Summary
In recent years, there has been massive progress in artificial intelligence (AI) with the development of deep neural networks, natural language processing, computer vision and robotics. These techniques are now actively being applied in healthcare with many of the health service activities currently being delivered by clinicians and administrators predicted to be taken over by AI in the coming years. However, there has also been exceptional hype about the abilities of AI with a mistaken notion that AI will replace human clinicians altogether. These perspectives are inaccurate, and if a balanced perspective of the limitations and promise of AI is taken, one can gauge which parts of the health system AI can be integrated to make a meaningful impact. The four main areas where AI would have the most influence would be: patient administration, clinical decision support, patient monitoring and healthcare interventions. This health system where AI plays a central role could be termed an AI-enabled or AI-augmented health system. In this article, we discuss how this system can be developed based on a realistic assessment of current AI technologies and predicted developments.
Keywords: Health service research, health policy, other public health
Introduction
Clinicians and health services are facing unprecedented pressure because of changing demographics, administrative requirements, workforce shortages and increasing morbidity as well as changes in information technology demand and expectations.1,2 In recent years, there has been major progress in artificial intelligence (AI) and its application in healthcare.3 In the coming years, these techniques are predicted to take over some of the activities currently being delivered by clinicians and healthcare administrators.4,5 However, there has also been an exceptional amount of inflation about the abilities of AI and even sometimes claims that AI will replace human clinicians altogether. These perspectives do not appear to reflect current limitations of AI systems.6,7 If one takes a balanced perspective of the limitations and promise of AI, one can gauge which parts of the healthcare industry are likely to feel significant impact of these technologies in the near future. Currently, there is little discussion in scientific literature or public policies as to how AI techniques can be incorporated in healthcare delivery. This article provides a high-level perspective on this topic.
What is AI?
While AI is one of the newest fields of engineering, the topic has been extensively researched formally since the 1950s.8 John McCarthy, one of the founding fathers of AI, defined it as ‘the science and engineering of making intelligent machines’.9 Alan Turing stated for a machine to be termed intelligent it would have to demonstrate behaviour indistinguishable from that of a human.10 With the advances in AI and its ability to emulate features of human intelligence such as reasoning and decision making, vision and language, knowledge representation, complex task processing and communication, some have suggested that AI is getting closer to passing the Turing test11 and even that AI will be the principal contributor to the fourth industrial revolution.12 In the past, there have been periods where the potential of AI was unable to be realised because of limitations in data, computing prowess and funding.13,14 However, the current period where there is access to enhanced computational power and volume of data coupled with increasing funding presents a more optimistic picture for the application of AI.15,16
Incorporating AI in healthcare delivery
The potential roles of AI techniques in healthcare delivery and medical research are becoming increasingly evident.17,18 Studies have highlighted the efficacy and potential of AI-enabled health applications. These technical developments are now being matched by significant investment in the application of AI in healthcare by governments and technology companies19,20 and the United States Food and Drug Administration is actively facilitating introduction of AI-enabled medical devices in the market.21 In our view, four areas where AI-enabled healthcare delivery is likely to have the most influence are: healthcare administration; clinical decision support; patient monitoring; and healthcare interventions.
Healthcare administration
The business of delivering healthcare has become complex with healthcare infrastructure in many countries being stretched to their capacity because of administrative burdens and resourcing constraints.22,23 Information technology tools have been demonstrated to alleviate this burden on health services and AI and data mining techniques have been identified as among the most promising approaches to support healthcare administration by augmenting clinical care and lessening administrative demands on clinicians.24 By undertaking repetitive and routine tasks like patient data entry and automated review of laboratory data and imaging results, AI can free time for clinicians to provide direct care for patients.25 Linking machine learning algorithms to electronic health records can help clinicians and administrators to retrieve accurate and context-relevant patient information.26 By using machine learning and concept-based information retrieval system, search accuracy and retrieval speed can be improved. However, at this stage, there are some issues like data and label availability, the explainability of the machine learning model and the ability to easily integrate such models with existing electronic health record systems that have yet to be addressed.27 New algorithmic approaches using transfer learning, contextual analysis, knowledge injection and knowledge distillation have been proposed to address these issues. Health services can also use optimised machine learning algorithms to support clinic scheduling and patient prioritisation thus reducing waiting times and more efficient use of services.28 AI techniques can help hospitals in predicting the length of stay of patients at the pre-admission stage, enabling more appropriate and efficient use of stretched hospital resources. Natural language processing applications that use voice-capture and transcription have been found effective in compiling electronic health record documentation and clinical note-taking leaving clinicians more time with patients.29
Clinical decision support
Clinical decision support systems are computer programs that draw upon clinical data and knowledge to support decisions made by healthcare professionals.30 Clinical decision support systems can help to reduce medical errors and increase healthcare consistency and efficiency and efforts to get clinical decision support systems into routine practice are increasing. AI techniques have been used in clinical decision support system research since the early 1970s, as in expert systems. Machine learning algorithms are now being used to predict the development of septic shock and aid diagnosis26 and treatment of chronic obstructive pulmonary disease patients and many other specialist decisions.31 They also have potential to help personalise treatment decisions for patients drawing upon large-scale data about previous cases that historically would have been difficult to make use of in clinical decision making. For example, a study identified how an AI framework employing sequential decision making could recommend alternate treatment paths, infer patient’s health status even when measurements were not available and refine treatment/management plans as new information was received.32
Artificial neural networks, an advanced form of machine learning, are now being trialled for medical diagnosis and appear to be capable of predicting and diagnosing medical conditions better than clinicians.33 Compared to traditional clinical decision support systems based on traditional software engineering, artificial neural networks are expected to have superior abilities in predicting many medical conditions such as cancer, cardiovascular disease and diabetes risk and artificial neural networks can be used for radiological and histopathological diagnosis. Studies have suggested that AI programs can at least match the performance of radiologists and pathologists18 and integration of deep learning into electronic health records may help in identify gaps in treatment protocols and reduce potential medical errors.34 Artificial neural networks can tolerate a certain amount of noise in the data but sometimes this can have an impact on the predictions.33 Therefore, it is important to combine the expertise and experience of clinicians with the discriminative power of the artificial neural networks.
Patient monitoring
The adoption of electronic health records and proliferation of smartphones and fitness monitoring devices has created unprecedented access to digital data and the potential to exploit AI techniques for monitoring patients.26 As a result, we have details on patients’ sleep patterns, blood pressure, heart rate and other measures in ways that we never had before. In addition to these advancements, we have had increases in other settings as well. For example, waveform pattern learning can improve monitoring and analysis of electrocardiographs, electroencephalographs, electromyographs and Doppler ultrasounds in hospitals.18 AI-enabled software can be used in intensive care units for cardiovascular and respiratory monitoring through the interpretation of vital signs. After a hospital visit, health services can use natural language processing-enabled virtual assistants to communicate appropriate health and medication information and schedule follow-up visits for patients.17 The use of such virtual health assistants has been found to increase medication compliance and reliable follow-up.35,36
Healthcare interventions
Emergence of AI has helped health interventions to be tailored for individuals or sub-groups of populations.26 Machine learning programs integrated with electronic health records can analyse biometric and other medical data of individual patients and recommend treatment plans based on current clinical guidelines.18 AI programs linked to hospital servers and capable of analysing recorded patient data and posing patient queries can reduce waiting times in stretched emergency departments.37 AI programs based on Fuzzy logic, a form of many-valued logic, can be used to administer medication. For example, fuzzy controllers have been used to administer vasodilators for postoperative patients.18
Significant developments in computer vision and robotics in recent years promise speedier and less expensive diagnostic and treatment services. Computer vision has been used for several years for automated analysis of 3D medical images,38 but it is also now being used to assess a patient’s condition through facial analysis.39 Elderly care presents the greatest opportunity for utilising robots in healthcare. Many older citizens live in the community but may have little support from family or carers which presents health risks. Robotic assistants have been found to fill some of the current gaps in the support of the elderly including reminding them about regular activities and guiding them through unfamiliar environments.40
| Panel 1: Application of AI techniques in Healthcare |
| Machine Learning/Deep Learning: Personalised Medicine, Patient record management and information Retrieval, Patient Monitoring, Drug Discovery, Infectious disease Surveillance |
| Natural Language Processing: Virtual Health Assistants, Note taking and transcription |
| Expert Systems: Knowledge based and non-knowledge based CDSS, Prediction, diagnosis and treatment of medical conditions |
| Computer Vision: Radiological and Histopathological image analysis |
| Robots: Elderly care, End of life care, Robotic Surgery, Emergency Medicine |
Other areas of application and future trends
This is by no means a comprehensive list of AI innovations in the four healthcare delivery areas we have focused on, but it already suggests many potential capabilities of AI to automate and improve healthcare delivery. AI applications can extend beyond these healthcare delivery areas. Machine learning has been used to accelerate drug development and its entry to the market.26 AI has been used for syndromic surveillance to spot emergence of disease outbreaks41 and to predict outcomes for critically ill and cancer patients.18 AI has been used to reduce and, in some instances, eliminate tests thus reducing costs for health services. Perhaps the greatest potential is in the use of Robotics. Different types of robots including mobile autonomous, industrial and educational robots are being used in the health system.42 Hence, considerable investment and research is occurring to develop humanoid robots because humans may feel less anxious in the presence of robots that look like humans.43 Development of realistic looking humanoid robots or computer-generated virtual health assistants may accelerate the incorporation of AI in healthcare. At this stage, surgical robots are driven by human surgeons and many are still only sophisticated manipulation device. However, there is much optimism about developments in the field of ‘autonomous surgery’ and it is not hard to foresee routine and minor surgeries led by robots in the future.44
Figure 1.
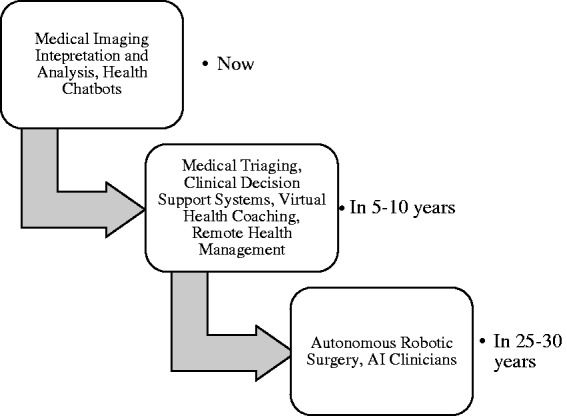
Maturity levels of application of AI in healthcare delivery.
Challenges
While the rapid progress and investment in AI and associated innovations have great promise for health services in alleviating resource and administrative challenges, the hyperbole is considerable and caution is needed. The full maturity of many AI applications is yet to be realised (see Figure I). Aside from the many technical limitations of current AI technologies45 in comparison with human vision, language processing and context-specific reasoning, other distinctive challenges exist in applying AI techniques in healthcare delivery.
First and foremost is the medico-legal context46 in which AI applications will be operated. Even within current medical regulation, lines of responsibilities are not always clear when medical errors occur, and it is even less clear where responsibilities should lie when AI ‘agents’ increasingly support or even autonomously deliver healthcare services.47 Determination of liability regarding the use of the system, the system and the user need further definition and clarification. This is an area in which regulatory and legal authorities must consult closely with a wide range of stakeholders in the health services as well as clinicians and software developers.
Governments across the world have increasingly adopted favourable positions in adoption of AI in various disciplines and activities.48,49 While some governments have actively involved themselves in the application of AI in healthcare, others have supported private developers in the development of relevant AI applications.19,50 As successes of AI in medicine become more evident,18,51 governments and funders may be required to formulate strategies outlining how AI gets applied in healthcare delivery and how this process will be funded.
Another concern is to ensure that people can understand how AI agents make clinical decisions and remain critically alert. Because of the complexity of deep learning and other sophisticated algorithms, some aspects of decision making may be opaque – this is often called the ‘black box’ problem.33 Clinicians must be closely involved in – and ideally lead – the development of AI services, scrutinise the data used to train the algorithms and retain a significant degree of responsibility over AI use.
An increasingly recognised issue is the potential for bias by the AI program towards certain population sub-groups if inappropriate sampling and training of the algorithms has occurred.52 Health services may also face resistance from their workforce in adopting AI programs, which will sometimes be mistaken but sometimes based on a deep understanding of patient care and service delivery. As difficulties emerge in adoption of electronic health records, change management methods that empower all stakeholders to participate must be adopted. Finally, access to context-specific patient data is critical for training and improving the accuracy of AI programs. Recent episodes have demonstrated major sensitivities with respect to health services sharing data with AI developers53,54 demonstrating a need to not only involve clinicians and policy specialists but also patient representatives in developing appropriate protocols to ensure acceptable service design and use of personal data.
Clinicians have traditionally been slow adopters of new technology relying on tried and trusted methods to deliver clinical care.55 Introduction of AI-enabled applications would no doubt encounter resistance even when the applications have progressed through relevant regulatory channels.7 It is important then for developers and authorities to have involved clinicians in the design and testing of these applications to not only create a sense of trust in the applications but also ensure these applications do not add work for clinicians.56 Also, important is the availability of a user-friendly interface and integration with existing health information technology systems.57,58
Conclusion
Rapid advances in AI research and the resources being provided by governments and industry make it highly likely that AI will be used extensively in healthcare delivery and there is huge potential for cost-saving as well as service quality improvement. However, questions remain as to how and how fast this development will and should occur. As well as ensuring that engineering practice and standards of evidence are of the highest quality before adoption takes place, ‘soft’ issues like fair and open access to data, medico-legal responsibilities in decision making and equitable distribution of benefits have to be addressed. As governments invest in the development and deployment of AI in healthcare, enthusiasm for promised changes needs to be matched by caution and careful planning.
Declarations
Competing Interests
None declared.
Funding
None declared.
Ethics approval
Not applicable.
Guarantor
SR.
Contributorship
SR conceived the idea and drafted the paper. All authors contributed to the paper and agreed with its final content.
Acknowledgements
None.
Provenance
Not commissioned; peer-reviewed by David Ellis.
References
- 1.Hurst J. Challenges for health systems in member countries of the Organisation for Economic Co-operation and Development. Bull World Heal Organ 2000; 78: 751–760. [PMC free article] [PubMed] [Google Scholar]
- 2.Innes G. Sorry—we’ re full! Access block and accountability failure in the health care system. CJE 2015; 17: 171–179. [DOI] [PubMed] [Google Scholar]
- 3.Gambhir S, Malik SK, Kumar Y. Role of soft computing approaches in healthcare domain: a mini review. J Med Syst 2016; 40: 1–20. See 10.1007/s10916-016-0651-x (last checked 8 November 2018). [DOI] [PubMed] [Google Scholar]
- 4.Topol E. The Patient Will See You Now: The Future of Medicine is in Your Hands, New York: Basic Books, 2015, pp. 364–364. [Google Scholar]
- 5.Diprose W, Buist N. Artificial intelligence in medicine: humans need not apply? N Z Med J 2016; 129: 73–76. [PubMed] [Google Scholar]
- 6.Chennu S. DeepMind: can we ever trust a machine to diagnose cancer? The Conversation 2017; See https://theconversation.com/deepmind-can-we-ever-trust-a-machine-to-diagnose-cancer-88707 (last checked 8 November 2018).
- 7.Coiera EW. Artificial intelligence in medicine: the challenges ahead. J Am Med Inf Assoc 1996; 3: 363–366. See http://www.ncbi.nlm.nih.gov/pubmed/8930853 (last checked 8 November 2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Russell S, Norvig P. Artificial Intelligence: A Modern Approach, 3rd ed Essex: Pearson Education Limited, 2016, pp. 1095–1095. [Google Scholar]
- 9.McCarthy J. What is artificial intelligence? See http://www-formal.stanford.edu/jmc/whatisai/ (last checked 3 June 2018).
- 10.Turing A. Computing machinery and intelligence. Mind 1950; 59: 433–460. [Google Scholar]
- 11.Baum SD, Goertzel B, Goertzel TG. How long until human-level AI? Results from an expert assessment. Technol Forecast Soc Change 2011; 78: 185–195. See 10.1016/j.techfore.2010.09.006 (last checked 8 November 2018). [DOI] [Google Scholar]
- 12.Monostori L. Cyber-physical production systems: roots, expectations and R&D challenges. Procedia CIRP 2014; 17: 9–13. See 10.1016/j.procir.2014.03.115 (last checked 8 November 2018). [DOI] [Google Scholar]
- 13.London AJ. Groundhog day for medical artificial intelligence. Hastings Cent Rep 2018; 48: 1002–1002. [DOI] [PubMed] [Google Scholar]
- 14.Hendler J. Avoiding another AI winter. IEEE Intell Syst 2008; 23: 2–4. [Google Scholar]
- 15.Poole DL, Mackworth AK. Artificial Intelligence: Foundations of Computational Agents, 1st edn Cambridge, UK: Cambridge University Press, 2010, pp. 653–653. [Google Scholar]
- 16.UK Govermment. Industrial Strategy Artificial Intelligence Sector Deal. See https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/702810/180425_BEIS_AI_Sector_Deal__4_.pdf (last checked 8 November 2018).
- 17.Agah A. Medical Applications of Artificial Intelligence. Agah A, ed. Boca Raton: CRC Press, 2017: 461.
- 18.Ramesh AN, Kambhampati C, Monson JRT, Drew PJ. Artificial intelligence in medicine. Ann R Coll Surg Engl 2004; 86: 334–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miliard M. AI funding tops $1 billion mark as mobile investments wane. Healthcare IT News. See http://www.healthcareitnews.com/news/health-it-funding-surpasses-7-billion-first-time-ai-and-analytics-biggest-winners (last checked 7 June 2018).
- 20.Minion L. Supercharged sector as the Federal Government backs $200 million Digital Health CRC. Healthcare IT News. See https://www.healthcareit.com.au/article/supercharged-sector-federal-government-backs-200-million-digital-health-crc (last checked 7 June 2018).
- 21.Tirrell M. FDA moves to encourage AI in medicine, drug development. CNBC News. See https://www.cnbc.com/2018/04/26/fda-moves-to-encourage-a-i-in-medicine-drug-development.html (last checked 7 June 2018).
- 22.AMA. Public hospitals stretched by rising demand. Australian Medicine. See https://ama.com.au/ausmed/public-hospitals-stretched-rising-demand (last checked 11 June 2018).
- 23.Wells J. Canadian Health System, like UK, “Stretched To Max Capacity”. American Council on Science and Health. See https://www.acsh.org/news/2017/08/28/canadian-health-system-uk-stretched-max-capacity-11753 (last checked 11 June 2018).
- 24.Snyder CF, Wu AW, Miller RS, Jensen RE, Bantug ET, Wolff AC. The role of informatics in promoting patient-centred care. Cancer J 2011; 17: 211–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Derrington D. Artificial intelligence for health and health care. See https://www.healthit.gov/sites/default/files/jsr-17-task-002_aiforhealthandhealthcare12122017.pdf (last checked 8 November 2018).
- 26.Saria S. A $3 trillion challenge to computational scientists: transforming healthcare delivery. IEEE Intell Syst 2014; 29: 82–87. [Google Scholar]
- 27.Xiao C, Choi E, Sun J. Opportunities and challenges in developing risk prediction models with electronic health records data: a systematic review. J Am Med Informatics Assoc 2018; 25: 1419–1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huang J, Jennings NR and Fox J. An agent-based approach to health care management. Appl Artif Intell 1995; 9: 401–420. See http://eprints.ecs.soton.ac.uk/2099/ (last checked 8 November 2018).
- 29.Leventhal R. How natural language processing is helping to revitalize physician. Healthcare Informatics 2017; October 2017: 8–13. [Google Scholar]
- 30.Musen MA. Biomedical Informatics. New York: Springer, 2006: 698–736. See http://link.springer.com/10.1007/0-387-36278-9 (last checked 8 November 2018).
- 31.Anakal S and Sandhya P. Clinical decision support system for chronic obstructive pulmonary disease using machine learning techniques. In: International Conference on Electrical, Electronics, Communication, Computer and Optimisation Techniques. 2017: 1–4. https://ieeexplore.ieee.org/document/8284601.
- 32.Indiana University. Can computers save health care? IU research shows lower costs, better outcomes. News Release. See http://newsinfo.iu.edu/news-archive/23795.html (last checked 11 June 2018).
- 33.Amato F, López A, Peña-Méndez EM, Vaňhara P, Hampl A, Havel J. Artificial neural networks in medical diagnosis. J Appl Biomed 2013; 11: 47–58. [Google Scholar]
- 34.Hernandez I, Tello J, Belda C, Ureña A, Salcedo I, Espinosa-Anke L, et al. Savana: re-using electronic health records with artificial intelligence. Int J Interact Multimed Artif Intell 2017; 1: 8–12. See http://www.ijimai.org/journal/node/1619 (last checked 8 November 2018).
- 35.Contreras I, Vehi J. Artificial intelligence for diabetes management and decision support: literature review. J Med Internet Res 2018; 20: e10775–e10775. See http://www.jmir.org/2018/5/e10775/ (last checked 8 November 2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chung K, Park RC. Chatbot-based heathcare service with a knowledge base for cloud computing. Cluster Comput 2018; 5: 1–13. See 10.1007/s10586-018-2334-5 (last checked 8 November 2018). [DOI] [Google Scholar]
- 37.Yousefi M, Yousefi M, Ferreira RPM, Kim JH, Fogliatto FS. Chaotic genetic algorithm and Adaboost ensemble metamodeling approach for optimum resource planning in emergency departments. Artif Intell Med 2018; 84: 23–33. See 10.1016/j.artmed.2017.10.002 (last checked 8 November 2018). [DOI] [PubMed] [Google Scholar]
- 38.Szeliski R. Computer Vision: Algorithms and Applications., 1st edn London: Springer-Verlag, 2011, pp. 812–812. [Google Scholar]
- 39.Thevenot J, López MB, Hadid A. A survey on computer vision for assistive medical diagnosis from faces. IEEE J Biomed Heal Informatics 2018; 1: 1479–1511. [DOI] [PubMed] [Google Scholar]
- 40.Pollack ME, Engberg S, Matthews JT, Dunbar-Jacob J, Mccarthy CE, Thrun S. Pearl: a mobile robotic assistant for the elderly. Architecture 2002; 2002: 85–91. See http://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:Pearl+:+A+Mobile+Robotic+Assistant+for+the+Elderly#0 (last checked 8 November 2018). [Google Scholar]
- 41.Chen HCH, Zeng D. AI for global disease surveillance. IEEE Intell Syst 2009; 24: 66–82. [Google Scholar]
- 42.Mathiason G, Cerilli J, Goodwin V. The transformation of the workplace through robotics, artificial intelligence, and automation. Littler Rep 2014. See http://shared.littler.com/tikit/2014/14_Robotics_Event_2-14/pdf/WP_Robotics_2-12-14_download.pdf (last checked 8 November 2018). [Google Scholar]
- 43.Ben-Ari M, Mondada F. Elements of robotics, Cham: Springer Nature, 2018, pp. 308–308. [Google Scholar]
- 44.Shademan A, Decker RS, Opfermann JD, Krieger A, Kim PCW, Leonard S. Supervised autonomous robotic soft tissue surgery. Sci Transl Med 2016; 8: 337–337. See http://ezproxy.deakin.edu.au/login?url=http://search.ebscohost.com/login.aspx?direct=true&db=edselc&AN=edselc.2-52.0-84969980426&site=eds-live&scope=site (last checked 8 November 2018). [DOI] [PubMed] [Google Scholar]
- 45.Taddy M. The technological elements of artificial intelligence. See http://www.nber.org/papers/w24301 (last checked 8 November 2018).
- 46.Marcus P. Book Review of Medical Malpractice Law: A Comparative Law Study of Civil Responsibility Arising from Medical Care, Williamsburg, VA: Faculty Publications, 1981, pp. 1138–1138. [Google Scholar]
- 47.Kingston J. Artificial Intelligence and Legal Liability. Research and Development in Intelligent Systems XXXIII, Cambridge, UK: Springer, Cham, 2016, pp. 269–279. [Google Scholar]
- 48.Pencheva I, Esteve M, Mikhaylov SJ. Big data and AI – a transformational shift for government: so, what next for research? Public Policy Adm 2018. Epub ahead of print: https://journals.sagepub.com/doi/full/10.1177/0952076718780537 . See https://journals.sagepub.com/doi/full/10.1177/0952076718780537 10.1177/0952076718780537. See https://doi.org/10.1177/0952076718780537 (last checked 8 November 2018). [DOI] [Google Scholar]
- 49.Nott G. Budget 2018: funding boost for AI and machine learning projects: the government is hoping to boost Australia’s artificial intelligence (AI) and machine learning capabilities with $29.9 million in funding over four years for projects that make use of the technologies. CIO 2018; 1 See: https://www.cio.com.au/article/640928/budget-2018-funding-boost-ai-machine-learning-projects/ (last checked 9 May 2018). [Google Scholar]
- 50.Jiang F, Jiang Y, Zhi H, Dong Y, Li H, Ma S, et al. Artificial intelligence in healthcare: past, present and future. Stroke Vasc Neurol 2017; 2: 230–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.The Lancet. Artificial intelligence in health care: within touching distance. Lancet 2017; 390: 2739. See 10.1016/S0140-6736(17)31540-4 (last checked 8 November 2018). [DOI] [PubMed]
- 52.Caliskan A, Bryson JJ, Narayanan A. Semantics derived automatically from language corpora contain human-like biases. Science 2017; 356: 183–186. [DOI] [PubMed] [Google Scholar]
- 53.Naughton J. Giving Google our private NHS data is simply illegal. The Guardian. See https://www.theguardian.com/commentisfree/2017/jul/09/giving-google-private-nhs-data-is-simply-illegal (last checked 12 June 2018).
- 54.Phillips K. Grindr says it will stop sharing users’ HIV data with third-party firms amid backlash. The Washington Post. See https://www.washingtonpost.com/news/to-your-health/wp/2018/04/03/grindr-says-it-will-stop-sharing-users-hiv-data-with-third-party-firms-amid-backlash/?noredirect=on&utm_term=.a40833550609 (last checked 3 April 2018).
- 55.Lapointe L, Rivard S. Getting physicians to accept new information technology: insights from case studies. CMAJ 2006; 174: 1573–1578. See https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1459884/ (last checked 8 November 2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Editors. Making sense of our digital medicine Babel. The Lancet. See http://patientsafetymovement (last checked 8 November 2018). [DOI] [PubMed]
- 57.Heston TF. Making health care smart. In: eHealth - Making Health Care Smarter. 1st edn. London: IntechOpen, 2018. See http://www.intechopen.com/books/ehealth-making-health-care-smarter/introductory-chapter-making-health-care-smart (last checked 8 November 2018).
- 58.Alscher MD and Schmidt N. The practice of medicine in the age of information technology. In: eHealth: Making Health Care Smarter . 1st edn. London: IntechOpen, 2018. See 10.5772/intechopen.75482 (last checked 8 November 2018). [DOI]


