Abstract
We present the case of a man with oligometastatic prostate cancer who underwent a PSMA-targeted 18F-DCFPyL PET/CT scan in order to illustrate how the PSMA-RADS grading sytem can be successfully used to support clinical decision-making and treatment planning. Notably, the presented patient was found to have an equivocal bone lesion (PSMA-RADS-3B) which was further worked up with a tumor protocol MRI and found to be definitively benign (PSMA-RADS-1B) and thus removed from the oligometastatic treatment plan. Remaining avid lesions were incorporated into the treatment plan or deferred for later work-up or monitoring, as indicated within the PSMA-RADS framework.
Keywords: PSMA, DCFPyL, Prostate cancer, Oligometastatic
Introduction
The oligometastatic state, typically defined as ≤5 sites of distant disease, is a potentially curable form of prostate cancer (PCa).1 In our clinical practice, hybrid positron emission tomography/computed tomography (PET/CT) with the 18F-labeled small-molecule prostate-specific membrane antigen (PSMA) inhibitor 18F-DCFPyL, is often used to assist in staging men with potentially oligometastatic PCa. This imaging test is available at our center through several clinical trials. For patients imaged with 18F-DCFPyL, we routinely employ the PSMA reporting and data system (PSMA-RADS) version 1.0 standardized framework to describe the likelihood of the presence of PCa at a given anatomic location.2 This five-point scoring system allows radiologists to communicate diagnostic confidence and follow-up recommendations to referring clinicians.
Herein, we present a case report of a 60-year-old man with newly diagnosed oligometastatic PCa in which the PSMA-RADS reporting framework was used to guide patient care.
Case presentation
A 60-year-old man presented with a serum prostate specific antigen (PSA) level of 8.24 ng/mL and cT2a digital rectal examination. The patient's history was significant for a prior poorly tolerated prostate biopsy that had demonstrated Grade Group 1 prostatic adenocarcinoma with a subsequent plan for active surveillance. The patient had, however, been lost to follow-up. When he re-presented, he underwent magnetic resonance imaging (MRI) that demonstrated extraprostatic extension and possible perirectal and obturator lymph node metastases. A repeat prostate biopsy showed progression to Grade Group 2 prostate cancer. The findings on MRI prompted a contast-enhanced CT that demonstrated indeterminate perirectal and mesenteric lymph nodes as well as a mixed lucent and sclerotic lesion in the right iliac bone. The patient also underwent a 99mTc-methylene diphosphonate bone scan which was negative for evidence of osseous metastases.
Due to the potential for metastatic disease, a PSMA-targeted 18F-DCFPyL PET/CT scan was obtained on a clinical trial evaluating the impact of PSMA-targeted PET on PCa patient management (ClinicalTrials.gov NCT02825875). 18F-DCFPyL-avid lesions included regional lymph nodes (PSMA-RADS-4), distant lymph nodes (PSMA-RADS-3A and −4; Fig. 1) and an osseous iliac lesion (PSMA-RADS-3B; Fig. 2). Additional foci of radiotracer uptake included the prostate gland (no PSMA-RADS score assigned) and a thyroid nodule (PSMA-RADS-3C). The patient's findings on the PSMA scan are summarized in Table 1.
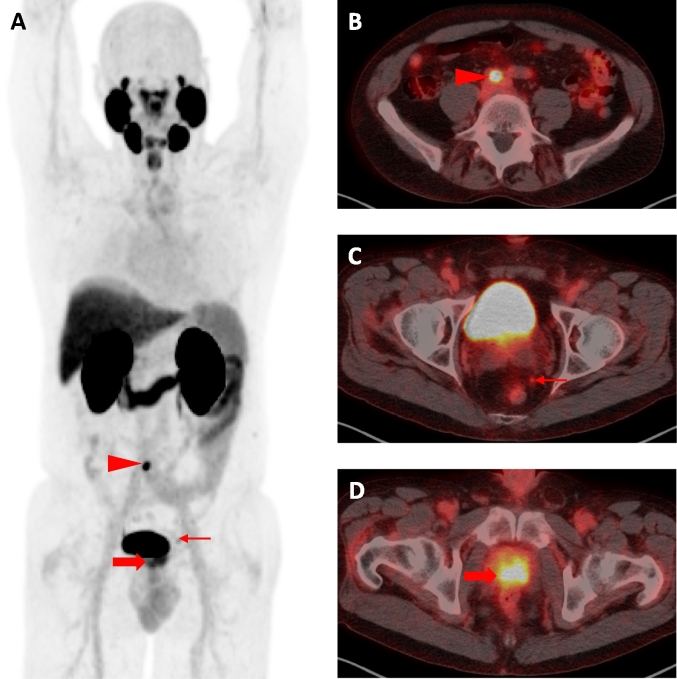
Fig. 1.
(A) Anterior, whole-body, maximum intensity projection image from the patient's 18F-DCFPyL PET demonstrating multiple findings discussed in the text including a common iliac lymph node with intense radiotracer uptake (red arrowhead, PSMA-RADS-4), a small perirectal lymph node with moderate radiotracer uptake (thin red arrow, PSMA-RADS-4), and the primary tumor (thick red arrow). (B–D) Axial 18F-DCFPyL PET/CT images redemonstrate the findings shown on the maximum intensity projection image.
Fig. 2.
(A) Axial non-contrast CT, (B) axial 18F-DCFPyL PET, and (C) axial 18F-DCFPyL PET/CT images through the pelvis demonstrate a partially lucent, partially sclerotic lesion in the posterior right iliac bone with focal radiotracer uptake (red arrowheads, PSMA-RADS-3B). (D) Axial apparent diffusion coefficient (ADC) map from tumor protocol MRI demonstrates no evidence of focally dark signal to suggest restricted diffusion in the lesion as well as a high average ADC value of 456 (red arrowhead). (E) Axial, T1-weighted in-phase and (F) axial, T1-weighted out-of-phase images from tumor protocol MRI demonstrate signal drop-out throughout much of the lesion on the out-of-phase image (average signal 822 on in-phase image and 502 on out-of-phase image), compatible with the presence of fat and indicative of a benign lesion such as a hemangioma (red arrowheads, PSMA-RADS-1B).
Table 1.
Findings on 18F-DCFPyL PET/CT and associated clinical decision-making.
| # | FINDINGS on 18F-DCFPyL PET/CT | PSMA-RADS SCORE1 | INTERPRETATION and CLINICAL DECISION-MAKING |
|---|---|---|---|
| 1 | Focally radiotracer avid, nonenlarged LNs in the left periaortic space, right common iliac chain, and left obturator chain, compatible with sites of prostate cancer involvement. | PSMA-RADS-4 – PCa highly likely- |
Lymph nodes within the adjuvant radiation field will be treated with radiation boosts; those outside of the adjuvant radiation field will be targeted with focused radiation. |
| 2 | Additional small lymph nodes in the retroperitoneum have approximately blood pool levels of uptake and are not definitive for sites of prostate cancer. | PSMA-RADS-3A – Equivocal uptake in soft tissue sites in a typical distribution for PCa |
Lymph nodes will be followed serially as per usual imaging follow-up, i.e, every 6 months. |
| 3 | Mild radiotracer uptake in a posterior right iliac bone lesion. | PSMA-RADS-3B – Equivocal uptake in a bone lesion not definitive but also not atypical for PCa on anatomic imaging |
Obtained MRI tumor protocol – PSMA-RADS-3B lesion is definitively benign, therefore it is reassigned to PSMA-RADS-1B (a benign lesion with radiotracer uptake). |
| 4 | Large left predominantly substernal thyroid nodule with radiotracer uptake. | PSMA-RADS-3C – Equivocal uptake in a site highly atypical of all but advanced stages of PCa |
Patient will have thyroid ultrasound and be considered for ultrasound-guided biopsy after completing PCa therapy. |
| 5 | Heterogeneous radiotracer uptake throughout much of the prostate, most focally in the base and mid of the left side of the gland. | No score assigned —PSMA-RADS score is not assigned to primary disease | Prostate has biopsy-proven PCa. Plan to offer prostatectomy following neoadjuvant therapy |
PCa: prostate cancer.
In accordance with recommendations from the PSMA-RADS system,2 the patient's iliac bone lesion merited further work-up in the context of a patient possibly being offered metastasis-directed therapy. Thus, the patient underwent a subsequent tumor protocol contrast enhanced MRI (which utilized a different protocol and different field-of-view relative to his prior prostate MRI), which showed a lack of diffusion restriction as well as definitive signal dropout on out-of-phase imaging indicating fat within the presumed lesion, definitive for a benign lesion and most suggestive of a hemangioma (PSMA-RADS-1B, Fig. 2). Additionally, uptake in a the patient's thyroid nodule was suspicious for a non-prostate malignancy (PSMA-RADS-3C), although it was recommended that further work-up be deferred until therapy for the patient's PCa had been completed.
Based on the findings of the 18F-DCFPyL scan that was further informed by the MRI, that patient was staged as having oligometastatic cT1N1M1a PCa. The patient was in turn offered several treatment options for his remaining radiotracer-avid lesions: standard of care therapy (androgen deprivation therapy alone OR androgen deprivation therapy + chemotherapy), or a clinical trial designed to provide definitive therapy to men with oligometastatic PCa (ClinicalTrials.gov NCT02716974). The patient opted for definitive therapy and he was treated with chemohormonal therapy with docetaxel, leuprolide, and abiraterone, with a plan to undergo subsequent cytoreductive prostatectomy followed by adjuvant radiation therapy, and then focused radiation to oligometastatic lesions outside of the pelvic radiation field. Synchronous androgen deprivation therapy was started with a planned duration of one year.
Discussion
This case report illustrates the use of the PSMA-RADS reporting framework to facilitate the metastatic work-up, and to establish a treatment plan, in a man with newly diagnosed oligometastatic PCa.
PSMA-targeted PET scans take advantage of the overexpression of PSMA on prostate cancer cells to increase the overall diagnostic performance of PCa imaging. However PSMA may be overexpressed in tissues other than PCa,3 impacting on the ability to interpret results of a PSMA-targeted PET scan. Overall, PSMA-targeted PET scans are believed to have very high sensitivity and specificity,4 although there are interpretive pitfalls that imaging specialists and referring clinicians should be aware of.5 PSMA-RADS facilitates the interpretation of these imaging studies by categorizing equivocal lesions and providing recommendations for further noninvasive advanced imaging work-up. As shown in this case, a standardized reporting framework such as PSMA-RADS can contribute substantially to decision-making in PCa patients with a limited amount of disease who are undergoing focal therapy. PSMA-RADS designations allowed for a diagnosis of oligometastatic disease, and a plan to target the sites of metastasis (PSMA-RADS-4 lesions) while also avoiding overtreatment of a radiotracer avid iliac bone lesion (PSMA-RADS-3B) which was found on follow-up MRI to be a benign lesion. Additionally, the PSMA-RADS system drew attention to thyroid nodule (PSMA-RADS-3C) that potential represents a non-prostate malignancy that will require work-up after the patient's PCa is treated.
Conclusion
This case report delineates how PSMA-RADS may be used to guide the work-up and treatment plan of PSMA avid lesions in patients with oligometastatic PCa. PSMA-RADS provides diagnostic confidence and recommendations for further work-up as needed. PSMA-RADS enables the clinician to understand the relevancy of the radiographic findings and to assimilate them into their clinical decision-making.
Conflicts of interest
M.G.P. is a co-inventor on a U.S. patent covering 18F-DCFPyL and as such is entitled to a portion of any licensing fees and royalties generated by this technology. This arrangement has been reviewed and approved by the Johns Hopkins University in accordance with its conflict-of-interest policies. M.A.G. has served as a consultant to Progenics Pharmaceuticals, the licensee of 18F-DCFPyL. S.P.R., M.A.G., K.J.P., and M.G.P. have all received research funding from Progenics Pharmaceuticals. No other authors have declared any relevant conflicts of interest.
Acknowledgements
We gratefully acknowledge funding from the Prostate Cancer Foundation Young Investigator Award, Progenics Pharmaceuticals, Inc., and the National Institutes of Health grants CA134675, CA183031, CA184228, and EB024495. This project has received funding from the European Union's Horizon 2020 research and innovation programme under the Marie Sklodowska-Curie grant agreement No 701983.
References
- 1.Reyes D.K., Pienta K.J. The biology and treatment of oligometastatic cancer. Oncotarget. 2015;6:8491–8524. doi: 10.18632/oncotarget.3455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rowe S.P., Pienta K.J., Pomper M.G., Gorin M.A. Proposal for a structured reporting system for prostate-specific membrane antigen-targeted PET imaging: PSMA-RADS version 1.0. J Nucl Med. 2018;59:479–485. doi: 10.2967/jnumed.117.195255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Salas Fragomeni R.A., Amir T., Sheikhbahaei S. Imaging of nonprostate cancers using PSMA-targeted radiotracers: rationale, current state of the field, and a call to arms. J Nucl Med. 2018;59:871–877. doi: 10.2967/jnumed.117.203570. [DOI] [PubMed] [Google Scholar]
- 4.Perera M., Papa N., Christidis D. Sensitivity, specificity, and predictors of positive 68Ga-prostate-specific membrane antigen positron emission tomography in advanced prostate cancer: a systematic review and meta-analysis. Eur Urol. 2016;70:926–937. doi: 10.1016/j.eururo.2016.06.021. [DOI] [PubMed] [Google Scholar]
- 5.Sheikhbahaei S., Afshar-Oromieh A., Eiber M. Pearls and pitfalls in clinical interpretation of prostate-specific membrane antigen (PSMA)-targeted PET imaging. Eur J Nucl Med Mol Imaging. 2017;44:2117–2136. doi: 10.1007/s00259-017-3780-7. [DOI] [PubMed] [Google Scholar]