Abstract
We examined HIV prevalence among patients 18–49 year olds admitted to a psychiatric hospital in Botswana in 2011 and 2012. The retrospective study analyzed females (F) and males (M) separately, comparing proportions with chi-square test and continuous variables with Wilcoxon rank-sum test, assessing significance at the 5% level.
HIV seroprevalence among hospitalized psychiatric patients was much more common among females (53%) compared with males (19%) (p<0.001). These women also appeared more vulnerable to infection compared with females in the general population (29%) (p<0.017). Among both women and men, HIV-infection appeared most common among patients with organic mental disorders (F:68%, M:41%) and neurotic, stress related and somatoform disorders (F:68%, M:42%). The largest proportion of HIV infections co-occurred among patients diagnosed with schizophrenia, schizotypal and other psychotic disorders (F:48%; M:55%), mood (affective) disorders (F:21%; M:16%) and neurotic, stress-related and somatoform disorders (F:16%; M:20%).
Interventions addressing both mental health and HIV among women require development.
Keywords: HIV/AIDS, Mental health, Psychiatry, Hospitalized, Gender
INTRODUCTION
UNAIDS reports Botswana’s HIV infection rate is the third highest in the world after Swaziland and Lesotho: 22% among adults 15–49 years old (1). The country has offered treatment publicly since January 2002 (2). In 2012, Botswana introduced a once-daily, single dose combination of TDF+FTC+EFV or TDF+FTC (or TDF+FTC and NVP /ritonavir, as indicated) to all HIV-positive patients with a CD4 count of ≤350 cell/μL (3). However, new HIV treatment guidelines issued in May 2016 introduced a ‘Treat All’ Strategy concurrent with the use of TDF+FTC +DTG (or ABC+3TC+DTG if indicated) as first line regimens (4). Programs to fight the spread of HIV including Prevention of Mother to Child Transmission (PMTCT) and routine testing for patients visiting health institutions have run for more than 10 years, however only recently was Pre-Exposure Prophylaxis (PrEP) advised for those engaging in high risk sexual activity (4). However, currently there are no programs specifically targeting persons with mentally illness, who may be a high risk for contracting and transmitting HIV infection.
While no representative epidemiological studies have been conducted to calculate the prevalence of HIV among people with different types of mental illness, a number of studies utilizing secondary data have found high rates of HIV among people who were treated in specialty mental health settings. Blank and colleagues (5) carried out a cross-sectional study used Medicaid claims data and welfare recipient files for persons aged 18 years or older for fiscal years 1994 through 1996 in Philadelphia. The results showed a period prevalence of 0.6% among Medicaid recipients who did not have a diagnosis of a serious mental illness and 1.8% among those who did. After sex, age, race, and time on welfare during the study period were controlled for, patients with a schizophrenia spectrum disorder were 1.5 times as likely to have a diagnosis of HIV infection, and patients with a diagnosis of a major affective disorder were 3.8 times as likely. Similarly, Walkup and colleagues (6) identified Medicaid beneficiaries with HIV/AIDS through the merging of New Jersey HIV/AIDS Registry and Medicaid eligibility files. Claims histories were used to create a typology of individuals with schizophrenia spectrum disorder, major affective disorder, or no serious mental illness. HIV was identified in 8294 individuals, of whom 5.7% were identified as having schizophrenia spectrum disorders, and 6.8% as having major affective disorder. They found that individuals with serious mental illnesses were more likely than other groups to be injection drug users and to have claims indicative of substance abuse. In fact, among people with schizophrenia spectrum disorders within the Veterans Administration (VA), Himelhoch and colleagues confirmed elevated rates of HIV, however after controlling for substance abuse, there was no excess risk for HIV for people with schizophrenia spectrum disorder in the absence of substance abuse (7).
Among men (8) and women (9) with HIV infection, high rates of depression have been found. Others using convenience samples have found elevated rates of HIV among people receiving mental health services in a variety of settings (10,11,12). Other papers report depression is predisposing to contracting HIV as well as consequential (13,14,15). The increased rates of HIV among people with mental illnesses is thought to be due to increased sexual risk behaviors as well as risk associated with high rates of substance abuse (5,6,7).
We found no previous studies in Botswana that have estimated HIV prevalence among mentally ill patients; consequently, it is not known whether the mentally ill in general or any subset of the mentally ill are a vulnerable group in need of special intervention. Most studies that have estimated the co- occurrence of HIV and mental illness describe populations of high –income countries with relatively low seroprevalence rates (5,16,17). Fewer studies have been carried out in low and middle income countries. Lundberg et al.(18) found an HIV prevalence rate of 11.3% in a cross sectional hospital- based study in Uganda compared with 7.3% in the general population. Their finding appears lower than the 18% prevalence rate estimated by Maling et al. among first-time psychiatric admissions at two national referral hospitals in urban Kampala (19). Studies in other countries in the region have found even higher rates of infection among the severely mentally ill (SMI): 26.5% in South Africa and 23.8% in Zimbabwe (20,21). These studies point to the severely mentally ill or those with mental illness per se as a vulnerable group.
In sub-Saharan Africa and in Botswana, women face a greater risk of HIV infection than men (22). Females have higher prevalence rates compared with males in both the general population (females: 21.0%; males: 15.6%) (23) and youth 15–24 years old (females: 11.1%; males: 4.0%) (23). Biological (24), economic, and social differences (25,26) affect the dynamics of HIV-infection transmission differently for women and men, often placing women at greater risk of infection (27,28,29,30). In Botswana, women face a greater vulnerability to infection through biological characteristics and established social inequalities in sexual decision making (31).
We set out to estimate the HIV prevalence rate among inpatients admitted to the only national referral hospital for psychiatric patients in Botswana. We also aimed to explore differences in seroprevalence for persons with different classes of mental illness, and to develop models of demographic and diagnostic factors associated with having a documented HIV-positive status.
STUDY POPULATION AND METHODS
Health care system in Botswana –
The public sector largely dominates health care provision in Botswana; its largely decentralized health care system is based on the primary care model. Eighty-four percent of the total population lives within 5km of a health facility.
The referral system is however organized in a hierarchical manner with National Referral Hospitals at the top of the pyramid, that support the district hospitals, primary hospitals, clinics and mobile stops at each level below in the pyramid. Currently, there is no compulsory national universal insurance coverage; most patients seeking help in public facilities are uninsured however health facilities charge a nominal fee (<USD$1) for services in the public sector.
Because of the integration of mental health care into the general health care system, mentally ill patients are seen at all levels of the referral system. Quite often non-specialized health nurses or doctors carry out an initial consultation in outpatient, referring to psychiatric nurses or psychiatrists as needed. Psychiatrists and psychiatric nurses perform outreach and supervisory visits to areas which are far removed from specialized psychiatric facilities to support nationwide access to specialized care. Additional information on the provision of mental health services in Botswana is reported elsewhere (32).
Study population and setting –
The Sbrana Hospital Epidemiology Study (SHES) gathered data from medical records for patients hospitalized at the Sbrana Psychiatric Hospital (SPH), located in Lobatse, Botswana. The hospital remains the only national referral hospital for psychiatric patients in the country and functions as a teaching hospital for both medical students and nurses. The study included all hospitalized patients admitted between January 1, 2011 and December 31, 2012.
Data collection –
Once the study obtained both IRB clearance and assent from the SPH management, four data abstractors (two nurses with additional training in mental health, and two psychiatric hospital medical record keepers) were trained to review and abstract information from patient charts of documented age, gender, level of education, marital status and employment status declared at the time of admission, mental illness diagnosis, length of stay, total number of documented psychiatric admissions, substance use, and HIV status.
Mental illness diagnoses found in patient charts were coded according to the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). Due to limited details of the diagnosis found in patient charts, coders largely focused on coding by condition (first three characters of the ICD-10-CM classification. Patients with final diagnoses recorded only as ‘suicide attempts’ and having neither a mood or psychotic disorder, were coded as “reactions to severe stress and adjustment disorders”. To confirm reliability of diagnoses documented, a psychiatric specialist serving as a fifth data abstractor, independently reviewed and abstracted from a randomly selected sub-sample of 30 study patients. Comparison of psychiatric diagnoses abstracted by the psychiatric specialist and those of the initial abstraction team found psychiatric diagnoses abstracted matched for all (100%) of sub-sampled patients (n=30, Kappa 1.000, p<0.0001).
Chart documented HIV status was captured through routine testing of all patients for HIV (33), in accordance with Botswana’s national guidelines active (3,34). At the time of patient care, guidelines advised HIV testing to occur by either parallel rapid testing conducted as part of voluntary counselling and testing offered to patients, or, if bloodwork was ordered for the patient during hospitalization, by routine testing at the hospital laboratory using concordant parallel ELISA tests. Discordant tests were repeated again after 2–4 weeks; if after repeated testing results remained indeterminate, PCR testing or Western Blot was advised.
Data collectors gathered information on hospitalized patients admitted in 2011 and 2012, identifying patients hospitalized during the two-year period serially from the hospital’s admissions register. Data from charts of patients hospitalized multiple times during the two-year period were abstracted only once, referring to the most recent admission as the hospitalization closest to December 31, 2012. Collection avoided duplicate extraction of the patients by marking covers of medical record charts already abstracted.
Statistical analysis –
Our analysis explores co-occurrence of (documented) HIV seroprevalence with different mental illness diagnoses and demographic characteristics (at most recent admission), using Chi-square test/Fisher’s Exact test for proportion for discrete variables and rank-sum test for continuous variables. Tabulations of HIV prevalence among patients with different psychiatric diagnoses present statistical test p-values of all ICD general classifications, as well as sub-group classifications with statistically significant p-values. For patients with multiple psychiatric diagnoses, tabulations included all in estimates of both prevalence of mental health diagnoses, and the proportion with HIV-infection among them. Calculations of percent diagnosed were out of all patients; as some patients may have had more than one psychiatric disorder, some tabulated totals exceeded 100%.
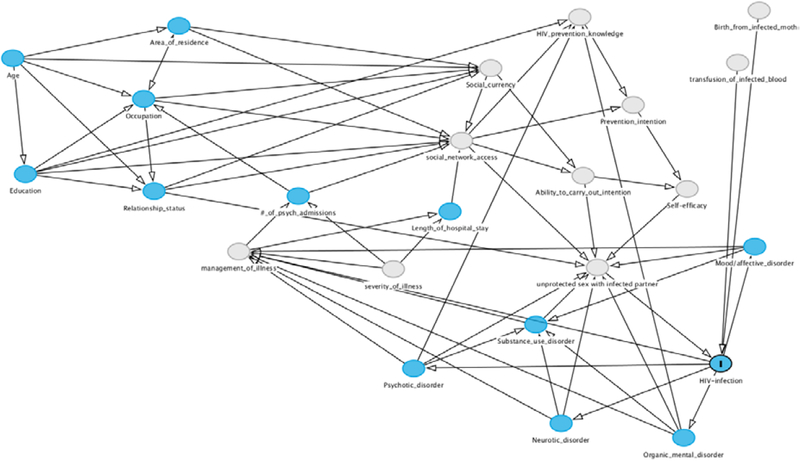
Multivariate analysis was limited to those aged 18–49 years to align co-variate measures with available data on HIV status and the low numbers of hospitalized patients outside this age range. Logistic regression was employed to evaluate factors independently associated with documented HIV-infection. Directed Acyclic Graphs (DAGs) or causal diagrams are developed to illustrate a theoretical causal structure of the variables considered in the analysis (35) and help recognize and minimize the influence of potential sources of biases in an analysis, including minimizing bias by adjustment for confounders and avoiding the introduction of bias by adjustment for colliders (36,37,38). Prior to estimating covariate effects, variable selection was guided by construction of a Directed Acyclic Graph (DAG) for HIV-infection in this population using DAGitty 3.0 (39) with information drawn from the literature and subject matter experts (Figure 1). Recognizing the well documented gender differences in HIV transmission (40,41,42), we developed separate regression models for male and female patients and estimated effect sizes for variables showing open pathways in our DAG model. Initial candidate models included variables deemed sufficient to reduce bias per methods described by Pearl and others (38). We could not determine if mental health diagnoses developed before or after the HIV diagnosis; as such, temporality could not be established to allow for a longitudinal analysis. All testing considered significance at the 5% level, and statistical analyses were performed using Stata 13.1 (43).
FIGURE 1:
SHES Directed Acyclic Graph (DAG) for HIV-Infection among Psychiatric Inpatients
This DAG depicts the model of cause and effect relationships considered in our statistical analysis. DAGs help guide the appropriate selection of variables to condition on, to control for confounding of exposure variables on the outcome variable HIV-infection.
A sensitivity analysis assessed the influence of missing data on the estimates of HIV seroprevalence and the results of the multivariate analysis, comparing estimates from the complete case analysis with those derived from analysis of 20 datasets ‘completed’ by Multiple Imputation (MI). In MI datasets, missing values for HIV sero-status and education level were replaced with values imputed from models that considered both predictors of missing values of the variable as well as predictors of known values (44). Estimates of parameters and variance from each of the 20 ‘completed’ datasets were pooled into a single MI estimate. Imputation and estimation of pooled results utilized Multiple Imputation Using Chained Equations (MICE) in Stata 13.1 (45).
Ethics –
The study received ethical approval following review by review boards of participating institutions (BLINDED). Permission to carry out the study was further obtained from the senior management team of the psychiatric hospital.
RESULTS
Of 2619 hospitalizations of 1998 unique patients admitted between January 1, 2011 and December 31, 2012, our data collection team was able to locate and abstract data from 1725 charts (86% of the 1998 unique patients who were hospitalized). Of these patients 377 had been hospitalized more than once at the referral hospital during the sampled period. We limited our analysis to the 1482 hospitalized, mentally ill patients of known gender, who were aged 18–49 years at their most recent admission.
Patients were more likely to be men (67%, 1000/1482) than women (33%, 482/1482). The overall median age of admission was 30 years (IQR 24–37); men (median 29 years IQR 24–36) appeared slightly younger than women (median 31 years IQR 25–38) (p<0.001). Most patients were documented as single (95%, 1377/1455); five percent (66/1455) were married; and less than one percent (13/1455) indicated they were divorced, widowed or cohabited with a partner. Documented relationship status suggests women were more likely to be or have been in a relationship at the time of admission compared with men (p<0.001). See Table I for details.
Table I:
Characteristic of 18–49 year old hospitalized patients: overall and by gender
| Characteristics | Overall (n=1482) | Gender (n=1482) |
||
|---|---|---|---|---|
| % Females | % Males | p-value* | ||
| Total | 1482 | 33% (482/1482) | 67% (1000/1482) | - |
| Admission year | 0.840 | |||
| 2011 | 41% (602/1482) | 40% (194/482) | 41% (408/1000) | |
| 2012 | 59% (880/1482) | 60% (288/482) | 59% (592/1000) | |
| Median age at admission in years | 30 (24 – 37) (n=1482) |
31 (25 – 38) n=482 |
29 (24 – 36) n=1000 |
<0.001 |
| Relationship status | <0.001 | |||
| Single | 95% (1376/1455) | 90% (425/471) | 97% (951/984) | |
| Married | 5% (66/1455) | 8% (37/471) | 3% (29/984) | |
| Divorced | <1% (11/1455) | 1% (7/471) | <1% (4/984) | |
| Widowed | <1% (1/1455) | <1% (1/471) | 0% (0/984) | |
| Cohabiting | <1% (1/1455) | <1% (1/471) | 0% (0/984) | |
| Occupation | 0.002 | |||
| Unemployed | 58% (654/1137) | 54% (195/364) | 59% (459/773) | |
| Skilled | <1% (3/1137) | 0% (0/364) | <1% (3/773) | |
| Student | 11% (128/1137) | 12% (43/364) | 11% (85/773) | |
| Professional | 2% (21/1137) | 3% (11/364) | 1% (10/773) | |
| Self-employed | 3% (38/1137) | 4% (13/364) | 3% (25/773) | |
| Blue Collar | 17% (188/1137) | 14% (52/364) | 18% (136/773) | |
| White Collar | 9% (105/1137) | 14% (50/364) | 7% (55/773) | |
| Education level | 0.181 | |||
| None/Reception | 2% (22/1244) | 1% (6/413) | 2% (16/831) | |
| Primary incomplete | 8% (101/1244) | 6% (25/413) | 9% (76/831) | |
| Primary complete | 9% (114/1244) | 11% (47/413) | 8% (67/831) | |
| Secondary incomplete | 34% (429/1244) | 33% (136/413) | 35% (292/831) | |
| Secondary complete | 23% (292/1244) | 23% (93/413) | 24% (197/831) | |
| Tertiary incomplete | 2% (21/1244) | 1% (6/413) | 2% (15/831) | |
| Tertiary complete | 21% (265/1244) | 24% (97/413) | 20% (168/831) | |
| Area of residence | 0.425 | |||
| Village | 28% (405/1425) | 30% (139/467) | 28% (265/958) | |
| City | 27% (384/1425) | 25% (116/467) | 28% (268/958) | |
| Town | 45% (637/1425) | 45% (212/467) | 44% (425/958) | |
statistical test assesses differences between males and females for each characteristic
A majority did not indicate an occupation or were unemployed (57%, 654/1137). Occupations classifiable as ‘blue collar’ (17%, 188/1137), student (11%, 128/1137), and ‘white collar’ (9%, 106/1137) comprise most of the occupations declared. Women were more likely to indicate having white collar occupations, compared with men (p<0.001). A total of 46% (578/1244) indicated they had completed schooling at the secondary level. Forty-five percent (637/1425) of patients resided in towns; 28% (404/1425) lived in a village and 27% (384/1425) lived in cities. See Table I for further details.
Psychiatric diagnoses –
Table II lists common primary psychiatric diagnoses among admitted patients during the study period. Diagnoses of schizophrenia, schizotypal or other related disorders appeared the most common among admitted patients (55%, 812/1482), followed by mood disorders (18%, 273/1482), substance use disorders (18%, 267/1482) and neurotic, stress related and somatoform disorders (11%, 160/1482). About 5% (67/1482) of patients had organic mental disorders while 3% (44/1482) of patients were diagnosed with personality disorders; for 3% (49/1482), the diagnosis of mental disorder was unspecified.
Table II:
Documented psychiatric diagnoses at patient’s most recent hospitalization: overall and by gender
| ICD General Classification and Psychiatric Diagnoses |
ALL (n=1482) |
FEMALES (n=482) |
MALES (n=1000) |
Chi2 test p-value** | |||
|---|---|---|---|---|---|---|---|
| n | %* | n | %* | n | %* | ||
| 1. Organic mental disorders | 67 | 4.5% | 27 | 5.6% | 40 | 4.0% | 0.164 |
| Vascular dementia | 1 | 0.1% | 1 | 0.2% | 0 | 0.0% | |
| 2 | 0.1% | 1 | 0.2% | 1 | 0.1% | ||
| 2 | 0.1% | 1 | 0.2% | 1 | 0.1% | ||
| 22 | 1.5% | 14 | 2.9% | 8 | 0.8% | ||
| 2 | 0.1% | 0 | 0.0% | 2 | 0.2% | ||
| 38 | 1.60% | 10 | 2.1% | 28 | 2.8% | ||
| 2. Substance use disorders | 267 | 18.0% | 29 | 6.0% | 238 | 23.8% | <0.001 |
| Alcohol related disorders | 114 | 7.7% | 17 | 3.5% | 97 | 9.7% | <0.001 |
| 94 | 6.3% | 6 | 1.2% | 88 | 8.8% | <0.001 | |
| 1 | 0.1% | 0 | 0.0% | 1 | 0.1% | ||
| 5 | 0.3% | 1 | 0.2% | 4 | 0.4% | ||
| 1 | 0.1% | 1 | 0.2% | 0 | 0.0% | ||
| 52 | 3.5% | 4 | 0.8% | 48 | 4.8% | <0.001 | |
| 3. Schizophrenia, schizotypal and other psychotic disorders | 812 | 54.8% | 235 | 48.8% | 577 | 57.7% | 0.001 |
| Schizophrenia | 520 | 35.1% | 115 | 23.9% | 405 | 40.5% | <0.001 |
| 1 | 0.1% | 0 | 0.0% | 1 | 0.1% | ||
| 13 | 0.9% | 5 | 1.0% | 8 | 0.8% | ||
| 140 | 9.4% | 50 | 10.4% | 90 | 9.0% | ||
| 136 | 9.2% | 64 | 13.3% | 72 | 7.2% | <0.001 | |
| 2 | 0.1% | 1 | 0.2% | 1 | 0.1% | ||
| 4. Mood(affective)disorders | 273 | 18.4% | 127 | 26.3% | 146 | 14.6% | <0.001 |
| Manic episode | 35 | 2.4% | 11 | 2.3% | 24 | 2.4% | |
| 119 | 8.0% | 47 | 9.8% | 72 | 7.2% | ||
| 10 | 0.7% | 4 | 0.8% | 6 | 0.6% | ||
| 102 | 6.9% | 60 | 12.4% | 42 | 4.2% | <0.001 | |
| 5 | 0.3% | 3 | 0.6% | 2 | 0.2% | ||
| 1 | 0.1% | 1 | 0.2% | 0 | 0.0% | ||
| 1 | 0.1% | 1 | 0.2% | 0 | 0.0% | ||
| 5. Neurotic, stress-related and somatoform disorders | 160 | 10.8% | 64 | 13.3% | 96 | 9.6% | 0.033 |
| Other anxiety disorders | 39 | 2.6% | 16 | 3.3% | 23 | 2.3% | |
| 46 | 3.1% | 12 | 2.5% | 34 | 3.4% | ||
| 75 | 5.1% | 36 | 7.5% | 39 | 3.9% | 0.003 | |
| 6. Disorders assoc. w/physical, physiological factors | 11 | 0.7% | 8 | 1.7% | 3 | 0.3% | 0.004 |
| Puerperal psychosis | 9 | 0.6% | 8 | 1.7% | 1 | 0.1% | <0.001 |
| 2 | 0.1% | 0 | 0.0% | 2 | 0.2% | ||
| 7. Personality disorders | 44 | 3.0% | 13 | 2.7% | 31 | 3.1% | 0.669 |
| Paranoid personality disorder | 11 | 0.7% | 5 | 1.0% | 6 | 0.6% | |
| 2 | 0.1% | 1 | 0.2% | 1 | 0.1% | ||
| 23 | 1.6% | 3 | 0.6% | 20 | 2.0% | 0.044 | |
| 3 | 0.2% | 1 | 0.2% | 2 | 0.2% | ||
| 4 | 0.3% | 3 | 0.6% | 1 | 0.1% | ||
| 1 | 0.1% | 0 | 0.0% | 1 | 0.1% | ||
| 8. Mental retardation | 6 | 0.4% | 3 | 0.6% | 3 | 0.3% | |
| Mild mental retardation | 6 | 0.4% | 3 | 0.6% | 3 | 0.3% | |
| 9. Disorders of psychological development | 1 | 0.1% | 0 | 0.0% | 1 | 0.1% | |
| Other pervasive developmental disorders | 1 | 0.1% | 0 | 0.0% | 1 | 0.1% | |
| 10. Childhood and adolescent disorders | 9 | 0.6% | 4 | 0.8% | 5 | 0.5% | |
| Conduct disorder confined to family context | 4 | 0.3% | 2 | 0.4% | 2 | 0.2% | |
| 1 | 0.1% | 0 | 0.0% | 1 | 0.1% | ||
| 2 | 0.1% | 0 | 0.0% | 2 | 0.2% | ||
| 1 | 0.1% | 1 | 0.2% | 0 | 0.0% | ||
| 1 | 0.1% | 1 | 0.2% | 0 | 0.0% | ||
| 11. Unspecified mental disorders | 49 | 3.3% | 6 | 1.2% | 43 | 4.3% | 0.002 |
| Mental disorder, not otherwise specified | 49 | 3.3% | 6 | 1.2% | 43 | 4.3% | 0.002 |
| Total number of patients* | 1482 | 114.6% | 482 | 107.1% | 1000 | 118.3% | |
percent is calculated out of all patients; as some patients may be diagnosed with more than one psychiatric disorder, total exceeds 100%.
statistical test comparing the proportion with the psychiatric diagnosis by gender. The table presents p-values of all ICD general classifications, as well as sub-group classifications with p-values less than 0.05.
We examined if rates of psychiatric diagnoses varied between men and women. Substance use disorders appeared more common among male admissions: alcohol use disorder was more than twice as common among men (M: 10%, 97/1000; F: 4%, 17/482; p<0.001), and cannabis use disorder nearly seven times more common among men (M: 9%, 88/1000; F: 1%, 6/482; p<0.001). Similarly, we noted a higher proportion of men diagnosed with Schizophrenia (M: 41%, 405/1000; F: 24%, 115/482; p<0.001). Admissions with Schizoaffective disorders (M: 7%, 72/1000; F: 13%, 64/482; p<0.001) were more common among women than men, as was depression (M: 5%, 50/1000; F: 13%, 65/482; p<0.001). Although not strictly a mental health diagnosis, our study found documentation of having attempted suicide more common among women (M: 4%, 39/1000; F: 8%, 36/482; p=0.003).
HIV prevalence –
From information found in patient medical charts and further review of laboratory registers, the study was able to obtain documentation of HIV status for 955/1482 (64%) of all patients hospitalized during the study period. We analyzed the abstracted data first under an assumption that HIV status was Missing-Completely-At-Random (MCAR). Of patients with documented HIV status, 31% (299/955) were HIV seropositive. Among women, more than half (53%, 187/356) were documented as HIV-positive – more than twice the rate observed among men (19% (112/599)) (p<0.001).
Recognizing the large number of patients without documentation of HIV status, we performed sensitivity analyses, first replacing missing HIV status values with either all positive or all negative values. Overall, HIV prevalence among women estimated ranged between 39% - 65%. Among women ages 19 to 24 years, HIV prevalence estimates range between 14% - 52%; among women ages 25 to 49 years, HIV prevalence estimates range between 46% - 68%. Among men, HIV prevalence estimates ranged between 11% - 51% overall. HIV prevalence estimates ranged 3% - 48% for men 19–24 years of age, and 14% - 52% for men 25 – 49 years of age.
We further compared estimates from the incomplete, abstracted data and those derived from the 20 MI datasets which suggests the influence of missing data on estimates of HIV seroprevalence and factors associated with HIV appears minimal. Compared with those of the original abstracted data, pooled MI estimates for HIV seroprevalence were slightly lower for both women (51% 95% CI 45.6%,56.5%) and men (17.5 95% CI 14.7%, 20.4%). All effects reported in the multivariate analysis of the original abstracted data also remained significant in the pooled estimates derived from MI datasets for both men and women.
Among women, HIV rates did not appear to vary significantly by relationship status (p=0.651). In contrast, HIV among married men (46%, 6/13) appeared more common than among single men (18%, 102/571) (p=0.021). Generally, those infected with HIV were older (median 35 years IQR 29–40) compared with HIV-negative patients (median 29 years IQR 24–36) (p<0.001).
Students, both men and women, appeared less likely to have HIV compared with those of other occupations (M students: 6% (2/35) vs others: 21% (85/413), p=0.033; F students: 15% (3/20) vs others: 56% (138/248), p<0.001). Among men, we also found documented HIV-infection more common among blue-collar workers (M blue-collar workers: 35% (31/88) vs others: 16% (56/360), p<0.001)) but less common among the unemployed (M unemployed: 15% (43/281) vs others: 26% (44/167), p=0.004). In contrast, among women with documented occupation, HIV rates proved higher among those deemed unemployed compared with others (F unemployed: 60% (93/156) vs others: 43% (48/112), p=0.007). We also noted HIV infection less common among women with at least secondary school education (F secondary level education: 42% (56/133) vs those with less formal education: 60% (104/174), p=0.002); we did not observe this difference across education groups among men (p=0.465). See Table III.
Table III:
Characteristic of hospitalized patient infected with HIV: overall and by gender
| Characteristics | Among all with known HIV status (n=955) | Among all with known gender and HIV-status (n=955) |
||||
|---|---|---|---|---|---|---|
| Infected with HIV | p-value | Females infected with HIV (n=356) | p-value | Males infected with HIV (n=599) | p-value | |
| Total | 31% (299/955) | - | 53% (187/356) | - | 19% (112/599) | <0.001 |
| Admission year | 0.479 | 0.902 | 0.449 | |||
| 2011 | 33% (117/358) | 53% (72/136) | 20% (45/222) | |||
| 2012 | 30% (182/597) | 52% (115/220) | 18% (67/377) | |||
| Median age at admission in years* | 35 (29–40) (n=299) |
<0.001 | 35 (29–40) (n=187) |
<0.001 | 35 (30–39) (n=112) |
<0.001 |
| Relationship status | 0.095 | 0.651 | 0.021 | |||
| Single | 30% (269/886) | 53% (167/315) | 18% (102/571) | |||
| Married | 45% (19/42) | 45% (13/29) | 46% (6/13) | |||
| Divorced | 30% (3/10) | 50% (3/6) | 0% (0/4) | |||
| Cohabiting | 100% (1/1) | 100% (1/1) | -% (0/0) | |||
| Occupation | <0.001 | 0.001 | <0.001 | |||
| Unemployed | 31% (136/437) | 60% (93/156) | 15% (43/281) | |||
| Skilled | 100% (2/2) | -% (0/0) | 100% (2/2) | |||
| Student | 9% (5/55) | 15% (3/20) | 6% (2/35) | |||
| Professional | 33% (5/15) | 22% (2/9) | 50% (3/6) | |||
| Self-employed | 32% (7/22) | 40% (4/10) | 25% (3/12) | |||
| Blue Collar | 44% (58/132) | 61% (27/44) | 35% (31/88) | |||
| White Collar | 28% (15/53) | 41% (12/29) | 13% (3/24) | |||
| Education level | 0.002 | <0.001 | 0.428 | |||
| None/Reception | 18% (3/17) | 25% (1/4) | 15% (2/13) | |||
| Primary incomplete | 38% (25/66) | 86% (18/21) | 16% (7/45) | |||
| Primary complete | 44% (36/81) | 62% (24/39) | 29% (12/42) | |||
| Secondary incomplete | 31% (94/301) | 55% (61/110) | 17% (33/191) | |||
| Secondary complete | 33% (59/180) | 53% (39/74) | 19% (20/106) | |||
| Tertiary incomplete | 0% (0/6) | 0% (0/1) | 0% (0/5) | |||
| Tertiary complete | 20% (28/141) | 29% (17/58) | 13% (11/83) | |||
| Area of residence | 0.553 | 0.857 | 0.668 | |||
| Village | 32% (88/274) | 54% (56/103) | 19% (32/171) | |||
| City | 29% (66/229) | 51% (42/83) | 16% (24/146) | |||
| Town | 33% (135/410) | 54% (84/156) | 20% (51/254) | |||
median age among all HIV infected in the group; p-values represent Wilcoxon rank-sum test of median age of HIV positive patients compared with those HIV negative.
HIV prevalence among admitted SPH patients vs. general community –
Comparing HIV infection rates among SPH inpatients with community prevalence estimates from the Botswana AIDS Impact Survey IV (BAISIV) (23), rates among 19–24 year olds appear significantly higher among women hospitalized at SPH (F Sbrana: 23% (14/62) vs. BAISIV: 13.4%, p=0.017), but not among men of this age group (M Sbrana: 6% (9/144) vs. BAISIV: 4.6%, p=0.172). Among 25–49 year olds in Botswana communities, HIV infection rates again appeared higher among women hospitalized at SPH (F SPH: 59% (172/291) vs. BAISIV: 38.5%, p<0.001), however we noted a lower rate of HIV-infection among hospitalized men of this age group (M SPH: 22.9% (103/450), vs. BAISIV: 29.1%, p=0.002).
HIV prevalence by psychiatric diagnoses –
Rates of HIV appeared higher among patients with particular diagnoses. Nearly half (53%, 51/97) of patients with stress related and somatoform disease and a similar proportion of patients with organic mental diseases (55%, 24/44) were documented as HIV-infected. Some 32% (57/176) of patients with mood (affective) disorders were documented HIV-positive, as were 31% (8/26) with personality disorders. Among some common disorder classifications like schizophrenia, schizotypal and other disorders (28%, 152/545) and substances use disorders (15%, 22/150), patient HIV-infection rates were lower than among admissions overall.
Table IV presents rates of documented HIV-infection by gender. Due to varying transmission dynamics and different rates of missing data, our analysis looked at HIV-prevalence among different psychiatric diagnoses separately for men and women.
Table IV:
Documented psychiatric diagnoses and HIV status at the most recent admission, by gender
| ICD General Classification and Psychiatric Diagnoses | HIV INFECTED - OVERALL | HIV INFECTED FEMALES | HIV INFECTED MALES |
|||||
|---|---|---|---|---|---|---|---|---|
| a/n* | % | a/n* | % | p-value ** | a/n* | % | p-value *** | |
| All diagnoses | 299/955 | 31.3% | 187/356 | 52.5% | - | 112/599 | 18.7% | - |
| 1. Organic mental disorders | 24/44 | 54.5% | 15/22 | 68.2% | 0.106 | 9/22 | 40.9% | 0.005 |
| Vascular dementia | - | - | - | - | - | - | - | - |
| Dementia in other diseases classification | 2/2 | 100.0% | 1/1 | 100.0% | 1.000 | 1/1 | 100.0% | 0.181 |
| Unspecified dementia | 0/1 | 0% | 0/1 | 0% | 0.485 | - | - | - |
| Delirium due to known physiological | 1/2 | 50.0% | 1/1 | 100.0% | 1.000 | 0/1 | 0.0% | 1.000 |
| Other mental disorders due to known | 17/20 | 85.0% | 11/13 | 84.6% | 0.015 | 6/7 | 85.7% | <0.001 |
| Personality and behavioral disorder | 0/1 | 0.0% | - | - | - | 0/1 | 0.0% | 1.000 |
| Epilepsy and recurrent seizures | 4/18 | 22.2% | 2/6 | 33.3% | 0.437 | 2/12 | 16.7% | 1.000 |
| 2. Substance use disorders | 22/150 | 14.7% | 10/19 | 52.6% | 0.917 | 12/131 | 9.2% | 0.003 |
| Alcohol related disorders | 13/65 | 20.0% | 5/10 | 50.0% | 0.925 | 8/55 | 14.6% | 0.472 |
| Cannabis related disorders | 5/53 | 9.4% | 2/4 | 50.0% | 1.000 | 3/49 | 6.1% | 0.021 |
| Sedative, hypnotic, or anxiolytic | - | - | - | - | - | - | - | - |
| Cocaine related disorders | 1/3 | 33.3% | 1/1 | 100.0% | 1.000 | 0/2 | 0.0% | 1.000 |
| Hallucinogen related disorders | 1/1 | 100.0% | 1/1 | 100.0% | 1.000 | - | - | - |
| Other psychoactive substance related | 2/28 | 7.1% | 1/3 | 33.3% | 0.613 | 1/25 | 4.0% | 0.066 |
| 3. Schizophrenia, schizotypal and other psychotic disorders | 152/545 | 27.9% | 90/177 | 50.9% | 0.818 | 62/368 | 16.8% | 0.356 |
| Schizophrenia | 83/359 | 23.1% | 45/89 | 50.6% | 0.843 | 38/270 | 14.1% | 0.028 |
| Schizotypal disorder | 0/1 | 0.0% | - | - | - | 0/1 | 0.0% | 1.000 |
| Delusional disorders | 5/9 | 55.6% | 3/4 | 75.0% | 0.624 | 2/5 | 40.0% | 0.225 |
| Brief psychotic disorder | 27/83 | 32.5% | 13/32 | 40.6% | 0.199 | 14/51 | 27.5% | 0.073 |
| Schizoaffective disorders | 36/91 | 39.6% | 28/51 | 54.9% | 0.598 | 8/40 | 20.0% | 0.752 |
| Other psychotic disorders not due to substance/physiological condition | ½ | 50.0% | 1/1 | 100.0% | - | 0/1 | 0.0% | 1.000 |
| 4. Mood(affective)disorders | 57/176 | 32.4% | 39/93 | 41.9% | 0.034 | 18/83 | 21.7% | 0.371 |
| Manic episode | 4/22 | 18.2% | 2/8 | 25.0% | 0.164 | 2/14 | 14.3% | 1.000 |
| Bipolar disorder | 20/76 | 26.3% | 12/35 | 34.3% | 0.033 | 8/41 | 19.5% | 0.813 |
| Major depressive disorder, single episode, mild | 0/6 | 0.0% | 0/3 | 0.0% | 0.113 | 0/3 | 0.0% | 1.000 |
| Major depressive disorder, single episode, moderate | 30/67 | 44.8% | 22/43 | 51.2% | 0.965 | 8/24 | 33.3% | 0.049 |
| Major depressive disorder, recurrent | 1/3 | 33.3% | 1/2 | 50.0% | 1.000 | 0/1 | 0.0% | 1.000 |
| Persistent mood [affective] disorders | 1/1 | 100.0% | 1/1 | 100.0% | 1.000 | - | - | - |
| Unspecified mood [affective] disorder | 1/1 | 100.0% | 1/1 | 100.0% | 1.000 | - | - | - |
| 5. Neurotic, stress-related and somatoform disorders | 51/97 | 52.6% | 29/43 | 67.4% | 0.026 | 22/54 | 40.7% | <0.001 |
| Other anxiety disorders | 24/29 | 82.8% | 11/12 | 91.7% | 0.005 | 13/17 | 76.5% | <0.001 |
| Reaction to severe stress, and adjustment disorders | 9/25 | 36.0% | 4/7 | 57.1% | 1.000 | 5/18 | 27.8% | 0.347 |
| Dissociative and conversion disorders | - | - | - | - | - | - | - | - |
| Suicide attempt (seems to relate to trauma) | 18/43 | 41.9% | 14/24 | 58.3% | 0.487 | 4/19 | 22.1% | 0.762 |
| 6. Disorders assoc. w/physical, physiological factors | 2/4 | 50.0% | 2/4 | 50.0% | 1.000 | - | - | - |
| Puerperal psychosis | 2/4 | 50.0% | 2/4 | 50.0% | 1.000 | - | - | - |
| Abuse of non-psychoactive substances | - | - | - | - | - | - | - | - |
| 7. Personality disorders | 8/26 | 30.8% | 5/9 | 55.6% | 0.804 | 3/17 | 17.6% | 1.000 |
| Paranoid personality disorder | 2/7 | 28.6% | 2/3 | 66.7% | 1.000 | 0/4 | 0.0% | 1.000 |
| Schizoid personality disorder | 1/2 | 50.0% | 1/1 | 100.0% | 1.000 | 0/1 | 0.0% | 1.000 |
| Antisocial personality disorder | 1/11 | 9.1% | 0/3 | 0.0% | 0.113 | 1/8 | 12.5% | 1.000 |
| Borderline personality disorder | 1/2 | 50.0% | - | - | - | 1/2 | 50.0% | 0.330 |
| Personality disorder, unspecified | 2/3 | 66.7% | 2/2 | 100.0% | 0.499 | 0/1 | 0.0% | 1.000 |
| Other impulse disorders | 1/1 | 100.0% | - | - | - | 1/1 | 100.0% | 0.330 |
| 8. Mental retardation | 1/3 | 33.3% | 1/1 | 100.0% | 1.000 | 0/2 | 0.0% | 1.000 |
| Mild mental retardation | 1/3 | 33.3% | 1/1 | 100.0% | 1.000 | 0/2 | 0.0% | 1.000 |
| 9. Disorders of psychological development | - | - | - | - | - | - | - | - |
| Other pervasive developmental disorders | - | - | - | - | - | - | - | - |
| 10. Childhood and adolescent disorders | 1/7 | 14.3% | 1/2 | 50.0% | 1.000 | 0/5 | 0.0% | 0.591 |
| Conduct disorder confined to family context | 1/3 | 33.3% | 1/1 | 100.0% | 1.000 | 0/2 | 0.0% | 1.000 |
| Conduct disorder, childhood-onset type | 0/1 | 0.0% | - | - | - | 0/1 | 0.0% | 1.000 |
| Conduct disorder, unspecified | 0/2 | 0.0% | - | - | - | 0/2 | 0.0% | 1.000 |
| Selective mutism | - | - | - | - | - | - | - | - |
| Adult onset fluency disorder | 0/1 | 0.0% | 0/1 | 0.0% | 0.485 | - | - | - |
| 11. Unspecified mental disorders | 2/27 | 7.4% | 0/3 | 0.0% | 0.113 | 2/24 | 8.3% | 0.284 |
| Mental disorder, not otherwise specified | 2/27 | 7.4% | 0/3 | 0.0% | 0.113 | 2/24 | 8.3% | 0.284 |
Percent is calculated out of all patients with the psychiatric disorder diagnosis who have a known HIV status. As some patients may be diagnosed with more than one psychiatric disorder, patients may be counted multiple times for different diagnoses.
Among female patients, p-value of chi-square test comparing proportion of HIV-positive patients with the psychiatric condition with the proportion among other psychiatric conditions.
Among male patients, p-value of chi-square test comparing proportion of HIV-positive patients with the psychiatric condition with the proportion among other psychiatric conditions.
Among women, we noted HIV-infection lower among those diagnosed with bipolar disorder (F bipolar disorder: 34% (12/35) vs. others: 55% (174/316), p=0.033). Rates appeared higher among women with particular mental disorders due to known physiological conditions (ICD-10 code group F06) (F mental disorders due to known physiological conditions: 85% (11/13) vs. other 50% (181/360), p=0.015) and higher among those with panic disorder, generalized anxiety disorder and other mixed anxiety and specific anxiety disorders (ICD-10 code group F41) (F other anxiety disorder: 85% (11/13) vs. others: 50% (181/360), p=0.015).
Among men, our analysis found HIV-infection rates higher among those with particular mental disorders due to known physiological conditions (ICD-10 code F06) (M mental disorders due to known physiological conditions: 86% (6/7) vs. others: 17% (122/577), p<0.001), depression (M major depressive disorder, single episode, moderate: 33% (8/24) vs. others: 18% (120/682), p<0.049), and higher among those with panic disorder, generalized anxiety disorder and other mixed anxiety and specific anxiety disorders (ICD-10 code group F41) (M other anxiety disorder: 76% (13/17) vs. others: 17% (115/689), p<0.001). Documented HIV rates appeared lower among men diagnosed with substance abuse disorders (9%, 12/131), particularly those with cannabis use disorders (M cannabis use disorder: 6% (3/49) vs. others: 19% (125/657), p=0.024), and lower among those with schizophrenia (M schizophrenia spectrum disorder: 14% (38/270) vs. others: 21% (90/436), p=0.028).
We compared HIV prevalence among patients with affective disorder and those with schizophrenia spectrum disorder. Men diagnosed with affective disorders had marginally higher rates of HIV compared with men with schizophrenia spectrum disorders (excluding dual-diagnosed, M affective: 24% (16/67) vs. schizophrenia spectrum: 16% (57/347), p=0.071). However, women with affective disorders had marginally lower HIV rates compared with women with schizophrenia spectrum disorders (excluding dual-diagnosed, F affective: 43% (37/87) vs. schizophrenia spectrum: 51% (88/171), p=0.087).
Based on the Directed Acyclic Graph constructed for HIV-infection among psychiatric admissions (Figure 1), we estimated total effects for education and age. Among hospitalized women, education appeared to have a protective effect against HIV-infection. The odds of HIV infection among women with at least secondary school level education were 43% less than among women with less education (OR 0.57 95% CI 0.35–0.91, after adjustment for age). Among women, age was associated with a modest increase in risk of HIV-infection (OR 1.06 95% CI 1.03–1.09, after adjustment for education level). Among hospitalized men, age was also modestly associated with an increased risk of HIV infection (OR 1.07 95% 1.04–1.10, after adjusting for education level).
DISCUSSION
This is the first study in Botswana that examined rates of HIV infection among psychiatric inpatients. Several studies conducted in the United States and elsewhere in the developed world have shown that people with mental illness have higher rates of HIV infection than the general population, and that rates among psychiatric inpatients are elevated relative to those receiving outpatient care (46). Findings from this study of hospitalized, mentally-ill patients suggest that although this may be true for women in Botswana, this may not be the case for men.
This study found greatly elevated rates of HIV among female inpatients and this finding held in the sensitivity analysis (see above). This finding appears consistent with other studies that assert women are at greater risk of HIV infection: women face an increased risk of acquiring infection during heterosexual intercourse with an HIV seropositive partner as compared with men and, generally less power to assert choice in reproductive decision making. This study supports that mentally ill women whose mental illnesses required hospitalization experienced increased vulnerability to HIV infection. Generally, community dwelling persons with mental illness are at increased risk for HIV due to homelessness, poor decision making, and higher rate of sex work or trading sex for goods and services. Complicating matters is that these patients may not recognize that they are at increased risk, or even necessarily define themselves as trading sex, since they may perceive themselves as just having sex with the person who’s letting them sleep in their apartment or on their couch or feeding them.
From prior studies, we expected higher rates of HIV among people with affective disorders compared with people with schizophrenia spectrum disorders. Findings from our study appear consistent with this for men, but not women, among whom HIV prevalence was 8% higher among patients diagnosed with schizophrenia spectrum disorders compared with affective disorders. We were not able to examine how substance abuse interacted with various mental illnesses, since the only indicator of substance abuse was a formal diagnosis of a substance abuse disorder. Himelhoch and his colleagues found that in the absence of substance abuse, rates of HIV among veterans with schizophrenia were actually lower than in the general population, perhaps reflecting the difficulty that the negative symptoms of the disease has for men and sexual behavior (7).
This paper presents analyses of cross-sectional data that limited our ability to establish whether a psychiatric condition occurred before, or following, HIV infection. It is plausible, for example, that patients were admitted with a stress related or somatoform disorders such as adjustment disorder, shortly after learning about their HIV diagnosis. The psychiatric admission diagnosis in such instances could arguably have arisen as an initial manifestation of the HIV infection, or awareness of it, to contribute in part to the higher rates of HIV among the mentally ill inpatient population. There is recent evidence that severity of psychiatric illness is related to elevated rates of HIV (47), as well as evidence that psychiatric inpatients have higher rates of HIV than do outpatients (46).
The classification of a disorder diagnosis based on the data available from medical records presented a number of analytical challenges. Although abstractors did receive training to collect the data, medical chart documentation and completeness varies with care provider, and classifications assigned to each patient’s diagnosis arose from each data abstractor’s interpretation of the information they found in the patient chart. Some ICD disease classifications, ‘other mental disorders due to known physiological conditions’ and ‘other anxiety disorders’, had very high rates of HIV and low numbers of cases, requiring further study.
The study relies on information on co-occurrence for patients with specific psychiatric conditions and documentation of HIV infection in medical records of admissions. Detecting differences in HIV rates among those with rarer psychiatric conditions involved higher Type II error – failing to detect a statistically significant difference in HIV-infection rate among those with a particular disorder – compared with those with more common psychiatric conditions. To conclude whether patients with rarer disorders had higher or lower infection rates would require a larger sample size or employ matching or other statistical techniques.
Concerning documentation of HIV status, since 2004, a national policy has mandated routine testing of all patients for HIV (33); all patients admitted to inpatient care at SPH routinely test for HIV unless they opted-out. In 2011–12, routine testing was accepted by over 80% of patients; facility reviews carried out in other years suggest as many as 97% of patients accepted testing (48). This suggests that a majority of SPH patients without documented HIV status had actually been tested and reflection of this in the patient’s chart did not relate to the outcome itself or patient characteristics, but systemic issues. During the study period, the medical records at SPH underwent conversion to an electronic medical record system. Although this ultimately will improve the quality of record keeping, the process presented logistical difficulty in identifying when physical records were being used and their location, and when a given inpatient had transitioned to an electronic record. Given the robust findings obtained by the study, the likelihood that the results arose from errors in record keeping or bias arising from patients without HIV status data in either physical or electronic records appears remote.
Findings of this study suggest that systematic screening for HIV infection among patients – particularly women - with mental illness, and screening for mental illness among women infected with HIV, may support detection of dually diagnosed patients in Botswana. HIV counselling and testing services should be made available at all outpatient mental health settings for both men and women. As well, incorporating monitoring and management of comorbid psychiatric treatment into the care plan for HIV-infected patients is warranted, given the likelihood that symptoms associated with depression, anxiety and psychosis adversely affect immune function (49,50,51). Furthermore, HIV program planners should consider introducing specific HIV prevention interventions targeting women with mental illness. These could include broadening guidelines to include women with mental illness as a high-risk group eligible for PrEP, and developing specific HIV prevention interventions that help mentally-ill women to recognize their vulnerability to infection, exploitation, and to effectively negotiate condom use with sexual partners.
REFERENCES:
- 1.UNAIDS. HIV and AIDS estimates (2015). [Google Scholar]
- 2.De Korte D, Mazonde P, Darkoh E. Perspectives and Practice in Antiretroviral Treatment. Introducing ARV Therapy in the Public Sector in Botswana Case Study. Geneva: World Health Organization; 2004. [Google Scholar]
- 3.Botswana Ministry of Health. Botswana National HIV & AIDS Treatment Guidelines, 2012. Gaborone, Botswana: Ministry of Health. [Google Scholar]
- 4.Botswana Ministry of Health. Handbook of the Botswana 2016 Integrated HIV Clinical Care Guidelines. Botswana: Ministry of Health. [Google Scholar]
- 5.Blank MB, Mandell DS, Aiken L, Hadley TR. Co-occurrence of HIV and serious mental illness among Medicaid recipients. Psychiatr Serv. 2002;53(7):868–73. [DOI] [PubMed] [Google Scholar]
- 6.Walkup J, Crystal S, Sambamoorthi U. Schizophrenia and major affective disorder among Medicaid recipients with HIV/AIDS in New Jersey. Am J Public Health. 1999;89(7):1101–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Himelhoch S, McCarthy JF, Ganoczy D, Medoff D, Dixon LB, Blow FC. Understanding associations between serious mental illness and HIV among patients in the VA Health System. Psychiatr Serv. 2007;58(9):1165–72. [DOI] [PubMed] [Google Scholar]
- 8.Perkins DO, Stern RA, Golden RN, Murphy C, Naftolowitz D, Evans DL. Mood disorders in HIV infection: prevalence and risk factors in a nonepicenter of the AIDS epidemic. Am J Psychiatry. 1994;151(2):233–6. [DOI] [PubMed] [Google Scholar]
- 9.Morrison MF, Petitto JM, Ten Have T, et al. Depressive and Anxiety Disorders in Women with HIV Infection. Am J Psychiatry. 2002;159(5):789–96. [DOI] [PubMed] [Google Scholar]
- 10.Brown GR, Rundell JR, McManis SE, Kendall SN, Zachary R, Temoshok L. Prevalence of psychiatric disorders in early stages of HIV infection. Psychosom Med. 1992;54(5):588–601. [DOI] [PubMed] [Google Scholar]
- 11.Williams JW, Rabkin JG, Remien RH, Gorman JM, Ehrhardt AA. Multidisciplinary baseline assessment of homosexual men with and without human immunodeficiency virus infection. II. Standardized clinical assessment of current and lifetime psychopathology. Arch Gen Psychiatry. 1991;48(2):124–30. [DOI] [PubMed] [Google Scholar]
- 12.Rosenberger PH, Bornstein RA, Nasrallah HA, et al. Psychopathology in human immunodeficiency virus infection: lifetime and current assessment. Compr Psychiatry. 1993;34(3):150–8. [DOI] [PubMed] [Google Scholar]
- 13.Shrier LA, Harris SK, Sternberg M, Beardslee WR. Associations of depression, self-esteem, and substance use with sexual risk among adolescents. Prev Med. 2001;33(3):179–89. [DOI] [PubMed] [Google Scholar]
- 14.Nduna M, Jewkes RK, Dunkle KL, Shai NP, Colman I. Associations between depressive symptoms, sexual behaviour and relationship characteristics: a prospective cohort study of young women and men in the Eastern Cape, South Africa. J Int AIDS Soc. 2010;13:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Perretta P, Akiskal HS, Nisita C, et al. The high prevalence of bipolar II and associated cyclothymic and hyperthymic temperaments in HIV-patients. J Affect Disord. 1998;50(2–3):215–24. [DOI] [PubMed] [Google Scholar]
- 16.Ayuso-Mateos JL, Montanes F, Lastra I, Picazo de la Garza J, Ayuso-Gutierrez JL. HIV infection in psychiatric patients: an unlinked anonymous study. Br J Psychiatry. 1997; 170:181–5. [DOI] [PubMed] [Google Scholar]
- 17.Cournos F, Empfield M, Horwath E, et al. HIV seroprevalence among patients admitted to two psychiatric hospitals. Am J Psychiatry. 1991;148(9):1225–30. [DOI] [PubMed] [Google Scholar]
- 18.Lundberg P, Nakasujja N, Musisi S, Thorson AE, Cantor-Graae E, Allebeck P. HIV prevalence in persons with severe mental illness in Uganda: a cross-sectional hospital-based study. Int J Ment Health Syst. 2013;7: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maling S, Todd J, Van der Paal L, Grosskurth H, Kinyanda E. HIV-1 seroprevalence and risk factors for HIV infection among first-time psychiatric admissions in Uganda. AIDS Care. 2011;23(2):171–8. [DOI] [PubMed] [Google Scholar]
- 20.Collins PY, Berkman A, Mestry K, Pillai A. HIV prevalence among men and women admitted to a South African public psychiatric hospital. AIDS Care. 2009;21(7):863–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Acuda SW, Sebit MB. Serostatus surveillance testing of HIV-I infection among Zimbabwean psychiatric inpatients, in Zimbabwe. Cent Afr J Med. 1996. September; 42 (9): 254–7. [PubMed] [Google Scholar]
- 22.UNAIDS. Prevention gap report. Geneva: UNAIDS; 2016. Available at: http://www.unaids.org/sites/default/files/media_asset/2016-prevention-gap-report_en.pdf. Accessed August 28, 2016. [Google Scholar]
- 23.Statistics Botswana/National AIDS Coordinating Authority (NACA). Preliminary Results. Botswana AIDS Impact Survey IV (BAIS IV) Stats Brief No. 2013/28 Statistics Botswana: Gaborone; 2013. [Google Scholar]
- 24.Nicolosi AA. The efficiency of male-to-female and female-to-male sexual transmission of the human immunodeficiency virus: a study of 730 stable couples. Italian Study Group on HIV Heterosexual Transmission. Epidemiology. 5(6):570–5. [DOI] [PubMed] [Google Scholar]
- 25.Andersson N, Cockcroft A. Choice-disability and HIV infection: a cross sectional study of HIV status in Botswana, Namibia and Swaziland. AIDS Behav. 2012;16(1):189–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kalmuss D Nonvolitional sex and sexual health. Arch Sex Behav. 2004;33(3):197–209. [DOI] [PubMed] [Google Scholar]
- 27.Ramjee G, Daniels B. Women and HIV in Sub-Saharan Africa. AIDS Res Ther. 2013;10:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mabala R From HIV prevention to HIV protection: addressing the vulnerability of girls and young women in urban areas. Environ Urban. 2006;18(2):407–32. [Google Scholar]
- 29.Griesbeck M, Scully E, Altfeld M. Sex and gender differences in HIV-1 infection. Clin Sci (Lond). 2016;130(16):1435–51. [DOI] [PubMed] [Google Scholar]
- 30.Magadi MA. Understanding the gender disparity in HIV infection across countries in sub-Saharan Africa: evidence from the Demographic and Health Surveys. Sociol Health Illn. 2011;33(4):522–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Republic of Botswana. Progress Report of the National Response to the 2011 Declaration of Commitments on HIV and AIDS Reporting Period: 2014. Gaborone, Botswana: National AIDS Coordinating Agency. [Google Scholar]
- 32.Seloilwe ESE. Community mental health care in Botswana: approaches and opportunities. Int Nurs Rev. 2007;54(2):173–8. [DOI] [PubMed] [Google Scholar]
- 33.Kenyon K Routine HIV testing: a view from Botswana. Health Hum Rights. 2005; 8 (2): 21–23. [PubMed] [Google Scholar]
- 34.Botswana Ministry of Health. Botswana National HIV/AIDS Treatment Guidelines: 2008 Version. Department of HIV/AIDS Prevention and Care. Gaborone, Botswana: 1 November 2008 Available at: http://www.moh.gov.bw/Publications/HIVAIDS%20TREATMENT%20GUIDELINES.pdf. Accessed June 12, 2016 [Google Scholar]
- 35.Elwert F Chapter 13. Graphical Causal Models In Morgan SL (ed). Handbook of Causal Analysis for Social Research, Handbook of Sociology and Social Research. Dordrecht, Netherlands: Springer Science + Business Media, 2013. DOI 10.1007/978-94-007-6094-3_13 . Downloaded from URL: 10.1007/978-94-007-6094-3_13http://www.ssc.wisc.edu/soc/faculty/pages/docs/elwert/Elwert%202013.pdf. Downloaded from URL: http://www.ssc.wisc.edu/soc/faculty/pages/docs/elwert/Elwert%202013.pdf . [DOI] [Google Scholar]
- 36.Cole SR, Platt RW, Schisterman EF, et al. Illustrating bias due to conditioning on a collider. Int J Epidemiol. 2010;39(2):417–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shahar E, Shahar DJ. Causal diagrams and the cross-sectional study. Clin Epidemiol. 2013;5:57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shrier I, Platt RW. Reducing bias through directed acyclic graphs. BMC Med Res Methodol. 2008;8:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Textor J, Hardt J, Knuppel S. DAGitty: a graphical tool for analyzing causal diagrams. Epidemiology. 2011;22(5):745. [DOI] [PubMed] [Google Scholar]
- 40.Langen TT. Gender power imbalance on women’s capacity to negotiate self-protection against HIV/AIDS in Botswana and South Africa. Afr Health Sci. 2005;5(3):188–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Weiser SD, Leiter K, Bangsberg DR, et al. Food insufficiency is associated with high-risk sexual behavior among women in Botswana and Swaziland. PLoS Med. 2007;4(10):1589–97; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ho-Foster A, Laetsang D, Masisi M, et al. Gender-specific patterns of multiple concurrent sexual partnerships: a national cross sectional survey in Botswana. AIDS Care. 2010;22(8):1006–11. [DOI] [PubMed] [Google Scholar]
- 43.Multiprocessor STATA (for Windows) [computer program]. Version 13.1. College Station, TX: StataCorp; 2013. [Google Scholar]
- 44.Multiple Imputation in Stata. The University of Wisconsin - Madison: Social Science Computing Cooperative. October 2012. Downloaded from URL: https://www.ssc.wisc.edu/sscc/pubs/stata_mi_intro.htm
- 45.White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011;30(4):377–99. [DOI] [PubMed] [Google Scholar]
- 46.Blank MB, Himelhoch SS, Balaji AB, et al. A multisite study of the prevalence of HIV with rapid testing in mental health settings. Am J Public Health. 2014;104(12):2377–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wu ES, Rothbard A, Blank MB. Using psychiatric symptomatology to assess risk for HIV infection in individuals with severe mental illness. Community Ment Health J. 2011;47(6):672–8. [DOI] [PubMed] [Google Scholar]
- 48.Personal communication with Dr Leech, Deputy Superintendent, Sbrana Psychiatric Hospital, on June 10, 2016. [Google Scholar]
- 49.Blume J, Douglas SD, Evans DL. Immune suppression and immune activation in depression. Brain Behav Immun. 2011;25(2):221–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Leserman J, Petitto JM, Perkins DO, Folds JD, Golden RN, Evans DL. Severe stress, depressive symptoms, and changes in lymphocyte subsets in human immunodeficiency virus-infected men. A 2-year follow-up study. Arch Gen Psychiatry. 1997;54(3):279–85. [DOI] [PubMed] [Google Scholar]
- 51.Evans DL, Ten Have TR, Douglas SD, et al. Association of depression with viral load, CD8 T lymphocytes, and natural killer cells in women with HIV infection. Am J Psychiatry. 2002;159(10):1752–9. [DOI] [PubMed] [Google Scholar]