Abstract
Purpose
To report diffuse lamellar keratitis (DLK) occurring in an eye that underwent epithelium-off (epi-off) corneal cross-linking (CXL) as a treatment for post-surgical ectasia and the successful treatment of progressive ectasia with a novel epi-on CXL and conductive keratoplasty (CK) treatment.
Observations
A 42-year-old man presented with corneal ectasia in his right eye 3 years after laser in situ keratomileusis (LASIK) surgery. He underwent epi-off corneal CXL using the Dresden protocol. Grade II DLK was diagnosed within days of CXL. Despite successful treatment of DLK, best-corrected visual acuity in the right eye deteriorated over the next 4 months due to progression of ectasia and remained worse than the patient's pre-operative baseline 1 year after epi-off CXL. Because of apparent disease progression, despite his CXL treatment, the patient underwent a novel, transepithelial CXL (TE-CXL) treatment combined with conductive keratoplasty (CK). This treatment improved his vision and stabilized his ectasia without subsequent DLK. Approximately 3 years after CK and TE-CXL, his eye remains stable with 4 Snellen lines of improved vision and no progression of ectasia.
Conclusion and importance
Epithelium-off CXL is used increasingly to treat post-LASIK ectasia. First, in this case, DLK occurred after epi-off CXL. We suggest careful scrutiny of such cases as DLK is difficult to identify after epi-off CXL. Second, the epi-off CXL was unsuccessful in stopping the post-LASIK ectasia. Transepithelial CXL successfully treated the ongoing ectasia after resolution of the DLK with no subsequent re-occurrence of DLK. We suggest that TE-CXL may provide a successful initial treatment for post-LASIK ectasia that also minimizes the epithelial disruption that can lead to DLK.
Keywords: DLK, Epithelium-off, Dresden protocol, CXL, LASIK, Complications, Transepithelial
1. Introduction
Diffuse lamellar keratitis (DLK) occurs when the lamellar interface created during laser in situ keratomileusis (LASIK) does not completely heal and remains a potential space for interface inflammation.1 Diffuse lamellar keratitis may occur due to epithelial abrasions or erosions following LASIK surgery,2,3 after epithelial debridement when using photorefractive keratectomy for post-LASIK enhancements,4,5 or after epithelium-off (epi-off) corneal cross-linking (CXL) for post-LASIK ectasia.6, To date, there has been only one published case report of DLK as a complication of epi-off CXL.10 However, because epi-off CXL may be utilized with increasing frequency, the incidence of DLK as a complication also may be expected to increase.
We present a patient who developed DLK after treatment with epi-off CXL for post-refractive ectasia. Despite resolution of the DLK, his ectasia progressed with deterioration in best-corrected visual acuity, increased myopia, and astigmatism.
2. Case report
A 42-year-old man presented to the Wilmer Johns Hopkins Cornea Service with iatrogenic post-refractive ectasia in both eyes 3 years after undergoing bilateral myopic LASIK surgery and 2 enhancements to the right eye. At presentation, his uncorrected visual acuity was 20/400 OD and 20/20 OS. His right eye corrected to 20/50 with a −5.00 sphere. Corneal tomography with Pentacam (Oculus, Wetzler, Germany) was significant for irregular astigmatism, inferior steepening, posterior corneal elevation and corneal stromal thinning consistent with post-LASIK ectasia in the right eye.
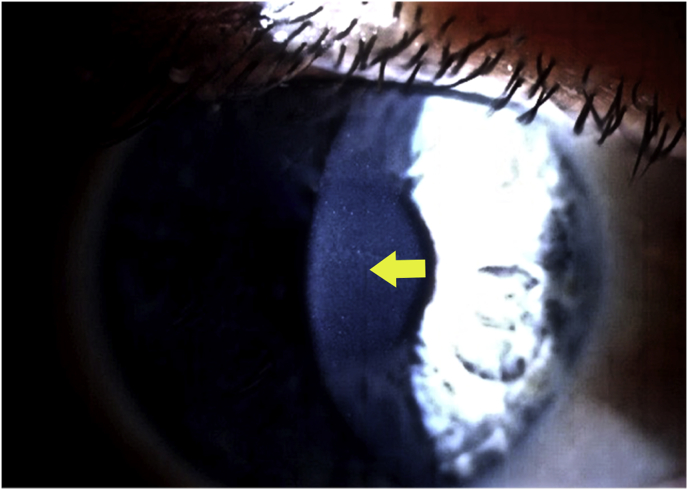
Corneal cross-linking was recommended for treatment of his ectasia. The patient underwent standard Dresden protocol epi-off CXL to the right eye (3mW/cm2, 30 minutes of UVA). The central corneal thickness was 409 μm by pachymetry at the time of the epi-off CXL procedure. Postoperatively, the patient developed sub-flap central infiltrates in the right eye, a clinical picture consistent with a diagnosis of interface inflammation (Fig. 1). Treatment with frequent topical dexamethasone was initiated with good clinical response.
Fig. 1.
Slit-lamp photography of stage II diffuse lamellar keratitis 12 days after the patient's initial epithelium-off, Dresden-protocol, corneal cross-linking. Yellow arrow shows visible clumped opacities in the lamellar interface. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
Four months after epi-off CXL, the interface inflammation had completely resolved; however best-spectacle corrected visual acuity in the right eye was reduced to 20/400 with −8.00 + 2.00 × 170° due to progression of the ectasia. One year after epi-off CXL, the patient's best-corrected visual acuity was still only 20/160 (−8.25 + 2.00 × 170) and a rigid contact lens was fitted to provide useful vision of 20/40.
Three years after the epi-off CXL procedure, the patient's myopia and astigmatism had worsened to −11.00 + 6.00 × 95 and the KMax increased from 49.2 to 51.5 diopters over a period of 1 year, suggesting continuing ectatic progression. Repeat CXL was recommended as salvage therapy prior to consideration of keratoplasty. The thinnest corneal pachymetry by Pentacam was 340 μm when the patient underwent thermokeratoplasty to regularize the cornea by conductive keratoplasty (CK; Refractec, Bloomington, MN) followed by a novel, transepithelial CXL (TE-CXL) procedure (CXLO; CXL Ophthalmics, Encinitas, California) 24 hours later.7,8
In brief, 4 CK spots were placed over the steep infero-central area to flatten the corneal apex as described previously.6,7 Under topical anesthesia, a novel, proprietary, TE-CXL system was utilized for 20 minutes and adequate stromal loading was confirmed by slit-lamp evaluation.9,10 The eye was exposed to ultraviolet light (365 nm) at 4 mW/cm2 cycled off and on with a proprietary duty cycle for 20 minutes (CXL Ophthalmics, Encinitas, CA).
Slit-lamp examination revealed no lamellar or other inflammation and the patient comfortably returned to work the day after the procedure. One year after his TE-CXL and CK, best-corrected visual acuity was 20/30–2 with a moderate myopic astigmatic error (−2.00 + 3.50 × 42). In addition, tomography demonstrated marked improvement in the amount of irregular astigmatism and flattening of the cornea. Approximately 3 years after CK and TE CXL, his eye remains stable without signs of progressive ectasia and with a good visual outcome.
3. Discussion
This report constitutes the second published case of DLK resulting from CXL treatment in which the epithelium was surgically removed. Diffuse lamellar keratitis is a well-recognized complication of LASIK, with published incidence estimates ranging from 0.1% to 7.7% with microkeratome flaps and 0.2%–19.4% using femtosecond laser flaps.5 To date, only one case report10 and a single study11 have documented DLK as a complication of epithelium-off CXL. However, LASIK involves the creation of a lamellar interface creating a potential space for interface inflammation as a result of epithelial disruption. Given the increasing usage of epi-off CXL after the Food and Drug Administration's 2016 approval of this procedure to treat post-surgical ectasia, the incidence of DLK as a complication of epi-off CXL may increase as more postsurgical eyes undergo epithelial removal. Unfortunately, epithelial defects and edema, as well as stromal swelling, can make early diagnosis and treatment of DLK difficult. Careful observation during the acute healing phase following surgical CXL procedures is therefore strongly advised otherwise this condition can be overlooked, under-reported and untreated.
A recent prospective study supports the association between low-grade DLK and CXL.11 This study treated healthy myopic eyes with a customized protocol of CXL through the flap immediately after LASIK to prevent iatrogenic ectasia and compared these to eyes treated with LASIK alone. In the group treated with both LASIK and CXL, 38% of eyes had stage 1 or 2 DLK on post-operative day one compared to only 4% in the group that received LASIK alone. This finding was statistically significant. Of note, DLK resolved after one week in all eyes with topical steroid treatment and none of the eyes developed stage 3 DLK. Interestingly, CXL was performed after the LASIK flap was repositioned and yet DLK developed in the treated eyes despite the absence of a frank epithelial defect.
This report also represents the second published case of the successful usage of a novel TE-CXL procedure to treat post-LASIK ectasia refractory to epi-off CXL.6 This patient's ectasia had progressed despite traditional epi-off CXL. The failure rate of the standard epi-off CXL is known to be as high as 7.6%, especially in more advanced cases of ectasia.12 In the current case, novel treatment with CK followed by non-invasive TE-CXL with a proprietary transepithelial riboflavin formulation and system9 successfully treated advanced ectasia and stabilized the patient's vision without complications such as DLK.
4. Conclusion
In this case, the patient not only failed to achieve the expected stabilization in visual acuity and corneal topography after traditional epi-off CXL therapy for post-LASIK ectasia, but the procedure induced an additional complication (DLK).This demonstrates two points. One is the occurrence of DLK as a complication of epi-off CXL. Two, TE-CXL can successfully treat ongoing postsurgical ectasia after epi-off CXL. We also suggest that effective TE-CXL8 may, by avoiding surgical removal or disruption of the corneal epithelium, reduce the risk of DLK, infection, scarring and extended recovery that can occur as a result of epi-off CXL6,9 in this situation.
Patient consent
Oral, but not written, consent was obtained to publish the case report. This report does not contain any personal information that could lead to identification of the patient.
Acknowledgments and disclosures
Funding
No funding or grant support
Conflicts of interest
Dr. Rubinfeld has a financial interest in CXL Ophthalmics, Encinitas, CA and CXLUSA, LLC, Bethesda, MD, USA.
The following authors have no financial disclosures
DBM, USS, ASJ.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship"
Acknowledgements
None.
References
- 1.Smith R.J., Maloney R.K. Diffuse lamellar keratitis: a new syndrome in lamellar refractive surgery. Ophthalmology. 1998;105(9):1721–1726. doi: 10.1016/S0161-6420(98)99044-3. [DOI] [PubMed] [Google Scholar]
- 2.Shah M.N., Misra M., Wihelmus K.R., Koch D.D. Diffuse lamellar keratitis associated with epithelial defects after laser in situ keratomileusis. J Cataract Refract Surg. 2000;26(9):1312–1318. doi: 10.1016/s0886-3350(00)00570-8. [DOI] [PubMed] [Google Scholar]
- 3.Jeng B.H., Stewart J.M., McLeod S.D., Hwang D.G. Relapsing diffuse lamellar keratitis after laser in situ keratomileusis associated with recurrent erosion syndrome. Arch Ophthalmol. 2004;122(3):396–398. doi: 10.1001/archopht.122.3.396. [DOI] [PubMed] [Google Scholar]
- 4.Aboumerhi H., Erzurum S.A. Late-onset diffuse lamellar keratitis after surface ablation. JCRS Online Case Reports. 2014;2(3):61–62. [Google Scholar]
- 5.De Paula F.H., Khairallah C.G., Niziol L.M., Musch D.C., Shtein R.M. Diffuse lamellar keratitis after laser in situ keratomileusis with femtosecond laser flap creation. J Cataract Refract Surg. 2012;38(6):1014–1019. doi: 10.1016/j.jcrs.2011.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rubinfeld R.S., Epstein R.H., Majmudar P.A., Kim D., Choi M., Epstein R.J. Transepithelial crosslinking retreatment of progressive corneal ectasia unresponsive to classic crosslinking. J Cataract Refract Surg. 2017;43(1):131–135. doi: 10.1016/j.jcrs.2016.11.038. [DOI] [PubMed] [Google Scholar]
- 7.Cummings A.B., Sinjab M.M., Hatch K.M. Combined corneal cross linking and other procedures: indications and application models. In: Sinjab M.M., Cummings A.B., editors. Corneal Collagen Cross Linking. Springer International Publishing AG; Cham, Switzerland: 2017. pp. 135–138. [Google Scholar]
- 8.Stulting R.D., Trattler W.B., Woolfson J.M. Corneal crosslinking without epithelial removal. J Cataract Refract Surg. 2018;44(11):1363–1370. doi: 10.1016/j.jcrs.2018.07.029. ePublished Sept, 2018. [DOI] [PubMed] [Google Scholar]
- 9.Rubinfeld R.S., Stulting R.D., Gum G.G., Talamo J.H. Quantitative analysis of corneal stromal riboflavin concentration without epithelial removal. J Cataract Refract Surg. 2018;44(2):237–242. doi: 10.1016/j.jcrs.2018.01.010. Erratum 2018;44(4):523. [DOI] [PubMed] [Google Scholar]
- 10.Kymionis G.D., Bouzoukis D.I., Diakonis V.F., Portaliou D.M., Pallikaris A.I., Yoo S.H. Diffuse lamellar keratitis after corneal crosslinking in a patient with post-laser in situ keratomileusis corneal ectasia. J Cataract Refract Surg. 2007;33(12):2135–2137. doi: 10.1016/j.jcrs.2007.06.070. [DOI] [PubMed] [Google Scholar]
- 11.Seiler T.G., Fischinger I., Koller T., Derhartunian V., Seiler T. Superficial corneal crosslinking during laser in situ keratomileusis. J Cataract Refract Surg. 2015;41(10):2165–2170. doi: 10.1016/j.jcrs.2015.03.020. [DOI] [PubMed] [Google Scholar]
- 12.Koller T., Mrochen M., Seiler T. Complication and failure rates after corneal crosslinking. J Cataract Refract Surg. 2009;35(8):1358–1362. doi: 10.1016/j.jcrs.2009.03.035. [DOI] [PubMed] [Google Scholar]