Abstract
Background:
Gastrointestinal tract (GIT) is the most common extranodal site for non-Hodgkin's lymphoma (NHL) and constitutes about 10%-15% of all NHL. This was a prospective study to evaluate the epidemiological, clinicopathological characteristics, and treatment outcome of primary GIT diffuse large B-cell lymphoma (PGIL).
Materials and Methods:
Newly diagnosed patients of PGIL with DLBCL histology were eligible. Lugano staging system was used. All patients were treated with prephase treatment (1 mg vincristine and 100 mg prednisolone) followed by CHOP-based chemotherapy (with or without rituximab) as definitive treatment.
Results:
A total of 21 patients of PGIL were diagnosed. The median age was 46 years (range: 27–69 years) with male:female ratio of 2:1. Dull aching abdominal pain was the most common presenting complaint. Stomach was the most common site involved (52.4%, n = 11) followed by the colon (23.8%, n = 5). The estimated median survival in patients with Stage IV disease was significantly lower as compared to patients with localized disease (Stage I and II) (6.23 months vs. 23.4 months; P = 0.04). Patients, who did not achieve complete response (CR), had 15.5 times higher risk of death, as compared to those who achieved CR (P = 0.01).
Conclusions:
Stomach was the most common site for PGIL. Localized disease and CR after first-line chemotherapy were associated with better survival. A higher cost of rituximab was the prohibitive factor for cure in these patients.
Keywords: Diffuse large B-cell lymphoma, diffuse large B-cell lymphoma colon, diffuse large B-cell lymphoma stomach, gastrointestinal lymphoma
Introduction
Gastrointestinal tract (GIT) is the most common extranodal site for non-Hodgkin's lymphoma (NHL) constituting about 10%–15% of all NHLs and 30%–40% of all extranodal lymphoma.[1,2,3] Primary GIT lymphoma (PGIL) comprises only 3%–4% of all GIT malignancies, thus making it a rare entity. Stomach is the most common site of PGIL followed by small intestine and colon. Diffuse large B-cell lymphoma (DLBCL) is the most common histological subtype.[4] In 1961, Dawson et al. first proposed the diagnostic criteria to define PGIL. As per them, PGIL is a lymphoproliferative disorder which predominantly involves the GIT. They may involve lymph nodes which are confined to the drainage area of the primary tumor site. There should be no palpable peripheral lymph node. Liver or spleen should not be involved. Chest radiograph and the peripheral white cell count should be normal.[5] The optimal treatment of PGIL is a matter of debate. Surgery was the main treatment modality in the past, but now, it is replaced by the combination of anthracycline-containing chemotherapy and anti-CD20 antibody, rituximab.[6] Consolidation therapy with radiation is recommended in patients with localized disease.[7] This study was performed to know the incidence, clinicopathological characteristics, treatment pattern, and outcome of PGIL patients at a tertiary care center in India.
Materials and Methods
Study type
This was a prospective descriptive study carried out at Kidwai Cancer Institute, Bengaluru, India, from January 2016 to December 2017.
Objectives
To study the epidemiological, pathological, and clinical characteristics of PGIL patients
To study the treatment pattern and outcome among PGIL patients.
Eligibility criteria
Newly diagnosed patients of PGIL with DLBCL histology were eligible. Patients with secondary involvement of GIT were not eligible. Low-grade lymphoma (like marginal zone lymphoma) with transformation to DLBCL was excluded.
Method
All patients with suspected GIT malignancies underwent clinical examination after taking detailed medical history. Depending on the location of the tumor, diagnostic endoscopy was performed (upper GI endoscopy or colonoscopy). When the disease was confined to nonaccessible sites, such as small intestine, Tru-cut biopsy or laparoscopic biopsy of the involved part was performed. Patients presenting with GI obstruction, GI perforation, or massive hemorrhage were the candidates for upfront surgery.
Diagnosis of DLBCL was made after the histopathological examination with hematoxylin and eosin stain followed by immunohistochemistry (IHC) markers (LCA, CD20, PAX 5, CD3, CD10, BCL2, BCL6, MUM1, MYC, and cyclin D1). All cases were divided into germinal center B-cell (GCB) and Non-GCB (NGCB) subtypes of DLBCL using Hans algorithm.[8] The proliferative index was assessed using Ki-67 by counting 1000 cells and calculating the percentage of positively stained cells. Cases with IHC positive for MYC and BCL2 will be called double expresser DLBCL.[9]
Computed tomography (CT) scan or positron emission tomography (PET)/CT was used for staging purpose. Bone marrow biopsy was performed from unilateral iliac crest. Lugano staging system was used for assigning the stage.[10] All patients underwent routine blood investigations (complete blood count, serum urea, creatinine, liver function test, and uric acid serum lactate dehydrogenase [LDH]) before chemotherapy. Written consent was obtained from all patients for participation in the study.
Treatment and assessment
All patients received prephase treatment followed by definitive chemotherapy. Prephase treatment consisted of one dose of vincristine (1 mg) on day 6 as intravenous push and prednisolone 100 mg oral from day 6 to day 0.[11] As definitive chemotherapy, all patients received chemotherapy CHOP with or without rituximab repeated every 21 days for a total of six cycles. CHOP chemotherapy consists of cyclophosphamide 750 mg/m2 on day 1, doxorubicin 50 mg/m2 on day 1, vincristine 1.4 mg/m2 up to a maximum dose of 2 mg on day 1, rituximab 375 mg/m2 on day 1, and prednisone 100 mg/day orally on days 1–5.[12] Institutional protocol was followed for the prevention of chemotherapy-induced emesis. All patients above 60 years received prophylactic growth factor. Radiotherapy after chemotherapy was given as per the treating physician's discretion and case-to-case basis.
At the end of three cycles of chemotherapy, reassessment imaging (CT and PET/CT) was performed. Responding patients (complete response [CR]/unconfirmed CR and partial response [PR]) were planned for the continuation of chemotherapy. Patients with progressive disease (either at interim reassessment or at the completion of chemotherapy) were offered salvage chemotherapy followed by autologous stem cell transplantation. Patients were followed up every 3 monthly with physical examination and serum lactate dehydrogenase measurement.
Statistical analysis
Comparisons of clinicopathological variables were performed by Chi-square or Fisher's exact test for nominal variables. Survival was assessed using Kaplan–Meier method. Log-rank test was used to compare the survival between subgroups. P < 0.05 (two-sided) was considered to be statistically significant.
Results
A total of 21 patients of PGIL were diagnosed. The median age was 46 years (range: 27–69 years). Fifteen patients were male, while six patients were female (male:female = 2:1). Dull aching abdominal pain or discomfort was the most common complaint followed by decreased appetite and weight loss. Four patients presented with acute onset abdominal pain and underwent laparotomy at the time of presentation (3, small intestinal DLBCL and 1, colon DLBCL). Stomach was the most common site involved (52.4%, n = 11), followed by colon (23.8%, n = 5), small intestine (19.0%, n = 4), and esophagus (4.8%, n = 1). Based on Hans algorithm, 11 patients (52.4%) had GCB subtype, while 10 patients (47.6%) had NGCB subtype. MYC expression was assessed. Double expresser phenotype (concomitant expression of MYC and BCL2) was present in 28.6% (n = 6) of patients. There was a positive correlation between the Ki-67 index and MYC expression value (Pearson coefficient = 0.57). As per the Lugano staging system, 9.5% (n = 2) patients belonged to Stage IE, 66.7% (n = 14) patients had Stage IIE, and remaining 23.8% (n = 5) patients had Stage IV disease at presentation.
All patients received CHOP-based chemotherapy. Only five patients received rituximab along with CHOP chemotherapy. Out of 21 patients, 5 patients underwent surgery before definitive chemotherapy.
Among patients who presented with localized disease (Stage I and II, n = 16), 68.7% achieved CR, 25% achieved PR, and 6.3% are still receiving chemotherapy. Only one patient received radiotherapy after completion of chemotherapy.
Patients who presented with advanced disease (Stage IV, n = 5) responded poorly to chemotherapy. None of the patients in this group received rituximab. One patient had CR, two patients had PR, and one patient had progressive disease after completion of chemotherapy. One patient is still receiving chemotherapy.
After median follow-up of 9.2 months (range: 3.3–24.1 months), 61.9% (n = 13) patients were alive. The expected median survival was 23.4 months [Figure 1]. The estimated median survival in patients with Stage IV disease was significantly lower as compared to patients who presented with localized disease (Stage I and II) (6.2 months vs. 23.4 months; P = 0.04). On univariate analysis double expression phenotype, GCB and NGCB, age, sex, site, and baseline LDH were not associated with risk of death. Patients who did not achieve CR had 15.5 times higher risk of death as compared to those who achieved CR (P = 0.01).
Figure 1.
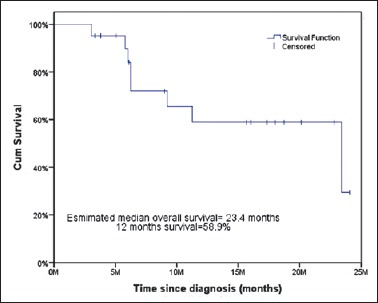
Overall survival of the patients with primary gastrointestinal diffuse large B-cell lymphoma
Discussion
PGILs are uncommon malignancies. GIT is the most common extranodal site involved by DLBCL. The incidence of PGIL is increasing as observed in population-based registries.[13] The median age in our study was 46 years which is consistent with other studies.[14] The stomach is the most common site involved in PGIL (37.8%–86%).[15] In our study also, stomach was the most common site involved (52.4%), followed by small intestine and esophagus. The nonspecific symptoms of abdominal pain, decreased appetite, and weight loss lead to delay in diagnosis.[16] Another difficulty for accurate diagnosis of PGIL is the variation in endoscopic abnormalities, which varies from minimal mucosal irregularities to bigger ulcerations making identification of primary tumor difficult.
The management of PGIL is controversial. Historically, surgery was used for radical treatment, but the results of a controlled clinical trial demonstrated that the outcome following chemotherapy (10-year survival rate of 92%) was superior to that of surgery alone or surgery in combination with chemotherapy (10-year survival rate of 28% and 82%, respectively). Hence, chemotherapy is considered the optimum treatment for PGIL.[17] Rituximab, a chimeric anti-CD20 antibody when added to standard chemotherapy (CHOP), improves the survival of GIT lymphoma.[18] Radiation therapy as consolidation after completion of chemotherapy improves the disease-free survival and overall survival. The cost of rituximab is still a major obstacle in the cure of PGIL in developing countries. In our study, 24% of patients received rituximab. Hence, the estimated median survival in our study is low (23.4 months) as compared to Western literature. Localized disease and CR to first-line chemotherapy were most important prognostic factors in our study.
Conclusions
Stomach was the most common site for PGIL. Localized disease and CR after first -line chemotherapy were associated with better survival. A higher cost of rituximab was the prohibitive factor for cure in these patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank Dr. Abhilasha Goyal for her help in writing this manuscript.
References
- 1.d’Amore F, Brincker H, Grønbaek K, Thorling K, Pedersen M, Jensen MK, et al. Non-Hodgkin's lymphoma of the gastrointestinal tract: A population-based analysis of incidence, geographic distribution, clinicopathologic presentation features, and prognosis. Danish lymphoma study group. J Clin Oncol. 1994;12:1673–84. doi: 10.1200/JCO.1994.12.8.1673. [DOI] [PubMed] [Google Scholar]
- 2.Bautista-Quach MA, Ake CD, Chen M, Wang J. Gastrointestinal lymphomas: Morphology, immunophenotype and molecular features. J Gastrointest Oncol. 2012;3:209–25. doi: 10.3978/j.issn.2078-6891.2012.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ghimire P, Wu GY, Zhu L. Primary gastrointestinal lymphoma. World J Gastroenterol. 2011;17:697–707. doi: 10.3748/wjg.v17.i6.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arora N, Manipadam MT, Pulimood A, Ramakrishna BS, Chacko A, Kurian SS, et al. Gastrointestinal lymphomas: Pattern of distribution and histological subtypes: 10 years experience in a tertiary centre in South India. Indian J Pathol Microbiol. 2011;54:712–9. doi: 10.4103/0377-4929.91502. [DOI] [PubMed] [Google Scholar]
- 5.Dawson IM, Cornes JS, Morson BC. Primary malignant lymphoid tumours of the intestinal tract. Report of 37 cases with a study of factors influencing prognosis. Br J Surg. 1961;49:80–9. doi: 10.1002/bjs.18004921319. [DOI] [PubMed] [Google Scholar]
- 6.Avilés A, Díaz-Maqueo JC, de la Torre A, Rodriguez L, Guzmán R, Talavera A, et al. Is surgery necessary in the treatment of primary gastric non-Hodgkin lymphoma? Leuk Lymphoma. 1991;5:365–9. doi: 10.3109/10428199109067630. [DOI] [PubMed] [Google Scholar]
- 7.Li Q, Li W, Wang L, Wang W, Niu S, Bi X, et al. Consolidation radiotherapy in stage IE-IIE, non-bulky primary gastric diffuse large B-cell lymphoma with post-chemotherapy complete remission. PLoS One. 2015;10:e0133469. doi: 10.1371/journal.pone.0133469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hans CP, Weisenburger DD, Greiner TC, Gascoyne RD, Delabie J, Ott G, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood. 2004;103:275–82. doi: 10.1182/blood-2003-05-1545. [DOI] [PubMed] [Google Scholar]
- 9.Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al., editors. Revised 4th ed. Lyon: IARC; 2017. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. [Google Scholar]
- 10.Rohatiner A, d’Amore F, Coiffier B, Crowther D, Gospodarowicz M, Isaacson P, et al. Report on a workshop convened to discuss the pathological and staging classifications of gastrointestinal tract lymphoma. Ann Oncol. 1994;5:397–400. doi: 10.1093/oxfordjournals.annonc.a058869. [DOI] [PubMed] [Google Scholar]
- 11.Lakshmaiah KC, Asati V, Babu K G, D Lokanath. Role of prephase treatment prior to definitive chemotherapy in patients with diffuse large B-cell lymphoma. [Last accessed on 2018 Jul 07];Eur J Haematol. 2018 100:644–648. doi: 10.1111/ejh.13068. Available from: https://doi.org/10.1111/ejh.13068 . [DOI] [PubMed] [Google Scholar]
- 12.Fisher RI, Gaynor ER, Dahlberg S, Oken MM, Grogan TM, Mize EM, et al. Comparison of a standard regimen (CHOP) with three intensive chemotherapy regimens for advanced non-Hodgkin's lymphoma. N Engl J Med. 1993;328:1002–6. doi: 10.1056/NEJM199304083281404. [DOI] [PubMed] [Google Scholar]
- 13.Gurney KA, Cartwright RA, Gilman EA. Descriptive epidemiology of gastrointestinal non-Hodgkin's lymphoma in a population-based registry. Br J Cancer. 1999;79:1929–34. doi: 10.1038/sj.bjc.6690307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gou HF, Zang J, Jiang M, Yang Y, Cao D, Chen XC, et al. Clinical prognostic analysis of 116 patients with primary intestinal non-Hodgkin lymphoma. Med Oncol. 2012;29:227–34. doi: 10.1007/s12032-010-9783-x. [DOI] [PubMed] [Google Scholar]
- 15.Koch P, del Valle F, Berdel WE, Willich NA, Reers B, Hiddemann W, et al. Primary gastrointestinal non-Hodgkin's lymphoma: I. Anatomic and histologic distribution, clinical features, and survival data of 371 patients registered in the German multicenter study GIT NHL 01/92. J Clin Oncol. 2001;19:3861–73. doi: 10.1200/JCO.2001.19.18.3861. [DOI] [PubMed] [Google Scholar]
- 16.Shawky H, Tawfik H. Primary gastrointestinal non-Hodgkin's lymphoma: A Retrospective study with emphasis on prognostic factors and treatment outcome. J Egypt Natl Canc Inst. 2008;20:330–41. [PubMed] [Google Scholar]
- 17.Avilés A, Nambo MJ, Neri N, Huerta-Guzmán J, Cuadra I, Alvarado I, et al. The role of surgery in primary gastric lymphoma: Results of a controlled clinical trial. Ann Surg. 2004;240:44–50. doi: 10.1097/01.sla.0000129354.31318.f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li X, Shen W, Cao J, Wang J, Chen F, Wang C, et al. Treatment of gastrointestinal diffuse large B cell lymphoma in China: A 10-year retrospective study of 114 cases. Ann Hematol. 2012;91:1721–9. doi: 10.1007/s00277-012-1507-1. [DOI] [PubMed] [Google Scholar]


