Abstract
Objective
This study aimed to determine the prevalence of hearing impairment in Bangladeshi people of all ages.
Methods
A nationally representative cross-sectional survey was carried out in 2013. A total of 4260 subjects (1774 males and 2486 females), with a mean age of 32 years, participated. Hearing impairment was determined by pure tone audiometry and otoacoustic emissions testing.
Results
Disabling hearing loss (greater than 40 dB loss in adults, and greater than 30 dB loss in children younger than 15 years, in their better hearing ears) was present in 9.6 per cent (95 per cent confidence interval, 8.5–10.8 per cent) of the respondents. Hearing loss was more prevalent in socio-economically deprived people and in those older than 60 years. Multiple logistic regression analysis identified age, socio-economic deprivation, family history, impacted ear wax, chronic suppurative otitis media, otitis media with effusion, and otitis externa as the significant predictors of disabling hearing loss.
Conclusion
Deafness prevention should focus mainly on chronic suppurative otitis media, otitis media with effusion, and impacted ear wax prevention, integrated within the primary healthcare system and addressing the equity issue.
Keywords: Bangladesh, Population, Hearing Impairment, Deafness, Disability Evaluation
Introduction
The burden of hearing-related disability is an important and common public health problem. The World Health Organization (WHO) reported that over 5 per cent of the world’s population has disabling hearing loss that jeopardises their daily life and livelihood.1 The estimated number of people with disabling hearing loss is 360 million, of which 32 million are children. Childhood development, especially speech and language, is seriously hampered as a result of disabling hearing loss.
Hearing impairment is a cause and consequence of poverty, especially in low and middle income countries.2 The Government of Bangladesh have estimated that hearing impairment is the second most common form of disability in Bangladesh, with economic, social, educational and vocational associations.3 Many factors, including genetic inheritance, some maternal diseases during pregnancy, various other diseases, ototoxic drugs, excessive noise over an extended period of time and ageing, are responsible for causing hearing impairment.4 Given that children are worst affected by hearing impairment, we must do our best to protect future generations from this avoidable problem.
A small-scale study carried out for the WHO in 2002 reported a prevalence of 7.9 per cent hearing impairment (in the better hearing ear) in Bangladeshi people.5 Studies in India have reported a similar prevalence (6.3 per cent).6 The impairment can be as severe as being unable to hear someone shouting (which is commonly known as deafness).
Experiences from other parts of the world indicate that half of hearing impairments are preventable through public education, early detection and effective treatment. However, for proper planning of programmes or interventions, representative data are essential to begin such an intervention. So far, nationally representative data on the prevalence of hearing impairment are not available in Bangladesh. Therefore, the present study has been carried out to determine the prevalence of disabling hearing impairment in Bangladeshi people of all ages.
Materials and methods
This survey was designed to obtain nationally representative information on the hearing impairment burden in Bangladesh. A cross-sectional study was conducted, which followed a modified WHO protocol for a population-based survey, to determine the prevalence and predictors of hearing impairment and other ear diseases.7
Study population
The target population of the survey included people of all ages who considered Bangladesh as their primary place of residence, with the following two exceptions: those visiting Bangladesh (e.g. tourists), and those who were institutionalised, including people residing in hospitals, prisons, nursing homes and dormitories.
Sampling frame
The sampling frame for this study was the population census conducted by the Bangladesh Bureau of Statistics in 2011.8 There are seven administrative divisions in Bangladesh. Each division is divided into several districts, and districts are divided into sub-districts (upazila). Within a sub-district, mauza and mahalla are the smallest geographical units with defined boundaries in rural and urban areas, respectively. They were used as primary sampling units for this study. Households from mauza and mahalla were used as the secondary sampling units; these were defined according to the Bangladesh Bureau of Statistics as ‘A dwelling in which persons either related or unrelated are living together and taking food from the same kitchen’. People who stayed in that particular household the night preceding the survey day were taken into account.
Reference population source
The country’s population is almost evenly distributed throughout its 7 divisions and 64 districts, apart from in Dhaka and Chittagong districts where it is dense as a result of large urban gatherings. The number of households is about 32 million. On average, a household consists of 4.4 persons. Urban areas are mainly metropolitan cities, city corporations and municipalities, where the population density is higher. However, the number of persons per household is very similar.8 According to the 2011 census, there were 64 407 primary sampling units (mauza and mahalla) in Bangladesh, which also included cantonment areas and depopulated areas defined as areas with less than 5 households. Cantonment and depopulated areas were excluded from this study. Therefore, the final number of primary sampling units for this survey was 58 755 (9474 urban and 49 281 rural).8
Selection of sampling units and individuals
The sampling design of this survey was based on the Non-communicable Disease Risk Factor Survey, Bangladesh 2010.9 This was a cross-sectional study adopting a multistage, geographically clustered, probability-based sampling approach, covering a representative sample of males and females of all ages.
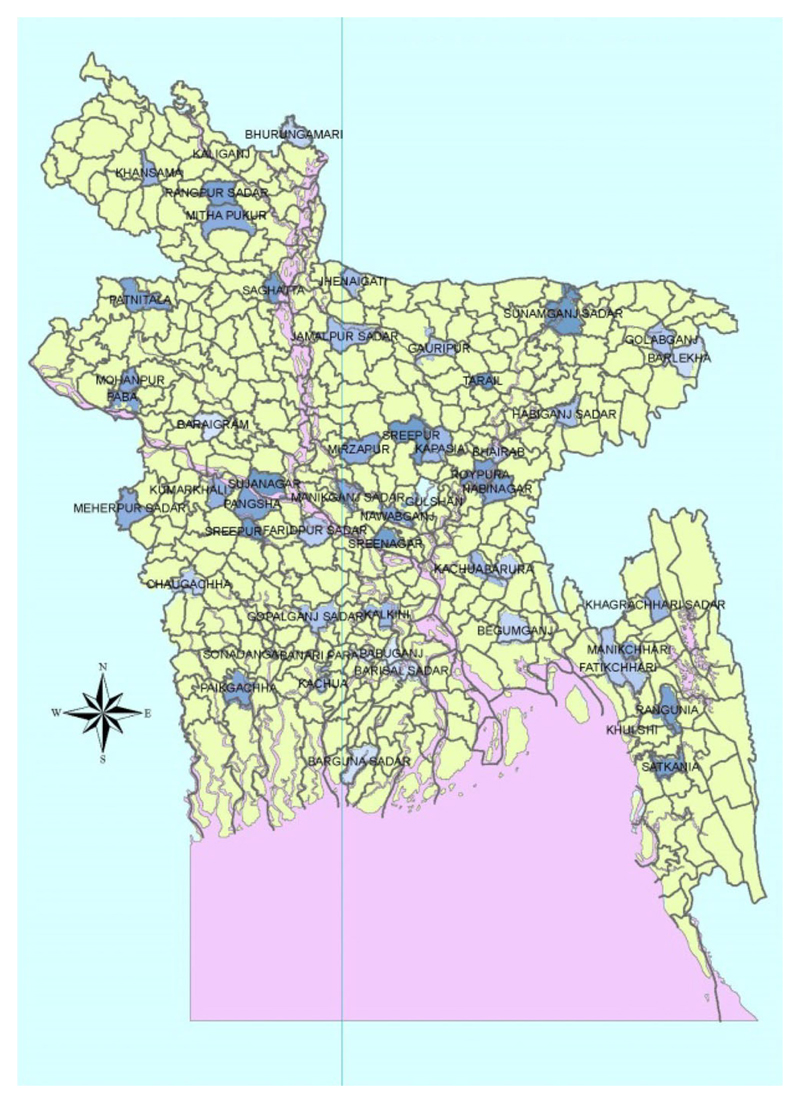
At the first stage, 52 primary sampling units (11 urban and 41 rural) were selected (locations are shown in Figure 1), with selection probability proportionate to size from all 7 divisions (including a 25 per cent proportion for urban areas), followed by a random selection of secondary sampling units from the map and list already available (updating was conducted with the help of local health assistants if necessary). Eighty households per mauza and 115 households per mahalla were then randomly selected. More households were selected from mahalla because of their higher population density. Finally, one person per secondary sampling unit was recruited randomly using a Kish table.
Fig. 1.
Map of Bangladesh showing the study locations (blue).
Every effort was made to limit non-response. If subjects were not at home at the time of the first visit, a second visit was made at a mutually agreed time. No third visit was made and no replacement of respondents was considered.
Sample size and response
Assuming a 7.9 per cent prevalence of hearing loss in Bangladesh,5 at 2 per cent precision for a 4 sub-group analysis (urban–rural and male–female), and with a design effect of 1.75 to adjust within-cluster population homogeneity, the calculated national sample size was 4891. Considering the individual response rate of 93.3 per cent reported in the recent Non-communicable Disease Risk Factor Survey, Bangladesh 2010,9 the sample size was inflated by 6.7 per cent to 5220.
Out of a targeted 5220 subjects from 52 primary sampling units, 4260 individuals (82 per cent in total; 68 per cent men and 95 per cent women) completed the full survey questionnaire and hearing tests.
Field team and its training
Each field team was headed by a research physician who had been undergoing residency training in otolaryngology for at least one year. The research physicians, audiologists and professional field enumerators underwent a 3-day extensive training course at Bangabandhu Sheikh Mujib Medical University on questionnaires, data collection, randomisation, interview technique and other relevant issues of field management. A dry run was then performed in the field to test the standard operating procedures. Experts from the WHO and the investigators conducted the training and field testing. Audiological methods were extensively demonstrated by expert otolaryngologists. All investigators (including divisional co-ordinators) were brought to the orientation for a uniform understanding of the procedures for field operations.
Survey instruments and data collection
The questionnaire had three sections, focusing on: (1) household and socio-demographic information; (2) hearing assessment; and (3) information with regard to basic ear assessment and risk factors of hearing impairment. The questionnaire was based on the protocol and standardised questionnaire prepared by the WHO.7 In order to determine the status of hearing, portable audiometers, tympanometers, otoacoustic emissions test equipment, otoscopes and tuning forks were used.
The socio-demographic questionnaire was administered by the field enumerators to selected individuals (if 15 years or older) or their parents (if the selected individuals were younger than 15 years). Information on 20 household assets was collected to determine the individuals’ economic status. After administering the socio-demographic questionnaire, each individual was asked to attend the clinical assessment camp established nearby.
Audiological equipment was calibrated in the Bangabandhu Sheikh Mujib Medical University audiology unit at the start of the survey. Daily calibrations were conducted by team members. Validations of the tests, both audiological and otoscopic, were performed by comparing a number of subjects with normal and abnormal hearing.
Field work
Two teams of data collectors were formed, with each team consisting of one research physician, one audiometrist, one field organiser and two enumerators. Each team used an assigned vehicle to carry survey equipment. Data were collected in a primary sampling unit for 2 to 3 days. Involvement of the local community was ensured through the local health authority.
On the first day, the field organiser visited as an advance party and started a household listing with the help of the local health assistant. The field organiser set up a camp for audiometric investigation in a preferred site with an electricity supply. The enumerators collected socio-demographic data from randomly selected households.
On the second and third days, random selection of one person out of the selected household was performed by one enumerator, while others carried out physical and clinical examinations on the referred cases in the camp set-up. Assessment of hearing in those aged less than five years was conducted via behavioural observation.
The field organiser moved to a new site on the second or third day as an advance party, and the others moved the following day. Each investigator had co-ordination and field supervision roles for their assigned divisions. They were the guarantors of the team in their respective divisions.
Quality control measures
Random selection of primary sampling units was carried out by one WHO staff member who was not an investigator. Eligible subjects from households were also selected randomly. Supervisors made regular checks on compliance to the standard operating procedures. In addition, a quality control team was vigilant at all times.
Data entry was performed by a professional data entry operator who had no knowledge of outcomes of interest. Concurrent data entry and interim analyses allowed the investigators to send messages to the field regarding improvements. Logical checks were carried out with the help of database software.
Ascertainment of hearing status
Before determining hearing status, necessary examinations were performed by the research physician to diagnose ear diseases. The most common disease was chronic suppurative otitis media (CSOM). This has been defined by the WHO as ‘Chronic inflammation of the middle ear and mastoid cavity, which presents with recurrent ear discharges or otorrhoea through a tympanic membrane perforation’.10 It included tubotympanic, atticoantral and dry perforation varieties. Chronic otitis media with effusion (OME) was considered to be a separate entity.
We used standard tests to determine hearing status. In neonates and infants from birth to six months, otoacoustic emissions (see below) testing was used. From 6 months to 18 months, a rattle was used to see whether the infant turned to the rattle source. Observation of infants’ behaviour, such as alerting, cessation of an activity, widening of eyes or facial grimacing, was used to determine their hearing status. This was done in addition to otoacoustic emissions testing for young children.
All examinations were performed carefully to avoid any pain or harm to the children. Details of the hearing test procedures and their interpretations is available elsewhere.11 We describe them briefly for readers’ convenience.
Tuning fork tests
These tests were carried out by vibration of tuning forks of 512 Hz frequency. The fork was sounded by striking the tines against the patella or elbow. Weber’s and Rinne’s tests were performed together as a ‘package’ to help identify the affected ear and type of hearing loss (conductive or sensorineural). The tuning fork test results were interpreted as follows: normal hearing = Rinne’s test result positive in both ears and Weber’s test central; hearing loss in one ear (conductive hearing loss) = Rinne’s test result negative in one ear and Weber’s test lateralised; hearing loss in both ears (conductive hearing loss) = Rinne’s test result negative in both ears and Weber’s test lateralised or central; sensorineural hearing loss = Rinne’s test result positive, but absolute bone conduction reduced.
Pure tone audiometry
This was carried out in participants aged five years or older. Pure tone audiometry was not performed in children aged zero to four years. Infants were assessed via otoacoustic emissions tests and behavioural observation. Differentiations in the degree of hearing loss in this age group were made for those children who could participate in a pure tone audiometry test. Children aged less than five years were classified as having normal hearing if they could: speak words; answer or point on command; move their head towards any sound; blink in response to a loud sound; or pass an otoacoustic emissions test. Those who failed otoacoustic emissions tests were labelled as having profound hearing loss.
Pure tone audiometry was first performed on the better hearing ear and repeated using bone conduction if necessary. The pure tone average was calculated from the 0.5, 1, 2 and 4 kHz values. The result showed the type and degree of hearing loss.
Tympanometry
This was used to diagnose middle-ear diseases and conditions, such as effusion, eustachian tube dysfunction and some types of sensorineural hearing loss, and involved measuring the compliance of the tympanic membrane (in response to the firing of a 225 Hz sound signal).
Otoacoustic emissions testing
This was used to screen hearing in neonates and in sensitive persons who showed poor co-operation with the procedures. It helped distinguish cochlear from retro-cochlear hearing loss. Otoacoustic emissions were absent in cochlear lesions.
Definition of hearing impairment
In line with the WHO classification, hearing impairment was defined according to the pure tone average in the better hearing ear.1 The hearing threshold level was calculated, using audiometry, as the better hearing ear average of four frequencies: 0.5, 1, 2 and 4 kHz.
Categories of hearing impairment were (1) no impairment (0–25 dB), (2) mild impairment (26–40 dB), (3) moderate impairment (41–60 dB), (4) severe impairment (61–80 dB) and (5) profound impairment (greater than 80 dB) according to the threshold levels. Disabling hearing impairment was defined as a permanent unaided hearing threshold level for the better hearing ear of 41 dB or greater (or greater than 30 dB in children younger than 15 years).
Ethical considerations
Ethical clearance was obtained from the Bangladesh Medical Research Council, the national body for such clearance. Community consent was obtained before the survey was conducted. Informed written consent was obtained from the participants or from the parents (in the case of children younger than 15 years).
All measures were taken to protect the confidentiality of data. A unique identification number was provided to each individual during household and socio-demographic data collection.
Arrangements were made for appropriate treatment or referral for survey subjects found to have diseases or hearing impairment. Measures were taken to avoid any physical or mental injury, and social or economic problems of any form.
Data management and analyses
After data collection for a few primary sampling units was complete, the aggregated data from the interviewers were sent to the project office through their divisional supervisors. The data manager aggregated the data weekly and gave feedback to the field teams if necessary. A coding instruction was used for data entry. The SPSS® statistical software program (version 17 for Windows) was used for data entry, cleaning and analysis.
The study produced estimates of ear diseases and hearing impairment prevalence for: six age groups (0–4 years, 5–14 years, 15–29 years, 30–44 years, 45–59 years, and 60 years or older), both sexes and two location types (rural or urban residences). Subjects were categorised by degree (mild, moderate, severe or profound) and nature (conductive, sensorineural or mixed) of hearing loss, as per WHO definitions.1 An additional category of disabling hearing loss was constructed as per the definition given above. Measures of uncertainty of prevalence estimates were given by 95 per cent confidence intervals for major findings.
A wealth index was constructed based on principal components analysis of information on ownership of 20 household items. Each asset was assigned a weight (factor score), and the resulting asset scores were standardised in relation to a normal distribution with a mean of 0 and standard deviation of 1. Each household was then assigned a score for each asset, and the scores were summed for each household; individuals were ranked according to the total score of their household. The sample was then divided into quartiles, with the first being the poorest and the fourth being the richest.
Finally, a multiple logistic regression analysis using a backward elimination approach was performed to determine the significant factors associated with disabling hearing loss. All variables (age, sex, residence, family history of hearing loss, history of consanguinity, wealth quartile, ear wax, CSOM, OME, acute suppurative otitis media, otitis externa and presence of a foreign body) were entered in the model, but only those with a p-value of 0.1 or less were retained in the model.
Results
We present here the prevalence of ear diseases and hearing impairment from a nationally representative sample of 4260 subjects. They represent the Bangladeshi population in terms of age structure, education and urban–rural areas of residence. Because most of the adult men were away from home for their livelihood, their representation was relatively low (42 per cent against a targeted 50 per cent) in this sample.
Respondent socio-demographics
The median age of our subjects was 30 years (interquartile range, 14–46 years). The median ages of males and females were 27 and 30 years, respectively. There were 27 infants in our sample, with an average age of 7 months. The sample had completed a median of four years of schooling (for those aged seven years or older, as Bangladeshi children enrol into primary schools at five or six years of age). One-quarter (25 per cent) of the respondents were from urban areas.
Table I describes the age and sex distribution of the respondents. They were categorised into six age groups (0–4 years, 5–14 years, 15–29 years, 30–44 years, 45–59 years, and 60 years or older) for our analyses. The proportion of female respondents was slightly higher in all groups, apart from the youngest and oldest groups. Among men, farmers (27.6 per cent) and students (29.2 per cent) were predominant, whereas home-makers (62.8 per cent) and students (21.5 per cent) were predominant among women (Table II).
Table I. Age and Sex Distribution of Respondents.
| Age group (years) | Males* | Female† | Both sexes‡ |
|---|---|---|---|
| 0–4 | 150 (8.5) | 120 (4.8) | 270 (6.3) |
| 5–14 | 434 (24.5) | 465 (18.7) | 899 (21.1) |
| 15–29 | 350 (19.7) | 596 (24.0) | 946 (22.2) |
| 30–44 | 319 (18.0) | 616 (24.8) | 935 (21.9) |
| 45–59 | 288 (16.2) | 451 (18.1) | 739 (17.3) |
| 60 + | 233 (13.1) | 238 (9.6) | 471 (11.1) |
Data represent numbers (and percentages) of respondents.
n=1774;
n = 2486;
n = 4260
Table II. Occupation of Respondents* .
| Age group (years) | No occupation | Student | Agriculture | Business | Industrial worker | Other service | Homemaker | Other |
|---|---|---|---|---|---|---|---|---|
| Males | ||||||||
| – 7–14 | 15 (4.2) | 330 (92.7) | 3 (0.8) | 3 (0.8) | 2 (0.6) | 1 (0.3) | – | 2 (0.6) |
| – 15–29 | 25 (7.4) | 119 (34.0) | 76 (21.7) | 48 (13.7) | 33 (9.4) | 31 (8.9) | – | 16 (4.6) |
| – 30–44 | 5 (1.6) | 3 (0.9) | 116 (36.4) | 83 (26.0) | 47 (14.7) | 47 (14.7) | – | 20 (6.3) |
| – 45–59 | 8 (2.8) | – | 137 (47.6) | 66 (22.9) | 36 (12.5) | 22 (7.6) | – | 17 (5.9) |
| – 60 + | 98 (42.1) | – | 94 (40.3) | 17 (7.3) | 9 (3.9) | 8 (3.4) | – | 7 (3.0) |
| – Total | 151 (9.8) | 452 (29.2) | 426 (27.6) | 217 (14.0) | 127 (8.2) | 109 (7.2) | – | 62 (4.0) |
| Females | ||||||||
| – 7–14 | 11 (2.9) | 369 (96.6) | 1 (0.3) | 1 (0.3) | – | – | – | – |
| – 15–29 | 50 (8.4) | 112 (18.8) | 4 (0.7) | 8 (1.3) | 15 (2.5) | 33 (5.5) | 370 (62.0) | 5 (0.8) |
| – 30–44 | 18 (2.9) | 10 (1.6) | 5 (0.8) | 11 (1.8) | 17 (2.8) | 34 (5.5) | 521 (84.6) | 3 (0.5) |
| – 45–59 | 18 (4.0) | – | 5 (1.1) | 5 (1.1) | 8 (1.8) | 14 (3.1) | 396 (87.8) | 3 (0.7) |
| – 60 + | 76 (31.9) | – | 2 (0.8) | 2 (0.8) | – | 7 (2.9) | 147 (61.8) | 3 (1.3) |
| – Total | 173 (7.5) | 491 (21.5) | 17 (0.7) | 27 (1.2) | 40 (1.8) | 88 (3.9) | 1434 (62.8) | 14 (0.6) |
| Both sexes | ||||||||
| – 7–14 | 26 (3.5) | 699 (94.7) | 4 (0.5) | 4 (0.5) | 2 (0.3) | 1 (0.1) | – | 2 (0.3) |
| – 15–29 | 75 (7.9) | 231 (24.4) | 80 (8.5) | 56 (5.9) | 48 (5.1) | 64 (7.0) | 370 (39.0) | 21 (2.2) |
| – 30–44 | 23 (2.5) | 8 (0.9) | 121 (12.9) | 94 (10.1) | 64 (6.8) | 81 (8.7) | 521 (55.7) | 23 (2.5) |
| – 45–59 | 26 (3.5) | 4 (0.5) | 142 (19.2) | 71 (9.6) | 44 (6.0) | 36 (4.9) | 396 (53.6) | 20 (2.7) |
| – 60 + | 174 (36.9) | 1 (0.2) | 96 (20.4) | 19 (4.0) | 9 (1.9) | 15 (3.2) | 147 (31.2) | 10 (2.1) |
| – Total | 324 (8.4) | 943 (24.6) | 443 (11.6) | 244 (6.4) | 167 (4.4) | 197 (5.1) | 1434 (37.5) | 76 (2.0) |
Data represent numbers (and percentages) of respondents.
n = 3828 (432 respondents aged less than 7 years were excluded from the analysis)
Ear diseases or conditions
On physical examination, 13.3 per cent of the sample population had some sort of ear disease: 6.2 per cent had CSOM (tubotympanic in 3.6 per cent, atticoantral in 0.6 per cent and dry perforation variety in 2.0 per cent), 5.3 per cent had otitis media with effusion (OME), 1.7 per cent had otitis externa and 0.1 per cent had acute suppurative otitis media. Additionally, 11.5 per cent had impacted wax and 0.3 per cent had foreign bodies in their ears (Table III). In total, one-quarter (25 per cent) of the subjects had some sort of physical ear problem at this stage of the assessment.
Table III. Condition of Ears Based on History and Physical Examination*.
| Age group (years) | Normal† | Wax | Foreign body | Otitis externa | OME | ASOM | CSOM |
|---|---|---|---|---|---|---|---|
| 0–4 | 171 (63.3) | 86 (31.9) | – | 5 (1.9) | 3 (1.1) | – | 5 (1.9) |
| 5–14 | 603 (67.1) | 197 (21.9) | 3 (0.3) | 15 (1.7) | 29 (3.2) | 1 (0.1) | 51 (5.7) |
| 15–29 | 814 (86.1) | 59 (6.2) | 1 (0.1) | 5 (0.5) | 29 (3.1) | 2 (0.2) | 36 (3.8) |
| 30–44 | 747 (79.9) | 42 (4.5) | 3 (0.3) | 15 (1.6) | 52 (5.6) | 2 (0.2) | 74 (7.9) |
| 45–59 | 555 (75.1) | 49 (6.6) | 1 (0.1) | 18 (2.4) | 52 (7.0) | – | 64 (8.7) |
| 60 + | 304 (64.5) | 56 (11.9) | 3 (0.6) | 13 (2.8) | 61 (13.0) | – | 34 (7.2) |
| Total | 3194 (75.0) | 489 (11.5) | 11 (0.3) | 71 (1.7) | 226 (5.3) | 5 (0.1) | 264 (6.2) |
Data represent numbers (and percentages) of respondents.
Number of respondents = 4260.
No visible ear disease, but 228 respondents were subsequently identified as having hearing loss. OME = otitis media with effusion; ASOM = acute suppurative otitis media; CSOM = chronic suppurative otitis media
Type of hearing loss
In the next step, tuning fork tests were performed on 3990 respondents. Based on history, observation, clinical examination and tuning fork test results, 11.7 per cent of respondents were found to have hearing loss in both ears, while 8.1 per cent had hearing loss in one ear. There was a gradual increase in hearing loss with age, with a sharp increase in those aged over 60 years (Table IV). Eighty per cent of subjects were found to have normal hearing at this stage.
Table IV. Status of Hearing Based on Clinical Assessment*.
| Age group (years) | Normal hearing | Hearing loss in 1 ear | Hearing loss in both ears |
|---|---|---|---|
| 0–4 | 235 (87.0) | 12 (4.4) | 23 (8.5) |
| 5–14 | 781 (86.9) | 61 (6.8) | 57 (6.3) |
| 15–29 | 856 (90.5) | 54 (5.7) | 36 (3.8) |
| 30–44 | 776 (83.0) | 88 (9.4) | 71 (7.6) |
| 45–59 | 552 (74.7) | 73 (9.9) | 114 (15.4) |
| 60 + | 217 (46.1) | 57 (12.1) | 197 (41.8) |
| Total | 3417 (80.2) | 345 (8.1) | 498 (11.7) |
Data represent numbers (and percentages) of respondents. Status of hearing was clinically assessed via patient history, behavioural observation (in the case of children aged less than five years) and tuning fork tests. These tests were used to differentiate between conductive or sensorineural hearing losses (see Materials and methods section for details).
n = 4260
Prevalence in terms of the nature of the hearing loss (conductive or sensorineural type) was also calculated. Conductive, sensorineural and mixed hearing losses affected 12, 4.5 and 3.8 per cent of respondents, respectively (Table V). Sensorineural and mixed types of hearing losses were increasingly prevalent with age.
Table V. Type of Hearing Loss Based on Clinical Assessment*.
| Variable | Conductive loss | Mixed loss | Sensorineural loss | Normal hearing | Total |
|---|---|---|---|---|---|
| Age group (years) | |||||
| – 5–14 | 102 (11.3) | 10 (1.1) | 7 (0.8) | 780 (86.8) | 899 (100.0) |
| – 15–29 | 74 (7.8) | 9 (1.0) | 8 (0.8) | 855 (90.4) | 946 (100.0) |
| – 30–44 | 128 (13.7) | 18 (1.9) | 13 (1.4) | 776 (83.0) | 935 (100.0) |
| – 45–59 | 112 (15.2) | 36 (4.9) | 38 (5.1) | 553 (74.8) | 739 (100.0) |
| – 60 + | 62 (13.2) | 79 (16.8) | 112 (23.8) | 218 (46.3) | 471 (100.0) |
| Residence | |||||
| – Urban | 92 (9.4) | 24 (2.4) | 21 (2.1) | 844 (86.0) | 981 (100.0) |
| – Rural | 386 (12.8) | 128 (4.3) | 157 (5.2) | 2338 (78.0) | 3009 (100.0) |
| Total | 478 (12.0) | 152 (3.8) | 178 (4.5) | 3182 (79.7) | 3990 (100.0) |
Data represent numbers (and percentages) of respondents. Type of hearing loss was clinically assessed via patient history, clinical examination and tuning fork tests.
n = 3990 (270 respondents from the 0–4 year age group were assessed separately as the nature of hearing loss could not be assessed clinically in this age group)
Degree of hearing loss
Finally, pure tone audiometry and otoacoustic emission tests were carried out. Hearing losses were categorised according to the WHO guidelines based on the findings for the better hearing ear.1 Age- and sex-specific results are given in Table VI.
Table VI. Degree of Hearing Loss*.
| Variable | No loss (0–25 dB) |
Mild loss (26–40 dB) |
Moderate loss (41–60 dB) |
Severe loss (61–80 dB) |
Profound loss or deafness (≥81 dB) |
Any hearing loss (26+ dB) |
|---|---|---|---|---|---|---|
| Age group (years) | ||||||
| – 0–4 | 233 (86.3) | 22 (8.1) | – | – | 15 (5.6) | 37 (13.7) |
| – 5–14 | 721 (80.2) | 168 (18.7) | 4 (0.4) | 2 (0.2) | 4 (0.4) | 178 (19.8) |
| – 15–29 | 762 (80.5) | 157 (16.6) | 23 (2.4) | 2 (0.2) | 2 (0.2) | 184 (19.5) |
| – 30–44 | 621 (66.4) | 265 (28.3) | 40 (4.3) | 5 (0.5) | 4 (0.4) | 314 (33.6) |
| – 45–59 | 355 (48.0) | 296 (40.1) | 68 (9.2) | 13 (1.8) | 7 (0.9) | 384 (52.0) |
| – 60+ | 96 (20.4) | 204 (43.3) | 123 (26.1) | 31 (6.6) | 17 (3.6) | 375 (79.6) |
| Residence | ||||||
| – Urban | 863 (81.1) | 145 (13.6) | 38 (3.6) | 10 (0.9) | 8 (0.8) | 201 (18.9) |
| – Rural | 1925 (60.2) | 967 (30.3) | 220 (6.9) | 43 (1.3) | 41 (1.3) | 1271 (39.8) |
| Total | 2788 (65.4) | 1112 (26.1) | 258 (6.1) | 53 (1.2) | 49 (1.2) | 1472 (34.6) |
Data represent numbers (and percentages) of respondents.
Based on pure tone audiometry and otoacoustic emissions testing (n = 4260)
The ability to hear sounds of 25 dB or less was considered to be normal. Slightly more than one-third (34.6 per cent) of respondents had some degree of hearing loss. Among them, 26.1 per cent had mild hearing loss (26–40 dB: able to hear and repeat words spoken in a normal voice at 1 metre), 6.1 per cent had moderate hearing loss (41–60 dB: able to hear and repeat words spoken using a raised voice at 1 metre), 1.2 per cent had severe hearing loss (61–80 dB: able to hear some words when these were shouted into the better hearing ear) and 1.2 per cent had profound hearing loss (greater than 80 dB: unable to hear and understand shouted words, otherwise known as deaf).
Strikingly, there was no moderate or severe hearing loss in the zero to four years age group, which is probably a result of the small sample size in this sub-group. Generally speaking, the degree of hearing loss showed an increasing trend with age. However, profound hearing loss was more prevalent in the youngest age group (zero to four years). Hearing loss was almost double in rural areas (39.8 per cent) compared with urban areas (18.9 per cent). We did not observe any sex difference in hearing loss (data not shown).
Disabling hearing loss
According to the WHO, disabling hearing loss is defined as a more than 40 dB loss in those aged 15 years or older, but a more than 30 dB loss in younger people. Table VII describes the prevalence of disabling hearing loss according to age groups and urban–rural residence. The prevalence of disabling hearing loss in the 0–14 year age group was 6.0 per cent.
Table VII. Prevalence of Disabling Hearing Loss*.
| Variable | Males | Females | Both sexes |
|---|---|---|---|
| Age groups (years) | |||
| – 0–4 (≥31 dB hearing loss) | 11 (7.3) | 4 (3.3) | 15 (5.6) |
| – 5–14 (≥31 dB hearing loss) | 27 (6.2) | 28 (6.0) | 55 (6.1) |
| – 15–29 (≥41 dB hearing loss) | 11 (3.1) | 16 (2.7) | 27 (2.9) |
| – 30–44 (≥41 dB hearing loss) | 12 (3.8) | 38 (6.2) | 50 (5.3) |
| – 45–59 (≥41 dB hearing loss) | 31 (10.8) | 57 (12.6) | 88 (11.9) |
| – 60+ (≥41 dB hearing loss) | 77 (33.0) | 95 (39.9) | 172 (36.5) |
| Residence | |||
| – Urban | 25 (5.6) | 38 (6.1) | 63 (5.9) |
| – Rural | 144 (10.8) | 200 (10.7) | 344 (10.8) |
| Total | 169 (9.5) | 238 (9.6) | 407 (9.6) |
Data represent numbers (and percentages) of respondents.
n = 4260
Overall, 9.6 per cent (95 per cent confidence interval, 8.5–10.8 per cent) of our sample population had disabling hearing loss. There was no apparent difference in prevalence between men and women. However, disabling hearing loss showed a clear increasing trend with age. This increase was very sharp for those aged over 60 years.
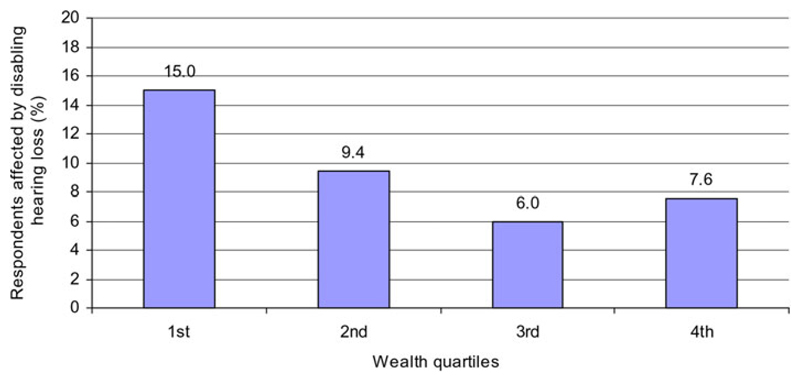
The relationship of disabling hearing loss with socio-economic status as determined by wealth quartiles was examined. There was a clear gradient of poverty linked with disabling hearing loss: disabling hearing loss affected 15.0 per cent in the first quartile compared with only 7.6 per cent in the fourth quartile (Figure 2).
Fig. 2.
Prevalence of disabling hearing loss according to wealth quartiles (with the first being the poorest and the fourth being the richest). Wealth indices constructed using principal components analysis based on ownership of 20 household items (see Materials and methods).
Finally, a multiple logistic regression analysis using a stepwise backward elimination approach was performed to determine the significant factors associated with disabling hearing loss. All variables (age, sex, residence, family history of hearing loss, history of consanguinity, wealth quartile, ear wax, CSOM, OME, acute suppurative otitis media, otitis externa and presence of foreign bodies) were initially entered in the model, but only those with a p-value of 0.1 or less were retained. Thus, the final model included age, family history of hearing loss, wealth quartile, ear wax, CSOM, OME and otitis externa. The results are shown in Table VIII. Although residence location (rural–urban) was a significant variable in the initial analysis, its significance disappeared in the multivariate analysis, probably because of the interaction with wealth indices.
Table VIII. Multiple logistic Regression Analysis Findings*.
| Variable | Beta coefficient | Standard error | p | Odds ratio |
|---|---|---|---|---|
| Age (years) | 0.05 | 0.00 | 0.00 | 1.1 |
| Family history of hearing loss (no = 0, yes = 1) | 0.35 | 0.18 | 0.05 | 1.4 |
| Wealth quartiles (poorest = 1 through richest = 4) | –0.26 | 0.05 | 0.00 | 0.8 |
| Impacted wax (no = 0, yes = 1) | 0.98 | 0.18 | 0.00 | 2.7 |
| CSOM (no = 0, yes = 1) | 2.08 | 0.17 | 0.00 | 8.0 |
| OME (no = 0, yes = 1) | 1.54 | 0.18 | 0.00 | 4.7 |
| Otitis externa (no = 0, yes = 1) | 1.08 | 0.34 | 0.00 | 2.9 |
Analysis conducted to determine the significant independent variables for disabling hearing loss. CSOM = chronic suppurative otitis media; OME = otitis media with effusion
Discussion
This is the first national level survey conducted using standard WHO methods to describe the prevalence of hearing impairments in Bangladesh. This study reports that, in general, one-quarter of the Bangladeshi population suffer from some sort of ear problem with or without hearing impairment. One-third of the Bangladeshi people suffered from some sort of hearing impairment. One in 10 of them suffered from disabling hearing impairment. We did not observe any sex difference, but age (especially age over 60 years) was an important predictor. Presbyacusis could be an important age-related issue that needs elucidation. Poverty had a clear link with disabling hearing loss; however, it could be perceived as a cause or an effect.
The only previous study in Bangladesh was carried out over one decade ago (2002).5 That study reported a slightly lower rate of disabling hearing loss (7.9 per cent, vs 9.6 per cent in the current study). However, the magnitude of ‘any hearing loss’ was almost the same (34.2 per cent, vs 34.6 per cent in the current study). From these two studies, it appears that the prevalence of hearing loss has remained fairly static over the last decade. Other than this, we do not have any other data from Bangladesh to make reasonable comparisons.
Our prevalence rates for disabling hearing loss are higher than those reported for Indian (6 per cent), Indonesian (4.2 per cent) and Maldivian (6 per cent) populations, but similar to Myanmar (8 per cent) and Sri Lankan populations.12 However, the prevalence rates reported for populations in Nepal (16.6 per cent) and Thailand (13.3 per cent) were substantially higher than ours.12 These differences should be cautiously interpreted because definitions are not necessarily the same. Most strikingly, we report here an almost 2.5 times higher prevalence (6 per cent) of disabling hearing loss in children younger than 15 years (Table VII) compared with a pooled estimate (2.4 per cent) given by the WHO for the South East Asia Region.1 From this, it can be concluded that a better child care system is required in Bangladesh, with special attention to ear care.
Bangladesh is a country with a population of 142 million, as per the 2011 census.8 Absolute numbers of people suffering from ear diseases or hearing impairments are given in Table IX. In terms of numbers, this gives us a frightening figure of the huge suffering of humanity here. Millions of people in Bangladesh need medical and surgical intervention, including cochlear implantations.
Table IX. Absolute Number of People in Bangladesh Suffering from Ear Diseases or Hearing Loss*.
| Disease or condition (prevalence) | Absolute number in millions |
|---|---|
| Chronic suppurative otitis media (6.2%) | 8.8 |
| Otitis media with effusion (5.3%) | 7.5 |
| Impacted wax (11.5%) | 16.4 |
| Any hearing loss (34.6%) | 49.2 |
| Disabling hearing loss (9.6%) | 13.7 |
| Profound hearing loss, i.e. deafness (1.2%) | 1.7 |
| Conductive hearing loss (12.0%) | 17.1 |
| Mixed hearing loss (3.8%) | 5.4 |
| Sensorineural hearing loss (4.5%) | 6.4 |
Total n = 142 million
Those who suffer from sensorineural and mixed hearing loss will need hearing aids for their rehabilitation (with the number of people who need hearing aids estimated at 11.8 million). Affected children aged zero to four years may need cochlear implants. Deaf and hearing-impaired children often experience delayed development of speech, language and cognitive skills, which may result in slow learning and other difficulties in school. Early detection and management of hearing impairments are essential for deaf or hearing-impaired babies to prevent permanent disability.
Age-related hearing loss is another burden on society. Similar to other populations,12 more than one-third of elderly people have disabling hearing loss in Bangladesh. These people may suffer from poor or even absent communication with other people, leading to social exclusion, loneliness and frustration. Society has a moral obligation to prevent this. This is especially important because of the poverty link in Bangladesh.
In addition to age and socio-economic status, multiple logistic regression analysis showed that impacted ear wax, CSOM, otitis media with effusion (OME) and otitis externa are independent predictors of disabling hearing loss. Millions of people with OME may develop perforation of the ear drum if no treatment is given, predisposing them to life-threatening complications, such as meningitis and brain abscesses. Otitis media is largely preventable, and can be effectively managed through medical and surgical approaches. Incorporating basic ear care into the primary healthcare system, and addressing equity, can provide a cost-effective and realistic solution.
Our study had some limitations. The environment in the camps where audiometry was conducted was not soundproof. Soundproofing is actually unrealistic in such a large-scale study in the field situation. Every effort was made to keep the room quiet and proper calibration of the equipment was carried out. Furthermore, otoacoustic emission tests were difficult to perform in infants who were awake. A separate schedule was provided to allow the infants to be calm and quiet when tested. In addition, the research physicians were extensively trained, but the employment of postgraduate specialists could add value to end point ascertainment. Lastly, this survey could not capture the possible roles of chronic noise exposure, ototoxic drugs and diabetes mellitus.
In conclusion, deafness prevention activities should primarily be focused on three areas in children: impacted ear wax, CSOM and OME, as these are the common problems. Intervention for deafness prevention should also focus on sensorineural hearing loss; hearing aids should be made available and accessible to everyone, especially to elderly people. Given that the problem is very common, deafness prevention should be integrated into the primary healthcare system, addressing the equity issue.
Nationally representative prevalence data on hearing impairment were not previously available in Bangladesh
This study reports a 9.6 per cent prevalence of disabling hearing impairment in Bangladeshi people of all ages
Chronic otitis media, otitis media with effusion, and impacted wax are important predictors of hearing loss
Hearing loss is more prevalent in socio-economically deprived people and in those older than 60 years
A primary care approach that addresses the equity issue should be used to control hearing impairment in Bangladesh
Acknowledgements
We are indebted to Dr Thushara Fernando of WHO Bangladesh for his guidance and support. Seven divisional co-ordinators of the study are acknowledged: Professor Zahedul Alam (Dhaka), Dr Abrar Ahmed (Barisal), Dr SK Ballav (Khulna), Dr Saber Ali (Rajshahi), Dr Md Harunur Rashid (Sylhet), Dr Md Ahsanul Habib (Rangpur) and Dr Mahabubul Alam Chowdhury (Chittagong). Dr AKM Jafar Ullah collaborated from the Directorate General of Health Services during this study. Comments from Drs Sudhangs Malhotra and Shelly Chadha of the WHO on a previous version of the manuscript were valuable when revising the manuscript, but this does not necessarily indicate their concurrence with the contents of the current version. The WHO Bangladesh Country Office provided the necessary funds and technical support for designing, implementing and reporting this study. However, the WHO does not have any influence on the findings and conclusions of the study. The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions or policies of the institutions with which they are affiliated.
Footnotes
Dr M M Zaman takes responsibility for the integrity of the content of the paper
Competing interests: None declared
References
- 1.WHO global estimates on prevalence of hearing loss. [21 February 2014]; http://www.who.int/pbd/deafness/WHO_GE_HL.pdf.
- 2.The Department for International Development. Disability, Poverty and Development. London: DFID; 2000. [Google Scholar]
- 3.Directorate General of Health Services, Ministry of Health Family Welfare, Government of Bangladesh. National Strategy on Prevention of Deafness and Hearing Impairment in Bangladesh: 2011–2016. Dhaka: Non Communicable Diseases Unit, Directorate General of Health Services; 2011. [Google Scholar]
- 4.World Health Organization. Strategies for prevention of deafness and hearing impairment. [21 February 2014]; http://www.who.int/pbd/deafness/activities/strategies/en/
- 5.Amin MN. Prevalence of hearing loss in Bangladesh [Report submitted to WHO Country Office for Bangladesh] Dhaka: 2002. Dec, [Google Scholar]
- 6.Garg S, Chadha S, Malhotra S, Agarwal AK. Deafness: burden, prevention and control in India. Natl Med J India. 2009;22:79–81. [PubMed] [Google Scholar]
- 7.World Health Organization. WHO Ear and Hearing Disorders Survey Protocol. Geneva: WHO; 1999. [Google Scholar]
- 8.Bangladesh Bureau of Statistics. Population and Housing Census 2011, Preliminary Result. Dhaka: Bangladesh Bureau of Statistics; 2011. [Google Scholar]
- 9.World Health Organization. Non-communicable Disease Risk Factor Survey, Bangladesh 2010. Dhaka: WHO; 2011. [Google Scholar]
- 10.World Health Organization. Chronic Suppurative Otitis Media: Burden of Illness and Management Options. Vol. 9 Geneva: WHO; 2004. [Google Scholar]
- 11.World Health Organization. Hearing measurement. [4 August 2013]; www.who. int/occupational_health/publications/noise8.pdf.
- 12.World Health Organization. Situation Review and Update on Deafness, Hearing Loss and Invention Programmes. New Delhi: WHO SEARO; 2007. [Google Scholar]