end-of-life are timely and appropriate.
Footnotes
Conflict of interest statement: The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The authors received no financial support for the research, authorship and/or publication of this article.
Contributor Information
Wendy Pearse, Sunshine Coast Hospital and Health Service, Nambour, QLD, Australia School of Health and Sports Sciences, University of the Sunshine Coast, Maroochydore DC, QLD, Australia.
Florin Oprescu, School of Health and Sport Sciences, University of the Sunshine Coast, Maroochydore DC, QLD, Australia; Cluj School of Public Health, Babeş-Bolyai University, Cluj-Napoca, Romania.
John Endacott, Sunshine Coast Hospital and Health Service, Nambour, QLD, Australia.
Sarah Goodman, Sunshine Coast Hospital and Health Service, Nambour, QLD, Australia.
Mervyn Hyde, School of Education, University of the Sunshine Coast, Maroochydore DC, QLD, Australia.
Maureen O’Neill, School of Law, University of the Sunshine Coast, Maroochydore DC, QLD, Australia.
References
- 1. Scott IA, Mitchell GK, Reymond EJ, et al. Difficult but necessary conversations – the case for advance care planning. Med J Aust 2013; 199: 662–666. [DOI] [PubMed] [Google Scholar]
- 2. Luckett T, Bhattarai P, Phillips J, et al. Advance care planning in 21st century Australia: a systematic review and appraisal of online advance care directive templates against national framework criteria. Aust Health Rev 2015; 39: 552–560. [DOI] [PubMed] [Google Scholar]
- 3. Bischoff KE, Sudore R, Miao Y, et al. Advance care planning and the quality of end-of-life care in older adults. J Am Geriatr Soc 2013; 61: 209–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Scott IA, Rajakaruna N, Shah D, et al. Normalising advance care planning in a general medicine service of a tertiary hospital: an exploratory study. Aust Health Rev 2016; 40: 391–398. [DOI] [PubMed] [Google Scholar]
- 5. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 2008; 300: 1665–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sellars M, Silvester W, Masso M, et al. Advance care planning in palliative care: a national survey of health professionals and service managers. Aust Health Rev 2015; 39: 146–153. [DOI] [PubMed] [Google Scholar]
- 7. Detering KM, Hancock AD, Reade MC, et al. The impact of advance care planning on end of life care in elderly patients: randomised controlled trial. BMJ 2010; 340: c1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bernacki RE, Block SD. Communication about serious illness care goals: a review and synthesis of best practices. JAMA Int Med 2014; 174: 1994–2003. [DOI] [PubMed] [Google Scholar]
- 9. De Vleminck A, Houttekier D, Pardon K, et al. Barriers and facilitators for general practitioners to engage in advance care planning: a systematic review. Scand J Prim Health Care 2013; 31: 215–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chan PS, Jain R, Nallmothu BK, et al. Rapid response teams: a systematic review and meta-analysis. Arch Int Med 2010; 170: 18–26. [DOI] [PubMed] [Google Scholar]
- 11. Jones DA, Bagshaw SM, Barrett J, et al. The role of the Medical Emergency Team in end-of-life care: a multicenter, prospective, observational study. Crit Care Med 2012; 40: 98–103. [DOI] [PubMed] [Google Scholar]
- 12. DeVita MA, Bellomo R, Hillman K, et al. Findings of the first consensus conference on Medical Emergency Teams. Crit Care Med 2006; 34: 2463–2478. [DOI] [PubMed] [Google Scholar]
- 13. Smith RL, Hayashi VN, Lee YI, et al. The Medical Emergency Team call: a sentinel event that triggers goals of care discussion. Crit Care Med 2014; 42: 322–327. [DOI] [PubMed] [Google Scholar]
- 14. Medical Emergency Team End-of-Life Care investigators. The timing of rapid-response team activations: a multicentre international study. Crit Care Resusc 2013; 15: 15–20. [PubMed] [Google Scholar]
- 15. Jones D, Moran J, Winters B, et al. The rapid response system and end-of-life care. Curr Opin Crit Care 2013; 19: 616–623. [DOI] [PubMed] [Google Scholar]
- 16. Jones DA, McIntyre T, Baldwin I, et al. The Medical Emergency Team and end-of-life care: a pilot study. Crit Care Resusc 2007; 9: 151–156. [PubMed] [Google Scholar]
- 17. Knott CI, Psirides AJ, Young PJ, et al. A retrospective cohort study of the effect of Medical Emergency Teams on documentation of advance care directives. Crit Care Resusc 2011; 13: 167–174. [PubMed] [Google Scholar]
- 18. Orosz J, Bailey M, Bohensky M, et al. Deteriorating patients managed with end-of-life care following Medical Emergency Team calls. Int Med J 2014; 44: 246–254. [DOI] [PubMed] [Google Scholar]
- 19. Sulistio M, Franco M, Vo A, et al. Hospital rapid response team and patients with life-limiting illness: a multicentre retrospective cohort study. Palliat Med 2015; 29: 302–309. [DOI] [PubMed] [Google Scholar]
- 20. Chen J, Flabouris A, Bellomo R, et al. The Medical Emergency Team system and not-for-resuscitation orders: results from the MERIT study. Resuscitation 2008; 79: 391–397. [DOI] [PubMed] [Google Scholar]
- 21. Stelfox HT, Bagshaw SM, Gao S. A retrospective cohort study of age-based differences in the care of hospitalized patients with sudden clinical deterioration. J Crit Care 2015; 30: 1025–1031. [DOI] [PubMed] [Google Scholar]
- 22. Tan LH, Delaney A. Medical Emergency Teams and end-of-life care: a systematic review. Crit Care Resusc 2014; 16: 62–68. [PubMed] [Google Scholar]
- 23. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Austin CA, Hanzaker C, Stafford R, et al. Utilization of rapid response resources and outcomes in a comprehensive cancer center. Crit Care Med 2014; 42: 905–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Boniatti MM, Azzolini N, da Fonseca DL, et al. Prognostic value of the calling criteria in patients receiving a Medical Emergency Team review. Resuscitation 2010; 81: 667–670. [DOI] [PubMed] [Google Scholar]
- 26. Calzavacca P, Licari E, Tee A, et al. Features and outcome of patients receiving multiple Medical Emergency Team reviews. Resuscitation 2010; 81: 1509–1515. [DOI] [PubMed] [Google Scholar]
- 27. Calzavacca P, Licari E, Tee A, et al. The impact of rapid response system on delayed emergency team activation patient characteristics and outcomes: a follow-up study. Resuscitation 2010; 81: 31–35. [DOI] [PubMed] [Google Scholar]
- 28. Calzavacca P, Licari E, Tee A, et al. A prospective study of factors influencing the outcome of patients after a Medical Emergency Team review. Intens Care Med 2008; 34: 2112–2116. [DOI] [PubMed] [Google Scholar]
- 29. Cardona-Morrell M, Chapman A, Turner RM, et al. Pre-existing risk factors for in-hospital death among older patients could be used to initiate end-of-life discussions rather than rapid response system calls: a case-control study. Resuscitation 2016; 109: 76–80. [DOI] [PubMed] [Google Scholar]
- 30. Casamento AJ, Dunlop C, Jones DA, et al. Improving the documentation of Medical Emergency Team reviews. Crit Care Resusc 2008; 10: 24–29. [PubMed] [Google Scholar]
- 31. Dargin JM, Mackey CG, Lei Y, et al. Resource utilization and end-of-life care in a US hospital following Medical Emergency Team-implemented do not resuscitate orders. J Hosp Med 2014; 9: 372–378. [DOI] [PubMed] [Google Scholar]
- 32. Downar J, Rodin D, Barua R, et al. Rapid response teams, do not resuscitate orders, and potential opportunities to improve end-of-life care: a multicentre retrospective study. J Crit Care 2013; 28: 498–503. [DOI] [PubMed] [Google Scholar]
- 33. Gouda A, Alqahtani S. Do not resuscitate: an expanding role for critical care response team. Ind J Crit Care Med 2016; 20: 146–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Jäderling G, Bell M, Martling CR, et al. Limitations of medical treatment among patients attended by the rapid response team. Acta Anaesthesiol Scand 2013; 57: 1268–1274. [DOI] [PubMed] [Google Scholar]
- 35. Jäderling G, Calzavacca P, Bell M, et al. The deteriorating ward patient: a Swedish-Australian comparison. Intens Care Med 2011; 37: 1000–1005. [DOI] [PubMed] [Google Scholar]
- 36. O’Horo JC, Sevilla Berrios RA, Elmer JL, et al. The role of the primary care team in the rapid response system. J Crit Care 2015; 30: 353–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Parr MJA, Hadfield JH, Flabouris A, et al. The Medical Emergency Team: 12 month analysis of reasons for activation, immediate outcome and not-for-resuscitation orders. Resuscitation 2001; 50: 39–44. [DOI] [PubMed] [Google Scholar]
- 38. Psirides AJ, Hill J, Jones D. Rapid response team activation in New Zealand hospitals – a multicentre prospective observational study. Anaesth Intens Care 2016; 44: 391–397. [DOI] [PubMed] [Google Scholar]
- 39. Schneider A, Calzavacca P, Jones D, et al. Epidemiology and patient outcome after Medical Emergency Team calls triggered by atrial fibrillation. Resuscitation 2011; 82: 410–414. [DOI] [PubMed] [Google Scholar]
- 40. Silva R, Saraiva M, Cardoso T, et al. Medical Emergency Team: how do we play when we stay? Characterization of MET actions at the scene. Scand J Trauma Resusc Emerg Med 2016; 24: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Smith RJ, Santamaria JD, Reid DA, et al. The mortality associated with review by the rapid response team for non-arrest deterioration: a cohort study of acute hospital adult patients. Crit Care Resusc 2014; 16: 119–123. [PubMed] [Google Scholar]
- 42. Smith RJ, Santamaria JD, Faraone EE, et al. The duration of hospitalization before review by the rapid response team: a retrospective cohort study. J Crit Care 2015; 30: 692–697. [DOI] [PubMed] [Google Scholar]
- 43. Sundararajan K, Flabouris A, Keeshan A, et al. Documentation of limitation of medical therapy at the time of a rapid response team call. Aust Health Rev 2014; 38: 218–222. [DOI] [PubMed] [Google Scholar]
- 44. Tam B, Salib M, Fox-Robichaud A. The effect of rapid response teams on end-of-life care: a retrospective chart review. Can Respir J 2014; 21: 302–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Tirkkonen J, Olkkola KT, Tenhunen J, et al. Ethically justified treatment limitations in emergency situations. Eur J Emerg Med 2016; 23: 214–218. [DOI] [PubMed] [Google Scholar]
- 46. Tirkkonen J, Ylä-Mattila J, Olkkola KT, et al. Factors associated with delayed activation of Medical Emergency Team and excess mortality: an Utstein-style analysis. Resuscitation 2013; 84: 173–178. [DOI] [PubMed] [Google Scholar]
- 47. Visser P, Dwyer A, Moran J, et al. Medical emergency response in a sub-acute hospital: improving the model of care for deteriorating patients. Aust Health Rev 2014; 38: 169–176. [DOI] [PubMed] [Google Scholar]
- 48. White K, Scott IA, Bernard A, et al. Patient characteristics, interventions and outcomes of 1151 rapid response team activations in a tertiary hospital: a prospective study. Intern Med J 2016; 46: 1398–1406. [DOI] [PubMed] [Google Scholar]
- 49. Teno J, Lynn J, Wenger N, et al. Advance directives for seriously ill hospitalized patients: effectiveness with the patient self-determination act and the SUPPORT intervention. J Am Geriatr Soc 1997; 45: 500–507. [DOI] [PubMed] [Google Scholar]
- 50. ACSQHC. National consensus statement: essential elements for safe and high-quality end-of-life care. 2015. [Google Scholar]
- 51. Devita MA, Jones DA. Rapid response systems call: an indication for a palliative care assessment. Crit Care Med 2014; 42: 459–460. [DOI] [PubMed] [Google Scholar]
- 52. Mills A, Walker A, Levinson M, et al. Resuscitation orders in acute hospitals: a point prevalence study. Aust J Age 2017; 36: 32–37. [DOI] [PubMed] [Google Scholar]
- 53. Rabow MW, Hauser JM, Adams J. Supporting family caregivers at the end of life: ‘They don’t know what they don’t know’. J Am Med Assoc 2004; 291: 483–491. [DOI] [PubMed] [Google Scholar]
- 54. Badger JM. A descriptive study of coping strategies used by Medical Intensive Care Unit nurses during transitions from cure- to comfort-oriented care. Heart Lung 2005; 34: 63–68. [DOI] [PubMed] [Google Scholar]
- 55. Virdun C, Luckett T, Lorenz K, et al. Dying in the hospital setting: a meta-synthesis identifying the elements of end-of-life care that patients and their families describe as being important. Palliat Med 2017; 31: 587–601. [DOI] [PubMed] [Google Scholar]
- 56. Weissman DE. Decision making at a time of crisis near the end of life. JAMA 2004; 292: 1738–1743. [DOI] [PubMed] [Google Scholar]
- 57. Haley WE, Allen RS, Reynolds S, et al. Family issues in end-of-life decision making and end-of-life care. Am Behav Sci 2002; 46: 284–298. [Google Scholar]
- 58. Brimblecombe C, Crosbie D, Lim WK, et al. The goals of patient care project: implementing a proactive approach to patient-centred decision-making. Intern Med J 2014; 44: 961–966. [DOI] [PubMed] [Google Scholar]
- 59. Psirides A, Hill J, Hurford S. A review of rapid response team activation parameters in New Zealand hospitals. Resuscitation 2013; 84: 1040–1044. [DOI] [PubMed] [Google Scholar]


