Abstract
Background
Penile lymphangiomas are rare manifestations of lymphangiomas or lymphatic malformations which are more commonly found in the head or neck region of the body. Lymphangiomas are further categorized as lymphangioma circumscriptum, cavernous lymphangioma, cystic hygroma, or acquired lymphangiomas (also known as lymphangiectasia), based on their depth and etiology.
Results
A literature review revealed only 30 cases of penile lymphangioma between 1947 and March 30, 2018. Several causes were attributed to the acquired penile lymphangiomas, including trauma, phimosis, and infection. While penile lymphangiomas can be initially mistaken for an infection, a thorough history and physical examination is sufficient to clinically diagnose a lymphangioma of the penis. Historically, surgical excision has been the gold standard of treatment for this condition. When asymptomatic, patients may opt for conservative management with avoidance of mechanical trauma alone. Other physicians have revealed novel treatment plans to rid patients of their penile lymphangioma such as a staged laser procedure.
Conclusion
In this article, we elucidate the causes, symptoms, treatments, and outcomes associated with penile lymphangiomas found in the literature while also presenting the case of a 30-year-old African-American man diagnosed with acquired penile lymphangioma.
Keywords: Cavernous, Circumscriptum, Cystic, Hygroma, Lymphangioma, Lymphangiectasis, Lymphangiectasia, Penile, Penis
Résumé
Contexte
Les lymphangiomes du pénis sont des manifestations rares des lymphangiomes ou des malformations lymphatiques qui sont plus fréquemment observés dans les régions de la tête ou du cou au niveau du corps. Les lymphangiomes sont aussi classés en lymphangiome circumscriptum, lymphangiome caverneux, hygroma kystique, ou en lymphangiomes acquis (aussi connus sous l’appellation lymphangiectasie), selon leur profondeur et leur étiologie.
Résultats
Une revue de la littérature ne révèle que 30 cas de lymphangiomes du pénis rapportés entre 1947 et Mars 2018. Plusieurs causes ont été attribuées aux lymphangiomes acquis du pénis, parmi lesquelles les traumatismes, le phimosis et les infections. Bien que les lymphangiomes péniens puissent être initialement pris pour une infection, une recherche des antécédents et un examen clinique minutieux sont suffisants pour diagnostiquer cliniquement un lymphangiome du pénis. L’excision chirurgicale a toujours constitué le gold standard du traitement de cette maladie. Lorsqu’elle est asymptomatique, les patients peuvent choisir un traitement conservateur en évitant les seuls traumatismes mécaniques. D’autres médecins ont proposé de nouveaux traitements ayant pour objectif de débarrasser les patients de leurs lymphangiomes péniens, comme la procédure au laser par étapes.
Conclusion
A partir des données de la littérature, nous avons clarifié dans cet article les causes, symptômes, traitements et résultats associés aux lymphangiomes du pénis ; nous avons aussi présenté le cas d’un homme afro-américain âgé de 30 ans diagnostiqué comme porteur d’un lymphangiome pénien acquis.
Mots-clés
Caverneux, Circumscriptum, Kystique, Hygroma, Lymphangiome, Lymphangiectasie, Pénien, Pénis.
Background
Redenbacher et al. first described lymphangiomas, or “lymphatic malformations,” in 1828 [1]. Since then, lymphangiomas have been classified further in the literature as lymphangioma circumscriptum, cavernous lymphangiomas, cystic hygromas, and acquired lymphangiomas (also known as lymphangiectasias). Lymphangiomas are most commonly found in the head and neck, and two-thirds of all lymphangiomas are found by two years of age. The literature provides detailed pathological, radiographical, and clinical findings associated with lymphangiomas of the head and neck. On the contrary, fewer than 50 cases of lymphangiomas of the penis have been reported since the first description by Ferris et al. in 1944. Presumably, lymphangiomas of the penis are under-reported because the penile lesions, unlike the pathological counterparts in the head/neck, often go unnoticed by not only the physician but also the patient [2]. Furthermore, lymphangiomas of the penis are often misdiagnosed and mistreated as genital warts, molluscum contagiosum or gonorrhea [3]. The objective of this study is to define the different types of penile lymphangiomas by etiology, clinical findings, and treatments. Also, we report a case of acquired lymphangioma of the penis in a 30-year-old male treated successfully by surgical excision.
Methods
We conducted a literature review identifying all publications using the keywords: “penile” OR “penis” AND “lymphangioma” OR “lymphangiectasis” OR “lymphangiectasia.” Following our institutional protocol, the literature review identified relevant studies via a computer-aided search of American (MEDLINE from 1946 – March 31, 2018) and European articles (Embase 1947 – March 31, 2018). Publications found in languages other than English were excluded. Publications reporting lymphangiomas of the scrotum, perineum, and/or surrounding area not including the penis were excluded. The publications reporting benign transient lymphangiectasis of the penis (BTLP) were also excluded as BTLP, commonly known as sclerosing lymphangitis, is a transient condition that often results after sexual activity and holds minimal medical or surgical relevance. Classifications of penile lymphangioma found in Table 1 corresponding to the case classification from their original publication include “Acquired” (lymphangioma), “Cavernous” (lymphangioma), (lymphangioma) “Circumscriptum,” and (lymphangioma) “Circumscriptum Cysticum” (for cystic hygroma). The classification “Acquired [inferred]” was reserved for cases of lymphangiectasis/lymphangiectasia as well as reported cases of lymphangioma circumscriptum resulting from non-congenital causes. Although controversy exists in the difference between lymphangioma and lymphangiectasis/lymphangiectasia, all cases of lymphangiectasis/lymphangiectasia are reported as “Acquired [inferred]” in Table 1 for simplicity.
Table 1.
A summary of penile lymphangioma cases reported in the literature
| Author | Diagnosis | Age of Onset | Causes/Comorbidities | Location | Treatment | Outcome |
|---|---|---|---|---|---|---|
| Present case | Acquired | 30 years old with 21-year history | Skin of penis caught in zipper when patient was 9 years old | Asymptomatic bumps circumferentially around distal shaft of penis | Surgical resection | No pain, erythema or discharge found at 1 month follow-up |
| Gupta S et al. [11] | Acquired | 20 years old | Recurrent swelling with multiple, minute, papulo-vesicular lesions in right foot and leg from age of 3–4 months | Asymptomatic papular lesions on penis and scrotum present for 2–3 months | Simple electrofulguration of visible papulo-vesicles on penis | – |
| Acquired | 35 years old with 20-year history | – | Papular lesions and gradual swelling of scrotum and penis (shaft, frenulum and around external urethral meatus) | No intervention | – | |
| S Adikari et al. [10] | Acquired | 47 years old with 25-year history | Misdiagnosed as genital warts, treated for gonorrhea 5 years after | Smooth to palpation, wart-like lesion on dorsal aspect of penis, otherwise asymptomatic | Surgical excision | Successful with no sign of reccurrence |
| D. M. Piernick 2nd et al. [8] | Acquired | 48 years old with 5-year history | Hidradenitis suppurativa of buttocks, gluteal cleft and perineal area | Asymptomatic, multiple semitranslucent skin colored papules coalescing into plaques on penile shaft, scrotum and perineum | None | – |
| Errichetti et al. [4] | Acquired | 61 years old with 1-year history | Severe phimosis | Constricting phimotic ring and considerable edema of glans and distal foreskin with several translucent preputial papulovesicles (some slightly hyperkeratotic) localized close to balanopreputial sulcus | None - patient was waiting for surgery to correct phimosis – no follow-up information was provided | – |
| Zhang et al. [6] | Acquired | 8 years old with 2-week history | Surgery to correct phimosis | Asymptomatic, multiple small vesicular lesions on glans | “watch and wait” policy | Lesions resolved in 3 weeks |
| Dehner LP. et al. [21] | Acquired | 39 years old with 6-week history | – | Shaft, dorsum of penis | Surgical excision | Successful with no sign of recurrence |
| Ferris et al. [2] | Acquired | 35 years old with 30-year history | Measles? Circumcision? Pneumonia? All illnesses exacerbated condition | Lesions on foreskin of penis, scrotum and adjacent areas of the thigh and perineum | Surgical excision with skin graft | Successful with no sign of recurrence |
| Hagiwara et al. [9] | Acquired | 65 years old with 18-year history | Filariasis | Scrotum, extending to foreskin | Surgical excision and skin grafting | Successful with no sign of recurrence - transient penile edema present for few weeks |
| Sadikoglu et al. [5] | Acquired (inferred) | 15 years old with 3-year history | Blunt trauma caused skin thickening | Penile and scrotal skin | Surgical excision and skin grafting | Successful with no sign of recurrence |
| Kokcam et al. [19] | Acquired (inferred) | 19 years old with 3-year history | – | Multiple translucent and hemorrhagic vesicles on shaft and glans of penis. Surface was smooth, some umbilicated | Pt refused surgical intervention, advised to avoid mechanical trauma, apply silver sulfadiazine cream to ruptured lesions | No new lesions, overall number of lesions declined markedly with no other complications |
| Latifoglu et al. [22] | Acquired (inferred) | 10 years old with 6-year history | – | Penoscrotal lymphedema with erythematous plaque (irregular, well-defined border) on penile shaft and gelatinous-appearing, coalescent, verrucous vesicles and papules on scrotum | Surgical resection | Successful with no sign of recurrence |
| Maloudijan et al. [26] | Acquired (inferred) | 50 years old with 10-year history | – | Asymptomatic, 2 mm large vesicular lesions in sulcus coronarius from adjacent foreskin and glans | Patient abstained | – |
| Cestaro et al. [23] | Acquired (inferred) | 24 years old | HPV - genotype 6 comorbidity | Lesions on inguinal area, scrotum, penis, glans with associated edema of penis and lips | Surgery | Successful with no recurrence |
| Shi G. et al. [7] | Acquired [inferred] | 23 years old with 40-day history | Circumcision following phimosis 5 years ago | Asymptomatic translucent, yellowish, elevated, thick walled cystic lesions on right side of glans | 2940 nm nonablative fractional Er:YAG laser at 2–3 week intervals with power density of 3 J/cm2 at 20 ms and a 5 mm spot size | Lesions disappeard obviously after 4 sessions, no recurrence, dyspigmentation and paresthesia |
| Shah A. et al. [24] | Acquired [inferred] | 11 years old with few month history | – | Asymptomatic, soft mass on dorsal aspect of penis with extension towards right hemiscrotum | Local surgical resection | Recurrence 11 months following surgery |
| Bardazzi et al. [25] | Acquired [inferred] | 45 years old | – | Sulcus of prepuce | Diathermy | Successful with no sign of recurrence |
| Llanes et al. [16] | Cavernous | 20 years old | – | Soft lesion in dorsal area of prepuce | Circumcision | Successful with no sign of recurrence |
| Hayashi et al. [17] | Cavernous | 32 years old | – | Tumor on coronary sulcus of glans and submucosa | – | – |
| Cavernous | 35 years old | – | Tumor on coronary sulcus of glans and submucosa | – | – | |
| Geuekdjian et al. [27] | Circumscriptum | 3 years old | Congenital [inferred] | Asymptomatic, edematous swelling of penis particularly in skin spreading upwards to left groin | En bloc resection | Successful with no sign of recurrence |
| Demir et al. [18] | Circumscriptum | 21 years old with history since childhood | Congenital [inferred] | Recurrent infections, drainage of vascular lesions, penoscrotal deformity and inability to have sexual intercourse | Surgical excision | Successful, no sign of remission |
| Ferro et al. [3] | Circumscriptum | 16 years old | Congenital [inferred] | Tense vesicles filled with clear fluid on coronal region | 3 surgeries - remission every time. Denuded penis buried in tunnel guided through scrotum, 6 months after - shaft lift and recreated with scrotal skin | No negative consequences, local hairiness treated cosmetically |
| Osborne et al. [14] | Circumscriptum | 45 years old | Lichen planus - treated with cryotherapy | Cluster of translucent vesicles on shaft of penis and coronal sulcus. Balanomegaly. | Treatment declined | – |
| Tsur et al. [28] | Circumscriptum | 8 month old | Congenital [inferred] | asymptomatic elevated lesions on glans penis around meatus and dorsal aspect of penis | Surgical excision | Successful with no sign of recurrence |
| Drago et al. [12] | Circumscriptum | 27 years old | Ulceritive colitis | – | – | |
| Handa et al. [29] | Circumscriptum | 10 years old with 9 year history | Congenital [inferred] | Penis, scrotum, groins bilaterally | – | – |
| Swanson et al. [13] | Circumscriptum | 16 years old | Recurrent cellulitis of the penis and scrotum | Subcutaneous tissue of penis proximal to glans and skin of left proximal scrotum | – | – |
| Greiner et al. [15] | Circumscriptum cysticum | 13 years old | Congenital malformation | Edematous thickening of penile and scrotal skin | – | – |
A summary of penile lymphangioma cases reported in the literature
Case presentation
A 30-year-old African-American male presented to his primary care physician with a chief complaint of a several-year history of unhealing wounds on the right side of his penile shaft after his penis was caught in his zipper several years ago. Patient became concerned after noting white penile discharge 2 weeks prior. He denies any anal or oral lesions as well as exposure to any sexually transmitted diseases (STDs). Following outpatient specialty referral, the dermatologist reported excess skin tissue with underlying edema circumferentially on the distal penile shaft with overlying multiple firm skin-colored papules, some with exophytic crusting [Fig. 1]. Chlamydia trachomatis, human immunodeficiency virus (HIV), Neisseria gonorrhea and syphilis were negative. Subsequent biopsy found dilated vascular channels consistent with benign acquired lymphangioma of the penis (Fig. 2), and the patient was referred to urology for evaluation and management. With the urologist, the patient elected for surgical intervention due to cosmetic concerns despite the asymptomatic nature of the lymphangioma.
Fig. 1.

Clinical examination of patient’s penile shaft and glans: Multiple firm skin-colored papules, some with exophytic crusting and underlying edema, present on the right side of the patient’s penile shaft, immediately proximal to the glans
Fig. 2.
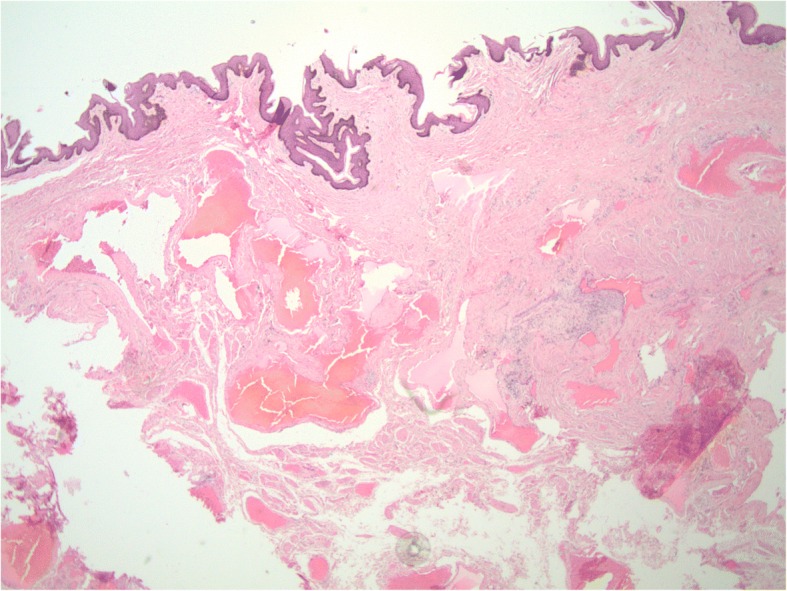
Histopathological image following biopsy of patient’s penile lesions: Histopathological staining from biopsy by punch technique of distal dorsal penile shaft shows dilated vascular channels consistent with benign lymphangioma of the penis
The patient underwent circumcision for redundant prepuce, excision of the skin lesion and penile foreskin reconstruction. A circumferential incision was made on the mucosa 0.5 cm proximal to the glans, distal to the lymphangioma. The foreskin was then retracted and another circumferential incision was made around the mucosal skin. The foreskin was then dissected using Bovie cautery and blunt dissection while the foreskin with lymphangioma tissue was excised. Intraoperative and postoperative courses were unremarkable. At 1-month follow-up, the patient reported no pain, erythema or discharge from the wound.
Results
The current literature review identified 27 cases in 25 publications. In the largest group, the 18 acquired lymphangiomas of the penis identified in the literature review encompassed a wide variety of cases. One was attributed to phimosis and 2 to trauma [4, 5]. Two iatrogenic cases resulted from correction of phimosis [6, 7]. One infectious case was attributed to filariasis (1 case), and 1 inflammatory case was attributed to hidradenitis suppurativa (1 case) [8, 9]. Two idiopathic cases were previously mistaken for genital warts and gonorrhea [10, 11].
Lymphangioma circumscriptum of the penis in this literature review was reported in eight, five of which were ruled to be congenital. The other three were notable for comorbidities of ulcerative colitis, recurrent cellulitis, and Lichen planus [12–14]. The only case of lymphangioma circumscriptum cysticum or cystic hygroma was found to have a congenital origin [15]. Lastly, cases of cavernous lymphangioma were attributed to a tumor (2 cases) and one with an unknown cause [16, 17].
Discussion
Lymphangiomas are generally described as uncommon, hamartomatous malformations of the lymphatic system. Based on depth and size of the lymph vessels, classifications include lymphangioma circumscriptum (most superficial), cavernous lymphangioma and cystic hygroma (most deep). Further subdivisions derive from perceived cause. Congenital lymphangiomas are thought to result from fetal lymph vessels that failed to involute and/or failed to join with the central lymphatic system. On the contrary, acquired lymphangiomas may result from trauma, certain infections (cellulitis, neoplastic disease, tuberculosis, filariasis), radiotherapy, pregnancy, scleroderma, severe phimosis or STDs [10].
Although the causes of these various types of lymphangioma may differ, the clinical presentation is often similar. The majority of the penile lymphangiomas present as asymptomatic, fluid-filled, translucent lesions or vesicles most commonly on the shaft or coronal sulcus of the penis. Symptomatic lesions, on the other hand, typically focus on sexual dysfunction. One case of acquired lymphangioma presented with severe phimosis and inability to produce an erection [4]. Also, one case of lymphangioma circumscriptum caused recurrent infection, intermittent drainage and sexual inactivity [18]. Given the similarities in clinical presentation, a proper diagnosis becomes contingent on a thorough history and physical examination in the case of lymphangioma of the penis. To that end, clinicians seeking to properly diagnose and treat lymphangiomas of the penis must effectively rule out certain infectious diseases such as molluscum contagiosum and gonorrhea [19]. This is generally possible following a thorough history and physical examination alone. However, in some rare cases, a biopsy with accompanying pathology report or an infectious disease workup may be necessary. Dermatology consultation may be selected for unclear cases. Interestingly, Errichetti et al. recently elucidated the potential role of dermoscopy in the diagnosis of penile lymphangioma by describing the presence of “yellowish-reddish, well-demarcated, round or oval lacunae surrounded by whitish areas or lines,” which may be common characteristics of lymphangiomas [4, 20]. This observation warrants further investigation into the utility of dermoscopy as a quick, non-invasive method of definitively diagnosing lymphangiomas.
Many authors may argue that lymphangiomas of the penis do not always require treatment, given the mostly asymptomatic nature of these lesions. However, patients may request intervention for cosmetic reasons. Of the 18 acquired lymphangiomas reported in Table 1 (including the present case), 9 were treated by surgical excision [2, 5, 9, 10, 21–23] – only one of which recurred 11 months following surgery [24]. And, one case reported an electrofulguration (or electrocautery) of the visible papulo-vesicles on the penis [11]. Shi et al. found that the acquired lymphangioma of the penis was amenable to 2940-nm Erbium-doped Yttrium Aluminum Garnet laser once every 2–3 weeks, wherein the lesions disappeared after the fourth session with no evidence of recurrence, dyspigmentation or paresthesia [7]. Bardazzi et al. utilized high-frequency electric currents, called diathermy, to successfully obliterate the acquired lymphangioma without evidence of recurrence [25]. On the other hand, Zhang et al. advocated for a “watch and wait” policy that interestingly allowed the lesions to self-heal within three weeks time [6]. Lymphangiomas that develop following circumcision may spontaneously resolve. Abstinence from treatment was observed in two patients, one of whom opted for protecting the lesions from mechanical trauma and applying a silver sulfadiazine cream to any ruptured lesions [19, 26]. This management decreased the number of existing lesions and prevented new lesions. Finally, one patient was waiting for surgery to correct phimosis; no follow-up information was provided [4]. Neither treatment nor follow-up was documented in the remaining two cases [8, 11].
Of the 3 cavernous lymphangiomas reported in Table 1, one underwent circumcision with no sign of recurrence following the treatment [16]. The other two cases failed to specify treatment [17]. Of the 8 cases of lymphangioma circumscriptum of the penis, 3 underwent surgical resection successfully with no signs of recurrence [18, 27, 28]. Another patient with lymphangioma circumscriptum (Table 1) underwent 3 surgeries with recurrence every time. For the fourth operation the physicians adopted a more radical surgical approach, in which the penile shaft was denuded and buried in the scrotum [3]. Six months later, the penile shaft was raised, and the skin was reconstructed using a scrotal graft. The outcome of this procedure was favorable with the only noteworthy complication of growth of transposed hair, treated cosmetically. Of the remaining 4 lymphangioma circumscriptum cases shown in Table 1, treatment was denied for 1, and the remaining 3 had no information on treatment or outcome [12–14, 29].
Conclusions
In summary, penile lymphangioma can be divided into four categories: 1) acquired, 2) lymphangioma circumscriptum, 3) cavernous lymphangioma, and 4) cystic hygroma. Commonly mistaken for infectious lesions, lymphangiomas underscore the importance of an appropriate history and physical to properly identify and treat the lymphatic malformation.
Acknowledgments
Not applicable.
Funding
There are no funding sources to report.
Availability of data and materials
The datasets used and/or analyzed for this study can be procured from the corresponding author upon request.
Abbreviations
- BTLP
Benign transient lymphangiectasis of the penis
- HIV
Human immunodeficiency virus
- STDs
Sexually transmitted diseases
Author’s contributions
MM assisted in manuscript composition and final review. SA assisted in manuscript composition and data collection. *MM and SA contributed equally to this submission. Hayan Jaratli provided the images and histology description. AD edited the manuscript and confirmed the accuracy of manuscript content. All authors read and approved the final manuscript
Ethics approval and consent to participate
This study was approved by the Henry Ford Hospital Institutional Review Board (IRB #11419).
Consent for publication
Upon outpatient follow-up, the patient consented to publishing his information and images (although they have been anonymized). The appropriate forms have been uploaded.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mohamed Macki, Email: mmacki2@hfhs.org.
Sharath Kumar Anand, Email: asharath@med.wayne.edu.
Hayan Jaratli, Email: hjaratl1@hfhs.org.
Ali A. Dabaja, Phone: (313) 916-2064, Email: adabaja2@hfhs.org
References
- 1.Redenbacher EAH. Dissertatio inauguralis medica de Ranula sub lingua, speciali cum casu congenito: Lindauer. 1828. [Google Scholar]
- 2.Ferris DO, Holmes CL. Extensive lymphangioma of scrotum, penis and adjacent areas; report of a case. J Urol. 1947;58(6):453–457. doi: 10.1016/S0022-5347(17)69584-3. [DOI] [PubMed] [Google Scholar]
- 3.Ferro F, Spagnoli A, Villa M, Papendieck CM. A salvage surgical solution for recurrent lymphangioma of the prepuce. Br J Plast Surg. 2005;58(1):97–99. doi: 10.1016/j.bjps.2003.12.025. [DOI] [PubMed] [Google Scholar]
- 4.Errichetti E, De Francesco V, Pegolo E. Acquired lymphangioma of the penis in a patient with severe phimosis. Int J Dermatol. 2015;54(11):e501–e503. doi: 10.1111/ijd.12922. [DOI] [PubMed] [Google Scholar]
- 5.Sadikoglu B, Kuran I, Ozcan H, Gozu A. Cutaneous lymphatic malformation of the penis and scrotum. J Urol. 1999;162(4):1445–1446. doi: 10.1016/S0022-5347(05)68336-X. [DOI] [PubMed] [Google Scholar]
- 6.Zhang RZ, Yang YH, Zhu WY. Acquired lymphangiectasia of the glans following circumcision. J Dtsch Dermatol Ges. 2014;12(7):623–624. doi: 10.1111/ddg.12314. [DOI] [PubMed] [Google Scholar]
- 7.Shi G, He XZ, Fan YM. Successful treatment of acquired Balanic Lymphangiectasia following circumcision using 2,940-nm erbium-doped yttrium Aluminium garnet laser. Dermatol Surg. 2016;42(8):1017–1018. doi: 10.1097/DSS.0000000000000778. [DOI] [PubMed] [Google Scholar]
- 8.Piernick DM, 2nd, Mahmood SH, Daveluy S. Acquired lymphangioma circumscriptum of the genitals in an individual with chronic hidradenitis suppurativa. JAAD Case Rep. 2018;4(1):64–66. doi: 10.1016/j.jdcr.2017.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hagiwara K, Toyama K, Miyazato H. Nonaka S. a case of acquired lymphangioma due to a suspected old filariasis and a review of literature. J Dermatol. 1994;21(5):358–362. doi: 10.1111/j.1346-8138.1994.tb01753.x. [DOI] [PubMed] [Google Scholar]
- 10.Adikari S, Philippidou M, Samuel M. A rare case of acquired lymphangioma circumscriptum of the penis. Int J STD AIDS. 2017;28(2):205–207. doi: 10.1177/0956462416657238. [DOI] [PubMed] [Google Scholar]
- 11.Gupta S, Radotra BD, Javaheri SM, Kumar B. Lymphangioma circumscriptum of the penis mimicking venereal lesions. J Eur Acad Dermatol Venereol. 2003;17(5):598–600. doi: 10.1046/j.1468-3083.2003.00884.x. [DOI] [PubMed] [Google Scholar]
- 12.Drago F, Rampini P, Muzio G, Rebora A. Lymphangioma circumscriptum of the penis. Acta Derm Venereol. 1997;77(3):252. doi: 10.2340/0001555577252. [DOI] [PubMed] [Google Scholar]
- 13.Swanson DL. Genital lymphangioma with recurrent cellulitis in men. Int J Dermatol. 2006;45(7):800–804. doi: 10.1111/j.1365-4632.2006.02782.x. [DOI] [PubMed] [Google Scholar]
- 14.Osborne GE, Chinn RJ, Francis ND, Bunker CB. Magnetic resonance imaging in the investigation of penile lymphangioma circumscriptum. Br J Dermatol. 2000;143(2):467–468. doi: 10.1046/j.1365-2133.2000.03695.x. [DOI] [PubMed] [Google Scholar]
- 15.Greiner R, Schmid GH. Lymphography of the skin of the scrotum and of the penis in a case of lymphagioma circumscriptum cysticum. Lymphology. 1971;4(4):140–144. [PubMed] [Google Scholar]
- 16.Llanes L, Ortega P, Paez A, Berenguer A. Cavernous lymphangioma of the prepuce. Braz J Surg. 2002;28:138–139. [Google Scholar]
- 17.Hayashi T, Tsuda N, Shimada O, Kishikawa M, Iseki M, Nishimura N, et al. A clinicopathologic study of tumors and tumor-like lesions of the penis. Acta Pathol Jpn. 1990;40(5):343–351. doi: 10.1111/j.1440-1827.1990.tb01571.x. [DOI] [PubMed] [Google Scholar]
- 18.Demir Y, Latifoglu O, Yenidunya S, Atabay K. Extensive lymphatic malformation of penis and scrotum. Urology. 2001;58(1):106. doi: 10.1016/S0090-4295(01)01111-6. [DOI] [PubMed] [Google Scholar]
- 19.Kokcam I. Lymphangioma circumscriptum of the penis: a case report. Acta Dermatovenerol Alp Pannonica Adriat. 2007;16(2):81–82. [PubMed] [Google Scholar]
- 20.Errichetti E, Pegolo E, De Francesco V. Acquired lymphangiectasia of the vulva. J Dtsch Dermatol Ges. 2015;13(3):237–239. doi: 10.1111/ddg.12505. [DOI] [PubMed] [Google Scholar]
- 21.Dehner LP, Smith BH. Soft tissue tumors of the penis. A clinicopathologic study of 46 cases. Cancer. 1970;25(6):1431–1447. doi: 10.1002/1097-0142(197006)25:6<1431::AID-CNCR2820250624>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 22.Latifoglu O, Yavuzer R, Demir Y, Ayhan S, Yenidunya S, Atabay K. Surgical management of penoscrotal lymphangioma circumscriptum. Plast Reconstr Surg. 1999;103(1):175–178. doi: 10.1097/00006534-199901000-00028. [DOI] [PubMed] [Google Scholar]
- 23.Cestaro G, De Rosa M, Gentile M, Massa S. A case of HPV and acquired genital lymphangioma: over-lapping clinical features. Ann Ital Chir. 2015;86 (ePub). PubMed PMID: 25818349. [PubMed]
- 24.Shah A, Meacock L, More B, Chandran H. Lymphangioma of the penis: a rare anomaly. Pediatr Surg Int. 2005;21(4):329–330. doi: 10.1007/s00383-004-1346-9. [DOI] [PubMed] [Google Scholar]
- 25.Bardazzi F, Orlandi C, D'Antuono A, Patrizi A. Lymphangioma circumscriptum of the penis. Sex Transm Infect. 1998;74(4):303–304. [PubMed] [Google Scholar]
- 26.Maloudijan M, Stutz N, Hoerster S, Rominger MB, Krause W. Lymphangioma circumscriptum of the penis. Eur J Dermatol. 2006;16(4):451–452. [PubMed] [Google Scholar]
- 27.Gueukdjian SA. Lymphangioma of the genitalia in children. Pediatrics. 1958;22(2):247–249. [PubMed] [Google Scholar]
- 28.Tsur H, Urson S, Schewach-Millet M. Lymphangioma circumscriptum of the glans penis. Cutis. 1981;28(6):642–643. [PubMed] [Google Scholar]
- 29.Handa N, Rao P, Kachhawa D, Rana K, Rekha S. Penile Lymphangioma Circumscriptum-A Rare Case Report. J Clin Exp Dermatol Res. 2016;7(318):2. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed for this study can be procured from the corresponding author upon request.


