Abstract
Background
The present study aimed to determine whether arthroscopic remplissage with Bankart repair is an effective treatment for improving outcomes for collision athletes with Bankart and non-engaging Hill-Sachs lesions.
Methods
Twenty collision athletes underwent arthroscopic Bankart repair with posterior capsulotenodesis (B&R group) and were evaluated retrospectively, using pre- and postoperative WOSI (Western Ontario Shoulder Instability), EQ-5D (EuroQOL five dimensions), EQ-VAS (EuroQol-visual analogue scale) scores and Subjective Shoulder Value (SSV). The recurrence and re-operation rates were compared to a matched group with isolated arthroscopic Bankart repair (B group).
Results
The mean age was 25 years with an mean follow-up of 26 months. All mean scores improved with SSV of 90%. There was a mean deficit in external rotation at the side of 10°. One patient was treated with hydrodilatation for frozen shoulder. One patient had residual posterior discomfort but no apprehension in the B&R group compared to 5% persistent apprehension in the B group. In comparison, the recurrence and re-operation rates were 5% and 30% (p = 0.015), 5% and 35% (p = 0.005) in the B&R and B groups, respectively.
Conclusions
This combined technique demonstrated good outcomes, with lower recurrence rates in high-risk collision athletes. The slight restriction in external rotation does not significantly affect any clinical outcomes and return to play.
Keywords: athlete, Bankart repair, non-engaging Hill-Sachs, remplissage, shoulder instability
Introduction
The primary treatment for traumatic anterior shoulder dislocation has satisfactory results with short-term immobilization and physiotherapy,1,2 although high recurrence rates in some group of patients have been reported.3–5 The failure rates following surgical Bankart repair are also significantly higher in contact athletes, resulting in impaired sport performances.3,6–11 Moreover, a recent systematic review and meta-analysis confirmed that the redislocation rate for collision athletes was significantly higher, compared to noncollision athletes, following arthroscopic Bankart repair, ranging between 5.9% and 38.5%.12
It is generally accepted that critical anteroinferior glenoid bone loss, comprising 20% to 25% or more of the inferior glenoid diameter, must be addressed by glenoid bone block procedures, using either a coracoid transfer (Latarjet procedure), iliac crest graft or different allografts.13 However, there is no clear consensus on how to deal with patients with bipolar lesions, who have varying degrees of bone loss of the glenoid, as well as the proximal humerus (Hill-Sachs defects), where soft tissue structures have also undergone plastic deformation both anteriorly and posteriorly, as the result of multiple episodes.
Burkhart and De Beer14 reported the concept of significant bone defects, either on the humerus or the glenoid, and also described the ‘engaging’ Hill-Sachs (HS) lesions: this could engage on the anterior glenoid in a position of athletic performances and resulting in failure of the traditional arthroscopic repair. This has also highlighted that the restoration of the soft tissues alone would not be sufficient to stabilize the humeral head.
Wolf and Pollack15 and Wolf and Arianjam16 described an arthroscopic technique of HS remplissage associated with Bankart repair. This can provide a filling effect into the engaging humeral head defect, by performing a capsulotenodesis of the infraspinatus. Some studies have already confirmed that simultaneous Bankart repair with the remplissage procedure for engaging HS can provide lower recurrence rates compared to Bankart repair alone.17–19
The present study aimed to determine whether arthroscopic remplissage with Bankart repair is an effective treatment for improving outcomes for high-risk collision athletes with Bankart and ‘non-engaging’ Hill-Sachs lesions.
Materials and Methods
The present study comprises a retrospective analysis of collision athletes who underwent arthroscopic management of combined non-engaging HS and Bankart lesions between 2009 and 2014. The inclusion criteria were: (i) primary or recurrent traumatic anterior instability in professional collision athletes; (ii) Bankart lesion with non-engaging HS defect at dynamic intra-operative assessment; and (iii) no substantial glenoid bone loss (< 20%). Exclusion criteria were: (i) revision surgery; (ii) multidirectional or voluntary instability; (iii) unstable painful shoulder; (iv) no HS lesion; (v) humeral avulsion of the glenohumeral ligament (HAGL) or rotator cuff tear; and (vi) hyperlaxity, psychological conditions or epilepsy. All patients gave their agreement prior to enrolment and the study was approved by our local hospital institutional review board. We identified 22 professional athletes who underwent arthroscopic Bankart repair and remplissage, although one patient was lost to follow-up and another patient was excluded as a result of incomplete data. Twenty patients were available for analysis [arthroscopic Bankart repair with posterior capsulotenodesis (B&R) group] and there were 18 males and two females with a mean age of 25 years (range 15 years to 40 years), operated on from 2012 to 2014, with a mean follow-up of 26 months (24 months to 43 months).
Clinical evaluation
All patients were evaluated pre-operatively, at 4 weeks, 8 weeks, 6 months and every year postoperatively. Active range of movements (ROM) were measured pre-operatively and postoperatively, with anterior forward elevation (AFE), external rotation elbow at side (ER1) and at 90° of abduction (ER2), and internal rotation with level of the thumb on the spine (IR1) and at 90° of abduction (IR2). Stability was assessed using the relocation test and the apprehension test, with the arm in the ABER position (abduction and external rotation). Sulcus sign was used to rule out hyperlaxity and O’Brien's test for superior labrum anterior and posterior (SLAP) tears. The recurrence was recorded when patients reported signs of subluxation, one or more frank dislocations, or at least one episode of dead arm syndrome. Objective functional results were evaluated with pre- and postoperative Western Ontario Shoulder Instability (WOSI), EuroQOL five dimensions (EQ-5D), EuroQol-visual analogue scale (EQ-VAS) scores. Subjective results were based on postoperative pain (VASp), instability (VASi), stiffness (VASs) and strength (VASst) for Visual Analogue Scores scale and Subjective Shoulder Value (SSV), ranging from 0% to 100%. Return to play (RTP) and sport level were also documented.
Radiographic evaluation
Pre-operatively, plain radiographs (anteroposterior, lateral and axillary views) and a computed tomography scan (with three-dimensional reconstruction) or an arthro-magnetic resonance imaging (MRI) scan were systematically used to assess bone defects and soft tissue injuries. Postoperatively, plain radiographs were performed at each review to follow the radiographic evolution of absorbable anchors used for the Bankart repair and the Hill-Sachs remplissage. Signs of osteolysis around the anchors were carefully analyzed. Glenohumeral osteoarthritis was classified in accordance with the Samilson and Prieto classification.20
Comparison with matched group
Our database was used to create a control group. After applying the same patient demographics and follow-up period, all imaging studies and operative notes were reviewed to apply our strict criteria. Finally, all patients with incomplete data were excluded and we compared the clinical outcomes (recurrence and re-operation rates, RTP) with a historical group of 20 matched collision athletes (all males) who had undergone isolated Bankart repair (B group) between 2009 and 2013. The mean age was 25 years (range 18 years to 32 years), with a mean follow-up of 29 months (range 25 months to 47 months). There were no significant differences in the demographic data between the two groups (Table 1).
Table 1.
Patients’ demographics of both groups.
| B&R group | B group | |
|---|---|---|
| Number of patients | 20 patients (18 males, 2 females) | 20 patients (20 males) |
| Mean age | 25 years (15 years to 40 years) | 25 years (18 years to 32 years) |
| Operated side | 12 right, 8 left side (60% dominant) | 5 right, 15 left side (45% dominant) |
| Injury | 8 primary, 12 recurrent instability | 9 primary, 11 recurrent instability |
| Pre-operative mean number of instability | subluxation 5.8 (1 to 30), dislocation 1.9 (1 to 7) | subluxation 5.5 (1 to 21), dislocation 2 (1 to 8) |
| Labral lesions | 11 Bankart, 9 ALPSA lesion | 18 Bankart, 2 ALPSA lesion |
| Associated lesions | 3 associated SLAP lesion | 5 associated SLAP lesion |
| Calandra grades of Hill Sachs defect | 13 grade 2, 7 grade 3 | 15 grade 2, 5 grade 3 |
| Mean time to surgery | 7.2 weeks | 8.6 weeks |
| Mean number of anchors | 3.9 (2 to 5) | 3.1 (2 to 5) |
| Mean follow-up time | 26 months (24 months to 43 months) | 29 months (25 months to 47 months) |
B&R, Bankart and remplissage; B, Bankart; ALPSA, anterior labroligamentous periosteal sleeve avulsion; SLAP, superior labral anterior posterior tear.
The statistical analysis was performed using Prism, version 5.0 (GraphPad Software Inc., San Diego, CA, USA). The chi-squared test was used to analyze differences between the categorical data. The level of significance was set at p < 0.05.
Surgical technique
All procedures were performed by the senior surgeon, with patients in beach-chair position, under an interscalene nerve block with/without intravenous sedation or general anaesthesia. The operated arm was draped freely and the load-and-shift and sulcus sign test were performed in both shoulders, to check translations and general laxities. The 30° arthroscope was inserted into the glenohumeral joint through a standard posterior viewing portal. An anterior working portal was created over the superior edge of the subscapularis tendon as laterally as possible. An 8.5-mm cannula was inserted and a probe introduced to assess the integrity of the labrum. The entire joint was inspected thoroughly to assess the glenoid bone loss (based on the bare spot), to diagnose associated SLAP tears and exclude posterior labral lesions, HAGL lesions, chondral defects or rotator cuff tears. The HS defects were classified arthroscopically according to Calandra grading21 (grade I = lesion in the articular surface only; grade II = subchondral bone involvement, and grade III = large defect of the subchondral bone). Intra-operatively, the translation of the glenohumeral joint was assessed dynamically in different positions of arm abduction and external rotation, to determine the presence of the ‘engaging’ nature of the HS lesion.14 An additional anterosuperior working portal was created superiorly in the rotator interval, and a 7-mm cannula was inserted. Then, the entire capsulolabral complex was fully mobilized medially, from the base of the anterior glenoid neck. The previously described ‘Flying Swan technique’22 was performed for the Bankart repair and capsular shift, using Bioraptor Knotless or SutureFix anchors (Smith & Nephew Endoscopy, Andover, MA, USA). In the historical B-group, the Kinsa (Smith & Nephew Endoscopy, Andover, MA, USA) or the Bioknotless anchors (DePuy-Mitek, Raynham, MA, USA) were used. When present, a SLAP lesion was repaired with one or two additional anchors.
Then, for the remplissage procedure (only B&R group), the arthroscope was switched from posterior to anterior portal and the accessory posterolateral portal was created with a spine needle oriented perpendicular to the HS lesion. A posterior to anterior manual translation of the humeral head enhanced the view and the access to the posterior chamber. A working 7-mm cannula was inserted, the HS lesion was abraded until bleeding surfaces and one double-loaded absorbable Healicoil anchor (Smith & Nephew Endoscopy) was placed in the valley of the defect through transtendinous passage. Then, with the help of a penetrating grasper, superior and inferior mattress sutures were made and tied through the posterior aspect of the capsule and the infraspinatus tendon, creating a posterior capsulotenodesis. Finally, after switching back the arthroscope in the posterior portal, all repairs were checked (the Bankart repair with capsularshift with/without remplissage).
Postoperative care
The rehabilitation was standardized in both groups. The operated arm was placed in a sling, in internal rotation, for 4 weeks, with elevation up to 90°, external rotation to neutral position and only isometric exercises were allowed. Then, for another 4 weeks, a progression to full range of movement was initiated, with formal physiotherapy and isokinetic strengthening. After 8 weeks, once the strength was symmetrical and comparable to the other arm, dynamic weights and further conditioning for return to sport were supervised. Contact sports activities were not allowed usually until the third month, or until (i) the operated shoulder was pain-free; (iii) there no apprehension clinically; and (iii) a trial of contact in training was successful.
Results
Overall functional results
The mean WOSI, EQ-5D and EQ-VAS scores improved from 41.7% to 86.5%, 0.75 to 0.92 and 72.7 to 84.5, respectively, with SSV of 90% (80 to 100). Outcome scores were good, with low mean VAS scores for pain [VASp: 0.3 (0 to 1)], instability [VASi: 1.3 (0 to 2)], stiffness [VASs: 1.6 (0 to 3)] and strength [VASstr: 2.3 (0 to 4)]. Comparing active range of movements pre-operatively and at last follow-up, there were no major differences and the deficit in the mean external rotation elbow at side and at 90° of abduction was of 10° (0° to 15°) and 2° (0° to 5°), respectively (p > 0.05) (Table 2).
Table 2.
Range of movements.
| ROM | Pre-operative | Postoperative at last follow-up | Mean difference |
|---|---|---|---|
| AFE (°) | 170 (150 to 175) | 167 (155 to 170) | 3 |
| ER1 (°) | 75 (45 to 80) | 65 (40 to 70) | 10 |
| ER2 (°) | 85 (65 to 90) | 83 (60 to 90) | 2 |
| IR2 (°) | 75 (60 to 80) | 72 (60 to 75) | 3 |
| IR1 (level) | T6 | T7 |
AFE, active forward elevation; ER1, external rotation elbow at side; ER2, external rotation in 90° of abduction; IR1, internal rotation determined by the level of the thumb on the spine; IR2, internal rotation in 90° of abduction.
Complications
No iatrogenic postoperative complications were reported. Three patients had initial pain in extreme ROM of the shoulder but only one patient described some persistent posterior discomfort in shoulder rotations beyond the second month after the surgery and the MRI identified no significant abnormalities. Five patients had initial weakness but no final decrease in subjective muscle strength after the second month postoperatively. Five patients had initial stiffness but only one contact athlete had residual pain-free mild stiffness with full AFE, ER1 of 45°, although without affecting sport activities. All of these initial symptoms were commonly associated with recurrent instabilities (68%) and ALPSA (anterior labroligamentous periosteal sleeve avulsion) lesions (64%). Another patient was treated successfully with fluoroscopic-guided intra-articular hydrodilatation and steroid injection for frozen shoulder at 3 months postoperatively. One patient had transient axillary nerve palsy following the initial traumatic dislocation, which fully recovered without any effect on clinical outcomes or RTP.
Radiographic analysis
At final follow-up, no patients had signs of osteoarthritis or osteolysis around the anchors.
Comparison with matched group (recurrence and re-operation rates, as well as RTP)
We have summarized the comparative data in Table 3. There were statistically significant differences in recurrence (p = 0.015) and re-operation (p = 0.005) rates between the B&R and B groups. There was only one patient in B&R group who had a traumatic re-dislocation at 8 months postoperatively, following re-injury when playing rugby at the same level. Three weeks later, he underwent a diagnostic arthroscopy, which revealed failure of the anterior reconstruction but intact remplissage and a more medially located new Hill-Sachs lesion (grade 1) (Figures 1 and 2). Open coracoid transfer with the congruent arc technique was performed successfully with RTP again at 10 weeks. Six unstable B group patients (one subluxation, five dislocations) underwent revision surgery without any complication. All of them were stable with no apprehension at final follow-up and successful RTP. One other patient in B group underwent arthroscopic interposition arthroplasty for osteoarthritis 3 years after the stabilization surgery, with moderate success.
Table 3.
Comparative data with matched group.
| B&R group | B group | p | |
|---|---|---|---|
| Persistent apprehension | 0% | 5% (one patient) | 0.3 (NS) |
| Recurrence | 5% (one patient) | 30% (six patients) | 0.015 |
| Reoperation | 5%; one patient: open coracoid transfer at 8 months | 35%; seven patients: | 0.005 |
| Two arthroscopic revision at 3.5 months and 6 months | |||
| Four open coracoid transfer at 2 years | |||
| One interposition arthroplasty at 3 years for OA | |||
| RTP at same level | 100% at the mean of 13 weeks (10 weeks to 18 weeks) | 90% at the mean of 13 weeks (10 weeks to 16 weeks) | 0.14 (NS) |
B&R, Bankart and remplissage; B, Bankart; NS, not significant; OA, osteoarthritis; RTP, return to play.
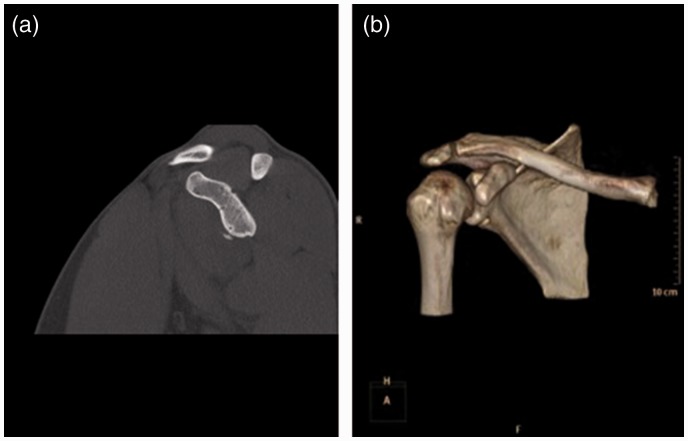
Figure 1.
(a) Sagittal computed tomography image of the glenoid and (b) three-dimensional reformat reveal another small bony Bankart lesion following a traumatic redislocation in the arthroscopic Bankart repair with posterior capsulotenodesis group.
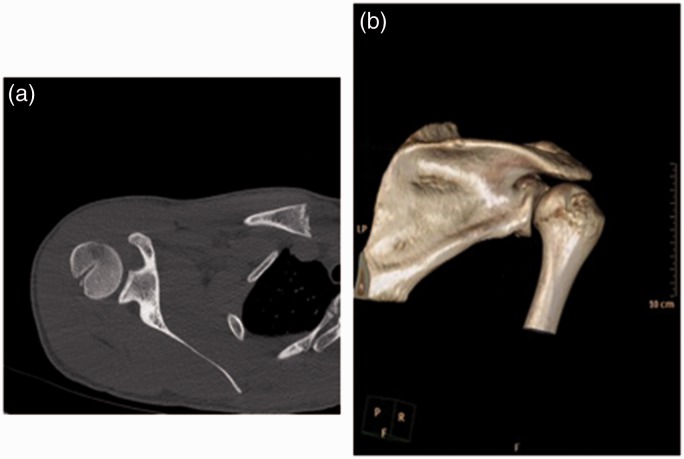
Figure 2.
(a) Axial computed tomography image of the shoulder and (b) three-dimensional reformat show the previous Hill-Sachs remplissage without any sign of re-injury in the same shoulder.
There was no statistically significant difference in the return to sport activities between the two groups. 100% of patients in the B&R group participated actively in professional contact sport at the same level, whereas only 90% (18) patients of B group managed to return to the same level of collision sport. One patient with persistent apprehension sign but without subluxation or dislocation failed to return to rugby at the same level. Another patient, who sustained a permanent axillary nerve lesion at the time of the primary dislocation, failed to participate in any sport activities postoperatively because this proved to be a career-ending injury.
Discussion
The results of the present study confirm that arthroscopic Bankart repair alone did not provide the stabilization necessary to prevent further instability in high-risk contact sport patients, even in the case of non-engaging HS lesions.
In a comparative study, Yamamoto et al.11 reported that the recurrence rate of contact athletes was two times higher in the open repair group and three times higher in the arthroscopic repair group compared to noncontact athletes; however, this was not statistically significant.
The literature also reports5,10,23 that young male patients, contact athletes and patients who have had several dislocations may be regarded as high-risk populations. These may benefit from bone block procedures or more secure soft tissue reconstructions, the so-called ‘arthroscopic plus’ procedures, rather than the traditional single-row anterior stabilization technique.
The technically challenging double-row labral repair method has been described in several studies that report satisfactory results and a lower redislocation rate.24,25 It has also been confirmed, in two cadaveric models,26,27 that the footprint surface area of the native capsulolabral complex was significantly better re-created with double-row fixation, compared to single-row fixation.
For more robust labral fixation, other arthroscopic techniques have been described to achieve a more uniform load distribution of the entire labrum.22,28 Although no proven superior clinical outcomes have been published yet, they are possibly more secure compared to classic techniques, in which the labrum is fixed only with ‘spot welds’ at each anchor. The labral bridge technique uses a LabralTape (Arthrex, Naples, FL) to secure the torn labrum to the glenoid between each suture anchor, for better pressure distribution.28 We used a similar ‘Flying Swan’ technique,22 which also relies on producing a kind of soft tissue seal, with a ‘double-mattress suture bridge’ medial to the glenoid margin. This augments the buttress effect of the labrum and improves contact and potentially healing process between the capsulolabral tissue and the bone between the anchors.
Maiotti et al.29 also reported results of the capsulolabral repair with subscapularis tenodesis augmentation, for patients with small glenoid bone loss and any size of HS lesion. The redislocation rate was 3.4%, with a mean deficit of ER1 of 6° and ER2 of 3°, which is very similar to the clinical results reported in the present study.
Recently Tennent et al.30 described the technique of arthroscopic conjoint tendon transfer, which can provide a dynamic sling effect additional to the traditional labral repair, for patients without significant anteroinferior glenoid bone loss (<15%).
Burkhart and De Beer14 reported the concept of significant bone defects either on the humerus or the glenoid and also described the ‘engaging’ Hill-Sachs lesions. Burkhart and De Beer14 also highlighted that the one-sided restoration of the soft tissues alone with Bankart repair would not be adequate in these cases. The importance of a bipolar fixation in anterior instability with Bankart and HS lesions was emphasized after the concept of glenoid track with ‘on-track’ and ‘off-track’ humeral head defects proposed by Yamamoto et al.31 and then investigated further by Di Giacomo et al.32
Filling of the engaging HS lesions with arthroscopic tenodesis of the infraspinatus and the posterior capsule into the defect, as described by Wolf and Pollack,15 can be performed to prevent recurrent instability. Although the remplissage with Bankart repair procedure has had increasing acceptance, there are still some concerns about postoperative stiffness and especially external rotation loss.33–35 However, the biomechanical study of Argintar et al.36 showed that the Bankart repair restored all ER to normal values at 0° and 60° abduction, and the addition of the remplissage procedure did not significantly alter the overall ROM and the anteroposterior translation. In our series, we also found that remplissage is safe and it did not impair the overall ROM or the function of the infraspinatus muscle and the slight restriction in ER1 does not significantly affect any clinical outcomes and RTP in the collision athletes.
The recurrence rate after arthroscopic Bankart repair with remplissage for engaging HS lesions is reported as being less than 10% in the literature.16,23,33,37 A few other studies17–19 compared the two procedures (isolated arthroscopic Bankart repair versus remplissage with Bankart repair) for patients with engaging HS lesions, and confirmed lower recurrence rates with the combined technique.
Most studies have focused solely on the management of engaging HS lesions with remplissage but, regardless of the location and the size, all Hill-Sachs lesions, including those classified as ‘non-engaging’, have to be engaged at least once to be created.38,39 It is also important to note that the posterior musculotendinous structures may be injured along with the anteroinferior structures and undergo plastic deformation; thus, a traditional one-sided anterior capsulolabral complex repair may not provide the expected results, especially in high-risk athletes. Because quantifying these posterior lesions is difficult, the so-called ‘bipolar fixation’ with combined arthroscopic Bankart stabilization with remplissage can be useful. Kany et al.38 reported the results of this bipolar fixation with a recurrence rate of 3.85%, which was used even in the case of no HS lesions when the posterior capsulotenodesis was performed on the bare area of the humeral head. Similarly, the aim of the present study was to investigate whether arthroscopic remplissage with Bankart repair can improve outcomes for ‘non-engaging’ HS lesions and we also report only 5% of recurrence rate in professional contact athletes. As in a previous study by Park et al.,40 this may be because, in the case of recurrence, the remplissage still showed almost complete filling of the previous HS defect, even with a failed anterior Bankart repair, which we also confirmed during revision arthroscopy. The redislocation rate was significantly higher in the historical control group (B group), which is likely multifactorial. We tried to eliminate confounding factors (matched groups with the same ‘Flying Swan’ technique), although other possible reasons are: (i) different levels of surgical experience; (ii) other types of anchors; (iii) no remplissage was performed; and (4) the use of standardized but possibly different rehabilitation protocols.
Study limitations
There are several limitations to the present study. (i) This was a retrospective analysis not a randomized trial, and the mean follow-up period was relatively short. (ii) The glenoid bone loss was not accurately measured with well-accepted pre-operative imaging methods. (iii) The size of HS lesion was not accurately measured volumetrically with cross-sectional imaging. (iv) Inter-observer variability exists in the dynamic assessment of the engagement of a HS lesion during arthroscopy. (v) Our data were compared with a historical group of patients and different anchors were used for labral fixation, which may have influenced our results.
The present study has several strengths as well. (i) All patients in this series were operated on by a single upper limb surgeon, with the same indication, surgical technique and standardized rehabilitation protocol, thereby reducing the variability of the clinical results. (ii) The arthroscopic evaluation of the glenoid defect based on the bare spot41 and the Calandra grading21 of the size of HS defect were systematically performed, aiming to minimize the potential confounding role of glenoid and humeral bone loss in our interpretation. (iii) We selected an appropriate, comparable historical group of patients, with specific parameters and strict criteria. (iv) Although this limited our ability to obtain large cohort for both groups as similar-sized non-engaging HS lesions were needed to compare and demonstrate the additional role of adding the remplissage procedure to an arthroscopic Bankart repair, in terms of preventing recurrent instability.
Conclusions
The present study has demonstrated an increased prevalence of recurrence with Bankart repair alone and a trend toward improved failure rates with the remplissage procedure for professional collision athletes with Bankart and ‘non-engaging’ HS lesions in the absence of significant glenoid defects. We consider that the additional remplissage tenodesis plays a crucial role in the increased stability in the case of moderate to large non-engaging HS lesions, and one-sided traditional Bankart repair will not provide the necessary stabilization to prevent failures in high-risk patients possibly as a result of the plastic deformation of posterior structures. In the present study, remplissage was confirmed to be a safe and effective method, without any significant complications affecting professional contact sport activities. Our relatively short-term follow-up does not exclude the occurrence of degenerative changes and other complications in the long-term and future investigations are necessary to further clarify the indication and the pros and cons of the remplissage procedure in anterior shoulder instability.
Acknowledgements
We acknowledge the support of the BESS for the podium presentation at the Annual BESS meeting.
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The authors declare that Andrew L. Wallace is acting as a teaching consultant and surgeon mentor for Smith & Nephew, Inc. There are no other conflicts of interest.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Review and Patient Consent
All patients gave their agreement prior to enrolment and the study was approved by the local hospital institutional review board.
References
- 1.Hovelius L, Augustini BG, Fredin H, Johansson O, Norlin R, Thorling J. Primary anterior dislocation of the shoulder in young patients: a ten-year prospective study. J Bone Joint Surg Am 1996; 78: 1677–1684. [DOI] [PubMed] [Google Scholar]
- 2.Longo UG, Loppini M, Rizzello G, Ciuffreda M, Maffulli N, Denaro V. Management of primary acute anterior shoulder dislocation: systematic review and quantitative synthesis of the literature. Arthroscopy 2014; 30: 506–522. [DOI] [PubMed] [Google Scholar]
- 3.Dickens JF, Owens BD, Cameron KL, et al. Return to play and recurrent instability after in-season anterior shoulder instability: a prospective multicenter study. Am J Sports Med 2014; 42: 2842–2850. [DOI] [PubMed] [Google Scholar]
- 4.Hovelius L, Olofsson A, Sandström B, et al. Nonoperative treatment of primary anterior shoulder dislocation in patients forty years of age and younger. A prospective twenty-five-year follow-up. J Bone Joint Surg Am 2008; 90: 945–952. [DOI] [PubMed] [Google Scholar]
- 5.Porcellini G, Campi F, Pegreffi F, Castagna A, Paladini P. Predisposing factors for recurrent shoulder dislocation after arthroscopic treatment. J Bone Joint Surg Am 2009; 91: 2537–2542. [DOI] [PubMed] [Google Scholar]
- 6.Owens BD, Agel J, Mountcastle SB, Cameron KL, Nelson BJ. Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med 2009; 37: 1750–1754. [DOI] [PubMed] [Google Scholar]
- 7.Sachs RA, Lin D, Stone ML, Paxton E, Kuney M. Can the need for future surgery for acute traumatic anterior shoulder dislocation be predicted? J Bone Joint Surg Am 2007; 89: 1665–1674. [DOI] [PubMed] [Google Scholar]
- 8.Cho NS, Hwang JC, Rhee YG. Arthroscopic stabilization in anterior shoulder instability: collision athletes versus noncollision athletes. Arthroscopy 2006; 22: 947–953. [DOI] [PubMed] [Google Scholar]
- 9.Roberts SN, Taylor DE, Brown JN, Hayes MG, Saies A. Open and arthroscopic techniques for the treatment of traumatic anterior shoulder instability in Australian rules football players. J Shoulder Elbow Surg 1999; 8: 403–409. [DOI] [PubMed] [Google Scholar]
- 10.Castagna A, Delle Rose G, Borroni M, et al. Arthroscopic stabilization of the shoulder in adolescent athletes participating in overhead or contact sports. Arthroscopy 2012; 28: 309–315. [DOI] [PubMed] [Google Scholar]
- 11.Yamamoto N, Kijima H, Nagamoto H, et al. Outcome of Bankart repair in contact versus non-contact athletes. Orthop Traumatol Surg Res 2015; 101: 415–419. [DOI] [PubMed] [Google Scholar]
- 12.Alkaduhimi H, van der Linde JA, Willigenburg NW, Paulino Pereira NR, van Deurzen DF, van den Bekerom MP. Redislocation risk after an arthroscopic Bankart procedure in collision athletes: a systematic review. J Shoulder Elbow Surg 2016; 25: 1549–1558. [DOI] [PubMed] [Google Scholar]
- 13.Gerber C, Nyffeler RW. Classification of glenohumeral joint instability. Clin Orthop Relat Res 2002; 400: 65–76. [DOI] [PubMed] [Google Scholar]
- 14.Burkhart S, De Beer JF. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000; 16: 677–694. [DOI] [PubMed] [Google Scholar]
- 15.Wolf EM, Pollack ME. Hill-Sachs ‘remplissage’: an arthroscopic solution for the engaging Hill-Sachs lesion. Arthroscopy 2004; 20: 14–15. [DOI] [PubMed] [Google Scholar]
- 16.Wolf EM, Arianjam A. Hill-Sachs remplissage, an arthroscopic solution for the engaging Hill-Sachs lesion: 2- to 10-year follow-up and incidence of recurrence. J Shoulder Elbow Surg 2014; 23: 814–820. [DOI] [PubMed] [Google Scholar]
- 17.Franceschi F, Papalia R, Rizzello G, et al. Remplissage repair – new frontiers in the prevention of recurrent shoulder instability: a 2-year follow-up comparative study. Am J Sports Med 2012; 40: 2462–2469. [DOI] [PubMed] [Google Scholar]
- 18.Garcia GH, Wu HH, Liu JN, Huffman GR, Kelly JD., IV Outcomes of the remplissage procedure and its effects on return to sports: average 5-year follow-up. Am J Sports Med 2016; 44: 1124–1130. [DOI] [PubMed] [Google Scholar]
- 19.Cho NS, Yoo JH, Juh HS, Rhee YG. Anterior shoulder instability with engaging Hill-Sachs defects: a comparison of arthroscopic Bankart repair with and without posterior capsulodesis. Knee Surg Sports Traumatol Arthrosc 2016; 24: 3801–3808. [DOI] [PubMed] [Google Scholar]
- 20.Samilson RL, Prieto V. Dislocation arthropathy of the shoulder. J Bone Joint Surg Am 1983; 65: 456–460. [PubMed] [Google Scholar]
- 21.Calandra JJ, Baker CL, Uribe J. The incidence of Hill-Sachs lesions in initial anterior shoulder dislocations. Arthroscopy 1989; 5: 254–257. [DOI] [PubMed] [Google Scholar]
- 22.Alexander S, Wallace AL. The ‘flying swan’ technique: a novel method for anterior labral repair using a tensioned suture bridge. Arthrosc Tech 2014; 3: 119–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Boileau P, O'Shea K, Vargas P, Pinedo M, Old J, Zumstein M. Anatomical and functional results after arthroscopic Hill-Sachs remplissage. J Bone Joint Surg Am 2012; 94: 618–626. [DOI] [PubMed] [Google Scholar]
- 24.Lafosse L, Baier GP, Jost B. Footprint fixation for arthroscopic reconstruction in anterior shoulder instability: the Cassiopeia double-row technique. Arthroscopy 2006; 22: 231–231. [DOI] [PubMed] [Google Scholar]
- 25.Iwaso H, Uchiyama E, Sakakibara S, Fukui N. Modified double-row technique for arthroscopic Bankart repair: surgical technique and preliminary results. Acta Orthop Belg 2011; 77: 252–257. [PubMed] [Google Scholar]
- 26.Ahmad CS, Galano GJ, Vorys GC, Covey AS, Gardner TR, Levine WN. Evaluation of glenoid capsulolabral complex insertional anatomy and restoration with single- and double-row capsulolabral repairs. J Shoulder Elbow Surg 2009; 18: 948–954. [DOI] [PubMed] [Google Scholar]
- 27.Kim DS, Yoon YS, Chung HJ. Single-row versus double row capsulolabral repair: a comparative evaluation of contact pressure and surface area in the capsulolabral complex-glenoid bone interface. Am J Sports Med 2011; 39: 1500–1506. [DOI] [PubMed] [Google Scholar]
- 28.Ostermann RC, Hofbauer M, Platzer P, Moen TC. The ‘Labral Bridge’: a novel technique for arthroscopic anatomic knotless Bankart repair. Arthrosc Tech 2015; 4: 91–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maiotti M, Russo R, Zanini A, Schröter S, Massoni C, Bianchedi D. Arthroscopic Bankart repair and subscapularis augmentation: an alternative technique treating anterior shoulder instability with bone loss. J Shoulder Elbow Surg 2016; 25: 898–906. [DOI] [PubMed] [Google Scholar]
- 30.Tennent D, Colaco HB, Arnander M, Pearse E. Arthroscopic conjoint tendon transfer: A technique for revision anterior shoulder stabilization. Arthrosc Tech 2016; 5: 201–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yamamoto N, Itoi E, Abe H, et al. Contact between the glenoid and the humeral head in abduction, external rotation and horizontal extension: a new concept of glenoid track. J Shoulder Elbow Surg 2007; 16: 649–656. [DOI] [PubMed] [Google Scholar]
- 32.Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from ‘engaging/non-engaging’ lesion to ‘on-track/off-track’ lesion. Arthroscopy 2014; 30: 90–98. [DOI] [PubMed] [Google Scholar]
- 33.Nourissat G, Kilinc AS, Werther JR, Doursounian L. A prospective, comparative, radiological, and clinical study of the influence of the ‘remplissage’ procedure on shoulder range of motion after stabilization by arthroscopic Bankart repair. Am J Sports Med 2011; 39: 2147–2152. [DOI] [PubMed] [Google Scholar]
- 34.Zhu YM, Lu Y, Zhang J, et al. Arthroscopic Bankart repair combined with remplissage technique for the treatment of anterior shoulder instability with engaging Hill-Sachs lesion: a report of 49 cases with a minimum 2-year follow-up. Am J Sports Med 2011; 39: 1640–1647. [DOI] [PubMed] [Google Scholar]
- 35.Deutsch AA, Kroll DG. Decreased range of motion following arthroscopic remplissage. Orthopedics 2008; 31: 492–495. [DOI] [PubMed] [Google Scholar]
- 36.Argintar E, Heckmann N, Wang L, Tibone JE, Lee TQ. The biomechanical effect of shoulder remplissage combined with Bankart repair for the treatment of engaging Hill-Sachs lesions. Knee Surg Sports Traumatol Arthrosc 2016; 24: 585–592. [DOI] [PubMed] [Google Scholar]
- 37.Buza JA, 3rd, Iyengar JJ, Anakwenze OA, Ahmad CS, Levine WN. Arthroscopic Hill-Sachs remplissage: a systematic review. J Bone Joint Surg Am 2014; 96: 549–555. [DOI] [PubMed] [Google Scholar]
- 38.Kany J, Pankappilly B, Guinand R, Kumar HA, Amaravati RS, Valenti P. ‘Bipolar fixation’: a novel concept in the treatment of recurrent anterior shoulder instability – a prospective study of 26 cases with minimum 2-year follow-up. Tech Should Surg 2013; 14: 10–16. [Google Scholar]
- 39.Purchase RJ, Wolf EM, Hobgood ER, et al. Hill-Sachs ‘remplissage’: an arthroscopic solution for engaging Hill-Sachs lesion. Arthroscopy 2008; 24: 723–726. [DOI] [PubMed] [Google Scholar]
- 40.Park MJ, Garcia G, Malhotra A, et al. The evaluation of arthroscopic remplissage by high-resolution magnetic resonance imaging. Am J Sports Med 2012; 40: 2331–2336. [DOI] [PubMed] [Google Scholar]
- 41.Burkhart SS, De Beer JF, Tehrany AM, et al. Quantifying glenoid bone loss arthroscopically in shoulder instability. Arthroscopy 2002; 18: 488–491. [DOI] [PubMed] [Google Scholar]