Abstract
Introduction:
Posterior tibialis tendon insufficiency is the most common cause of adult acquired flatfoot deformity in elderly patients. We performed a literature search of primary and secondary journal articles pertaining to posterior tibialis tendon insufficiency in the geriatric population. We examined relevant data from these articles regarding current evaluation in addition to both conservative and advanced treatment approaches that correspond to disease severity.
Significance:
There is a paucity of literature to guide treatment of posterior tibialis tendon insufficiency in the elderly, and this condition may be more prevalent in geriatric patients than previously realized.
Results:
Posterior tibialis tendon insufficiency is an acquired defect that affects 10% of the geriatric population and disproportionately affects women. It is typically caused by degenerative changes. There are four primary stages of posterior tibialis tendon with subcategorizations that range from mild to severe. Conservative treatment with a variety of available ankle braces and non-steroidal anti-inflammatory medications are typically used to treat the first and second stage disease. Surgical repair is warranted for advanced second stage and above posterior tendon insufficiency. A variety of techniques have been proposed, and can include tendon transfer, hindfoot fusion, and even total ankle arthroplasty in extreme cases.
Conclusion:
Posterior tibialis tendon insufficiency causes marked discomfort and alters normal gait biomechanics. Elderly patients typically present with more severe manifestations of the disease. For patients requiring surgery, and especially geriatric patients, the ideal treatment is thought to be a procedure that is minimally invasive in order to maximize positive outcomes for elderly patients. More work is needed to examine clinical and radiographic outcomes of geriatric patients treated for posterior tibialis tendon insufficiency.
Keywords: foot and ankle surgery, fragility fractures, gait disorders, geriatric medicine, geriatric trauma
Introduction
Musculoskeletal decline and weakness is a common hallmark of aging.1 Associated age-related musculoskeletal impairments such as decreased connective tissue strength, increased bone turnover, and reduced cartilage ultimately contribute to increased joint laxity, weak bones, and arthritic changes that are seen with advanced age.2 Ultimately, these changes lead to impaired balance, increased pain, and reduced functionality. The foot and ankle region are particularly affected by these changes.
The posterior tibialis tendon terminates with plantar, main, and recurrent branches that insert into the second, third, and fourth metatarsals; navicular tuberosity and medial cuneiform; and sustentaculum tali of the calcaneus, respectively. It both stabilizes the medial longitudinal arch and inverts the midfoot. Posterior tibialis tendon insufficiency (PTTI) is a well-documented foot and ankle pathology and is the most common cause of acquired flatfoot deformity in the elderly patient.3 Although the exact etiology of PTTI remains unclear, it is postulated to be caused by degenerative changes (inflammation, attrition, and trauma) in the posterior tibialis tendon.3,4 Insufficient tendon structure results in the characteristic loss of arch known as “flat-foot” that is visible both radiographically and clinically.4
Posterior tibialis tendon insufficiency is present in up to 10% of the geriatric population and disproportionately affects women.3 The deformity itself is not necessarily debilitating. However, it causes a characteristic midfoot pain that may alter normal foot biomechanics, which, in turn, impairs functionality and use.5 The presence of pes planovalgus, one of the results of PTTI, has been correlated with other musculoskeletal complaints, such as anterior knee pain and low back pain.6 During a gait cycle in patients with PTTI, the everted state of the hindfoot, coupled with a flexible midfoot, increases biomechanical stress on the midfoot due to overload. As a result, abnormal articulation of the tibiotalar and calcaneonavicular joints leads to degeneration. This causes imbalance and gradual elongation of the posterior tibial tendon that affects its contraction leading to inevitable collapse of the medial longitudinal arch.5,7,8
Posterior tibialis tendon insufficiency is classified into 4 stages that are determined by radiographic and clinical evidence. The stages range from no gross anatomical changes to long-standing, rigid, hindfoot deformities.9 Given that PTTI commonly affects females in their mid-50s, some PTTI or associated sequelae could present with combined advanced degenerative midfoot and hindfoot arthritis with a rigid flatfoot deformity.
Management of PTTI includes both nonsurgical and surgical approaches that typically correspond with the stage of progression at time of diagnosis. Early diagnosis and treatment prevents progression of deformity, aggravation of pain, and typically leads to better functional outcomes. The purpose of this article is to review current management of PTTI in elderly patients based on the current body of literature.
Epidemiology and Disease Stage in Elderly Patients
Relatively little work has been done to identify the prevalence of PTTI in geriatric patients and the stage at which they most commonly present. Recent studies have suggested that PTTI occurs frequently but is underdiagnosed in the elderly population.3,10 One study conducted in 2009 surveyed 1000 women in England to determine the prevalence of PTTI in women older than 40 years. The authors identified a bimodal age distribution, with peaks in the fourth and eighth decades. Notably, this survey had high nonresponder rates among patients from both periods of peak disease prevalence. Nevertheless, the highest prevalence rates were among women aged 75 to 80 and 85 to 90 years (5.0% and 12.5%, respectively). In sum, these data suggest PTTI may be more prevalent among geriatric patients than previously recognized.10 It has been speculated that elderly individuals may be at a higher risk of sustaining more severe form of PTTI compared to the general population as a result of age-related decrease in muscle mass and bone density.10 However, to our knowledge, no epidemiological studies have been performed to determine whether or not geriatric patients are more likely to present with advanced-stage PTTI than their younger counterparts.
Characterization and Stages of PTTI
Patients with PTTI are often misdiagnosed, as the condition may mimic other foot and ankle pathologies such as midfoot arthritis and chronic ankle sprain.3 However, the diagnosis of PTTI can be made by identifying patients at risk of the disorder along with clinical signs of PTTI, in addition to utilizing imaging modalities such as X-ray and magnetic resonance imaging (Figure 1). Risk factors for the development of PTTI include congenital pes planus, obesity, previous medial ankle surgical procedures, and a history of steroid exposure.11-13 However, these risk factors were identified on limited data, and little recent work has been performed to affirm or negate these findings.
Figure 1.
Anteroposterior and lateral radiographs of stages I, II, III, and IV PTTI are shown. The progression from a mild deformity to a severe flattening of the medial arch is apparent. PTTI indicates posterior tibialis tendon insufficiency.
Initially, 3 stages of PTTI were proposed by Johnson and Strom.14 An additional fourth stage was added by Myerson (Table 1).15-17 Stage I is notable for inflammation and occasional swelling of the posterior tibialis tendon along with weakness of midfoot inversion, in the setting of flattened medial arch, but without a significant forefoot abduction or hindfoot valgus deformity. Stage II presents with passively correctable structural changes of the foot; the talonavicular joint can be inverted and the heel alignment can be neutralized with a passive maneuver. Stage II is subdivided into 2 classes based on the degree of deformity. Stage IIa describes a mild-to-moderate flexible deformity with less than 30% to 40% talar head uncoverage on the standing anteroposterior (AP) radiographs. Stage IIb shows a more pronounced deformity with more than 30% to 40% talar head uncoverage in the AP radiographs. Stage III represents a more advanced and fixed deformity characterized by a rigid midfoot abduction and hindfoot valgus, which are not passively correctable to a neutral or plantigrade position of the foot. Stage III is often accompanied by degenerative arthritis of the talonavicular, subtalar, and calcaneocuboid joints. Myerson added stage IV, which is characterized by valgus deformity of the tibiotalar joint secondary to the deltoid ligament insufficiency. Stage IVa describes flexible foot deformity, whereas stage IVb describes fixed foot deformity.14,16
Table 1.
Stages of PTTI Summarized by Deland.17
| Stage | Deformity | Surgical Treatment |
|---|---|---|
| I | No deformity from adult-acquired flatfoot deformity (may have preexisting flatfoot) | Tenosynovectomy, possible tendon transfer, and/or medial slide osteotomy |
| IIa | Mild/moderate flexible (minimal abduction through talonavicular joint, <30% talonavicular uncoverage) | Tendon transfer, medial slide osteotomy, possible Cotton procedure |
| IIb | Severe flexible deformity (abduction deformity through talonavicular joint, >30% talonavicular uncoverage) | Tendon transfer, medial slide osteotomy, and possible lateral column lengthening hindfoot fusion (subtalar or talonavicular and calcaneocuboid fusion) Cotton procedure or metatarsal–tarsal fusion performed as needed for elevation of the first ray |
| III | Fixed deformity (involving the triple-joint complex) | Hindfoot fusion, most commonly triple arthrodesis. Correction requires fusion of all 3 joints |
| IV | Foot deformity and ankle deformity (lateral talar tilt) | Complete resection of foot deformity, possible deltoid reconstruction. For severe arthritis, perform ankle fusion or total ankle arthroplasty, including correction of foot deformity |
| IVa | Flexible foot deformity | Foot deformity corrected as with stage IIb |
| IVb | Fixed foot deformity | Foot deformity corrected as with stage III |
Abbreviation: PTTI, posterior tibialis tendon insufficiency.
Nonsurgical Management of PTTI
Nonsurgical management is always indicated as the first line of treatment for all stages of PTTI and is likely to alleviate the majority of symptoms for most patients.17 These conservative measures are aimed at reducing inflammation (usually with nonsteroidal anti-inflammatory drugs [NSAIDs]) and stabilizing the foot to preserve function and avoid further deterioration of the tendon structure with an orthosis and physical therapy. In reducing inflammation, it is important to note that steroid injection is contraindicated as it may lead to tendon rupture.4,13,18 Immobilization with an ankle brace, such as a lace-up brace ankle stabilizing orthosis (ASO), an airsport brace, PTTD brace, or rigid stirrup brace to rest or relieve tension on the posterior tibial tendon is typically indicated for mild conditions (Figure 2). Although this type of brace offloads the inversion motion, it allows dorsi- and plantar flexion motion. If this first line of intervention is ineffective or if the inflammation is severe, a short period of immobilization with controlled ankle movement, walker boot, or a walking cast maybe tried to relieve the inflammation. Regarding immobilization, a period of 4 to 8 weeks is recommended as it allows for better pain management, structural preservation, increased activity, and stabilizing the ankle at a neutral position.17,19-22 Early diagnosis and intervention is critical as the use of orthotics has been shown to be successful in most patients.23,24
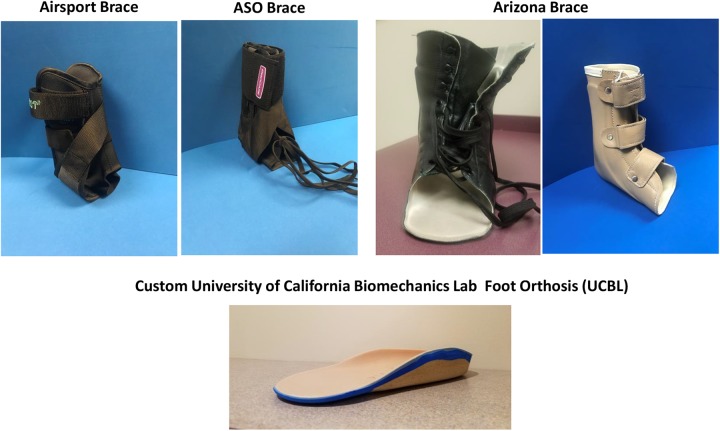
Figure 2.
A select variety of the bracing and orthotics options available for the treatment of PTTI is shown. PTTI indicates posterior tibialis tendon insufficiency.
In the elderly patients with a relatively mild deformity, a generic orthosis with medial arch support can provide substantial pain relief. A full-length orthosis with a soft inlay material, such as plastazote, is preferred over a partial-length device containing a hard arch support. The addition of a medial wedge is preferred when a flexible hindfoot valgus deformity is present. In more advanced stages of PTTI (greater than stage 2), custom University of California Biomechanics Lab foot orthosis orthotics and variations of ankle foot orthoses (AFOs), such as the Arizona brace, articulating AFO, or dynamic response ankle foot orthosis should be considered (Figure 1).22,24
While these recommendations are applicable to the majority of elderly patients with PTTI, there are some cases in which a patient will benefit to a significantly greater extent with a particular brace. In a study conducted by Chao et al, patients with fixed deformities and greater than 10° forefoot varus relative to a neutral calcaneal position benefit most from a molded articulating ankle foot orthosis (AFO).25,26 According to Alvarez et al, patients with PTTI who were both unable to perform a single heel raise and symptomatic for 3 months were improved with a short articulated AFO.27 Both authors report a 67% and 83% improvement in subjective and functional outcomes, respectively.25,27 The majority of patients who undergo conservative treatment with NSAIDs and orthotics are able to avoid surgery. Lin et al suggested that only 30% of nonsurgically managed patients with stage II PTTI needed surgery after a decade of treatment.28 In addition to use of brace and orthotics, physical therapy should be recommended to facilitate motion and activity. Patients who engage in physical therapy in addition to orthotics and/or bracing have been shown to have improved outcomes relative to those who exclusively used orthotics.24 Houck et al have suggested that higher intensity, supervised physical therapy may benefit patients more than a home-based exercise program.29 Despite these measures, elderly patients may face obstacles such as cognitive decline, financial instability, limited access to care, and insurance status that may play a role in poor compliance and ultimately disease progression that may warrant surgical intervention.30
Surgical Management of PTTI
There are several methods of surgically correcting PTTI, with varying recommendations depending on the stage at presentation. Surgery is more likely to be needed with advanced-stage PTTI.
Although stage I and early stage II can be corrected nonsurgically, some patients with these early stages of PTTI fail conservative management. No studies have been published examining whether elderly patients with early-stage PTTI are more likely to fail conservative management than their younger counterparts. With that said, the outcome profiles of surgical treatment for PTTI have generally been found to be quite favorable for young and elderly patients alike. One study found favorable outcomes in patients with stage I PTTI who failed a 3-month period of conservative treatment. These patients underwent tenosynovectomy, repair, and debridement, with 74% and 84% of patients reporting complete pain relief and return of function, respectively.31 In stage II PTTI, flexor digitorum longus (FDL) tendon transfer with medializing calcaneal osteotomy (MCO) yielded pain relief in 97% of patients, with 94% reporting improved functionality according to Myerson and Corrigan.32 A similar result was shown in a study in which patients received an MCO, lateral column lengthening, FDL transfer, and tendon Achilles lengthening, though there was no breakdown of outcomes by age.33 Moreover, one study found that patients older than 65 years with stage II PTTI had improvements in patient-reported outcomes that were not significantly different from those younger than 65. These patients also did not experience increased rates of revision surgeries relative to their younger counterparts.34
Other studies on long-term results of foot reconstruction for PTTI (3-5 years and 15 years of follow-up) showed maintenance of improved pain and function.35-37 Stages III and IV usually require more extensive surgical procedures such as a triple arthrodesis, although single (subtalar joint) or double (talonavicular and subtalar joints) arthrodesis are more common procedures.38,39 More extensive surgical treatment options, such as fusion of major joints, often correlates with poorer outcomes. Kitoaka et al showed that nearly half of arthrodesis patients have persisting pain.39
In elderly patients, surgery is associated with increased rates of complications, including prolonged healing, length of physiotherapy, and decreased activity levels. These are all factors that may lead to suboptimal outcomes when compared to younger populations.40,41 A thorough biopsychosocial assessment should be performed in the evaluation of any elderly patient considering surgery as a treatment option for PTTI. Thorough assessment of the geriatric patient’s activity level is vital in determining the need for surgical intervention. If one is living a relatively sedentary lifestyle, risk and benefit of the surgical intervention and the patient’s expectations should be thoroughly discussed prior to undertaking an extensive surgical treatment. In most patients with advanced stage PTTI, a selective arthrodesis of the painful joint is likely to produce more reliable clinical result than an extensive, joint-sparing reconstruction procedure (Figure 3). At present, we are not aware of any clinical study that has used patient-reported outcomes, revision rates, complication rates, or radiographic markers to compare different surgical treatment options for flatfoot reconstruction in elderly patients. This will be an area of future research.
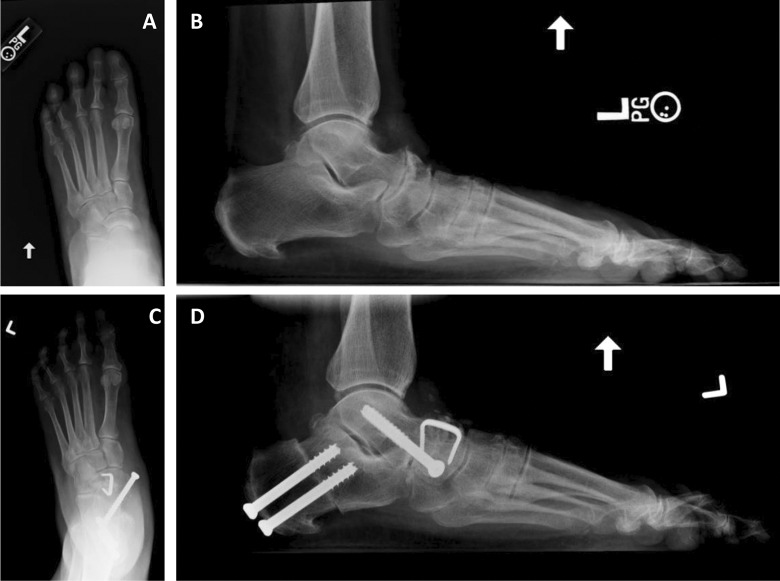
Figure 3.
Pre- and postoperative radiographs of a 73-year-old female who presented with a rigid flatfoot deformity and painful degenerative arthritis of the talonavicular joint (stage 3 PTTI). Intraoperatively, a tear of the posterior tibialis tendon was noted. Left foot Achilles tendon lengthening, talonavicular joint arthrodesis, and medializing calcaneal osteotomy were performed, with improvement in the patient’s deformity and clinical status. PTTI indicates posterior tibialis tendon insufficiency.
Conclusion
Although PTTI is generally believed to be most prevalent in middle-aged women, there is some preliminary data that suggest it may be more common in the elderly population than previously thought. In elderly patients, frailty and weakness that accompany advanced age can make it particularly difficult to maintain balance in the setting of compromised gait mechanics. Posterior tibialis tendon insufficiency, as with many foot-and-ankle pathologies, requires careful management and follow-up in elderly patients to preserve function and avoid potential debilitating sequela.
Nonsurgical management of PTTI can result in favorable outcomes despite the expected late presentation of the pathology in elderly patients. For those who require surgical intervention to correct foot deformity secondary to PTTI, an approach that minimizes surgical disruption and revision surgeries is felt to be ideal, but there remains a paucity of evidence regarding the optimal surgical approach. Given the prevalence of this condition and the impact of the associated declines in mobility with age, more research is needed to characterize the demographic characteristics of patients with PTTI, to better understand the progression or lack thereof of the disease, and to determine appropriate treatment paradigms for geriatric patients.
Footnotes
Authors’ Note: J.B. and T.I. contributed to data analysis and manuscript writing. R.C. and I.O. contributed to study design, data analysis, and manuscript writing.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: James D. Brodell Jr.  http://orcid.org/0000-0001-6969-781X
http://orcid.org/0000-0001-6969-781X
References
- 1. Ikpeze TC, Elfar JC. The geriatric driver. Geriatr Orthop Surg Rehabil. 2016;7(2):106–109. doi:10.1177/2151458516644818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lotz M, Loesser R. Effects of aging on articular cartilage homeostasis. Bone. 2012;51(2):241–248. doi:10.1016/j.immuni.2010.12.017.Two-stage. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kohls-Gatzoulis J, Angel J, Singh D. Tibialis posterior dysfunction as a cause of flatfeet in elderly patients. Foot. 2004;14(4):207–209. doi:10.1016/j.foot.2004.06.003. [Google Scholar]
- 4. Myerson M. Adult aquired flat foot deformity. J Bone Joint Surg. 1996;78A:780–792. [Google Scholar]
- 5. Mann R. Aquired flatfoot in adults. Clin Orthop Relat Res. 1983;181:46–51. [PubMed] [Google Scholar]
- 6. Kosashvili Y, Fridman T, Backstein D, Safir O, Bar Ziv Y. The correlation between pes planus and anterior knee or intermittent low back pain. Foot Ankle Int. 2008;29(8):910–913. doi:10.3113/FAI.2008.0910. [DOI] [PubMed] [Google Scholar]
- 7. Richie DH. Biomechanics and clinical analysis of the adult acquired flatfoot. Clin Podiatr Med Surg. 2007;24(4):617–644. doi:10.1016/j.cpm.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 8. Funk D, Cass J, Johnson K. Acquired adult flat foot secondary to posterior tibial-tendon pathology. J Bone Joint Surg. 1986;68(1):95–102. [PubMed] [Google Scholar]
- 9. Beals TC, Pomeroy GC, Manoli A. Posterior tibial tendon insufficiency: diagnosis and treatment. J Am Acad Orthop Surg. 1999;7(2):112–118. [DOI] [PubMed] [Google Scholar]
- 10. Kohls-Gatzoulis J, Woods B, Angel JC, Singh D. The prevalence of symptomatic posterior tibialis tendon dysfunction in women over the age of 40 in England. Foot Ankle Surg. 2009;15(2):75–81. doi:10.1016/j.fas.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 11. Kohls-Gatzoulis JA, Singh D, Angel JC. Tibialis posterior insufficiency occurring in a patient without peronei: a mechanical etiology. Foot Ankle Int. 2001;22(12):950–952. doi:10.1177/107110070102201203. [DOI] [PubMed] [Google Scholar]
- 12. Mann R, Thompson F. Rupture of the posterior tibial tendon causing flat foot. J Bone Joint Surg. 1985;67A:556–561. [PubMed] [Google Scholar]
- 13. Holmes GJ, Mann R. Possible epidemiological factors associated with rupture of the posterior tibial tendon. Foot Ankle. 1992;13(2):70–79. [DOI] [PubMed] [Google Scholar]
- 14. Johnson K, Strom D. Tibialis posterior tendon dysfunction. Clin Orthop Relat Res. 1989;(239):196–206. [PubMed] [Google Scholar]
- 15. Guelfi M, Pantalone A, Mirapeix RM, Vanni D. Anatomy, pathophysiology and classification of posterior tibial tendon dysfunction. Eur Rev Med Pharmacol Sci. 2017;21:13–19. http://www.europeanreview.org/article/12022. [PubMed] [Google Scholar]
- 16. Bluman EM, Title CI, Myerson MS. Posterior tibial tendon rupture: a refined classification system. Foot Ankle Clin. 2007;12(2):233–249. doi:10.1016/j.fcl.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 17. Deland JT. Adult-acquired flatfoot deformity. J Am Acad Orthop Surg. 2008;16(7):399–406. doi:10.1016/j.cpm.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 18. Rees JD, Wilson AM, Wolman RL. Current concepts in the management of tendon disorders. Rheumatology. 2006;45(5):508–521. doi:10.1093/rheumatology/kel046. [DOI] [PubMed] [Google Scholar]
- 19. Marzano R. Functional bracing of the adult acquired flatfoot. Clin Podiatr Med Surg. 2007;24(4):645–656. doi:10.1016/j.cpm.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 20. Steb H, Marzano R. Conservative management of posterior tibial tendon dysfunction, subtalar joint complex, and pes planus deformity. Clin Pod Med Surg. 1999;16(3):439–451. [PubMed] [Google Scholar]
- 21. Sferra J, Rosenberg G. Nonoperative treatment of posterior tibial tendon pathology. Foot Ankle Clin. 1997;(2):261–273. [Google Scholar]
- 22. Bowring B, Chockalingam N. Conservative treatment of tibialis posterior tendon dysfunction – a review. Foot. 2010;20(1):18–26. doi:10.1016/j.foot.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 23. Augustin J, Lin S, Berberian W, Johnson J. Nonoperative treatment of adult acquired flat foot with the Arizona brace. Foot Ankle Clin. 2003;8(3):491–502. [DOI] [PubMed] [Google Scholar]
- 24. Kulig K, Reischl SF, Pomrantz AB, et al. Nonsurgical management of posterior tibial tendon dysfunction with orthoses and resistive excercise: a randomized controlled trial. Phys Ther. 2009;89(1):26–37. [DOI] [PubMed] [Google Scholar]
- 25. Chao W, Wapner K, Lee T, Adams J, Hecht P. . nonoperative management of posterior tibial tendon dysfunction. Foot Ankle Int. 1996;17(12):736–741. [DOI] [PubMed] [Google Scholar]
- 26. Wapner K, Chao W. Nonoperative treatment of posterior tibial tendon dysfunction. Clin Orthop Relat Res. 1999;(365):39–45. [DOI] [PubMed] [Google Scholar]
- 27. Alvarez RG, Marini A, Schmitt C, Saltzman CL. Stage I and II posterior tibial tendon dysfunction treated by a structured nonoperative management protocol: an orthosis and exercise program. Foot Ankle Int. 2006;27(1):2–8. doi:10.1177/107110070602700102. [DOI] [PubMed] [Google Scholar]
- 28. Lin JL, Balbas J, Richardson EG. Results of non-surgical treatment of stage II posterior tibial tendon dysfunction: a 7- to 10-year followup. Foot Ankle Int. 2008;29(8):781–786. doi:10.3113/FAI.2008.0781. [DOI] [PubMed] [Google Scholar]
- 29. Houck J, Neville C, Tome J, Flemister A. Randomized controlled trial comparing orthosis augmented by either stretching or stretching and strengthening for stage II tibialis posterior tendon dysfunction. Foot Ankle Int. 2015;36(9):1006–1016. doi:10.1177/1071100715579906. [DOI] [PubMed] [Google Scholar]
- 30. Ikpeze TC, Omar A, Elfar JH. Evaluating problems with footwear in the geriatric population. Geriatr Orthop Surg Rehabil. 2015;6(4):338–340. doi:10.1177/2151458515608672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Teasdall R, Johnson K. Surgical treatment of stage I posterior tibial tendon dysfunction. Foot Ankle Int. 1994;15(12):646–648. [DOI] [PubMed] [Google Scholar]
- 32. Myerson M, Corrigan J. Treatment of posterior tibial tendon dysfuncton with flexor digitorum longus tendon trasfer and calcaneoal osteotomy. Orthopedics. 1996;19(5):383–388. [DOI] [PubMed] [Google Scholar]
- 33. Silva MGAN, Tan SHS, Chong HC, Su HCD, Singh IR. Results of operative correction of grade IIB tibialis posterior tendon dysfunction. Foot Ankle Int. 2015;36(2):165–171. doi:10.1177/1071100714556758. [DOI] [PubMed] [Google Scholar]
- 34. Conti MS, Jones MT, Savenkov O, Deland JT, Ellis SJ. Outcomes of reconstruction of the stage II adult-acquired flatfoot deformity in older patients. Foot Ankle Int. 2018;39(9):1019–1027. doi:10.1177/1071100718777459. [DOI] [PubMed] [Google Scholar]
- 35. Wacker J, Hennessey M, Saxby T. Calcaneal osteotomy and transfer of the tendon of flexor digitorum longus for state II dysfunction of tibialis posterior. three- to five-year results. J Bone Jt Surg. 2002;84(1):54–58. [DOI] [PubMed] [Google Scholar]
- 36. Fayazi AH, Nguyen H-V, Juliano PJ. Intermediate term follow-up of calcaneal osteotomy and flexor digitorum longus transfer for treatment of posterior tibial tendon dysfunction. Foot Ankle Int. 2002;23(12):1107–1111. doi:10.1177/107110070202301205. [DOI] [PubMed] [Google Scholar]
- 37. Chadwick C, Whitehouse SL, Saxby TS. Long-term follow-up of flexor digitorum longus transfer and calcaneal osteotomy for stage II posterior tibial tendon dysfunction. Bone Joint J. 2015;97-B(3):346–352. doi:10.1302/0301-620X.97B3.34386. [DOI] [PubMed] [Google Scholar]
- 38. Laughlin T, Payette C. Triple arthrodesis and subtalar joint arthrodesis for the treatment of end-stage posterior tibial tendon dysfunction. Clin Pod Med Surg. 1999;16(3):527–555. [PubMed] [Google Scholar]
- 39. Kitoaka H, Patzer G. Subtalar arthrodesis for posterior tibial tendon dysfunction and pes planus. Clin Orthop Relat Res. 1997;(345):187–194. [PubMed] [Google Scholar]
- 40. Hamel M, Henderson W, Khuri S, Daley J. Surgical outcomes for patients aged 80 and older: morbidity and mortality from major noncardiac surgery. J Am Geriatr Soc. 2005;53(3):424–429. doi:10.1111/j.1532-5415.2005.53159.x. [DOI] [PubMed] [Google Scholar]
- 41. Turrentine FE, Wang H, Simpson VB, Jones RS. Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg. 2006;203(6):865–877. doi:10.1016/j.jamcollsurg.2006.08.026. [DOI] [PubMed] [Google Scholar]