Introduction
Definition
Atraumatic shoulder instability is best defined as abnormal motion or position of the shoulder that leads to pain, subluxations, dislocations and functional impairment, but importantly it happens without any history of a significant preceding injury.
Aetiology
There are multiple causes of atraumatic shoulder instability. The majority of patients will have a combination of underlying laxity with an associated loss of muscle control. Repetitive micro-trauma may result in structural damage to the capsular restraints, often above shoulder height and when using the shoulder at extremes for example in throwing sports. This may lead to increased joint laxity and instability. Non-structural causes may be congenital, developmental or psychological.1
Shared decision-making
The General Medical Council’s (GMC) ‘Good Medical Practice guide’2 clearly states in the section on working in partnership with patients that doctors should:
Listen to patients and respond to their concerns and preferences.
Give patients the information they want or need in a way they can understand.
Respect patients’ right to reach decisions with the doctor about their treatment and care.
Support patients in caring for themselves to improve and maintain their health.
This can only be achieved by direct consultation between the patient and their treating clinician. Decisions about treatment taken without such direct consultation between patient and treating clinician are not appropriate, as they do not adhere to principles of good medical practice.
Continuity of care
Continuity and co-ordination of care are essential parts of the GMC’s Good Medical Practice guidance.2 It is therefore inappropriate for a clinician to treat a patient if there is no clear commitment from that clinician or the healthcare provider to oversee the complete care pathway of that patient including their diagnosis, treatment, follow-up and adverse event management.
Background
The majority of patients who develop shoulder instability do so after a traumatic event that leads to a documented dislocation resulting in subsequent recurrent instability and dislocations due to a structural defect.3 In contrast, the number of patients suffering with atraumatic instability is less. The true prevalence is unknown, with some authors suggesting it may be around 4% of those with shoulder instability,4 but the burden maybe much higher. There is, however, a wide spectrum of patients with this problem and while successful outcomes maybe achieved following non-operative treatment in 50–80% of cases,5,6 it should be noted that those who present with significant functional impairment usually prove resistant to standard conservative measures. In these instances, patients often require a more multidisciplinary team approach with consideration of psychosocial factors and other barriers to recovery if they are to be treated successfully.1
Patients with atraumatic instability become symptomatic when there is disruption of one or more of the following static or dynamic stabilisers that normally ensure that the shoulder joint remains congruent (in joint) throughout normal range of motion7:
Static stabilisers include:
The surface area and arc of contact and osteoarticular congruency
The capsulolabral complex and its proprioceptive and nociceptive systems
Dynamic stabilisers include:
The rotator cuff and the kinetic chain as a whole
The sensorimotor control systems – both peripheral and central
It should be noted that in the more extreme cases of atraumatic instability, frank shoulder dislocations can occur due to the loss of the dynamic stabilisers alone, i.e. with intact static stabilisers. Previously, such patients were often referred to as ‘voluntary dislocators’.
Patients with atraumatic instability can be classified and represent those in the Type II and III Polar groups of the Stanmore classification (Figure 1) and can have structurally normal or abnormal shoulders.6 Polar Type II instability is usually associated with localised or general hyperlaxity at the shoulder. Polar Type III instability is associated with a loss of muscle control and abnormal ‘patterns of movement’ with a structurally normal shoulder. However, the classification is designed so that mixed pathologies may co-exist such that patients may demonstrate both generalised signs of laxity, as well as muscle patterning. Such groups would be described as a Type II/III or alternatively a Type III/II, depending on the severity of their component pathologies. Moreover, the triangle allows a patient to migrate between the polar groups. This is particularly relevant when assessing the efficacy of the non-operative management of these patients.
Figure 1.
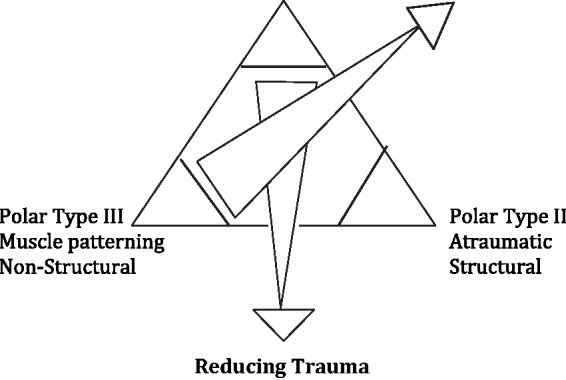
Stanmore classification of shoulder instability. Source: Reprinted with permission from Elsevier, 2004.10
The direction of the instability is variable. In traumatic instability the direction of instability is commonly anterior. In atraumatic instability the direction of instability may be anterior or posterior or associated with an inferior component. Very few patients are unstable in all three directions and are truly multidirectional, the term therefore is inaccurate. The direction of symptomatic instability can usually be defined by clinical testing.6,8–10
Assessment
Atraumatic shoulder instability predominantly affects young patients under the age of 25. The history often does not reveal a specific event or time when the symptoms began and can be very vague. Patients with laxity may have suffered a very subtle injury to the shoulder that is not regarded in their mind as a true injury or trauma, but could be enough to cause a structurally relevant injury to a susceptible individual that then leads to clinical instability. It is therefore important for clinicians to understand that laxity is a clinical sign, whereas instability is a symptom. The taking of a careful history in these patients is a critical part of the initial assessment to decide on which patients require further imaging and which patients should be referred directly for physiotherapy.
It is also important to specifically ask about multiple joint symptoms and not just those affecting the shoulder. A useful screening tool to aid in the assessment of joint laxity is the Beighton Score.11 This is a numeric score from 0 to 9 that is based on a number of clinical signs, and while the sensitivity of the score may vary with age, sex and environmental factors, such as a history of previous surgery, it remains a useful screening tool. The clinical signs that generate the score are as follows:
Hyperextension of the little fingers at the MCPJ (1 + 1 points),
If the thumb can be passively extended to the forearm with the hand pronated (1 + 1),
Greater than 10° of elbow hyperextension (1 + 1),
Greater than 10° of genu recurvatum while standing (1 + 1), and
If the patient can touch both palms to the floor while standing with the feet together and the knees straight (1).
The higher the score is, the more representative of a greater degree of joint laxity. This can therefore prove helpful in the assessment of those patients presenting with non-traumatic instability. However, if a formal diagnosis of hypermobility is needed, then the Beighton score must be combined with other clinical criteria that do not relate to the shoulder. These criteria are included in the 2017 Ehlers Danlos Syndrome (EDS) diagnostic criteria for Hypermobile EDS and replace previous diagnostic criteria.12 Indeed, these new diagnostic criteria are now more stringent, such that many patients will not fulfil the diagnosis of Joint Hypermobility Syndrome but instead will fall into a new category termed hypermobility spectrum disorder (HSD) and if the laxity is confined to the shoulders, then this will be further termed a localised HSD.13 The 2017 EDS Diagnostic may therefore act as a useful guide when considering patients with confounding hypermobility, as it may make the rehabilitation of patients with atraumatic shoulder instability more complicated.
As the presentation of atraumatic shoulder instability can be very varied, it is important that initial assessment in patients suspected as having the condition is thorough. Symptoms and signs at initial presentation are very variable and may not be related directly to the shoulder joint. Symptoms and signs include:
This group more commonly experience subluxations of the shoulder rather than dislocations.9
Feeling of shoulder insecurity or distrust which can occur during movement but may also occur in various positions or postures at rest or during sleep.
Pain symptoms can be complex in patients with atraumatic shoulder instability. The vast majority, however, experience pain local to the shoulder region, commonly localised to the long head of biceps.14–16
A small subgroup will present with more diffuse pain patterns that can refer through the arm to the hand. The pain can be characteristic of central pain such as ‘burning’, ‘sharp’ or ‘stabbing’ with associated paraesthesia or numbness. It is important to differentiate other causes such as thoracic outlet and neuropathic pain.14–16
Laxity and apprehension
Inability to perform certain tasks, particularly overhead that they may not attribute to their shoulder initially. This could be secondary to apprehension, pain or weakness. It is important to identify instability as the reason before beginning any course of investigation or treatment that may lead to a false diagnosis or cause harm when unnecessary.
Frank subluxation or dislocation
Most patients with atraumatic shoulder instability experience repeated subluxations rather than dislocations. A very small cohort may be able to voluntarily displace their shoulder often termed a ‘party trick’.
A subgroup can develop involuntary, habitual muscle patterns due to established abnormal muscle recruitment. Why this may occur is not always clear but can be due to general muscle deconditioning, fear and avoidance of movement as well as more complex psychosocial issues.16
Significant functional disruption with associated pain and severe muscle spasms that may make relocation difficult, leading to frequent attendances to the Accident & Emergency department.17
Red flags for the shoulder
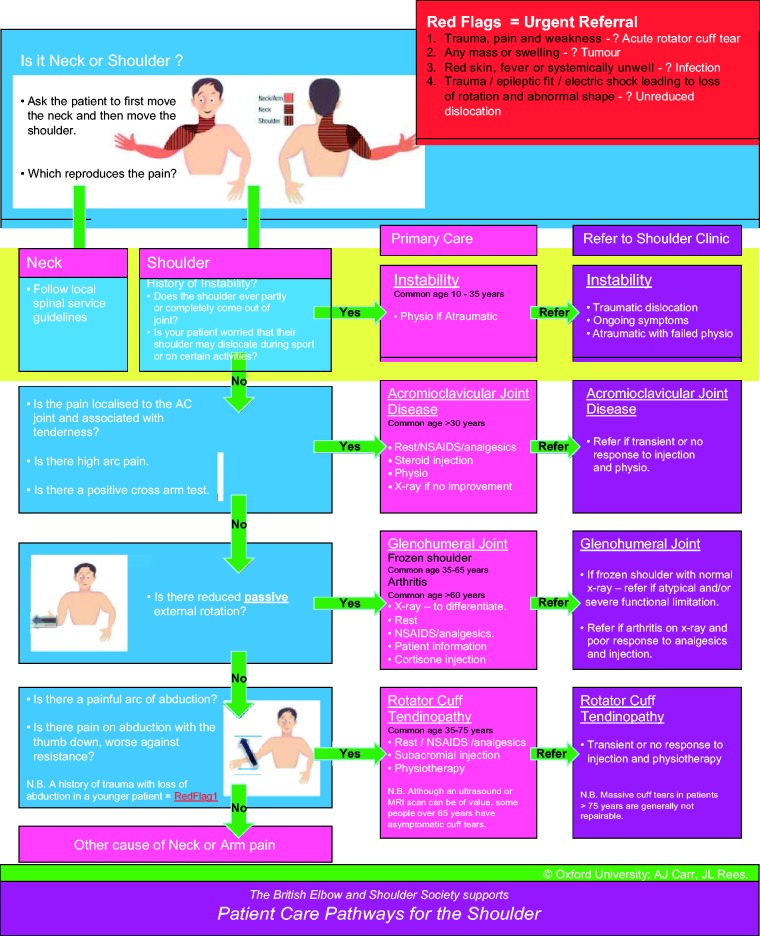
Acute severe shoulder pain needs proper and competent diagnosis. Any shoulder ‘Red Flags’ identified during primary care assessment need urgent secondary care referral (Figure 2).
A suspected infected joint needs same day emergency referral.
An unreduced dislocation needs same day emergency referral.
Suspected tumour and malignancy will need urgent referral following the local two-week cancer referral pathway.
An acute rotator cuff tear as a result of a traumatic event needs urgent referral and ideally should be seen in the next available specialist shoulder clinic.
It should be noted that 40% of patients over the age of 40 years suffering from a traumatic anterior glenohumeral dislocation will have a rotator cuff tear.3,18,19 Although not all of these will be clinically relevant, a careful examination of the rotator cuff strength should be performed and urgent referral sought if doubt remains regarding cuff integrity. The presence of infraspinatus weakness may indicate a large acute tear.
Figure 2.
Diagnosis of shoulder problems in primary care. Guidelines on treatment and referral.
Indicators for early tertiary referral
Most patients with atraumatic shoulder instability will respond to the right type of physiotherapy. However, there exists a subgroup of patients that are more difficult to treat and they are best served by early referral to a tertiary shoulder unit with experience in managing these complex patients. Individual cases that would benefit from an early referral to a tertiary centre include those with:
Frequent attendance at A&E for relocation
Persistent displacement or shoulder dislocation/subluxation
If under 18 years of age, absence from school (>20%) or work (>3 months)
Literature review of treatments
An up to date literature search was conducted to include a combination of search strategies, including MeSH searches with key words including but not limited to ‘multidirectional instability’, ‘atraumatic instability’ and ‘recurrent shoulder instability’. Up to and including April 2017 this yielded a total of nearly 400 publications. These were reviewed, and papers not relevant were excluded. Papers regarding the surgical management of atraumatic instability were reviewed in isolation. The search yielded mainly Level IV evidence,20–28 but there were three publications of Level II evidence, all from a prospective cohort study with controls.22,23,27 However, all of these three publications were produced from the same single cohort of patients. The volume of evidence available is therefore limited and of poor quality.
Rehabilitation
Some structured rehabilitation protocols that engage patients to a high level of compliance have reported good results.8–10,29–35 Burkhead and Rockwood33 reported good to excellent Rowe scores after physiotherapy alone in 80% of their patient cohort; however, there was a lack of pre-intervention scores to elucidate the treatment effect. Bateman et al.31 also reported a statistically significant improvement in Western Ontario Shoulder Index and Oxford Instability Shoulder Score in an atraumatic instability cohort but only reported short-term results. Short-term improvements in both Western Ontario Shoulder Index and Oxford Instability Shoulder Scores have also been reported after a 12-week structured physiotherapy rehabilitation programme by Watson et al.34
A recent randomised control trial was conducted by Warby and colleagues comparing two structured physiotherapy rehabilitation programmes.35 Their findings support the use of the Watson Multi-Directional Instability rehabilitation programme, with significantly better outcomes reported over a 24-week period when compared with the Rockwood Instability programme.
The best evidence identified constituted Level II evidence with additional Level IV retrospective cohort studies. Overall there is a lack of consistency in reported outcomes and thus, the lack of uniformity in outcome measures makes comparison of different interventions difficult. The current evidence regarding physiotherapy lacks robustness and methodological rigour and therefore it is difficult to extrapolate what constitutes best practice. There is also a lack of long-term follow-up studies reporting outcomes after managing patients with physiotherapy rehabilitation programmes. There is clearly a fundamental need for a well-designed trial looking at the results of high quality exercise-based interventions in the treatment of patients with atraumatic shoulder instability.8,36
Operative interventions
Outcomes from surgical intervention for atraumatic shoulder instability vary widely but throughout the published literature there is a lack of consistency in the outcome measures reported. Surgical procedures identified within the literature search include, but are not limited to, capsular shift, capsulorrhaphy, Bankart repair and bone block procedures. A review paper by Longo et al.5 reports recurrence rates of 22 and 24.5% for laser and thermal capsulorrhaphy, respectively; however, other authors have shown higher recurrence rates of 59%.26 In contrast, re-dislocation was reported in only 7.5% of shoulders undergoing open capsular shift and 7.8% of arthroscopic capsular shifts. This suggests that capsular shift procedures can be effective. In contrast, thermal capsulorrhaphy is no longer recommended.6 However, again, throughout the literature reviewed there is a lack of homogeneity with respect to the functional outcome scores used, making it difficult to compare interventions and outcomes in this population.
Need for guidance
Conservative rehabilitation continues to be generally accepted as the best initial management strategy for patients with atraumatic instability, while surgery is considered as a treatment that might exacerbate this particular shoulder problem further.6,8,29 Structured rehabilitation physiotherapy protocols that engage patients to a high level of compliance report good results. However, despite this being the more established treatment, any supportive evidence remains of low quality. Numerous surgical procedures have been described for the management of patients with atraumatic shoulder instability, but these are now generally restricted to varieties of soft tissue capsular procedures. The evidence for their use again remains of low quality and the lack of consistency in any reported outcome measures in the literature makes comparisons of any of these treatments difficult.
There is therefore a pressing need for further evidence to inform the treatment of patients with this difficult shoulder condition.8,29–35 Due to the lack of high quality evidence regarding the functional outcomes of patients treated with atraumatic shoulder instability, the following treatment guidelines are based on the limited but best evidence available and supported by expert consensus opinion.
Principles of treatment
While it is recommended that patients with atraumatic shoulder instability are best treated initially with a rehabilitation programme,10,37 a careful assessment by both a surgeon and physiotherapist is pivotal in identifying which patients may benefit from early referral for specialist tertiary care.32 Surgical management as first line treatment in patients with clinically obvious aberrant muscle patterning or those with a strong underlying psychological or psychosocial component will usually result in a poor outcome.6 This is why a distinction and recognition of this type of instability is important in order to prevent inappropriate surgery.
Treatment in primary care
Patients presenting with symptoms of instability as described above with no history of trauma should initially be referred in primary care for physiotherapy.
It is important to reassure such patients early on that the vast majority of patients will respond to treatment but that symptoms may take up to six months to resolve.
Imaging is not indicated in primary care (X-rays are often unhelpful).
Magnetic resonance or computer tomographic imaging is more appropriate in the secondary care setting after specialist assessment.
Glucocorticoid injections should not be used for pain relief as they can cause unnecessary harm, are unlikely to be of benefit and medicalises the pathology in the patients mind, therefore undermining physiotherapy rehabilitation.
- Physiotherapy should include education, reassurance and appropriate exercise prescription, targeting proprioception, the rotator cuff and scapula muscles.
- ○ If improvement is shown within 12 weeks then a further 3–6 months’ treatment is justified.
- ○ Failure to improve or presence of indicators for early referral should prompt early escalation.
Treatment in secondary care
Confirm diagnosis with thorough history and examination.
Ensure that appropriate initial physiotherapy rehabilitation has been undertaken and adhered to by the patient.
Reiterate that physiotherapy is successful in the majority of cases as long as it is the right type of programme and has been conducted properly and adhered to.
Specialist upper limb physiotherapists should be utilised in secondary care if physiotherapy in the primary care setting has been unsuccessful.
- Review the absence of concerning features that may warrant more specialist tertiary care input.
- ○ PainDETECT score >19.38
- ○ Attention seeking behaviour/significant emotional or psychological problems.
Adopt a multidisciplinary team approach in managing patients pain and psychological upset.
Consider magnetic resonance imaging in the form of arthrograms to assess capsulolabral structures or capsular volume.27,39
A shared decision-making process should be adopted early to understand and inform patient expectations and support adherence and engagement with agreed treatment plans.
- Surgery can be considered but should be adopted with extreme caution and only if:
- ○ No concerning features warranting referral to tertiary services are present – any doubt regarding the benefit of surgery should be discussed with tertiary centres.
- ○ Six months of structured physiotherapy with good compliance has been undertaken.
- ○ There is a clear target for surgical intervention, i.e. labrum repair or capsular shift.
- ○ Improvement has been made in an athlete but their residual symptoms prevent their return to activities.27
Inappropriate or incorrect surgery is associated with a poor outcome and therefore if doubt over the benefit of surgery persists, a tertiary referral should be requested.
Treatment in tertiary care
- Ideally, full multidisciplinary team involvement should be instigated early after referral including:
- ○ Shoulder surgeon with interest in complex instability
- ○ Specialist upper limb physiotherapists with experience in management of atraumatic instability patients
- ○ Pain services
- ○ Rheumatologists
- ○ Psychologists
- ○ Paediatricians
- ○ Neurophysiologists
- Further diagnostic evaluation may be necessary
- ○ Magnetic resonance arthrography
- ○ Computer tomographic imaging
- ○ Diagnostic injections to assess pain sources
- ○ Functional electromyelography and nerve conduction Studies
- ○ Diagnostic arthroscopy
Rheumatologist referral should be an early action if there is multiple joint involvement or evidence of hyperlaxity that may represent a collagen disorder
Neurophysiologist referral should be made to assess abnormal neurology found on examination or if there is suspicion of muscle discoordination40
- Psychologist referral early is appropriate if there is:
- ○ Low mood
- ○ Anxiety
- ○ Failure to attend work or school
- ○ Initial presentation was associated with a stressful time in the patient’s life
Botulinum toxin injections have been reported as an effective intervention in irreducible dislocations where there is persistent overactive tonic activity in global muscles such as pectoralis major and or latissimus dorsi.40 It may also be indicated in patients where there is a risk of inappropriate muscle activity in the recovery phase post-surgical stabilisation.41 However, expert opinion has shown that injections often have a temporary effect where inappropriate muscle patterning is driven by a central mechanism. Other patient-led strategies for affecting abnormal movement strategies may be more appropriate. Patients presenting with movement dystonias may be better served with onward referral to neurological functional movement disorder clinics where decisions around long-term botulinum injections for management can be better ascertained.
Operative interventions
Operative interventions should be approached with caution in patients with atraumatic shoulder instability and physiotherapy should always be the primary management strategy whether there is structural pathology or not.10,35,42 Eighty per cent of patients should respond to non-operative measures and only those with demonstrable pathology should be considered for surgical intervention or those with intractable symptoms despite appropriate rehabilitation.5,6 Publications describing surgical interventions are difficult to compare as they are not only sparse but also report many differing outcome measures5 such as Rowe Score, Constant score, American Shoulder and Elbow Surgeons score, University of California Los Angeles score, Western Ontario Shoulder Instability Index score.
It is difficult to compare surgical procedures given the diverse nature of the pathology in this patient group and given the lack of standardisation to reporting outcomes. For this particularly difficult shoulder problem, surgical procedures should be individualised and address each patient’s pathology rather than relying on one procedure for all. Surgery should always be approached with caution and an experienced multidisciplinary team is essential to maximise success. The patient needs to be fully aware of the very real risks of failure.
Procedures that have been used include:
Open capsular shift
Prospective cohort studies (Level II) and prospective case series (Level IV) evidence27,28,43–45
- Definitions of atraumatic shoulder instability varied between studies
- ○ Symptomatic instability with no history of trauma
- ○ Pain and symptomatic multi-directional instability
- ○ Hill–Sachs and Bankart lesions excluded
Only Rowe scores consistently reported
- Good outcomes
- ○ Post-operative Rowe score ranges – 90.6–94
These studies use different definitions of atraumatic instability and different outcome measures. They do, however, suggest that open or arthroscopic capsular shift can be successful in the management of atraumatic shoulder instability when combined with prescribed physiotherapy rehabilitation protocols. As the supporting evidence is of low quality, surgery should be approached with caution.
Arthroscopic capsulorrhaphy
Prospective cohort studies and case series (Level IV)25,46–48
Slightly higher volume studies (10–54)
No consistency in post-operative scoring of improvement
Patients with atraumatic instability mixed in with patients with traumatic instability
Failure rates from 16 to 59%
Complications other than recurrence of instability included neurological injury and adhesive capsulitis
These studies were particularly weak with mixed pathologies, small numbers and the use of different outcome scores. The high failure rates with no consistency among the reported outcomes leaves isolated arthroscopic capsulorrhaphy not recommended for atraumatic shoulder instability.
Summary
Evidence on which to base decision-making in the management of atraumatic shoulder instability is limited. This is due to the lack of a universal definition for the condition, small cohort studies and multiple outcome scores being used to evaluate treatment.
Despite these limitations it is evident that the vast majority of patients with atraumatic shoulder instability (with or without structural pathology) seem to improve with physiotherapy.
Physiotherapy should always be the first line (and second line) of management for such patients.
Patients that do not improve should be referred to a specialist orthopaedic shoulder surgeon and shoulder physiotherapist for careful assessment.
- If necessary, patients with certain indications may be referred directly to tertiary centres early
- ○ Frequent attendance at A&E for relocation
- ○ Persistent displacement or shoulder dislocation/subluxation
- ○ Absence from school (>20%) or work (>3 months)
A multidisciplinary team approach is essential in complex cases.
Evidence for operative intervention is poor and inconsistently reported in the literature. If surgery is to be undertaken then arthroscopic capsulorrhaphy is not recommended for the treatment of atraumatic shoulder instability.
Inappropriate or incorrect surgery is to be avoided as this has been shown to be associated with poor outcomes.
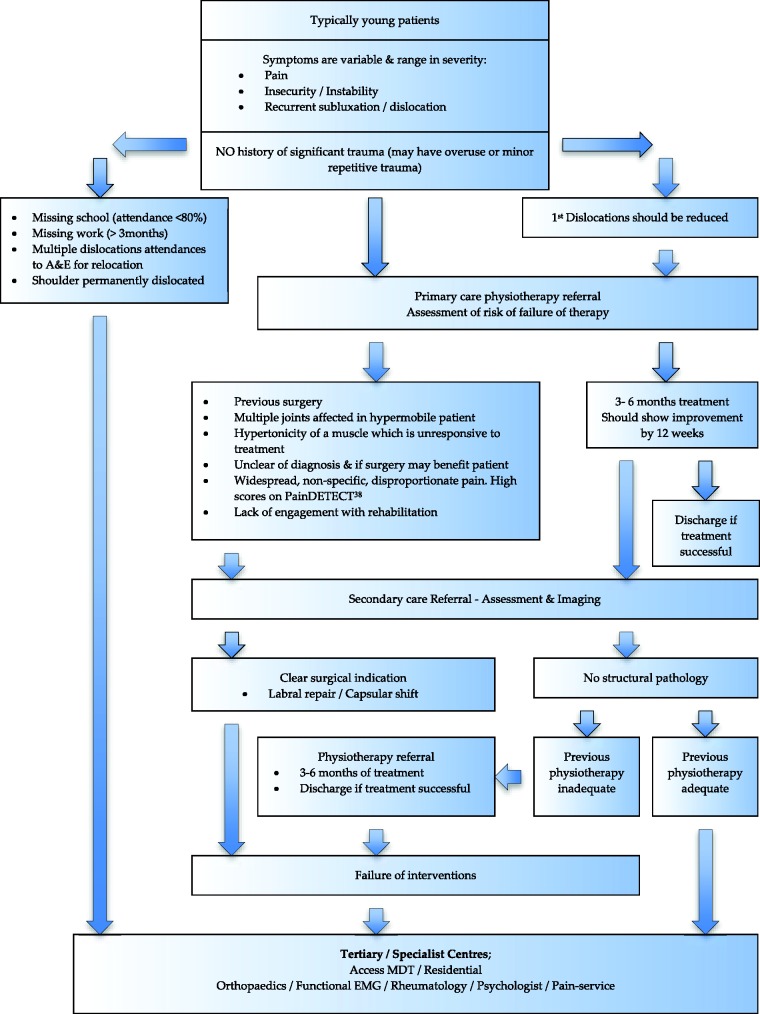
We propose a treatment algorithm as shown in Figure 3 to guide the management of patients with atraumatic shoulder instability based on the limited available evidence and expert consensus opinion.
Figure 3.
Proposed algorithm for the management of atraumatic shoulder dislocation. EMG: electromyography; MDT: multidisciplinary team.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Barrett C. The clinical physiotherapy assessment of non-traumatic shoulder instability. Shoulder Elbow 2015; 7: 60–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.General Medical Council. Good medical practice, https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/good-medical-practice (accessed 20 August 2017).
- 3.Brownson P, Donaldson O, Fox M, et al. BESS/BOA patient care pathways. Traumatic anterior shoulder instability. Shoulder Elbow 2015; 7: 214–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krøner K, Lind T, Jensen J. The epidemiology of shoulder dislocations. Arch Orthop Trauma Surg 1989; 108: 288–290. [DOI] [PubMed] [Google Scholar]
- 5.Longo UG, Rizzello G, Loppini M, et al. Multidirectional instability of the shoulder: a systematic review. Arthroscopy 2015; 31: 2431–2443. [DOI] [PubMed] [Google Scholar]
- 6.Jaggi A, Lambert S. Rehabilitation for shoulder instability. Br J Sports Med 2010; 44: 333–340. [DOI] [PubMed] [Google Scholar]
- 7.Gartsman GA, Brinker MR, Khan M, et al. Self-assessment of general health status in patients with five common shoulder conditions. JSES, 7: 228–237. [DOI] [PubMed] [Google Scholar]
- 8.Warby SA, Pizzari T, Ford JJ, et al. The effect of exercise-based management for multidirectional instability of the glenohumeral joint: a systematic review. J Shoulder Elbow Surg 2014; 23: 128–142. [DOI] [PubMed] [Google Scholar]
- 9.Johnson SM, Robinson CM. Shoulder instability in patients with joint hyperlaxity. JBJS 2010; 92: 1545–1557. [DOI] [PubMed] [Google Scholar]
- 10.Lewis A, Kitamura T, Bayley JIL. Mini symposium: shoulder instability (ii) the classification of shoulder instability: new light through old windows!. Curr Orthop 2004; 18: 97–108. [Google Scholar]
- 11.Grahame R, Bird HA, Child A. The revised (Brighton 1998) criteria for the diagnosis of benign joint hypermobility syndrome (BJHS). J Rheumatol 2000; 27: 1777–1779. [PubMed] [Google Scholar]
- 12.Malfait F, Francomano C, Byers P, et al. The 2017 international classification of the Ehlers-Danlos syndromes. Am J Med Genet Part C Semin Med Genet 2017; 175C: 8–26. [DOI] [PubMed] [Google Scholar]
- 13.Castori M, Tinkle B, Levy H, et al. A framework for the classification of joint hypermobility and related conditions. Am J Med Genet C Semin Med Genet 2017; 175: 148–157. [DOI] [PubMed] [Google Scholar]
- 14.Ngomo S, Mercier C, Bouyer L, et al. Alterations in central motor representation increase over time in individuals with rotator cuff tendinopathy. Clin Neurophysiol 2015; 126: 365–371. [DOI] [PubMed] [Google Scholar]
- 15.Kaas JH. Subcortical contributions to massive cortical reorganisations. Neuron 1999; 22: 657–660. [DOI] [PubMed] [Google Scholar]
- 16.Alexander CM. Altered control of the trapezius muscle in subjects with non-traumatic shoulder instability. Clin Neurophysiol 2007; 118: 2664–2671. [DOI] [PubMed] [Google Scholar]
- 17.Douglas T. Impact of Multidisciplinary rehabilitation on the socioeconomic burden of shoulder instability – a prospective study. In: BESS annual scientific meeting, Coventry, 23 June 2017.
- 18.Shin SJ, Yun YH, Kim DJ, et al. Treatment of traumatic anterior shoulder dislocation in patients older than 60 years. Am J Sports Med 2012; 40: 822–827. [DOI] [PubMed] [Google Scholar]
- 19.Hovelius L, Olofsson A, Sandström B, et al. Nonoperative treatment of primary anterior shoulder dis- location in patients forty years of age and younger, a prospective twenty-five year follow up. J Bone Joint Surg 2008; 90: 942–952. [DOI] [PubMed] [Google Scholar]
- 20.Moon YL, Singh H, Yang H, et al. Arthroscopic rotator interval closure by purse string suture for symptomatic inferior shoulder instability. Orthopaedics 2011; 34: 269. [DOI] [PubMed]
- 21.Engelsma Y, Willems WJ. Arthroscopic stabilization of posterior shoulder instability. Knee Surg Sports Traumatol Arthrosc 2010; 18: 1762–1766. [DOI] [PubMed] [Google Scholar]
- 22.Kiss RM, Illyés A, Kiss J. Physiotherapy vs. capsular shift and physiotherapy in multidirectional shoulder joint instability. J Electromyogr Kinesiol 2010; 20: 489–501. [DOI] [PubMed] [Google Scholar]
- 23.Illyés A, Kiss J, Kiss RM. Electromyographic analysis during pull, forward punch, elevation and overhead throw after conservative treatment or capsular shift at patient with multidirectional shoulder instability. J Electromyogr Kinesiol 2009; 19: 438–447. [DOI] [PubMed] [Google Scholar]
- 24.Voigt C, Schulz AP, Lill H. Arthroscopic treatment of multidirectional shoulder instability in young overhead athletes. Open Orthop J 2009; 3: 107–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alpert JM, Verma N, Wysocki R, et al. Arthroscopic treatment of multidirectional shoulder instability with minimum 270 degrees labral repair: minimum 2-year follow-up. Arthroscopy 2008; 24: 704–711. [DOI] [PubMed] [Google Scholar]
- 26.Hawkins RJ, Krishnan SG, Karas SG, et al. Electrothermal arthroscopic shoulder capsulorrhaphy. Am J Sports Med 2007; 35: 1484–1488. [DOI] [PubMed] [Google Scholar]
- 27.Baker CL, III, Mascarenhas R, Kline AJ, et al. Arthroscopic treatment of multidirectional shoulder instability in athletes: a retrospective analysis of 2- to 5-year clinical outcomes. Am J Sports Med 2009; 37: 1712–1720. [DOI] [PubMed] [Google Scholar]
- 28.Nyiri P, Illyes A, Kiss R, et al. Intermediate biomechanical analysis of the effect of physiotherapy only compared with capsular shift and physiotherapy in multidirectional shoulder instability. J Shoulder Elbow Surg 2010; 19: 802–813. [DOI] [PubMed] [Google Scholar]
- 29.Tillander B, Lysholm M, Norlin R. Multidirectional hyperlaxity of the shoulder: results of treatment. Scand J Med Sci Sports 1998; 8: 421–425. [DOI] [PubMed] [Google Scholar]
- 30.Misamore GW, Sallay PI, Didelot W. A longitudinal study of patients with multidirectional instability of the shoulder with seven- to ten-year follow-up. J Shoulder Elbow Surg 2005; 14: 466–470. [DOI] [PubMed] [Google Scholar]
- 31.Bateman M, Smith BE, Osborne SE, et al. Physiotherapy treatment for atraumatic recurrent shoulder instability: early results of a specific exercise protocol using pathology-specific outcome measures. Shoulder Elbow 2015; 7: 282–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kiss J, Damrel D, Makie A, et al. Non-operative treatment of multidirectional instability. Int Orthop 2001; 24: 354–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Burkhead WZ, Jr, Rockwood CA., Jr Treatment of instability of the shoulder with an exercise program. J Bone Joint Surg Am 1992; 74: 890–896. [PubMed] [Google Scholar]
- 34.Watson L, Balster S, Lenssen R, et al. The effects of a conservative rehabilitation program for multidirectional instability of the shoulder. J Soulder Elbow Surg 2018; 27: 104–111. [DOI] [PubMed] [Google Scholar]
- 35.Warby SA, Ford JJ, Hahne AJ, et al. Comparison of 2 exercise rehabilitation programs for multidirectional instability of the glenohumeral joint: a randomized controlled trial. Am J Sports Med 2018; 46: 87–97. [DOI] [PubMed] [Google Scholar]
- 36.Warby SA, Watson L, Ford JJ, et al. Multidirectional instability of the glenohumeral joint: etiology, classification, assessment and management. J Hand Ther 2017; 30: 175–181. [DOI] [PubMed] [Google Scholar]
- 37.Tibone JE, Bradley JP. Treatment of posterior subluxation in athletes. Clin Orthop 1993; 291: 124–137. [PubMed] [Google Scholar]
- 38.Freynhagen R, Tölle TR, Gockel U, et al. The PainDETECT project – far more than a screening tool on neuropathic pain. Curr Med Res Opin 2016; 32: 1033–1057. [DOI] [PubMed] [Google Scholar]
- 39.Gartsman GM, Roddey TS, Hammerman SM. Arthroscopic treatment of bidirectional glenohumeral instability: two- to five-year follow-up. J Shoulder Elbow Surg 2001; 10: 28–36. [DOI] [PubMed] [Google Scholar]
- 40.Sinha A, Higginson DW, Vickers A. Use of botulinum A toxin in irreducible shoulder dislocation caused by spasm of pectoralis major. J Shoulder Elbow Surg 1999; 8: 75–76. [DOI] [PubMed] [Google Scholar]
- 41.Donnellan CP, Scott MA, Antoun M, et al. Physiotherapy and botulinum toxin injections prior to stabilization surgery for recurrent atraumatic anteroinferior shoulder dislocation with abnormal muscle patterning. Shoulder Elbow 2012; 4: 287–290. [Google Scholar]
- 42.Lambert SM. Instability of the glenohumeral joint: oxford textbook of orthopaedics and trauma, 2nd ed Oxford: Oxford University Press, 2011. [Google Scholar]
- 43.Massoud SN, Levy O, Copeland SA. Inferior capsular shift for multidirectional instability following failed laser assisted capsular shrinkage. J Shoulder Elbow Surg 2002; 11: 305–308. [DOI] [PubMed] [Google Scholar]
- 44.Steinbeck J, Jerosch J. Surgery for atraumatic anteriorinferior shoulder instability. Acta Orthop Scand 1997; 68: 447–450. [DOI] [PubMed] [Google Scholar]
- 45.Marquardt B, Potzl W, Witt KA, et al. A modified capsular shift for atraumatic anterior-inferior shoulder instability. Am J Sports Med 2005; 33: 1011–1015. [DOI] [PubMed] [Google Scholar]
- 46.Miniaci A, McBirnie J. Thermal capsular shrinkage for the treatment of multidirectional instability of the shoulder. JBJS 2003; 85-A: 2283–2287. [DOI] [PubMed] [Google Scholar]
- 47.Frostick SP, Sinopidis C, Al Maskari S, et al. Arthroscopic shrinkage of the shoulder for the treatment of patients with multidirectional instability: minimum 2-year follow-up. Arthroscopy 2003; 19: 227–233. [DOI] [PubMed] [Google Scholar]
- 48.Fitzgerald BT, Watson BT, Lapoint JM. The use of thermal capsulorrhaphy in the treatment of multidirectional instability. J Shoulder Elbow Surg 2002; 11: 108–113. [DOI] [PubMed] [Google Scholar]



 BESS/BOA patient care pathways: Atraumatic shoulder instability
BESS/BOA patient care pathways: Atraumatic shoulder instability