Abstract
Background
There is no consensus on the most suitable treatment for tennis elbow but, in the USA, surgical intervention is increasing despite a lack of supportive research evidence. The aim of this systematic review was to provide a balanced update based on all relevant published randomized controlled trials conducted to date.
Methods
An electronic search of MEDLINE, EMBASE, CINAHL, BNI, AMED, PsycINFO, HBE, HMIC, PubMed, TRIP, Dynamed Plus and The Cochrane Library was complemented by hand searching. Risk of bias was assessed using the Cochrane Risk of Bias Tool and data were synthesized narratively, based on levels of evidence, as a result of heterogeneity.
Results
Twelve studies of poor methodological quality were included. The available data suggest that surgical interventions for tennis elbow are no more effective than nonsurgical and sham interventions. Surgical technique modifications may enhance effectiveness compared to traditional methods but have not been tested against a placebo.
Conclusions
Current research evidence suggests that surgery for tennis elbow is no more effective than nonsurgical treatment based on evidence with significant methodological limitations. Given the recalcitrant nature of tennis elbow for some patients, further research in the form of a high-quality placebo-controlled surgical trial with an additional conservative arm is required to usefully inform clinical practice.
Keywords: elbow, surgery, systematic review, tennis
Introduction
Tennis elbow is the most common cause of lateral elbow pain and has been reported to have a point prevalence of 1% to 3%.1 Tennis elbow is characterized by pain near the lateral epicondyle that is aggravated by contraction of the extensor muscles, particularly when gripping an object. It commonly affects adults of working age and can affect the individual’s ability to work and engage with other activities, including sport.2,3 A study of worker’s compensation claims in Washington State between 1990 and 1998 found the average work sickness absence for elbow epicondylitis of 219 days with an average claim cost of 8099 US dollars.4 There is currently no established consensus on the most appropriate form of treatment for this condition although a treatment algorithm has been proposed but has not yet been evaluated.5 Many treatment options are available ranging from conservative measures, such as physiotherapy, in the form exercise, manual therapy and strapping; injections of various substances, including corticosteroids and platelet-rich plasma; and surgical debridement. Evidence suggests that, although corticosteroid injections might offer short-term pain relief, in the long term, they lead to worse outcome than a wait-and-see approach and also negate the beneficial effects of therapeutic exercise treatments.5
Given the recalcitrant nature of tennis elbow for some patients, surgical intervention might be offered to this group. An increasing trend towards surgery is apparent in the USA with a rise in the proportion of patients with tennis elbow undergoing surgery from 1.1% in 2000 to 2002 to 3.2% in 2009 to 2011 at the Mayo Clinic (Rochester, MN, USA).6 Buchbinder et al.7 conducted a systematic review of surgery for lateral elbow pain (that included tennis elbow) in 2002 and updated their review in 2011.8 The conclusions from both reviews were similar, describing the lack of evidence to support or refute surgery for this condition. In particular there was a lack of high quality randomized controlled trials (RCTs) and specifically none that compared surgery to a placebo intervention. Given the rising incidence of this surgery in the USA and in light of the findings of previous systematic reviews, the aim of this current systematic review was to provide updated guidance based on all relevant published RCTs to date.
Materials and methods
A systematic review was conducted using a predetermined protocol registered on the PROSPERO database of systematic reviews (accessible via http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42016050849) in accordance with the PRISMA-P statement.9
Search strategy
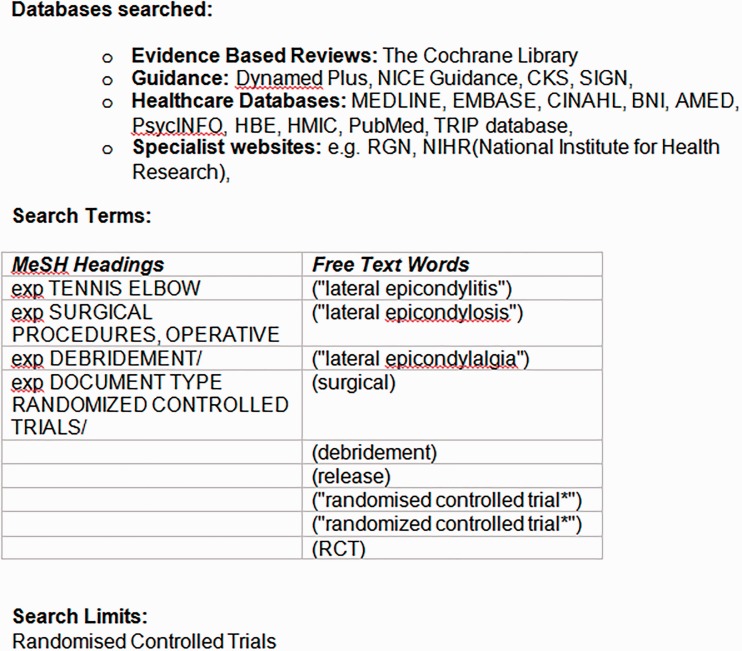
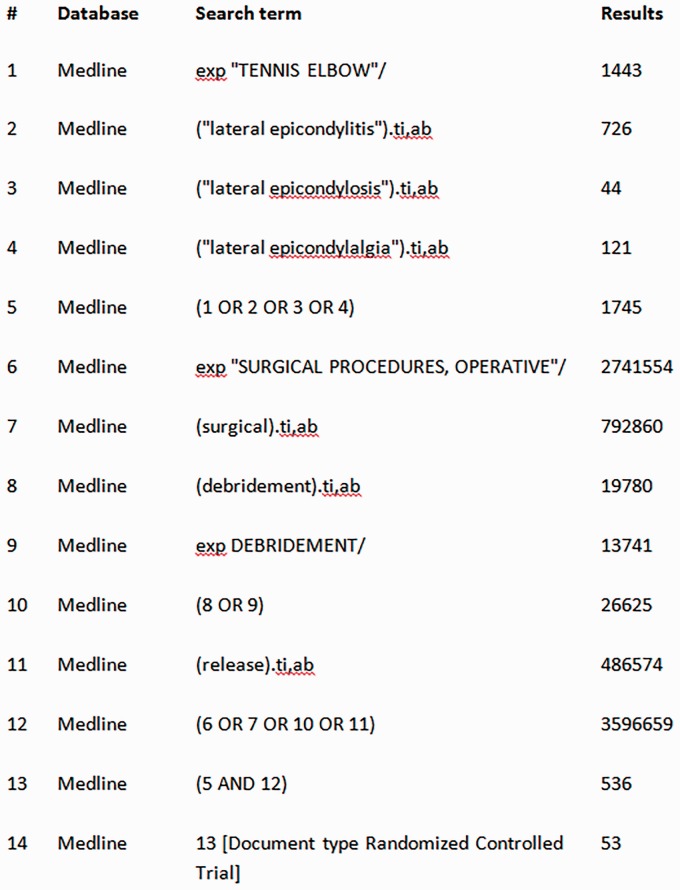
An electronic search of MEDLINE, EMBASE, CINAHL, BNI, AMED, PsycINFO, HBE, HMIC, PubMed, TRIP database, The Cochrane Library, Dynamed Plus, NICE Guidance, CKS, SIGN and Specialist websites, including RGN and NIHR (National Institute for Health Research), was conducted by a medical librarian (BR) on 8 and 9 March 2017 using search terms shown in Fig. 1. An example search of the MEDLINE database is shown in Fig. 2. The database searches were supplemented by hand searches of abstracts presented at the British Elbow & Shoulder Society Annual Scientific Meeting 2016 because these had yet to be published in the Shoulder & Elbow and therefore remained to be indexed on PubMed.
Figure 1.
Search Strategy
Figure 2.
Example search strategy using Medline
Two reviewers (MB and CL) then independently screened titles and abstract before selecting full-text papers, where available, based on pre-defined inclusion criteria:
Adults diagnosed with tennis elbow
Any form of surgical intervention
Any form of comparator treatment including other forms of surgery, injections, physiotherapy, sham surgery or wait-and-see
Randomized controlled trials only
English language
Primary outcomes: Patient-reported outcome measures of pain and function
Secondary outcomes: Return to work, return to sport
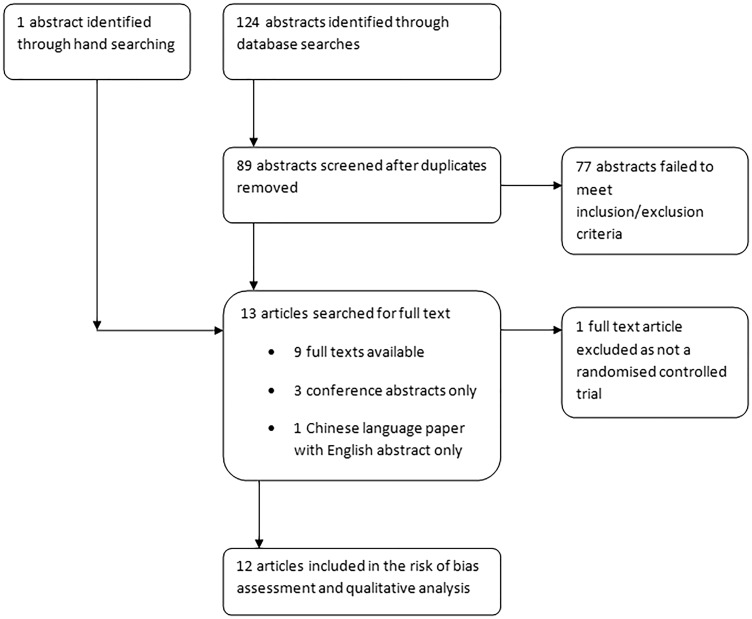
A third reviewer (AT) was available for arbitration in the event of disagreement but was not required. The study selection process is detailed in Fig. 3.
Figure 3.
Study selection flowchart
Data extraction
One reviewer (MB) extracted data in relation to study characteristics, participant characteristics, interventions and results before a second reviewer (CL) independently verified the findings. The extracted data are presented in Table 1.
Table 1.
Data extraction table
| Study characteristics | Participant characteristics | Interventions | Results |
|---|---|---|---|
| Dunkow et al.24 RCT comparing open Nirschl release23 versus percutaneous tenotomy Conducted in the UK | 45 patients (47 elbows) Age range 30 years to 58 years 22 male, 25 female Failed 12 months of conservative treatment including two 80-mg hydrocortisone injections | Open Nirschl release21 with three drill holes into the lateral epicondyle (n = 24) Percutaneous (1-cm incision) division of the common extensor origin (n = 23) Standardized physiotherapy for both groups postoperatively | 12-month follow-up: Significant improvements in Disability of Arm Shoulder Hand (DASH) score (p = 0.001) in both groups Patient satisfaction in favour of percutaneous group (p = 0.012) Median return to work 5 weeks in open group, 2 weeks in percutaneous group; p = 0.0001 in favour of percutaneous group |
| Keizer et al.15 RCT pilot study comparing botulinum toxin (botox) injection versus open release (Hohmann method30) Conducted in The Netherlands | 40 patients Mean age 42.8 years (25 years to 72 years) 19 male, 21 female Mean duration of symptoms 10.5 months with minimum of 6 months Failed conservative treatment 36 patients had previous steroid injections | 30 units to 40 units of botox injected into the extensor carpi radialis brevis (ECRB) (n = 20). Eight patients given a second injection as a result of a limited effect Hohmann technique of open release30 of ECRB (n = 20) followed by sling for 2 weeks | Outcomes measured by modified Verhaar score.31 Four patients in the botox group underwent open surgery as a result of a failed response Outcomes for these patients at 24 months were 1 good, 1 fair, 2 poor Main results at 24 months: Botox: 11/16 excellent result, 4/16 good, 1/16 fair Open surgery: 14/20 excellent result, 3/20 good, 3/20 poor Overall no significant differences reported in pain or range of motion at 3 months, 6 months, 12 months or 24 months Sick leave in favour of surgery group at 3 months (p = 0.01) but no difference at 6 months, 12 months or 24 months |
| Khashaba22 RCT comparing Nirschl technique of open release23 with or without drilling the bone of the anterolateral humeral condyle Conducted in the UK | 18 patients (23 elbows) Aged over 18 years Failed to improve with rest and physiotherapy Temporary (< 6 months) response to steroid injection 40 mg of depomedrone | Nirschl open release21 including three drill holes into the lateral epicondyle (n = 9 patients but number of elbows not stated) Nirschl open release21 without the drilling component (n = 9 but number of elbows not stated) | Mean wrist extension power improvement using AK-7000 extensionometer at 6 months: drilled 5.2 kg, nondrilled 6.5 kg Mean improvement in pain Visual Analogue Scale (VAS) 3 months to 6 months: drilled 4.6 cm, nondrilled 6.8 cm |
| Kroslak & Murrell16 RCT comparing open Nirschl release23 versus sham surgery (skin incision only) Conducted in Australia Conference abstract only | 26 patients Groups matched for age, sex, hand dominance, duration of symptoms Chronic tennis elbow for minimum 6 months Failed two nonsurgical modalities | Nirschl open release21 (n = 13) Sham surgery involving skin excision and exposure to level of ECRB tendon (n = 13) | Both groups improved subjective outcomes at 6 months and 12 months (p < 0.01). Both groups improved tenderness, pronation/supination range, grip strength and Orthopaedic Research Institute-Tennis Elbow Testingc System (ORI-TETS) score32 at 6 months (p < 0.05) No differences between groups in any measure at any time point Study stopped early as a result of a lack of difference between groups |
| Leiter et al.19 RCT comparing open versus arthroscopic release Conducted in Canada Conference abstract only | 71 patients Aged over 16 years Open group: mean age 47.1 years; 19 male, 15 female Arthroscopic group: mean age 45 years; 21 male, 13 female Failed to improve with 6 months conservative treatment | Open tennis elbow release (n = 34) Arthroscopic tennis elbow release (n = 34) ? Some individuals had bilateral surgery as a result of a discrepancy in total number of patients | No difference in pain VAS, DASH score or grip power between groups at any time point up to 12 months 17/34 met the minimally clinically important difference (MCID) in DASH score in the open group and 19/34 in the arthroscopic group |
| Leppilahti et al.25 RCT comparing open posterior interosseous nerve decompression versus open extensor carpi radialis brevis tenotomy Conducted in Finland | 26 patients (28 elbows) Nerve group: mean age 42 years (33 years to 50 years); 6 male, 7 female Tenotomy group: mean age 41 years (30 years to 52 years); 7 male, 7 female Mean symptom duration 23 months (5 months to 60 months) Failed conservative care including physiotherapy and mean number of steroid injections 4.5 | Open decompression of the posterior interosseous nerve (n = 14) Open z-shaped tenotomy of the ECRB (n = 14) | Mean follow-up 31 months (22 months to 48 months). No significant difference in grip strength between groups Subjective pain relief: Nerve group: 3 excellent, 4 good, 2 fair, 5 poor. Tenotomy group: 2 excellent, 4 good, 5 fair, 3 poor Patients undergoing repeat surgery as a result of poor outcome: nerve group 4, tenotomy group 3 |
| Meknas et al.14 RCT comparing radiofrequency microtenotomy versus open surgical release and repair Conducted in Norway | 24 patients 13 male, 11 female Open surgery: mean age 49.2 years (36 years to 62 years). Mean symptom duration 27.6 months Microtenotomy: mean age 46.7 years (30 years to 64 years). Mean symptom duration 22 months All patients had minimum symptoms 12 months with failed conservative treatment including 3 months of physiotherapy and at least three steroid injections | Open surgical release using modified Nirschl technique 21 (n = 11) Open 3-cm exposure of extensor tendon with microtenotomy using a radiofrequency device to a depth of 3 mm to 5 mm in three to six areas (n = 13) | No difference in pain VAS between groups at 3 weeks, 6 weeks, 12 weeks or 10 months to 18 months Both groups had significant pain reduction from 6 weeks onward (p < 0.04 open, p < 0.001 microtenotomy) 23/24 patients had reduced pain at 10 months to 18 months (p < 0.05) No difference in grip strength between groups at 12 weeks and no difference to contralateral side No difference in Mayo Elbow Performance Score (MEPS) between groups at 12 weeks but significantly better than pre-operatively (p < 0.01 open, p < 0.001 microtenotomy) |
| Meknas et al.13 RCT comparing radiofrequency microtenotomy versus open surgical release and repair Conducted in Norway | 24 patients 13 male, 11 female Open surgery: mean age 49.2 years (36 years to 62 years). Mean symptom duration 27.6 months Microtenotomy: mean age 46.7 years (30 years to 64 years). Mean symptom duration 22 months All patients had minimum symptoms 12 months with failed conservative treatment including 3 months of physiotherapy and at least three steroid injections | Open surgical release using modified Nirschl technique 21 (n = 11) Open 3-cm exposure of extensor tendon with microtenotomy using a radiofrequency device to a depth of 3 mm to 5 mm in three to six areas (n = 13) | 5-year to 7-year follow-up: One patient had died as a result of unrelated causes One patient in the microtenotomy group had revision open surgery Improved pain VAS in both groups (p < 0.005) but no differences between groups No difference in grip strength between groups Improved MEPS in both groups (p < 0.01) but no difference between groups |
| Monto23 RCT comparing Nirschl open release23 and repair with or without suture anchors Conducted in the USA | 60 patients with positive magnetic resonance imaging findings of tennis elbow No anchor group: mean age 48.2 years (30 years to 61 years); 16 male, 14 female Anchor group: mean age 49.3 years (30 years to 62 years); 18 male, 12 female Failed 6 months of conservative treatment including minimum 6 weeks of physiotherapy and one to three steroid injections Mean symptoms duration: Anchor group 10.4 months No anchor group 8.9 months | Elbow arthroscopy and debridement followed by Nirschl open release21 (n = 30) Elbow arthroscopy followed by open debridement, decortication and suture reattachment of ECRB tendon to the lateral epicondyle using two polyether ether ketone (PEEK) bone anchors (n = 30) | Improvements seen in both groups but no statistical analysis from baseline measurements Three patient outcomes in the no anchor group regarded as clinical failures. No failures in suture anchor group Between group improvements in MEPS and DASH score in favour of suture anchor group at 1 month, 2 months, 3 months, 6 months and 12 months (p = 0.001) |
| Morgan et al.17 RCT comparing platelet-rich plasma injection versus surgical release Conducted in the UK Conference abstract only | 92 patients but 11 lost to follow-up Mean age 47 years 34 male, 47 female Minimum symptom duration 6 months Failed non-operative treatment | Platelet-rich plasma (PRP) injection using a peppering technique (n = 42) Surgical release (n = 39) | 13/42 of PRP group requested surgery between 2 months and 6 months after injection One of 39 surgical patients subsequently had a PRP injection No significant difference in Patient-Reported Tennis Elbow Evaluation (PRTEE) or DASH scores between groups up to 12 months 42% of PRP patients reported definite benefit |
| Radwan et al.18 RCT comparing extracorporeal shockwave therapy (ESWT) versus percutaneous tenotomy Conducted in Egypt | 62 patients but six lost to follow-up ESWT group: mean age 40.14 years (23 years to 60 years); 15 male, 14 female Tenotomy group: mean age 39.26 years (22 years to 59 years); 18 male, 9 female Minimum symptom duration 6 months with failed conservative treatment including physiotherapy and steroid injection | ESWT to the common extensor origin at the point of maximum pain with a dose of 324.25 joules (n = 29) Grundberg & Dobson technique33 of percutaneous common extensor origin release with back-slab plaster immobilization for 1 week (n = 27) | No significant differences between groups in any measures at any time up to 12 months VAS improved (p < 0.01) at all time points in both groups for pressure pain up to 12 months VAS improved (p < 0.01) at 3 weeks and 6 weeks in both groups for rest pain VAS improved (p < 0.01) for night pain in ESWT group up to 12 months and tenotomy group up to 12 weeks |
| Yan et al.20 RCT comparing open versus arthroscopic Nirschl release23 Conducted in China English abstract only Full text only available in Chinese language | 26 patients (28 elbows) Mean duration of conservative care 23 months (4 months to 60 months) | Open Nirschl release21 (n = 13) Arthroscopic Nirschl21 release (n = 15) | Mean follow-up 17.4 months (4 months to 32 months) No difference between groups in pain VAS at rest or with daily living, return to work/sport or satisfaction Significant difference in pain VAS at work and sports and MEPS in favour of open group Open group: 100% good or excellent results Arthroscopic group: 93.3 good or excellent results |
RCT, randomized controlled trial.
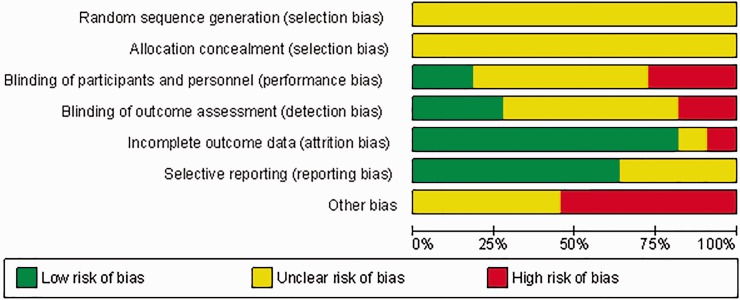
Risk of bias assessment
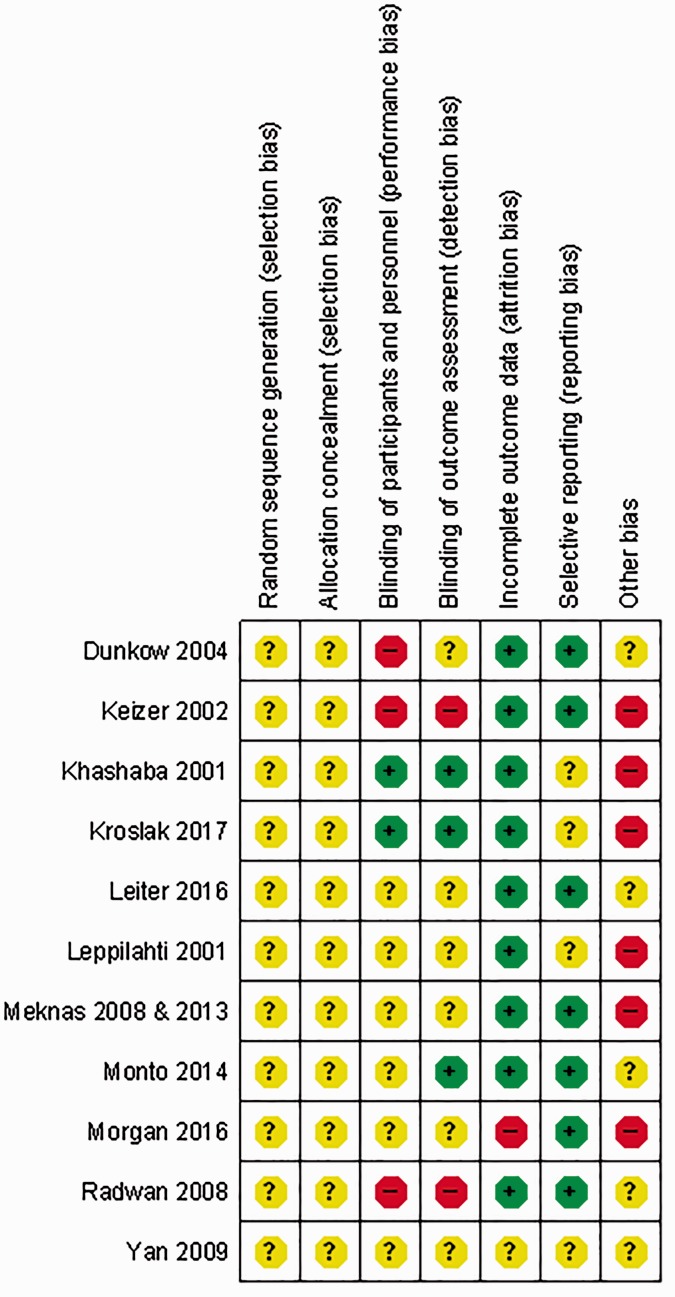
Risk of bias assessment was conducted independently by two reviewers (MB and CL) using the Cochrane Risk of Bias Assessment Tool.10 The process rates each study in terms of high risk, unclear risk and low risk of bias within seven domains based on published guidance.10 Any discrepancies between reviewers were then discussed and resolved. A third reviewer (AT) was available to cast a decisive vote; however, this was not required. The outcomes were compiled using Review Manager (RevMan), version 5.3 (The Cochrane Collaboration, Copenhagen, Denmark) and used to generate the risk of bias charts (Figures 4 & 5).
Figure 4.
Risk of bias across domains
Figure 5.
Risk of bias per study
As a result of heterogeneity across the retrieved studies in relation to surgical interventions and measures of clinical outcome, a narrative synthesis based on levels of evidence was undertaken.11 This rating system, shown in Table 2, was used to summarize the results in which the quality and outcomes of individual studies are taken into account.
Table 2.
Levels of evidence
| Strong evidence | Consistent findings in multiple high quality RCTs (n > 2) |
| Moderate evidence | Consistent findings among multiple lower quality RCTs and/or 1 higher quality RCT |
| Limited evidence | Only one relevant low quality RCT |
| Conflicting evidence | Inconsistent findings amongst multiple RCTs |
| No evidence from trials | No RCTs |
RCT, randomized controlled trial.
Results
In total, 124 abstracts were identified using database searches plus one additional paper from hand searching. After screening out duplicates and those that did not meet the inclusion criteria, 13 abstracts remained. Nine of these were available in full text versions plus three as conference abstracts only and one with an English translation abstract but full text in the Chinese language. One full text was excluded because it was a protocol for a randomized controlled trial that had not yet been completed.12
The remaining 12 studies were assessed for risk of bias and the results are shown in Figs 4 and 5. The two studies by Meknas et al.13,14 investigated the same cohort of patients over different time points and so details from each paper were merged for the assessment. It is notable that the risk of bias in all studies was unclear-to-high in five out of seven domains.
In total, the included studies investigated 490 patients (501 elbows). Four studies compared a surgical intervention versus nonsurgical intervention (including sham surgery).15–18 We acknowledge that sham surgery still involves a surgical skin incision; however, we regard this as a nonsurgical intervention or placebo because the area of pathology (i.e. the extensor tendons) is subject to no direct intervention and may not produce the same physiological changes. Two studies compared open versus arthroscopic surgical release.19,20 Two studies of the same patient group over different time periods investigated radiofrequency microtenotomy versus open release.13,14 Two studies compared the Nirschl surgical technique21 versus a modified technique.22,23 The remaining single studies compared open release versus a percutaneous mini-open technique24 and open release versus posterior interosseous nerve decompression.25 In studies where interventions were similar, heterogeneity in the terms of outcome measures precluded synthesis using a meta-analysis.
There is moderate evidence (four relevant low quality RCTs) that surgery, such as the Nirschl technique of open release,21 is not superior to nonsurgical interventions, including Botox injection, shockwave therapy, platelet-rich plasma injection and sham surgery, up to 12 months in terms of the primary outcome measure of pain and function including subjective pain measures, modified Verhaar score, Patient-Reported Tennis Elbow Evaluation (PRTEE) and Disability of Arm Shoulder Hand (DASH) scores.15–18 The sham surgery trial16 was terminated prematurely as a result.
There is conflicting evidence (inconsistent findings amongst two RCTs) in relation to the effectiveness of open versus arthroscopic surgical release.19,20 One RCT found no significant differences between groups in Visual Analogue Scale (VAS), DASH score or grip power at any time up to 12 months19 and the other RCT reported in favour of open surgery based on Mayo Elbow Performance Score and a subset of outcomes measuring pain VAS at work and during sport.20
There is limited evidence (one relevant low quality RCT) suggesting that there is no difference between radiofrequency microtenotomy and open surgical release in the short, medium or long term in relation to pain and function.13,14
There is limited evidence (two low quality RCTs) in relation to the effectiveness of the standard Nirschl release compared to a modified surgical technique.22,23 Both found in favour of the modified technique: one RCT reported in favour of extensor carpi radialis brevis (ECRB) tendon repair using suture anchors at 12 months23 and another in favour of not drilling the epicondylar bone at 6 months.22
There is limited evidence (one relevant low quality RCT) suggesting no difference between mini-open percutaneous release and traditional open release in terms of DASH score at 12 months but a faster return to activity in the minimally invasive group was reported with median return to work of 5 weeks in the open group compared to 2 weeks in the percutaneous group (p = 0.0001).24
There is limited evidence (one relevant low quality RCT) suggesting no difference between traditional open release and posterior interosseous nerve decompression at a mean follow-up of 31 months in terms of pain, grip strength and revision surgery.25
Discussion
The findings of this systematic review suggest that surgical interventions for tennis elbow are no more effective than nonsurgical and sham interventions. Procedural modifications may enhance the comparative effectiveness of surgical interventions but have not been compared against placebo interventions. These findings, however, are based on a body of evidence with significant methodological limitations.
In keeping with previous systematic reviews,7,8 these findings raise questions in relation to the effectiveness of surgery for tennis elbow and, considering risks and costs, whether nonsurgical interventions might be the current treatment of choice for this disorder. The question of how best to manage patients with persistent symptoms despite a period of failed conservative treatment still remains. Surgery has traditionally been regarded as being at the top of the treatment hierarchy, although our findings suggest that it may not be any more effective than a further course of nonsurgical treatment. However, this review also highlights the significant limitations in relation to the research evidence underpinning surgery for tennis elbow. Many of the included studies recruited small sample sizes with a high likelihood of Type II error and had questionable or unclear methods of randomization, as well as allocation concealment and a lack of blinding of participants and outcome assessment. These significant methodological limitations give rise to a high risk of bias in the studies completed to date. Furthermore, there was a wide variation in the methods of outcome assessment used meaning that meaningful data synthesis, that might counteract some of the limitations of the individual trials, is compromised. Patient expectations have also not been considered in the present study and evidence from rotator cuff surgery suggests that patient expectation of a surgical solution is the greatest predictor of whether conservative management fails.26
There is adequate justification to propose further research in light of the significant methodological limitations of the current body of evidence, given the recalcitrant nature of tennis elbow for some patients and recognizing that many do not resolve adequately with current treatment interventions. There is a clear indication for a high-quality, adequately powered RCT comparing surgical to sham surgical intervention including validated measures of patient-reported pain and function. Unfortunately, the reported sham study was terminated early because of a lack of difference in outcomes between groups, although the small numbers of recruits mean that this was underpowered and mean that the conclusion that surgery is no more effective than placebo cannot be strongly supported.16 Despite the challenges associated with sham-controlled surgical trials,27 precedent has been set in the upper limb in terms of a sham-controlled surgical trial investigating superior labral tears in the shoulder28 and a current UK trial comparing arthroscopic shoulder decompression surgery to a sham procedure,29 thus highlighting the feasibility of a larger trial.
Conclusions
The findings of this systematic review suggest that surgical interventions for tennis elbow are no more effective than nonsurgical or sham interventions for patients who have already undergone a course of conservative treatment. Caution is warranted, however, because these findings are based on a body of evidence with significant methodological limitations. There is now a clear indication for a high-quality, adequately powered RCT comparing surgical with sham surgical intervention, including validated measures of patient-reported pain and function to inform future clinical practice. The inclusion of a third treatment arm in the form of a credible conservative intervention (e.g. a structured physiotherapy package or a wait-and-see approach) would allow conclusions to be drawn regarding the most efficient and effective treatment strategy.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical review and patient consent
Not required for this article.
References
- 1.Bisset LM, Vicenzino B. Physiotherapy management of lateral epicondylalgia. J Physiother 2015; 61: 174–181. [DOI] [PubMed] [Google Scholar]
- 2.Harrington JM, Carter JT, Birrell L, Gompertz D. Surveillance case definitions for work related upper limb pain syndromes. Occup Environ Med 1998; 55: 264–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walker-Bone K, Cooper C. Hard work never hurt anyone – or did it? A review of occupational associations with soft tissue musculoskeletal disorders of the neck and upper limb. Ann Rheum Dis 2005; 64: 1112–1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Silverstein B, Viikari-Juntura E, Kalat J. Use of a prevention index to identify industries at high risk for work-related musculoskeletal disorders of the neck, back, and upper extremity in Washington state, 1990–1998. Am J Ind Med 2002; 41: 149–169. [DOI] [PubMed] [Google Scholar]
- 5.Coombes BK, Bisset L, Vicenzino B. Management of lateral elbow tendinopathy: one size does not fit all. J Orthop Sports Phys Ther 2015; 45: 938–49. [DOI] [PubMed] [Google Scholar]
- 6.Sanders TL, Jr, Maradit Kremers H, Bryan AJ, Ransom JE, Smith J, Morrey BF. The epidemiology and health care burden of tennis elbow: a population-based study. Am J Sports Med 2015; 43: 1066–1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buchbinder R, Green SE, Youd JM, Assendelft WJJ, Barnsley L, Smidt N. Systematic review of the efficacy and safety of shock wave therapy for lateral elbow pain. J Rheumatol 2006; 33: 1351–1351. [PubMed] [Google Scholar]
- 8.Buchbinder R, Johnston RV, Barnsley L, Assendelft WJ, Bell SN, Smidt N. Surgery for lateral elbow pain. Cochrane Database Syst Rev 2011; ▪▪: Cd003525–Cd003525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015; 4: 1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Higgins J, Green S (eds). Cochrane handbook for systematic reviews of interventions, version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. http://handbook.cochrane.org.
- 11.van Tulder M, Furlan A, Bombardier C, Bouter L. Updated method guidelines for systematic reviews in the cochrane collaboration back review group. Spine (Phila Pa 1976) 2003; 28: 1290–1299. [DOI] [PubMed] [Google Scholar]
- 12.Matache BA, Berdusco R, Momoli F, Lapner PL, Pollock JW. A randomized, double-blind sham-controlled trial on the efficacy of arthroscopic tennis elbow release for the management of chronic lateral epicondylitis. BMC Musculoskelet Disord 2016; 17: 239–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meknas K, Al Hassoni TN, Odden-Miland A, Castillejo M, Kartus J. Medium-term results after treatment of recalcitrant lateral epicondylitis: a prospective, randomized study comparing open release and radiofrequency microtenotomy. Orthop J Sports Med 2013; 1: 2325967113505433–2325967113505433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meknas K, Odden-Miland A, Mercer JB, Castillejo M, Johansen O. Radiofrequency microtenotomy: a promising method for treatment of recalcitrant lateral epicondylitis. Am J Sports Med 2008; 36: 1960–1965. [DOI] [PubMed] [Google Scholar]
- 15.Keizer SB, Rutten HP, Pilot P, Morre HH, v Os JJ, Verburg AD. Botulinum toxin injection versus surgical treatment for tennis elbow: a randomized pilot study. Clin Orthop Relat Res 2002; 401: 125–131. [DOI] [PubMed] [Google Scholar]
- 16.Kroslak M, Murrell GAC. Surgical treatment of lateral epicondylitis: a prospective, randomised, double blinded, placebo controlled clinical trial. Orthop J Sports Med 2017; 5: 2325967117S00120–2325967117S00120. [DOI] [PubMed] [Google Scholar]
- 17.Morgan B, Trail I, Watts A, Talwalker S, Nuttall D, Birch A. Comparing platelet-rich plasma (PRP) injection with surgical intervention for the management of refractory lateral epicondylosis. A randomised clinical trial. Shoulder Elbow 2016; 8: S29–S30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Radwan YA, ElSobhi G, Badawy WS, Reda A, Khalid S. Resistant tennis elbow: shock-wave therapy versus percutaneous tenotomy. Int Orthop 2008; 32: 671–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Leiter J, Clark T, McRae S, Dubberley J, MacDonald PB. Open versus arthroscopic tennis elbow release: randomized controlled trial. Orthop J Sports Med 2016; 4: 2325967116S00167–2325967116S00167. [Google Scholar]
- 20.Yan H, Cui G-Q, Liu Y-L, Xiao J, Yang Y-P, Ao Y-F. A randomized comparison of open and arthroscopic Nirschl debridement for refractory lateral epicondylitis. Zhonghua wai ke za zhi [Chinese Journal of Surgery] 2009; 47: 888–891. [PubMed] [Google Scholar]
- 21.Nirschl RP. Lateral extensor release for tennis elbow. JBJS 1994; 76: 951–951. [DOI] [PubMed] [Google Scholar]
- 22.Khashaba A. Nirschl tennis elbow release with or without drilling. Br J Sports Med 2001; 35: 200–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Monto RR. Tennis elbow repair with or without suture anchors: a randomized clinical trial. Tech Shoulder Elb Sur 2014; 15: 92–97. [Google Scholar]
- 24.Dunkow PD, Jatti M, Muddu BN. A comparison of open and percutaneous techniques in the surgical treatment of tennis elbow. J Bone Joint Surg Br 2004; 86: 701–704. [DOI] [PubMed] [Google Scholar]
- 25.Leppilahti J, Raatikainen T, Pienimaki T, Hanninen A, Jalovaara P. Surgical treatment of resistant tennis elbow. A prospective, randomised study comparing decompression of the posterior interosseous nerve and lengthening of the tendon of the extensor carpi radialis brevis muscle. Arch Orthop Trauma Surg 2001; 121: 329–332. [DOI] [PubMed] [Google Scholar]
- 26.Dunn WR, Kuhn JE, Sanders R, et al. 2013 Neer Award: predictors of failure of nonoperative treatment of chronic, symptomatic, full-thickness rotator cuff tears. J Shoulder Elbow Surg 2016; 25: 1303–1311. [DOI] [PubMed] [Google Scholar]
- 27.Wartolowska K, Collins GS, Hopewell S, et al. Feasibility of surgical randomised controlled trials with a placebo arm: a systematic review. BMJ Open 2016; 6: e010194–e010194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schrøder CP, Skare Ø, Reikerås O, Mowinckel P, Brox JI. Sham surgery versus labral repair or biceps tenodesis for type II SLAP lesions of the shoulder: a three-armed randomised clinical trial. Br J Sports Med 2017; 51: 1759–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beard D, Rees J, Rombach I, et al. The CSAW Study (Can Shoulder Arthroscopy Work?) – a placebo-controlled surgical intervention trial assessing the clinical and cost effectiveness of arthroscopic subacromial decompression for shoulder pain: study protocol for a randomised controlled trial. Trials 2015; 16: 210–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hohmann G. Das wesen und die behandlung des sogenannten tennisellenbogens. Munch Med Wochenschr 1933; 80: 250–252. [Google Scholar]
- 31.Verhaar J, Walenkamp G, Kester A, van Mameren H, van der Linden T. Lateral extensor release for tennis elbow. A prospective long-term follow-up study. J Bone Joint Surg Am 1993; 75: 1034–1043. [DOI] [PubMed] [Google Scholar]
- 32.Paoloni JA, Appleyard RC, Murrell GA. The Orthopaedic Research Institute-Tennis Elbow Testing System: a modified chair pick-up test-interrater and intrarater reliability testing and validity for monitoring lateral epicondylosis. J Shoulder Elbow Surg 2004; 13: 72–77. [DOI] [PubMed] [Google Scholar]
- 33.Grundberg AB, Dobson JF. Percutaneous release of the common extensor origin for tennis elbow. Clin Orthop Relat Res 2000; 376: 137–140. [DOI] [PubMed] [Google Scholar]