Abstract
The obesity epidemic among older adults is expected to continue increasing unless public-health efforts address this age group. Yet, little is known about psychosocial determinants of obesity that relate specifically to older persons. In this study, we investigated for the first time whether self-perceptions of aging (SPA), defined as beliefs about oneself as an older person that are assimilated from society, relate to new cases of obesity. This seemed plausible because older persons who report more-positive SPA tend to engage in more health-promoting behaviors. Our sample consisted of 5702 Americans in the nationally representative Health and Retirement Study who were aged 60 years or older and not obese at baseline. The participants were followed from 2008 to 2014. As predicted, older persons with more-positive SPA, compared to those with more-negative SPA, were significantly less likely to become obese over the next 6 years, after adjusting for relevant covariates. For example, according to our model, a participant with the most-positive SPA score was 27% less likely to become obese than a same-aged peer with an average score on the SPA measure. These findings suggest that interventions aimed at reducing the prevalence of obesity in later life could benefit from targeting SPA.
Keywords: Ageism, Stereotyping, Healthy aging, Obesity, Self perceptions of aging, Views of aging, Behaviors, Preventive health
1. Introduction
Obesity among older persons can have a detrimental impact on a wide range of outcomes, among them physical functioning, quality of life, dementia, and mortality (e.g., Han et al., 2011; Hruby et al., 2016). Currently, 39% of Americans aged 60 years or older meet the obesity definition (Robert Wood Johnson Foundation, 2018). Moreover, unless public-health efforts address the obesity epidemic, it is expected to continue increasing in this age group (Han et al., 2011). Although determinants of obesity and weight maintenance that apply to all ages have been identified (e.g., Hruby et al., 2016), cultural determinants that relate specifically to older persons remain unknown.
In the current study, we hypothesized that older persons with positive self-perceptions of aging (SPA) will have a lower risk of becoming obese than those with negative SPA. We define SPA as beliefs about oneself as an older person. Previous research has found that positive SPA, assimilated from the prevailing culture across the lifespan, buffer against stress and increase the likelihood of engaging in health-promoting behaviors, such as exercise and healthy eating, in later life (Levy, 2009; Levy and Myers, 2004; Wurm et al., 2008). Also, a field study demonstrated that positive SPA can be bolstered (Levy et al., 2014).
2. Methods
2.1. Participants
The cohort consisted of 5702 participants in the nationally-representative Health and Retirement Study (Sonnega and Weir, 2014). They met our criteria at baseline: (a) aged 60 years or older; (b) not obese (BMI of 29 kg/m2 or lower); and (c) responded to the SPA measure. The SPA measure was first measured in a random selection of half the participants in 2008 and the remaining participants in 2010. All covariates were measured at the time of baseline SPA. New cases of obesity were collected every 2 years after baseline until 2014. Participants with more-positive and more-negative SPA at baseline did not significantly differ by sex, race, or smoking history. Compared to those with more-positive SPA, those with more-negative SPA at baseline tended to be older, have significantly more chronic diseases and depressive symptoms (Radloff, 1977), and were less physically active, as defined by meeting the physical-activity guidelines for older adults based on frequency of engagement in vigorous-, moderate- and mild-intensity activities (Kämpfen and Jürgen, 2016). All of these factors were included in the models as covariates.
2.2. Measures
2.2.1. Predictor
The SPA predictor was measured with the Attitude Toward Aging subscale of the Philadelphia Geriatric Center Morale Scale (Lawton, 1975; Liang and Bollen, 1983). The subscale, which consists of five items (e.g., The older I get, the more useless I feel), was reverse-scored, so that a higher score indicated more-positive SPA. This subscale has been found to be valid for the age group of the participants (Levy et al., 2002). We treated the total scores, ranging from 5 to 30, as continuous variables in multivariate models. To examine whether those with more-negative and more-positive SPA differed at baseline, we dichotomized SPA at the mean of 15.
2.2.2. Outcome
The incident obesity outcome was measured by a BMI of 30 kg/m2 or over. Participants' newly developed obesity was recorded in follow-up waves at 2, 4, and 6 years after baseline. In our sample, 559 individuals, who were obesity-free at baseline, became obese.
2.2.3. Covariates
The covariates included in all models were selected because they have been found to be related to the predictor, the outcome, or both (Han et al., 2011; Hruby et al., 2016; Levy, 2009). The covariates consisted of initial BMI category (i.e., normal or overweight), age, race (i.e., White, Black, or other), sex, education (i.e., up to completion of high school or greater than high school), depression (Radloff, 1977), smoking history (i.e., ever smoked or had not), physical activity, and number of physician-diagnosed diseases (i.e., arthritis, cancer, diabetes, heart disease, hypertension, lung disease, or stroke). Covariates of age and number of physician-diagnosed diseases were included as continuous variables. Depression was included as a dichotomous variable based on the Center for Epidemiological Studies–Depression cut-off score of 16 to indicate individuals at risk of clinical depression (Lewinsohn et al., 1997; Radloff, 1977).
3. Results
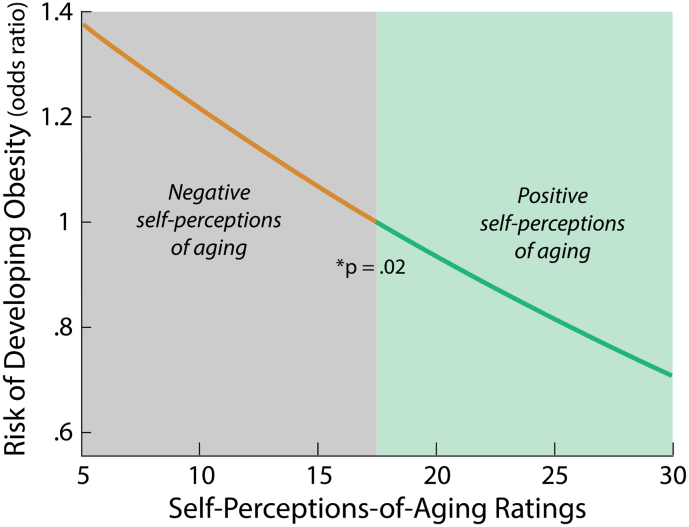
As predicted, older persons with more-positive SPA, compared to those with more-negative SPA, were significantly less likely to become obese over the next 6 years, OR = 0.90 (95% CI: 0.82, 0.99), p = .03, after adjusting for all covariates in a multivariate logistic model (see Fig. 1). For example, a person with the most-positive SPA score was 27% less likely to become obese than a person with the average score of 15 on the SPA measure.
Fig. 1.
Positive self-perceptions of aging predict lower risk of developing obesity across 6 years.
Note: Figure based on model with all covariates included. Reference point for model was the midpoint of the Self-Perception-of-Aging (SPA) scale, which was scored with a higher number indicating a more positive SPA. Participants were 60 years or older and obesity-free at baseline.
Odds ratio of greater than 1 denotes increased risk of developing obesity, whereas odds ratio of less than 1 denotes a protection against developing dementia.
4. Discussion
SPA, which have a cultural origin (Levy, 2009), provide previously unexplored approach to the urgent problem of obesity among older persons. For we found, as hypothesized, that those with more-positive SPA were significantly less likely to become obese than those with more-negative SPA.
The financial savings, and increased well-being, resulting from the reduction of obesity in later life could be considerable. Annual spending on obesity-related health costs for Americans aged 60 years and older is approximately $50 billion (Spieker and Pyzocha, 2016).
Future research could examine whether similar preventive benefits from SPA apply to other countries which have different patterns of later life obesity. Meanwhile, these results suggest that SPA could serve as the basis for an effective intervention aimed at mitigating the development of obesity among older persons living in the United States.
Acknowledgments
Acknowledgments
This study was supported by a National Institute on Aging grant (U01AG032284).
Conflict of interests
The authors declare that there are no conflicts of interest.
Dataset
The Health and Retirement Study is publicly available at: http://hrsonline.isr.umich.edu.
Contributor Information
Becca R. Levy, Email: Becca.Levy@yale.edu.
Martin D. Slade, Email: Martin.Slade@yale.edu.
References
- Han T.S., Tajar A., Lean M.E. Obesity and weight management in the elderly. Br. Med. Bull. 2011;97:169–196. doi: 10.1093/bmb/ldr002. [DOI] [PubMed] [Google Scholar]
- Hruby A., Manson J.E., Qi L. Determinants and consequences of obesity. Am. J. Public Health. 2016;106:1656–1662. doi: 10.2105/AJPH.2016.303326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kämpfen F., Jürgen M. Time to burn (calories)? The impact of retirement on physical activity among mature Americans. J. Health Econ. 2016;45:91–102. doi: 10.1016/j.jhealeco.2015.12.001. [DOI] [PubMed] [Google Scholar]
- Lawton M.P. The Philadelphia Geriatric Center Morale Scale: a revision. J. Gerontol. 1975;30:85–89. doi: 10.1093/geronj/30.1.85. [DOI] [PubMed] [Google Scholar]
- Levy B. Stereotype embodiment: a psychosocial approach to aging. Curr. Dir. Psychol. Sci. 2009;18:332–336. doi: 10.1111/j.1467-8721.2009.01662.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy B.R., Myers L.M. Preventive health behaviors influenced by self-perceptions of aging. Prev. Med. 2004;39:625–629. doi: 10.1016/j.ypmed.2004.02.029. [DOI] [PubMed] [Google Scholar]
- Levy B.R., Slade M.D., Kunkel S.R., Kasl S.V. Longevity increased by positive self-perceptions of aging. J. Pers. Soc. Psychol. 2002;83:261–270. doi: 10.1037//0022-3514.83.2.261. [DOI] [PubMed] [Google Scholar]
- Levy B.R., Pilver C., Chung P.H., Slade M.D. Subliminal strengthening: improving older individuals' physical function over time with an implicit-age-stereotype intervention. Psychol. Sci. 2014;25:2127–2135. doi: 10.1177/0956797614551970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn P.M., Seeley J.R., Roberts R.E., Allen N.B. Center for Epidemiological Studies_Depression Scale (CES_D) as a screening instrument for depression among community-residing older adults. Psychol. Aging. 1997;12:277–287. doi: 10.1037//0882-7974.12.2.277. [DOI] [PubMed] [Google Scholar]
- Liang J., Bollen K.A. The structure of the Philadelphia geriatric center morale scale: a re-interpretation. J. Gerontol. 1983;38:181–189. doi: 10.1093/geronj/38.2.181. [DOI] [PubMed] [Google Scholar]
- Radloff L.S. The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1:385–401. [Google Scholar]
- Robert Wood Johnson Foundation The state of obesity. 2018. https://stateofobesity.org/rates/recent
- Sonnega A., Weir D.R. Open Health Data. Vol. 2. 2014. The health and retirement study: a public data resource for research on aging; p. pe7. [Google Scholar]
- Spieker E.A., Pyzocha N. Economic impact of obesity. Prim. Care. 2016;43:83–95. doi: 10.1016/j.pop.2015.08.013. [DOI] [PubMed] [Google Scholar]
- Wurm S., Tomasik M.J., Tesch-Römer C. On the importance of a positive view on ageing for physical exercise among middle-aged and older adults: cross-sectional and longitudinal findings. Psychol. Health. 2008;25:25–42. doi: 10.1080/08870440802311314. [DOI] [PubMed] [Google Scholar]