Abstract
Background:
Rising mental health costs have brought with them the pressing need to identify cost-effective treatments. Identifying cost-effective treatments for depression among Latinos is particularly relevant given substantial disparities in access to depression treatment for Latinos compared to non-Latino whites.
Aims:
The goal of this paper is to (i) compare the cost-effectiveness of telephone and face-to-face cognitive behavioral therapy (CBT) for depression to usual care received in primary care; (ii) compare the cost-effectiveness of telephone CBT directly to face-to-face CBT.
Methods:
As part of a randomized trial study, primary care patients with depression were randomized into three groups: usual care, telephone CBT and face-to-face CBT. Incremental cost-effectiveness ratios (ICER) between respective groups are computed by dividing the incremental difference in mental health care costs by the incremental difference in mental health outcomes. Mental health care costs are computed as the sum of intervention costs (cost of administering sessions) and non-intervention costs (cost of mental health services used that are not part of the intervention). Prices for different types of mental health services are taken from the 2010 Medical Expenditure Panel Survey. Mental health costs are estimated using two-part models. Mental health outcomes are measured by two depression scales: Patient Health Questionnaire (PHQ-9) and Hopkins Symptom Checklist (HSCL), and are estimated using multiple linear regression models. The standard errors for ICERs are computed using 1000 bootstrapped samples and the delta method.
Results:
Each CBT intervention group is significantly more costly compared to usual care in terms of mental health care costs. Face-to-face CBT patients cost $732 more than usual care, and phone CBT patients cost $237 more than usual care. In terms of effectiveness, both intervention groups are associated with significantly reduced (improved) scores in PHQ9 and HSCL compared to usual care. Comparing the phone therapy directly to the same treatment offered face-to-face, we find that phone CBT is significantly less costly (by $501) and more cost effective than face-to-face when effectiveness is measures by improvement in PHQ9 scores. Specifically, for the phone CBT group, one score reduction in PHQ9 costs $634 less than face-to-face.
Discussion:
One limitation is that we observe the mental health service use of patients for only four months. Phone CBT might potentially lead to substantial savings or even cost-offset in the long-run. Additional studies with long-run service use data are needed to establish these findings.
Implication for Health Policy:
The finding that phone-based intervention is able to improve the depressive symptoms of patients just as effectively as face-to-face by spending less is crucial for policy makers and health institutions looking to adopt cost-effective depression treatments.
Introduction
As part of the Affordable Care Act (ACA), approximately 30 million uninsured individuals will become eligible for insurance coverage,1 with an estimated fifth to a quarter suffering from a mental health or substance use disorders.2 The expected rise in demand for mental health services have generated concern regarding the adequate supply of providers, rising expenditures for these services and the need to identify cost-effective treatments. Spending on mental health and substance abuse treatments increased from $84 billion to $172 billion from 1998 to 2009.3 One potential strategy for reducing costs and dealing with the limited supply of providers has been the use of telephone-based cognitive behavioral therapy (CBT).4 Telephone-based psychotherapy has been shown to significantly improve depression scores and mood,5–6 with a small number of studies finding that telephone based treatment is as effective as face-to-face treatment in improving depression outcomes.7,8 This paper is one of the first studies to compare the cost-effectiveness of telephone based CBT treatments to traditional face-to-face CBT treatments for depression.
Specifically, the focus of this paper is to examine and compare the cost-effectiveness of the telephone and face-to-face CBT interventions to treat depression among Latinos. Latino population is of interest since there are persistent disparities in depression care for Latinos compared to whites.9,10 Although depression prevalence rates are comparable between Latinos and non-Latino whites,11 and there is strong support for the effectiveness of CBT treatments for Latinos,12 very few Latinos access treatment.11
As part of a randomized trial of treatment for depression among Latinos (CERED*), primary care patients with depression were randomized into three groups: usual care, telephone CBT and face-to-face CBT. Usual care participants received the regular care from their primary care provider which might potentially include medications but not CBT treatment. Telephone and face-to-face participants got the CBT interventions on top of the primary care they received. Alegria et al.8 show that both types of interventions were effective in improving depression symptoms compared to usual care in primary care.
The goal of this paper is to answer two questions regarding the costs and cost-effectiveness of the study. First, we examine the costs and cost-effectiveness of each form of CBT intervention compared to usual care, separately. Second we explore whether the telephone intervention is more cost-effective than face-to-face by comparing the two intervention groups directly. The goal is to evaluate whether it costs less to achieve the same level of improvement in mental health scores using the telephone CBT compared to face-to-face CBT. Evidence regarding the cost-effectiveness of different types of depression treatment for Latinos will be crucial for policy makers in their efforts to increase treatment rates and decrease disparities.
The cost-effectiveness literature has explored the cost-effectiveness of randomized interventions to treat different mental disorders such as panic disorder,13–16 generalized anxiety disorder,17,18 psychosis,19 and depression.20–22 To the best of our knowledge, few studies explore the cost-effectiveness of an intervention to treat depression among Latinos.23 In addition, this paper extends the scope of related literature in cost-effectiveness by being one of the first to compare the cost-effectiveness of a telephone based intervention to face-to-face intervention.
In our analysis, intervention costs include the time costs incurred by patients to attend the sessions in addition to the cost of administering the sessions. By including patient time costs in our analysis, we take a social cost perspective; patient time costs are included in cost-effectiveness studies with a social perspective.23,24 Costs do not, however, include one-time research costs associated with recruitment, outreach or data collection.
Study Background
CERED (Comparative Effectiveness Research for Eliminating Disparities) is a randomized controlled trial designed to test the comparative effectiveness of a telephone-based intervention compared to the face-to-face intervention to treat depression among Latinos.8 The screening and enrollment process followed CONSORT guidelines*. Recruitment began in May 2011 with the final interviews completed in September 2012. Adult Latino patients (aged 18+) with depression were recruited from multiple clinics in two sites, Boston, Massachusetts and San Juan, Puerto Rico. Specifically, patients were recruited if they scored 10 or more in the Patient Health Questionnaire 9, met initial screening criteria for Major Depressive Disorder, had no psychosis or suicidal thoughts, and had not been in specialty mental health treatment within the last 3 months.
After the patients agreed to participate, they completed a baseline interview. The initial baseline interview assessed socio-demographic characteristics, depression, anxiety symptoms, trauma exposure, functional impairment, mental health service use and medication use†. After completing the baseline interview, patients were randomized into one of three groups: usual care, telephone CBT or face-to-face CBT. The usual care group received the typical standard of care from their primary care provider that potentially included antidepressant medication or brief counseling. The other two groups received a CBT intervention in addition to the usual care they received in primary care, called Engagement and Counseling for Latinos (ECLA) by telephone (ECLA-T) or face-to-face (ECLA-F). The ECLA consisted of six to eight sessions of CBT including psycho-education on depression, activities that decrease depressed mood, and challenging negative thoughts. The first four intervention sessions were conducted weekly, while the 5th and 6th sessions were conducted every two weeks unless the clinician felt the patient needed more immediate care. If the patient did not report improvement in depressive symptoms in the first six sessions, sessions were continued up to a total of 8 sessions.
Patients completed two follow up interviews at two and four months after the baseline interview. Follow up interviews assessed the same mental illness measures and symptoms as the baseline interview. For the purpose of this study, we limit effectiveness outcomes to reduction in depression symptoms as measures by the Patient Health Questionnaire (PHQ-9) and the Hopkins Symptom Checklist (HSCL).
Data
The final dataset includes a total of 257 patients across two sites with 86 in usual care, 84 in face-to-face, and 87 in phone intervention groups. Patients are comparable across the three study groups on socio-demographic characteristics including age, gender, education, employment status and income (Table 1). Overall, the majority of the patients are female (81.7%), aged 35–64 (71.2%), and only 16.3% are employed full-time (Table 1).
Table 1.
Summary Statistics for Demographic Variables and Outcomes by Study Group
| Demographics | Usual care | Face-to-face | Phone | p-value* | Total | ||||
|---|---|---|---|---|---|---|---|---|---|
| n=86 | % | n=84 | % | n=87 | % | n=257 | % | ||
| Sex | |||||||||
| Male | 15 | 17.4% | 19 | 22.6% | 13 | 14.9% | 0.417 | 47 | 18.3% |
| Female | 71 | 82.6% | 65 | 77.4% | 74 | 85.1% | 210 | 81.7% | |
| Age | |||||||||
| 18–34yr | 19 | 22.1% | 20 | 23.8% | 25 | 28.7% | 0.831 | 64 | 24.9% |
| 35–49yr | 32 | 37.2% | 30 | 35.7% | 32 | 36.8% | 94 | 36.6% | |
| 50–64yr | 30 | 34.9% | 32 | 38.1% | 27 | 31.0% | 89 | 34.6% | |
| > = 65yr | 5 | 5.8% | 2 | 2.4% | 3 | 3.4% | 10 | 3.9% | |
| Race (all are Latino) | |||||||||
| White | 27 | 31.4% | 22 | 26.2% | 24 | 27.6% | 0.697 | 73 | 28.4% |
| Black/Dark-skinned | 29 | 33.7% | 27 | 32.1% | 30 | 34.5% | 86 | 33.5% | |
| Unreported (only indicated Latino) | 28 | 32.6% | 28 | 33.3% | 26 | 29.9% | 82 | 31.9% | |
| Mixed/American Indian | 2 | 2.3% | 7 | 8.3% | 7 | 8.0% | 16 | 6.2% | |
| Education | |||||||||
| 6th grade or less | 18 | 21% | 20 | 24% | 20 | 23% | 0.240 | 58 | 23% |
| 7–11th grade | 23 | 27% | 31 | 37% | 20 | 23% | 74 | 29% | |
| HS diploma, GED, voc. or more | 45 | 52% | 33 | 39% | 47 | 54% | 125 | 49% | |
| Employment status | |||||||||
| Full-time | 17 | 19.8% | 14 | 16.7% | 11 | 12.6% | 0.676 | 42 | 16.3% |
| Part-time | 19 | 22.1% | 21 | 25.0% | 20 | 23.0% | 60 | 23.3% | |
| Unemployed | 15 | 17.4% | 10 | 11.9% | 20 | 23.0% | 45 | 17.5% | |
| Out of labor force | 29 | 33.7% | 30 | 35.7% | 26 | 29.9% | 85 | 33.1% | |
| Illness/disabled | 6 | 7.0% | 9 | 10.7% | 9 | 10.3% | 24 | 9.3% | |
| Personal Income | |||||||||
| < 15k | 67 | 77.9% | 61 | 72.6% | 68 | 78.2% | 0.576 | 196 | 76.3% |
| 15k-35k | 12 | 14.0% | 13 | 15.5% | 11 | 12.6% | 36 | 14.0% | |
| 35–75k | 5 | 5.8% | 3 | 3.6% | 2 | 2.3% | 10 | 3.9% | |
| Unreported | 2 | 2.3% | 7 | 8.3% | 6 | 6.9% | 15 | 5.8% | |
| Site | |||||||||
| Boston | 43 | 50.0% | 41 | 48.8% | 43 | 49.4% | 0.988 | 127 | 49.4% |
| Puerto rico | 43 | 50.0% | 43 | 51.2% | 44 | 50.6% | 130 | 50.6% | |
| Outcomes | Mean | SD | Mean | SD | Mean | SD | p-value | Mean | SD |
| MH care costs | $237 | $540 | $986 | $748 | $498 | $352 | 0.00 | $570 | $645 |
| #MH services used (non-intervention) | 1.37 | 2.39 | 2.14 | 3.87 | 0.89 | 1.95 | 0.02 | 1.46 | 2.88 |
| Baseline HSCL | 1.78 | 0.88 | 1.93 | 0.98 | 1.92 | 0.86 | 0.48 | 1.88 | 0.91 |
| Baseline PHQ9 | 15.96 | 3.97 | 17.42 | 4.45 | 16.77 | 4.26 | 0.08 | 16.71 | 4.26 |
p-values for demographic variables computed by chi-squared test; p-values for continuous variables computed by one-way ANOVA.
There are, however, significant differences across sites in terms of a few specific characteristics. Puerto Rico participants have a higher percentage of people who are out of labor force and earn less than $15,000 (data not shown). We control for site in all our analysis to account for site differences.
Cost Measures
Mental health (MH) care costs are computed as the sum of non-intervention costs and intervention costs. Non-intervention costs are MH service use costs that are not part of the intervention. Specifically, they are the self-reported monetary costs of mental health services patients used in the four months prior to the final interview. In related literature, it is quite common to use self-reports for utilization of services.21,23,25 Fenton et al.25 checks the validity of patient reports to service volume estimates derived from other sources and finds that patient self-reports correlate highly with the standard estimates.
We include the patient-reported number of MH services used for five types of service categories: primary care visits related to mental health, psychologist/therapist visits, psychiatrist visits, emergency department visits, and medication prescriptions. Price per each type of service is taken from the average expenditures reported in 2010 Medical Expenditure Panel Survey (MEPS), and then applied to our data to monetize the quantities of services reported by participants. One important thing to note is that expenditures reported in MEPS are based on payments, not charges. Payments are actually a better representative of costs than charges given that they more accurately reflect the dollars spent on a service.26 Table 2, Panel 1 shows the average prices from MEPS assigned to each of the five MH service categories.
Table 2.
Mental Health Care Costs Assigned to Each Type of Service
| Non-intervention costs | ||
| Service type | Average cost (per service) | Source |
| Primary care visit | $122.34 | Based on average expenditures reported in Medical Expenditure Panel Survey (MEPS) 2010 for each mental health care category |
| Psychologist visit | $136.63 | |
| Psychiatrist visit | $146.39 | |
| ER visit | $687.34 | |
| Rx (prescription) | $39.91 | |
| Intervention costs | ||
| Service type | Average cost (per service) | Source |
| Psychologist visit (face-to-face) | $136.63 | Based on average expenditures reported in Medical Expenditure Panel Survey (MEPS) 2010 for each mental health care category |
| Psychologist visit (phone) | $68.32 | |
| Time costs (face-to-face) | 1.5 hours | Patients time was priced using reported hourly wage |
| Time costs (phone) | 1 hour | |
The second component of MH care costs are the intervention costs, namely the cost of administering the individual CBT sessions and the cost of patient time lost during these sessions. Cost of administering a session is once again taken from MEPS. Specifically, we take the average price per individual psychologist/social worker visit from MEPS ($136.63) and assign it to the number of face-to-face sessions each patient completed. For telephone sessions, we assign half the price of regular psychologist/social worker visits ($68.32) as it was done in Katon et al. 2006.13 Given the lack of publicly available data on the cost of this type of therapy, we follow the previous literature and price telephone sessions at half the value of regular sessions. To ensure this pricing strategy is not driving the estimated cost advantages of phone CBT compared to in-person CBT, we performed a sensitivity check and estimated the model by pricing phone therapy at 90% of the cost of regular therapy. The overall trends and significance of findings remained the same.*
One advantage of telephone CBT compared to in-person CBT is that it saves time for patients. Patients save on transportation time and waiting time associated with face-to-face CBT. Each telephone session is assigned one hour of patient time since the CBT intervention takes one hour on average. We assign one and a half hours of patient time to each face-to-face session assuming transportation and waiting time is half an hour. Assigning a time period of half an hour to transportation and waiting is quite short compared to the literature.24,27 We wanted to keep the transportation and waiting time short to ensure we do not over-estimate the time-saving advantages of phone CBT compared to in-person. Patient time is priced using the reported hourly wage for each patient. Unemployed participants’ time is priced using the gender and site specific average hourly wage following the literature.20,23 Table 2, Panel 2 shows the average prices and patient times assigned to each face-to-face and phone session. Following the literature, research-specific costs associated with recruitment and outreach (material costs, reimbursements for taxi fares or cell phone minutes, etc.) are excluded from the analysis.13,23 These costs generally are excluded in the cost-effectiveness analysis since they wouldn’t be incurred in any possible real-life adoption of the interventions.
Effectiveness Measures: PHQ9 and HSCL
The measures used to assess the effectiveness of the intervention in improving depression outcomes are the Patient Health Questionnaire 9 (PHQ-9) and the Hopkins Symptom Checklist (HSCL-20). In cost-effectiveness studies, effectiveness is generally measured in quality adjusted life years (QALYs). Since we don’t have the necessary information in our dataset to compute QALYs, we use the 1-unit change in these two widely used scales to measure effectiveness of treatment. Specifically, ICERs are computed in terms of $ per 1-unit improvement in PHQ-9 or HSCL-20 scores. Several other papers in related literature also measured effectiveness by 1-unit improvements in mental health scores.14,28
PHQ-9 is a 9-item screening questionnaire that is widely used in primary care settings to determine the level of depressive disorder.29–31 It measures depression following DSM-IV criteria. Scores can range from 0 to 27, lower scores indicating lower levels of symptom severity. Scores greater than 20 are classified as indicating potentially severe major depressive disorder.
The HSCL-20 is a 20-item assessment depression scale comprised of the 13-items of the Hopkins Symptom Checklist Depression Scale and 7 additional items from the Hopkins Symptom Checklist-90-Revised.32 The HSCL-20 was designed to assess all diagnostic symptoms of depression and is widely used in the literature.6,13,33–39 HSCL-20 items are rated on a five-point scale and are assessed for the time period of previous 2 weeks. Responses are scored from 0 to 4. All items are averaged for a total score of 0–4, with higher scores indicating greater levels of depression.
Methods
The estimation methodology involves three main steps. First, we estimate the incremental effect of being in an intervention group on mental health outcomes PHQ9 and HSCL. Second, we estimate the incremental effect of being in an intervention group on MH care costs. Third, we compute the incremental cost-effectiveness ratios between the relevant study groups by dividing the incremental change in MH care costs by the incremental change in mental health outcomes. The ICER are in units of the form $/PHQ9 score and $/HSCL score.
First, to analyze the impact of the CBT intervention on effectiveness, we use multiple linear regression models. The outcome measures of interest are the values of the two depression measures (PHQ-9, HSCL) reported in the final interview. Respective baseline values of each depression measure (baseline PHQ-9 and HSCL) and a control for site are included as covariates in the regressions. Other socio-demographic characteristics are not used in regressions since patients are balanced in terms of socio-demographic characteristics after randomization as seen in Table 1. Sensitivity analysis conducted controlling for these covariates (i.e. age, sex, race/ethnicity and education level) showed that the results are not sensitive to the inclusion of these covariates. The magnitude and significance of our findings were essentially the same.
The model can be summarized by the following specification:
| (1) |
where Yif is the mental health outcome (PHQ-9 or HSCL) of patient i in the final assessment; Face to face and Phone are indicators for the two CBT intervention groups making usual care the reference group; Yib is the mental health outcome of patient i in baseline interview; and Sitei is an indicator for site (Boston vs. Puerto Rico). Estimated incremental effects and their standard errors as shown in Table 3 Columns (2) and (3) are based on the regression coefficients β1 and β2. Regression adjusted averages for usual care patients are computed using standardized predictions generated from regression coefficients.* To estimate the incremental effect of being in the phone group compared to face-to-face, we drop the usual care participants from the analysis and run the same regression as in Equation (1) without the indicator variable Face to face.
Table 3.
Incremental Effect of Being in Intervention Group on Outcome Measures
| Incremental Effects | ||||
|---|---|---|---|---|
| (1) average under usual care |
(2) incremental effect of face-to-face compared to usual care |
(3) incremental effect of phone compared to usual care |
(4) incremental effect ofphone compared to face-to-face |
|
| Cost measure | ||||
| MH care costs | $239.80 | $731.86*** | $236.76*** | − $501.18*** |
| p-value | 0.000 | 0.000 | 0.000 | |
| Effectiveness measures | ||||
| PHQ9 score | 11.75 | − 2.30* | − 2.98** | − 0.79 |
| p-value | 0.020 | 0.003 | 0.429 | |
| HSCL score | 1.52 | − 0.27* | − 0.33** | − 0.06 |
| p-value | 0.031 | 0.010 | 0.671 |
Notes:
p <.001,
p <.01,
p <.05
Second, we estimate the incremental effect of being in a CBT intervention group on MH care costs. Predicted MH care costs are estimated using two-part models. Two-part models are widely used in modeling costs since the characteristics of cost data such as restricted range (nonnegative observations), spike of zero values and skewness make ordinary least squares estimation biased and inefficient.40 Explicitly, two-part models model the probability of nonzero costs separately from their level conditional on nonzero costs.41,42 The first part of the model predicts the probability of any use (positive MH care costs) using a probit model. In practice, the outcome measure is an indicator variable taking the value of 1 if MH care costs are positive. From this probit regression, the predicted probability of having positive costs is estimated. In terms of econometric notation, the probit regression is of the form
| (2) |
where yi represents MH care costs, x is the vector of explanatory variables including baseline HSCL score and control for site, and is the cumulative distribution function of the standard normal.
The second part of the model is estimated using a Generalized Linear Model (GLM)43–45 with a log link function.40 We use the gamma distributional family to reflect the mean-variance relationship as implied by the results of our Park test (λ = 1:8). The second part predicts the level of costs conditional on nonzero costs. The formal specification of the model is given below.
| (3) |
Once the two parts of the model are estimated, unconditional predicted MH care costs are obtained by multiplying the probabilities of use from the first part by the expected levels from the second part as in Equation (4). The standard errors for incremental effects in the two-part model are computed using the delta method.46
| (4) |
Finally, we compute the incremental cost-effectiveness ratios (ICER) between the relevant intervention groups by dividing the estimated incremental effect on MH care costs by the estimated incremental effect on MH outcomes. ICER are in units of the form $/phq9 score. Specifically,
The standard errors for ICERs are computed by first creating 1000 bootstrapped estimates of incremental changes in MH care costs and effectiveness measurers, and then using first order Taylor expansion and delta method to compute the variance of each ratio as specified below.13
Results
Summary statistics on socio-demographic characteristics including age, gender, education, employment status and income are presented in Table 1, Panel 1. The majority of the patients in the sample are female (81.7%), and only 16.3% are employed full-time. Socio-demographic characteristics are balanced across the three study groups.
Unadjusted summary statistics for MH care costs, number of services used (non-intervention) and baseline mental health scores are shown in Table 1, Panel 2. MH care costs and number of services used differ significantly across the three study groups (p=0.00 and 0.02 respectively). Both intervention groups are more costly than usual care. This is not surprising since MH care costs include the cost of administering the intervention sessions and patient time which are not incurred by the usual care participants. Phone group patients use a smaller number of MH services on average (0.89) compared to usual care (1.37), whereas face-to-face group patients use more (2.14). The three study groups are balanced in terms of baseline PHQ9 and HSCL scores.
Table 3 shows the estimated incremental effect of being in each intervention group compared to usual care on costs and effectiveness measures, along with the incremental effect of being in the phone CBT group compared to face-to-face CBT. The estimates are derived from regression models that control for baseline mental health severity and site differences as explained in the previous section.
Columns (2) and (3) of Table 3 compares each intervention group to usual care separately. Estimates show that each intervention group is significantly more costly compared to usual care. Specifically, face-to-face group patients cost $732 more on average than usual care, and phone group patients cost $237 more than usual care.
Estimated incremental effects of the intervention on PHQ9 and HSCL scores reveal that both intervention groups are associated with significant improvement in MH outcomes. Being in the face-to-face group is associated with a 2.30 point reduction in PHQ9 score compared to usual care, whereas being in phone group is associated with a 2.98 point reduction. For HSCL, being in face-to-face and phone groups are associated with a 0.27 and 0.33 point reduction compared to usual care, respectively.
Column (4) of Table 3 compares the phone CBT group to the face-to-face CBT group. Estimates show that phone intervention is significantly less costly than face-to-face in terms of MH care costs. Specifically, phone group patients cost $501 less in terms of MH care costs compared to face-to-face. This is a rather important finding given that the level of effectiveness does not differ significantly between the two intervention groups. Phone intervention is as effective as face-to-face with significantly reduced costs.
Incremental cost-effectiveness ratios between each intervention group and usual care, and between the two intervention groups are presented in Table 4. As mentioned before, these ratios are computed by dividing the incremental change in MH care costs, by the incremental change in respective mental health outcomes (HSCL and PHQ-9).
Table 4.
Incremental Cost Effectiveness Ratios (ICER)
| (1) face-to-face vs. usual care |
(2) telephone vs. usual care |
(3) telephone vs. face-to-face |
|
|---|---|---|---|
| ICER ($/PHQ9) | 318.20* | 79.45** | − 633.78** |
| p-value | 0.018 | 0.001 | 0.009 |
| ICER ($/HSCL) | 2710.59** | 717.47** | − 8923.65† |
| p-value | 0.008 | 0.001 | 0.068 |
Notes:
p <.01,
p <.05,
p <.10
– ICER is computed by dividing the estimated incremental difference in MH costs by the incremental difference in effectiveness measures.
– Standard errors of ICER are computed by creating 1000 bootstrapped estimates and using delta method.
The estimated ICERs for face-to-face group versus usual care show that it costs $318 and $2711 more to achieve one score reduction in PHQ9 and HSCL, respectively, for face-to-face group compared to usual care (Table 4, Column 1). ICER estimates for telephone group versus usual care reveal that one score reduction in PHQ9 and HSCL scores for the phone group costs $79 and $717 more than usual care. These estimates are statistically significant at p= .01.
Our most significant finding is that phone intervention is significantly more cost-effective than face-to-face in terms of improvements in PHQ9 scores. The negative ICERs comparing phone group directly to face-to-face demonstrate that achieving one score reduction in phone group costs less than one score reduction in face-to-face group (Table 4, column 3). Specifically, one score reduction in PHQ9 costs $634 less than face-to-face (and one score reduction in HSCL in phone group costs $8924 less, although not significant). In other words, the phone intervention is as effective as face-to-face in improving PHQ9 scores with significantly smaller costs.
Discussion
The finding that phone intervention is significantly more cost-effective than face-to-face in improving depression symptoms is crucial for policy makers or health institutions considering providing a similar intervention in real-life. The fact that the phone-based intervention is able to improve the depressive symptoms of patients just as effectively as face-to-face by spending less may help motivate their decisions on which type of therapy service to provide.
It is important to acknowledge that there are certain limitations to this study. First, in cost-effectiveness studies effectiveness is generally measured in quality adjusted life years (QALYs) or depression free days. Since we do not have the necessary information in our dataset to compute QALYs or depression free days, we measure effectiveness by 1-unit improvement in PHQ9 or HSCL scores. Even though 1-unit decrease in these scores might not have an obvious clinical significance, they do suggest improvement in depression symptoms. Moreover, the ICERs computed using 1-unit improvement in scores can easily be transformed into measures with clinical significance. For instance, a 5-point change on the PHQ-9 is shown to be clinically significant47 where a drop of 5 points is the criteria for ‘adequate’ initial treatment response.48,49 The ICER estimates in Table 4 can easily be transformed into units of $ per 5-unit improvement in PHQ9 scores. Specifically, our estimates show that for face-to-face CBT group it costs $1591 more to achieve a 5-unit clinically significant reduction in PHQ9, compared to usual care. For the phone CBT group, it costs $397 more to achieve a 5-unit reduction in PHQ9, compared to usual care.
The second limitation is that we are not able to properly monetize and include many advantages of the phone intervention in our costs that are relevant from a social cost perspective. For instance, phone therapy patients may possibly save on child care costs due to participation in therapy over the phone and achieve utility gains due to the privacy and flexibility with phone based care. Given this limitation patient costs may be much higher for face-to-face encounters than it is estimated in this paper, which would make the telephone intervention even more attractive. It is also important to note that not all individuals can have the financial means to make lengthy phone calls. In our study, phone group patients were provided with phone cards with extra minutes so this was not an issue. However, it is a potential limitation to replicating the study outside of a controlled research environment.
Third limitation is related to the service use data reported. Service use on general medical services is not reported as part of the study, and this turns out to be a drawback given the generally high rates of medical co-morbidity with depression. In addition, we observe MH service use of patients for only four months prior to the final interview. Both phone and face-to-face interventions can potentially be associated with significant cost savings in the long-run if we were to observe long-run service use. Additional studies would be needed to establish such findings.
As one of the first studies comparing the cost-effectiveness of telephone versus face-to-face interventions for the low-income Latino population, the findings of this study will assist policy makers and healthcare institutions considering adopting similar services to under-served minority populations.
Acknowledgments
Source of Funding: This project was supported by NIMHD Research Grant # 3 P60 MDO 02261 (PI: Alegria) funded by the National Institute on Minority Health and Health Disparities. It was approved by the institutional review boards of Cambridge Health Alliance and the University of Puerto Rico.
Appendix
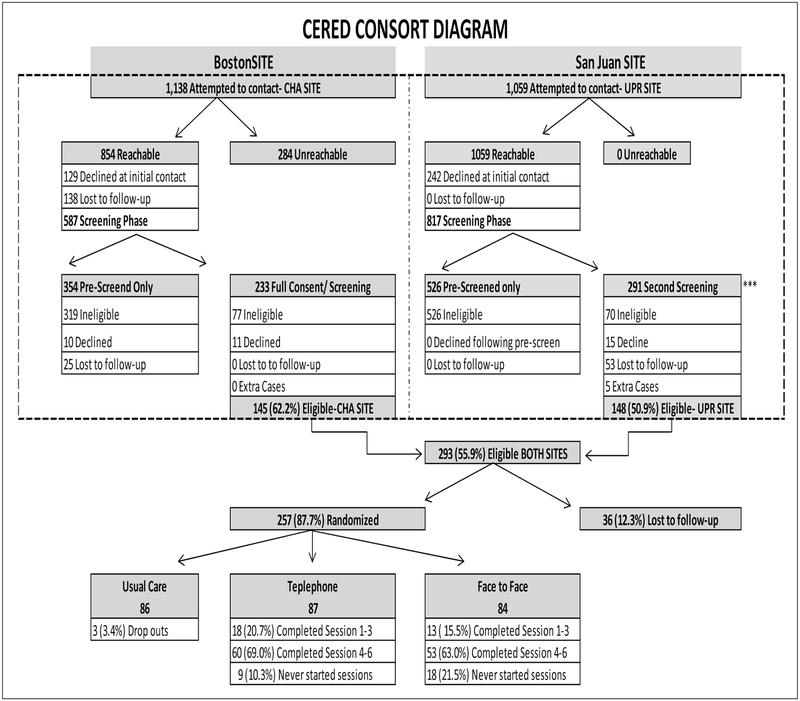
Figure A1.
CERED Consort Diagram
Footnotes
CERED (Comparative Effectiveness Research for Eliminating Disparities) is a randomized controlled trial designed to test the comparative effectiveness of a telephone-based intervention compared to the face-to-face intervention to treat depression among Latinos. See the section titled “Study Background” for a detailed description of the study.
For detailed CONSORT information please refer to Figure A.1 in the Appendix, and Alegria M, Ludman E, Kafali EN, et al., Effectiveness of the CERED (Comparative Effectiveness Research for Eliminating Disparities) Intervention in Low-Income Latinos. 2014.
Detailed explanation of these measures can be found in the Data section.
Phone CBT was still significantly less costly than face-to-face CBT, by $223 (p=.01).
Similar to Schoenbaum et al.21
References:
- 1.Estimates for the Insurance Coverage Provisions of the Affordable Care Act Updated for the Recent Supreme Court Decision. Congressional Budget Office;July 2012.
- 2.U.S.GPO. Patient Protection and Affordable Care Act (HR 3590). Public Law [111–148] 111th Congress; 2010.
- 3.Substance Abuse and Mental Health Services Administration. National Expenditures for Mental Health Services and Substance Abuse Treatment, 1986–2009. HHS Publication No. SMA-13–4740. Rockville, MD. 2013.
- 4.Mohr DC, Vella L, Hart S, Heckman T, Simon G. The Effect of Telephone Administered Psychotherapy on Symptoms of Depression and Attrition: A Meta Analysis. Clinical Psychology: Science and Practice 2008; 15(3): 243–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tutty S, Ludman EJ, Simon G. Feasibility and acceptability of a telephone psychotherapy program for depressed adults treated in primary care. Gen Hosp Psychiatry. 2005; 27(6): 400–410. [DOI] [PubMed] [Google Scholar]
- 6.Ludman EJ, Simon GE, Tutty S, Von Korff M. A randomized trial of telephone psychotherapy and pharmacotherapy for depression: continuation and durability of effects. J Consult Clin Psychol 2007; 75(2): 257–266 [DOI] [PubMed] [Google Scholar]
- 7.Mohr DC, Ho J, Duffecy J, Reifler D, Sokol L, Burns MN, Jin L, Siddique J. Effect of Telephone-Administered vs Face-to-face Cognitive Behavioral Therapy on Adherence to Therapy and Depression Outcomes Among Primary Care PatientsA Randomized Trial. JAMA 2012; 307(21): 2278–2285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alegria M, Ludman E, Kafali E, et al. Effectiveness of the CERED (Comparative Effectiveness Research for Eliminating Disparities) Intervention in Low-Income Latinos. (under review). 2014.
- 9.McGuire TG, Alegria M, Cook BL, Wells KB, Zaslavsky AM. Implementing the Institute of Medicine definition of disparities: an application to mental health care. Health Serv Res 2006; 41(5): 1979–2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miranda J, Cooper LA. Disparities in care for depression among primary care patients. J Gen Internal Med 2004; 19(2): 120–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alegria M, Chatterji P, Wells K, Cao Z, Chen CN, Takeuchi D, Jackson J, Meng XL. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatr Serv 2008; 59(11): 1264–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miranda J, Duan N, Sherbourne C, Schoenbaum M, Lagomasino I, Jackson-Triche M, Wells KB. Improving care for minorities: can quality improvement interventions improve care and outcomes for depressed minorities? Results of a randomized, controlled trial. Health Serv Res 2003; 38(2): 613–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Katon W, Russo J, Sherbourne C, Stein MB, Craske M, Fan MY, Roy-Byrne P. Incremental cost-effectiveness of a collaborative care intervention for panic disorder. Psychol Med 2006; 36(03): 353–363. [DOI] [PubMed] [Google Scholar]
- 14.McHugh RK, Otto MW, Barlow DH, Gorman JM, Shear MK, Woods SW. Cost-efficacy of individual and combined treatments for panic disorder. The Journal of clinical psychiatry. 2007; 68(7): 1038–1044. [DOI] [PubMed] [Google Scholar]
- 15.Roberge P, Marchand A, Reinharz D, Savard P. Cognitive-Behavioral Treatment for Panic Disorder With Agoraphobia A Randomized, Controlled Trial and Cost-Effectiveness Analysis. Behav Modif 2008; 32(3): 333–351. [DOI] [PubMed] [Google Scholar]
- 16.Issakidis C, Sanderson K, Corry J, Andrews G, Lapsley H. Modelling the population cost-effectiveness of current and evidence-based optimal treatment for anxiety disorders. Psychol Med 2004; 34(1): 19–35. [DOI] [PubMed] [Google Scholar]
- 17.Heuzenroeder L, Donnelly M, Haby MM, Mihalopoulos C, Rossell R, Carter R, Andrews G, Vos T. Cost-effectiveness of psychological and pharmacological interventions for generalized anxiety disorder and panic disorder. Aust NZ J Psychiatry. 2004; 38(8): 602–612. [DOI] [PubMed] [Google Scholar]
- 18.Guest JF, Russ J, Lenox-Smith A. Cost-effectiveness of venlafaxine XL compared with diazepam in the treatment of generalised anxiety disorder in the United Kingdom. Eur J Health Econ 2005; 6(2): 136–145. [DOI] [PubMed] [Google Scholar]
- 19.McCrone P, Craig TKJ, Power P, Garety PA. Cost-effectiveness of an early intervention service for people with psychosis. British J Psychiatry 2010; 196(5): 377–382. [DOI] [PubMed] [Google Scholar]
- 20.McCrone P, Knapp M, Proudfoot J, Ryden C, Cavanagh K, Shapiro DA, Ilson S, Gray JA, Goldberg D, Mann A, Marks I, Everitt B, Tylee A. Cost-effectiveness of computerised cognitive “behavioural therapy for anxiety and depression in primary care: randomised controlled trial. Br J Psychiatry 2004; 185(1): 55–62. [DOI] [PubMed] [Google Scholar]
- 21.Revicki DA, Siddique J, Frank L, Chung JY, Green BL, Krupnick J, Prasad M, Miranda J. Cost-effectiveness of evidence-based pharmacotherapy or cognitive behavior therapy compared with community referral for major depression in predominantly low-income minority women. Arch Gen Psychiatry 2005; 62(8): 868–875. [DOI] [PubMed] [Google Scholar]
- 22.Katon W, Russo J, Lin EHB, Schmittdiel J, Ciechanowski P, Ludman E, Peterson D, Young B, Von Korff M. Cost-effectiveness of a multicondition collaborative care intervention: a randomized controlled trial. Arch Gen Psychiatry 2012; 69(5): 506–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schoenbaum M, Miranda J, Sherbourne C, Duan N, Wells K. Cost-effectiveness of interventions for depressed Latinos. J Ment Health Policy Econ 2004; 7(2): 69–76. [PubMed] [Google Scholar]
- 24.Katon WJ, Roy-Byrne P, Russo J, Cowley D. Cost-effectiveness and cost offset of a collaborative care intervention for primary care patients with panic disorder. Arch Gen Psychiatry 2002; 59(12): 1098–1104. [DOI] [PubMed] [Google Scholar]
- 25.Fenton WS, Hoch JS, Herrell JM, Mosher L, Dixon L. Cost and cost-effectiveness of hospital vs residential crisis care for patients who have serious mental illness. Arch Gen Psychiatry. 2002; 59(4): 357–364. [DOI] [PubMed] [Google Scholar]
- 26.AHRQ. MEPS HC-121 2008 Full Year Consolidated Data File. Agency for Healthcare Research and Quality Center for Financing, Access, and Cost Trends; 2010.
- 27.Schoenbaum M, Unutzer Jr, Sherbourne C, Duan N, Rubenstein LV, Miranda J, Meredith LS, Carney MF, Wells K. Cost-effectiveness of practice-initiated quality improvement for depression. JAMA 2001; 286(11): 1325–1330. [DOI] [PubMed] [Google Scholar]
- 28.Otto MW, Pollack MH, Maki KM. Empirically supported treatments for panic disorder: Costs, benefits, and stepped care. J Consult Clin Psychol 2000; 68(4): 556–567. [PubMed] [Google Scholar]
- 29.Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann 2002; 32(9): 1–7. [Google Scholar]
- 30.Lowe B, Kroenke K, Herzog W, Grafe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord 2004; 81(1): 61–66. [DOI] [PubMed] [Google Scholar]
- 31.Rogers WH, Adler DA, Bungay KM, Wilson IB. Depression screening instruments made good severity measures in a cross-sectional analysis. J Clin Epidemiol 2005; 58(4): 370–377. [DOI] [PubMed] [Google Scholar]
- 32.Williams JJW, Stellato CP, Cornell J, Barrett JE. The 13-and 20-item Hopkins Symptom Checklist Depression Scale: psychometric properties in primary care patients with minor depression or dysthymia. Int J Psychiatry Med 2004; 34(1): 37–50. [DOI] [PubMed] [Google Scholar]
- 33.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behavioral science. 1974; 19(1): 1–15. [DOI] [PubMed] [Google Scholar]
- 34.Felker B, Katon W, Hedrick SC, Rasmussen J, McKnight K, McDonnell MB, Fihn SD. The association between depressive symptoms and health status in patients with chronic pulmonary disease. Gen Hosp Psychiatry 2001; 23(2): 56–61. [DOI] [PubMed] [Google Scholar]
- 35.Hedrick SC, Chaney EF, Felker B, Liu CF, Hasenberg N, Heagerty P, Buchanan J, Bagala R, Greenberg D, Paden G, Fihn SD, Katon W. Effectiveness of collaborative care depression treatment in Veterans’ Affairs primary care. J Gen Intern Med 2003; 18(1): 9–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Katon W, Robinson P, Von Korff M, Lin E, Bush T, Ludman E, Simon G, Walker E. A multifaceted intervention to improve treatment of depression in primary care. Arch Gen Psychiatry 1996; 53(10): 924–932. [DOI] [PubMed] [Google Scholar]
- 37.Kroenke K Depression screening is not enough. Ann Intern Med 2001; 134(5): 418–420. [DOI] [PubMed] [Google Scholar]
- 38.Jr Unutzer, Katon W, Callahan CM, Williams JW Jr, Hunkeler E, Harpole L, Hoffing M, Della Penna RD, Noël PH, Lin EH, Areán PA, Hegel MT, Tang L, Belin TR, Oishi S, Langston C. Collaborative care management of late-life depression in the primary care setting. JAMA 2002; 288(22): 2836–2845. [DOI] [PubMed] [Google Scholar]
- 39.Williams JW Jr, Barrett J, Oxman T, Frank E, Katon W, Sullivan M, Cornell J, Sengupta A. Treatment of dysthymia and minor depression in primary care. JAMA 2000; 284(12): 1519–1526. [DOI] [PubMed] [Google Scholar]
- 40.Buntin MB, Zaslavsky AM. Too much ado about two-part models and transformation? Comparing methods of modeling Medicare expenditures. J Health Econ 2004; 23(3): 525–542. [DOI] [PubMed] [Google Scholar]
- 41.Manning WG, Morris CN, Newhouse JP, et al. 1981. A two-part model of the demand for medical care: preliminary results from the health insurance study In: van der Gaag J, Perlman M. (Eds. Health, Economics, and Health Economics. North Holland, Amsterdam; (pp. 103–123). [Google Scholar]
- 42.Duan N, Manning WG, Morris CN, Newhouse JP. A comparison of alternative models for the demand for medical care. Journal of Business & Economic Statistics 1983; 1(2): 115–126. [Google Scholar]
- 43.Mullahy J Much ado about two: reconsidering retransformation and the two-part model in health econometrics. J Health Econ 1998; 17(3): 247–281. [DOI] [PubMed] [Google Scholar]
- 44.Blough DK, Madden CW, Hornbrook MC. Modeling risk using generalized linear models. J Health Econ 1999; 18(2): 153–171. [DOI] [PubMed] [Google Scholar]
- 45.Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ 2001; 20(4): 461–494. [DOI] [PubMed] [Google Scholar]
- 46.Duan N, Manning WG, Morris CN, Newhouse JP. A Comparison of Alternative Models for the Demand for Medical Care. 1982: R-2754-HHS, The Rand Corporation, SantaMonica, California. [Google Scholar]
- 47.ACP (American College of Physicians). Depression Care Guide. From Evaluation to Monitoring. http://depression.acponline.org/pp/chapters/dcg_s9_1.
- 48.The MacArthur Foundation. Depression Management Tool Kit. The JohnD. & Catherine T. MacArthur Foundation’s Initiative on Depression and Primary Care 2009; http://prevention.mt.gov/suicideprevention/13macarthurtoolkit.pdf.
- 49.Lowe B, Unutzer J, Callahan CM, Perkins AJ, Kroenke K. Monitoring depression treatment outcomes with the Patient Health Questionnaire-9. Med Care 2004; 42(12): 1194–1201. [DOI] [PubMed] [Google Scholar]