Abstract
Although patterns of African American and white women breast cancer incidence and mortality in St. Louis, Missouri is consistent with those seen elsewhere in the United States, rates vary greatly across zip codes within the city of St. Louis. North St. Louis, whose neighborhoods are primarily African American, exhibits rates of breast cancer mortality that are among the highest in the city and the state as a whole. Based on information that up to 50% of women in North St. Louis with a suspicious diagnosis of breast cancer never enter treatment, we conducted three 2-hour group model building sessions with 34 community stakeholders (e.g., breast cancer survivors or family members or caregivers and community support members such as navigators) to identify the reasons why African American women do not begin or delay breast cancer treatment. Participant sessions produced a very rich and dynamic causal loop diagram of the system producing disparities in breast cancer mortality in St. Louis. The diagram includes 8 major subsystems, causal links between system factors, and feedback loops, all of which shed light on treatment delays/initiation. Our work suggests that numerous intersecting factors contribute to not seeking treatment, which in turn may contribute to African American and white disparities in mortality.
Keywords: Breast Cancer Disparities, Treatment Initiation/Delay, Community-Based System Dynamics, Group Model Building, Community-Engaged Research, African American Women
INTRODUCTION
Breast cancer remains the most commonly diagnosed cancer among women in the United States as well as the second leading cause of cancer death among women after lung cancer (Siegel, Miller, & Jemal, 2017). African American women in the United States experienced lower incidence rates of breast cancer than white women until 2012 when the two rates converged (DeSantis, Fedewa, et al., 2016). Yet, although mortality from cancer has decreased in recent years, it remains the case that African American women are 43% more likely than white women to die from the disease (Hunt, Whitman, & Hurlbert, 2014).
African American and white women differ in the type of breast cancer they most commonly exhibit, which may affect outcomes (DeSantis, Fedewa, et al., 2016). African American women are more likely to be diagnosed with the earlier-onset, basal form of breast cancer, which is significant in terms of mortality because it is more lethal and aggressive than later-onset forms. This may help to explain why the median age of diagnosis for African American women was 58 years, while it was 62 years for white women. African American women’s overrepresentation of earlier-onset basal is thought to contribute to their younger age at diagnosis (DeSantis, Siegel, et al., 2016).
In St. Louis, Missouri, rates of breast cancer incidence and mortality are similar to nationwide trends. However, mortality is higher within the predominantly African American zip codes of North St. Louis. For instance, the breast cancer mortality rate of African American women in St. Louis City was 25.7 per 100,000 between 2009 and 2013, while the rate was 22.8 per 100,000 for the state as a whole (State Cancer Profiles, 2017). It also is the case that the predominantly African American residents of North St. Louis experience the worst social and health indicators (e.g., median family income, employment, life expectancy at birth, asthma, and allergy) in the St. Louis area (Saint Louis Regional Health Commission, 2012).
A white paper released in 2014 by the St. Louis affiliate of Susan G. Komen for the Cure and Washington University noted that over 50% of African American women diagnosed with breast cancer in St. Louis never start treatment (St. Louis Susan G. Komen Project, 2014). Other women may have begun treatment but after a delay. Although the underlying causes for the observable disparities in African American and white women breast cancer mortality outcomes are complex and not well understood, some authors have attributed it to treatment delay (Copson et al., 2014; McGee, Durham, Tse, & Millikan, 2013). Treatment delay is defined as time intervals between the date of diagnosis and initiation of first treatment/therapy. McGee et al., (2013) in the Carolina Breast Cancer Study examined determinants of treatment delay for African American and white women. They reported that although 94% of women meet their target of initiating treatment within 60 days of diagnosis, racial disparities persisted (McGee et al., 2013). Results further showed that African American women were more than twice as likely as white women to lose a job due to their diagnosis (6.6% vs. 2.7%), and less likely to undergo immediate reconstruction (25.2% vs. 37.9%). The delay for African American women exceeded the frequency for white women by more than 30% for the following categories: detection by a method other than a routine mammogram, clinical breast examination, or self or spouse-detection (70.0% for African American women vs. 33.3% for white women). Factors affecting delays include no insurance coverage (48.9% for African American women vs. 15.3% for white women), and households of 4 people (large family size) (53.5% for African American women vs. 23.2% for white women) (McGee et al., 2013).
Copson and colleagues (Copson et al., 2014) examined ethnicity and breast cancer outcomes among young breast cancer patients in the United Kingdom. These authors found that despite equal access to health care from the National Health Service, young African American women in the United Kingdom experienced highly significant poorer breast cancer outcome than white women (Copson et al., 2014). Factors affecting survival and recurrence include total tumor diameter, grade, nodal status and patient body mass index (BMI) (Copson et al., 2014). To shed light on factors producing racial/ethnic cancer disparities and ways to effectively reduce them, (Warnecke et al., 2008) developed a multi-level model of the determinants of cancer disparities and the interactions between them. The framework identified 3 primary levels of determinants including distal, intermediate and proximal (Gehlert & Colditz, 2011; Warnecke et al., 2008). We used this framework to help ensure that we considered a broad enough picture of the factors that influence disparities in breast cancer mortality.
Authors have implicated race/ethnicity as an issue in women’s decisions to seek additional diagnostic testing after a suspicious diagnosis of breast cancer and to adhere to treatment recommendations (Corner, Hopkinson, & Roffe, 2006; Iqbal, Ginsburg, Rochon, Sun, & Narod, 2015; Reeder-Hayes, Wheeler, & Mayer, 2015). In attempting to understand treatment delay or the failure to even begin treatment, the present study was conducted to examine the factors that may have contributed to the treatment delay of women with suspicious mammograms. We view treatment delay as a significant link between distal factors such as health policies at the local, state, and national level and more proximal factors like race and biology as they affect significant issues such as the onset of breast cancer (Warnecke et al., 2008).
METHODS
To help understand the dynamic complexity underlying the widening breast cancer disparities between African American women and white women in St. Louis, we used group model building (GMB) to develop a causal map of the social determinants influencing treatment delays. Specifically, we used community-based system dynamics (Hovmand, 2014), a community-based participatory research method for engaging communities in system dynamics. This approach has been used previously to understand various other behaviors affecting public health and recommended by the Institute of Medicine as a prevention community-based strategy (Pronk, 2013).
Formation of Core Modeling Team and Study Population
A five-member core modeling team (CMT) or “design team” comprised of faculty and staff from Washington University School of Medicine, Brown School Social System Design Lab and St. Louis City Department of Health affiliates were responsible for planning and facilitating the GMB workshops as well as recruited eligible women for the study.
Potential participants were identified from a larger sample of 432 African American breast cancer survivors diagnosed between 2000 and 2008, living in 8 zip codes (63106, 63107, 63112, 63113, 63115, 63120, and 63147) in North St. Louis, and an independent St. Louis County Zip code (63136) that was provided by the Missouri Cancer Registry. This cluster of 8 zip codes was chosen based on its high rates of late stage of breast cancer diagnosis. Breast cancer survivors, their family members, or caregivers’ women were recruited through specially designed flyers that were distributed in community clinics, laundromats, currency exchanges, shelters, buses, and churches in North St. Louis. Eligibility criteria for the current study were: (1) breast cancer survivor living in North St. Louis and self-identifying as African American, or (2) breast cancer survivor’s family member or (3) breast cancer survivor’s caregiver women, and (3) health care workers or volunteers working with this population (navigators, research coordinators, city workers and volunteers working with communities on women’s health issues). For the health care workers, we mailed invitation letter to navigators, research coordinators, city workers, volunteers, providers from federally qualified health center (FQHC), who participate in the quarterly St. Louis Regional Breast Cancer Workgroup. Potential women who responded were invited to participate in the group model building (GMB) workshop if they met the eligibility criteria established. Only women were included in the group, because we were seeking a female perspective and including males may have inhibited responses or affected them in some other way.
The final sample size was 34 women who participated in the workshop series, representing the two stakeholder groups (Table 1). Communication among group members/stakeholders is key to managing a successful GMB project/outcome. It is recommended that the group is large enough to represent diversity in the target area, but also small for sufficient interaction and discussion. Hence, GMB does not require the usual calculations of sample size. (Andersen, Richardson, & Vennix, 1997; Hovmand, 2014; Vennix, 1999).
Table 1.
Demographic Characteristics of Participants in the Group Model Building Session
| Session Number | Participants Number and Profile |
|---|---|
| Session I | 6 Community support members, including breast navigators, research coordinators, city workers and volunteers, participated worked in 2 work groups and later shared their models with everyone. |
| Session II | 28 African American breast cancer survivors from the community and family or caregiver. Participated in 7 work groups, and later shared their models. |
| Session III | All participants (N=34) came together and worked in 3 groups |
The dates for these sessions were March 21st, April 25th, and May 9th
Process/Procedure
The workshop series consisted of three 2-hour sessions: (1) African American women from the community [n=28], (2) community support members [n=6], and (3) both groups combined [N=34] (Table 1). The objective of the first and second sessions were to elicit discussions on factors contributing to the lack of breast cancer treatment initiation and develop a dynamic hypothesis to explain the disparities in the form of a causal loop diagram (CLD). During the third session, participants evaluated the synthesized CLD. To facilitate discussion and understanding about the issue, the women were engaged in a series of structured activities (scripts) at each session including variable elicitation, connection circle, CLD and dot exercise (Table 2).
Table 2.
Group Model Building Session Agenda and Description of Scripted Activities
| Sessions I and II: March 21st and April 25th: Introduction to group model building to elicit discussions on factors contributing to breast cancer treatment delay or initiation | |
| Scripted Activity | Description |
| Introduction to systems, community-based system dynamics, group model building and other important concepts and terms | Welcome, participants divided into work groups. Introduction to the approach of community-based system dynamics/group model building. Defining the primary concept – What is the meaning of breast cancer “treatment delay” (model problem). |
| Variable (factor) Elicitation | To facilitate consensus-based group discussion about treatment delay (model problem), each participant wrote down on A-4 sheet of papers as many factors or variables that responded to the prompt: “What are the key issues contributing to breast cancer treatment delay or may cause African American women with suspicious mammogram not to follow-up/delay.” The key variables became the input for next activity. |
| Variable Prioritization | Each participant prioritized (nominated) the most relevant and impactful variables produced in the previous activity based on the prompt – “Choose your five most important factors that may have contributed to treatment delay of breast cancer among African American women in St. Louis.” |
| Connection Circle | Based on the priority variables that emerged from the previous activity, the facilitators led participants through an exercise to develop a connection circle. A connection circle is a visual tool that can help us identify and understand variables and connections between them. Each work group used the highest rated variables to develop connection circle on sheets of chart paper. |
| Causal Loop Diagram (CLD)/Map Elaboration | Building on the last activity, facilitators introduced the next exercise by first explaining CLD and its purpose. Participants were led through an activity to develop a causal loop diagram describing the causal structure and feedback relationships on breast cancer treatment delay. Participants also nominated causal links, with pauses to discuss the specific assumptions of causality or negotiate definitions of terms as questions emerged. |
| Model Review | At the end of the CLD elaboration activity, facilitators led participants through a structured exercise to restate common definitions established for African American women breast cancer treatment delay as well identify important feedback loops and exogenous variables to ensure that the facilitators understood the issue from participants perceptive |
| Reflector Feedback | The core modeling team (CMT) met and shared highlights of the insights from the groups CLDs from a system thinking/system dynamics perspective to help synthesized all CLDs into one diagram. |
| Session III (All Participants): May 9th: Evaluation of structured CLD on breast cancer treatment delay in St. Louis to reduce disparities in mortality | |
| Introduction | Welcome, all participants (N=34) divided into 3 work groups. Participants revisited lessons learned from the previous session. |
| Review of Synthesized CLD Model put together by Core Model Team | Each work group was tasked to review the synthesized model showing factors contributing to treatment delay in St. Louis. Participants made changes in the form of new structures to the model, explained it, and identified major feedback loops and relationships. |
| Revisiting the CLD Model | New causal structures were incorporated into the model by the CMT. Any other remaining questions were clarified. |
| Dot Exercise and Model Review | At the end of the previous activity, facilitators led participants’ through discussion and dot exercise to identify places in the treatment delay system for potential intervention that could help reduce disparities in mortality among African American women in St. Louis. Each participant received 4 dots and was instructed to place their dots beside the variables/factors (items) they think were most important to them for policy intervention. Facilitators tallied the dots beside each item and created a ranked list of importance. Facilitators presented a summary of the CLD and meeting adjourned. |
In the variable elicitation exercise, each woman was given sheets of paper and markers. The task was for them to write down as many “key” variables/factors affecting breast cancer treatment initiation/delays. Results became input for the next activity ‒ connection circle. The purpose of this activity was to draw a circle, identify the variables and establish a connection between them from a systems perspective.
The next activity was the creation of causal loop map/diagram. The goal was for participants to identify and clearly see the feedback loops in the system. The last scripted activity the women participated in was “dot” exercise, to nominate places in the system (treatment delay) they would most like to see a change or intervention to improve breast cancer treatment outcomes in St. Louis. Each participant was given an equal number of “sticky dots” (4 in this case) to place next to the variables on the CLD that were most important to them in terms of addressing the disparity. All scripted activities (Table 2) were designed to explore interactions and interdependencies between factors affecting treatment delay (system) and develop a common model of the complex dynamics as well as explore possibilities for intervention to reduce disparities in breast cancer mortality in the St. Louis area.
Data Analysis
Analysis of the model happened during each section of the scripted activities as described in Table 2. This enabled the CMT to evaluate the structure of each model for face validity as well as to develop insights about how session participants understood the structure of the problem. Discussions and group insights shared by the participants were documented by the facilitation team through handwritten notes and reflected via revisions to the model. Throughout the course of the sessions, the group analysis drove the development of multiple iterations of the model, all of which were documented through photographs and notes (Trani, Ballard, Bakhshi, & Hovmand, 2016). For instance, each group used a different phrase to explain the important role social support plays in treatment delay reduction. This includes “support from close relatives and children”, “support from friends and coworkers”, “support from church members”, “support from husband and children” and “support from health care providers”. Through discussion and insight revealed about the model, participants and the CMT agreed to use “support system” to capture the various forms of support system. In addition, between sessions and at the end of each workshop, the CMT iterated a further series of the revised model using Vensim PLE software. Revisions primarily focused on closing implicit feedback loops and taking decisions about how constructs could be aggregated or disaggregated to clarify meaning. All revisions were grounded in the model itself and based on notes taken by the facilitation team during the GMB session to ensure that the experiences the women shared on treatment delay were preserved (Figure 1).
Figure 1.
GMB workshops with community support and community member groups
RESULTS
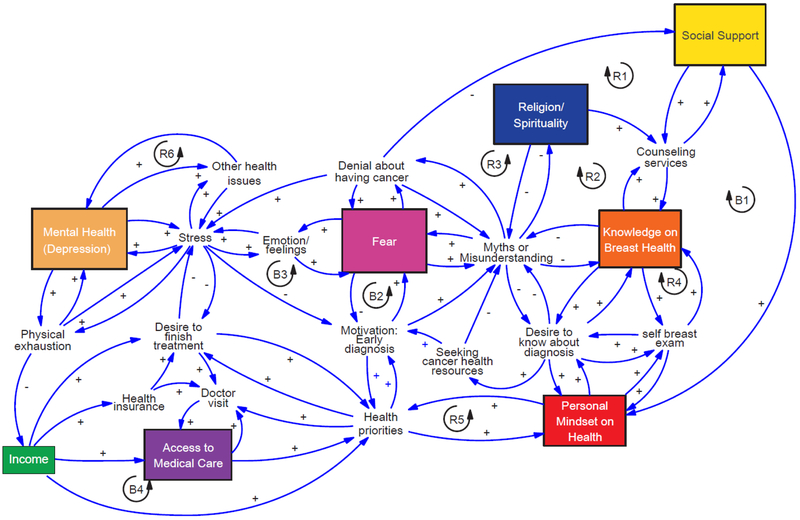
Outputs from the two GMB sessions were synthesized into a large system dynamics CLD by the CMT bearing in mind not to disrupt the stories shared by participants (Figure 2). The built CLD included 8 subsystems or sectors including mental health, access to health care, income, religion/spirituality, social support, knowledge on breast health, personal mindset on health/life and fear. The subsystems are causally linked and include feedback loops, which provide explanations for trends in breast cancer treatment delays in St. Louis.
Figure 2.
CLD showing factors identified by participants to be contributing to BC treatment delay in St. Louis
The next activity was the creation of causal loop map/diagram. The goal was for participants to identify and clearly see the feedback loops in the system. The last scripted activity the women participated in was “dot” exercise, to nominate places in the system (treatment delay) they would most like to see a change or intervention to improve breast cancer treatment outcomes in St. Louis. Each participant was given an equal number of “sticky dots” (4 in this case) to place next to the variables on the CLD that were most important to them in terms of addressing the disparity. All scripted activities (Table 2) were designed to explore interactions and interdependencies between factors affecting treatment delay (system) and develop a common model of the complex dynamics as well as explore possibilities for intervention to reduce disparities in breast cancer mortality in the St. Louis area.
Data Analysis
Analysis of the model happened during each section of the scripted activities as described in Table 2. This enabled the CMT to evaluate the structure of each model for face validity as well as to develop insights about how session participants understood the structure of the problem. Discussions and group insights shared by the participants were documented by the facilitation team through handwritten notes and reflected via revisions to the model. Throughout the course of the sessions, the group analysis drove the development of multiple iterations of the model, all of which were documented through photographs and notes (Trani, Ballard, Bakhshi, & Hovmand, 2016). For instance, each group used a different phrase to explain the important role social support plays in treatment delay reduction. This includes “support from close relatives and children”, “support from friends and coworkers”, “support from church members”, “support from husband and children” and “support from health care providers”. Through discussion and insight revealed about the model, participants and the CMT agreed to use “support system” to capture the various forms of support system. In addition, between sessions and at the end of each workshop, the CMT iterated a further series of the revised model using Vensim PLE software. Revisions primarily focused on closing implicit feedback loops and taking decisions about how constructs could be aggregated or disaggregated to clarify meaning. All revisions were grounded in the model itself and based on notes taken by the facilitation team during the GMB session to ensure that the experiences the women shared on treatment delay were preserved (Figure 1).
RESULTS
Outputs from the two GMB sessions were synthesized into a large system dynamics CLD by the CMT bearing in mind not to disrupt the stories shared by participants (Figure 2). The built CLD included 8 subsystems or sectors including mental health, access to health care, income, religion/spirituality, social support, knowledge on breast health, personal mindset on health/life and fear. The subsystems are causally linked and include feedback loops, which provide explanations for trends in breast cancer treatment delays in St. Louis.
The CLD can be read using the direction of arrows or links, which represent causal relationships. The plus symbol indicates a relationship in the same direction, while minus signs indicate an inverse relationship (Figure 2). Additionally, the CLD contains two major types of feedback loops: reinforcing (R) and balancing (B) loops. Reinforcing feedback loops amplify or accelerate the rate of change (Figure 2). While balancing feedbacks counteract and oppose change (Figure 2). For example, mental health will increase physical exhaustion leading to less income due to the inability of the woman to work. Less income will lead to lack of access to medical care and fewer health priorities. This will lead to lack of motivation/interest for early diagnosis, and fear resulting in denial about cancer, and isolation (decrease social support).
All of these will create a lack of interest in the woman to talk to an expert or go for counseling services. Her knowledge on breast health will be limited, leading to myths or misunderstanding about the disease, and lack of desire to know about her diagnosis or follow-up with any suspicious mammogram or treatment. This will also create negative perception (mindset) and fewer health priorities and desire to know about her diagnosis or even start and finish treatment. This will cause her stress level to increase as well as make her more depressed and exhausted – which becomes a vicious cycle (Figure 2).
Mental Health (including depression) Subsystem
According to the women in the study, mental health affects overall health in diverse ways. This subsystem highlights the relationship between mental health and overall wellbeing, and the impact of mental distress on physical exhaustion, stress, other health issues, and motivation for breast cancer testing. The main feedback loops discussed by the women include: physical exhaustion from general life activities leads to more mental health issues, creating other health issues, which leads to exhaustion that is more physical (Figure 2). Additionally, as mental health issues increase, more negative emotions/feelings about life occur, leading to less motivation to screen for early diagnosis, which can also lead to more health issues thus creating additional mental health problems. Stress, which can be caused by mental health issues, leads to an increase in emotions and feelings, which can result in women feeling more anxious about death, which ultimately leads to more mental health issues – which becomes a vicious cycle (Figure 2).
Access to Medical Care Subsystem
Health care access was identified as critical for breast cancer diagnosis and treatment. Factors that influence this subsystem include motivation and testing for early diagnosis, having primary care doctor (appointment/visit), health priorities, job/employment, transportation, insurance, and cost/affordability of treatment (Figure 2).
Health insurance was mentioned as an important determinant of health status, access, and utilization of health care services. Some of the main feedback loops discussed include access to health insurance and affordability of out-of-pocket payment (copays) can enable low-income women to keep up with doctor’s appointment (visit) regularly and seek early medical care for the health problem, especially cancer. Conversely, barriers like “the women reported that in their opinions, most low-income African American women in their communities lack health insurance.” Participants discussed that the majority of women in the community work in the service sector and are paid minimum wage. In addition, those jobs do not offer health benefits and the pay is not enough to buy insurance on their own. Participants further reported that health care subsidies, such as those offered through the Affordable Care Act or “Obamacare,” have the potential to help families pay for health care. However, barriers including “excessive paperwork, strict eligibility criteria and delays in the approval process” limit their access to those benefits. Others shared that even with Obamacare subsidies, “many women are not able to afford the high premiums and copays” (Figure 2). Further, participants reported that motivation for testing and an early diagnosis, having a primary care doctor, prioritizing health over other concerns, and regular transportation all contribute to treatment delay (Figure 2).
Income Subsystem
Income was another subsystem factor identified by participants. As noted in the previous section, socioeconomic status, identified in this model as “income,” is closely related to one’s ability to access health care. Research has demonstrated a strong relationship between SES and health disparities (Adler & Newman, 2002). A higher income level provides individuals with means to purchase health insurance and ensures access to health care as well as seek early diagnosis and treatment for any health problem (Figure 2).
In St. Louis, the median household income for African American households is $31,200, compared to $61,200 for white households. Similarly, the unemployment for African Americans is 2.8 times higher than it is for whites (St. Louis Regional Health Commission, 2012). Participants were quick to add, “when putting food on the table for your children is hard, the least you want to think of is treating your breast cancer”. The main feedback loops within this subsystem are higher income will improve a woman’s health priorities, increase her motivation to follow-up with suspicious mammogram/diagnosis, and reduce fear as well as denial of having breast cancer. High income can improve her stress and physical exhaustion levels leaving her with more energy to work, provide for her family and take care of her health (Figure 2).
Religion/Spirituality Subsystem
Religion and spirituality are essential to many in the African American community. Polite et al., (2017) (including the senior author of this paper) found that African American breast, lung, and colon cancer patients were more likely than white patients to report that God had a role in their cancer, even after controlling for income and education. Within this subsystem, participants shared that strong spiritual belief that “only God has the power to heal and decide on life and death,” is the reason why many do not seek early medical treatment. On the other hand, they mentioned that “spirituality and faith-based communities” also provide various support/benefits to many women faced with a serious illness like cancer. They noted that “faith in God and church attendance play a significant role not only in their spiritual life but in their overall life and well-being” (Figure 2).
Participants mentioned that being part of a church community is important to their physical needs. Church members are readily available to call on during the time of difficulties and can provide encouragement to seek treatment. The local church can also provide counseling services, or refer women to local providers for information about breast cancer as well as coping methods. Thus, churches can be “helpful gateway to professional services” that can help reduce mental health problems and minimize fear due to myths/misunderstanding about the disease (Figure 2).
Social Support Subsystem
A strong social support network is critical to physical and mental health during stressful and tough times. We gleaned from our workshop series that support from family, friends, and coworkers can be a good resource for breast cancer patients as they go through the journey of diagnosis, treatment, and survivorship. The women shared that within social support system, community supports, such as counseling services and breast cancer support groups, as well as family support and trust, are powerful factors in ensuring that a woman follows up with her suspicious mammogram, starts and finishes treatment.
Participants further shared that support groups can also provide opportunities to exchange information and ideas, connect with other women, provide counseling services, as well as educate women about coping and management of the disease. Strong, tight networks also will reduce feelings of loneliness, isolation, and create more opportunities for a woman to enlarge her network of support as well as reduce any negative perception, fear, and denial she may have about cancer and treatment (Figure 2).
Knowledge of Breast Health Subsystem
Participants reported that many women do not know much about breast health unless they have a problem that needs medical attention. They shared that “becoming familiar with breast anatomy and physiology” can help notice any “changes that occur during a woman’s lifetime.” For instance, a woman’s in-depth understanding on breast health will enable her to perform breast self-examination, which in turn will lead to more understanding on breast health (Figure 2). Additionally, knowledge on breast health will motivate her to follow up with any suspicious mammogram and finish treatment (Figure 2).
The women suggested during the model building that formal education in high school should include programs that teach young women the “importance of breast health and self-breast examination.” They also recommended “development of educational programs for high schools that focus on prevention, risk factors, and adherence to recommended breast cancer screening.” It was also revealed that traditionally, African American families do not “talk” about “disease” at home. They acknowledged the need for “family- and community-based breast health programs.”
Personal Mindset about Health/Life Subsystem
An individual’s personal mindset on health and life (positive or negative) can have a huge impact on disease diagnosis and treatment. Here, we define personal mindset as an individual’s ability to effectively handle the difficult circumstances they face in life. For cancer patients, in particular, positive mindset towards life during the time of diagnosis can be a challenge. Regarding this subsystem, participants brought up the issue of mindset or attitude. One participant said that maintaining a positive mindset on health and life will create a “woman’s desire to know about her diagnosis.” Another related that having a positive mindset can also “reduce the feeling of loneliness or not to be bothered” (Figure 2). The consensus of the groups was that cancer does not only affect a person’s body; emotions, feelings, cognition, and outlook are all impacted, but positive mindset can create “high self-esteem.” On the other hand, negative personal mindset, as shared by the women, may lead to greater social isolation as well as withdrawal and loss of trust in family, friends and society in general, because women feel that they either do not deserve connections or may cause some women to lash out at others in their social networks. Isolation will in turn decrease development of positive mindset about cancer and life (Figure 2).
Fear Subsystem
Despite the progress made in cancer treatment over the past two decades, the disease remains one of the most “dreadful” health concerns among African American women. As has been the case in previous studies using different research approaches (Clow, 2001; Dunn et al., 2015; Hall et al., 2008; Lengacher et al., 2015; Leyva et al., 2014; McGinty, Small, Laronga, & Jacobsen, 2016; Passmore, Williams-Parry, Casper, & Thomas, 2017; Talbert, 2008; Williams & Jeanetta , 2016), women in our study voiced their belief that fear of cancer leads to treatment delays among African American women, which in turn contribute to African American and white disparities in treatment initiation.
Besides, fear can lead to unnecessary anxiety due to the perception of cancer as a “death sentence” (Figure 2). The women noted that cancer is still viewed as a “death sentence” in the community because most of the people they knew who had the disease have died. The fear that “once you are diagnosed you are bound to die,” has caused many women to live in denial about the disease. Some shared that even though they felt changes in their breast and knew there might be something wrong, they refused to acknowledge it. The women in our study acknowledged the belief that fear contributes to further delays in being diagnosed or seeking treatment among African American women, which likely contributes to them being diagnosed at a later stage. They went on to say that being diagnosed at a later stage may increase the risk of mortality, and may be the reason why some African American women attribute dying to cancer. Further, they reported that cancer fear, fatalism, and beliefs about prevention and treatment is discouraging African American women from accessing regular check-ups and early screening services (Figure 2).
DISCUSSION
The determinants of racial/ethnic cancer disparities occur at multiple intersecting levels (Gehlert & Colditz, 2011; Warnecke et al., 2008). They, therefore, require complex system thinking approaches to defining and understanding the problem. This is necessary in order to understand how these determinants work together to fuel behaviors like treatment delays or failure to begin treatment that increase disparities in mortality and to identify appropriate leverage points for action. Using community-based system dynamics, this work engaged community members and health care providers in St. Louis to develop a causal map on factors influencing treatment delays/initiation among African American women. The community-driven model identified 8 subsystems showing interconnectedness among variables and feedbacks in the treatment delay system impacting African American women decision to follow up with a suspicious mammogram or seek early treatment in St. Louis.
Many of the subsystems identified by participants were social. Social factors often differ from community to community and place to place. It is important to understand them from a community or ground-up perspective in order to design successful interventions to decrease disparities. African American women are less likely than white women to begin treatment after a suspicious diagnosis of breast cancer and more to experience delays between diagnosis and treatment, which almost certainly contributes to the increasing African American/white disparity in breast cancer mortality (McGee et al., 2013; Sturtz, Melley, Mamula, Shriver, & Ellsworth, 2014; Wheeler, Reeder-Hayes, & Carey, 2013). The purpose of this model-building project was to better understand factors influencing racial disparities in breast cancer treatment delays among African American women in St. Louis and the interactions between these factors.
The findings from the community-based GMB workshop highlight the complex interrelationships previously suggested by others that distinguish racial/ethnic groups’ treatment delay and mortality among our sample of African American women (Gehlert & Colditz, 2011; Warnecke et al., 2008). The most commonly documented factors of treatment delays have been those related to socioeconomic status, including health insurance, income and education (Adler & Newman, 2002; Baquet & Commiskey, 2000; Bradley, Given, & Roberts, 2002; Clegg et al., 2009; Dai, 2010; Feinglass, Rydzewski, & Yang, 2015; McGee et al., 2013; Shavers & Brown, 2002; Ward et al., 2004; Williams, Tortu, & Thomson, 2010).
Despite the complexity of the factors involved, fear was recognized as one of the major issues contributing to not initiating treatment. While this finding is far from new, it underscores the need for well-coordinated community-based education (Salant & Gehlert, 2008) programs on breast cancer in St. Louis and other inner-city areas that are led by established community stakeholders and academic partnerships that are trusted because they have positive histories with neighborhood and community residents.
This study presents the first of its kind community-based system dynamics model to understand the complex dynamics associated with why women do not start breast cancer treatment. Our work revealed interesting insights regarding how to improve disparities in cancer as well as increase early treatment initiation among African American women in St. Louis. Finally, the model also demonstrates that increasing breast cancer treatment will require a comprehensive approach that involves community members, health care providers, and academics.
Leverage Places of Influence to Promote Early Treatment
Although many of the themes identified in our model building process are not new, our technique allowed us to position them into a single model and thus show how they might operate together. Figure 2 illustrates places in the system that were of the greatest concern to participants, and where they would like to see interventions to reduce breast cancer treatment delays and disparities between African American and white women in St. Louis. The overwhelming majority would like something to be done at the community level to decrease fear associated with the disease. This was followed by income, personal mindset about health and life, loss of sexual desire and partner/relationship, mental health among others. Even though income was recognized as a significant factor, participants noted that unlike other factors, they believed it would be difficult to arrive at a solution(s) that does not require “political debate.” The women suggested the focus of intervention in St. Louis should be on issues like fear, personal mindset, and knowledge on breast health that may not require “highly expensive resources to implement or lead to political debate.”
CONCLUSION
As noted by Gehlert et al. (Gehlert & Colditz, 2011) and Warnecke and colleagues (Warnecke et al., 2008), cancer disparities pose a challenge because they interact at multiple levels of influence, such as the neighborhood, institutional, and societal. The complexity of these interactions calls for an application of dynamic approaches such as community-based system dynamics/GMB to elucidate understanding on these issues and help facilitate the design and implementation of programs as well as policies to meet the needs of specific individuals in their social contexts as is the case in the present study.
Our findings also support the importance of including the voices of stakeholders in understanding and developing effective interventions to address complex problems like racial disparities in cancer. Women also identified a set of recommendations for action based on this structure as follows: (1) Formation of a community-based action group on women’s health in St. Louis like the Metropolitan Chicago Cancer Task Force (Metropolitan Chicago Cancer Task Force, 2014) and Baltimore City Community Health Coalition (Bone et al., 2013) that helped Metropolitan Chicago and Baltimore see a significant reduction in cancer disparities. This group should include community members and professionals working together to develop strategies to educate the community on their health and well-being. The women in the study were grateful to be involved in this project, and are poised to champion education on breast cancer in their community. A number formed a new support group entitled Urban Warriors against Breast Cancer to work with navigators to reduce fear-associated cancer in the community. (2) The design and implementation of strategies that help patient navigators and other health professionals to understand the best way(s) to address women’s fear of cancer at the time of diagnosis. (3) Education of spouse/partners to enhance their understanding and preparation of the potential impact of the disease on relationships, body image, and sexual function and their support. (4) Interventions to maintain the self-esteem of patients and to ensure that spouses and family are able to provide positive attitude and support during and after cancer treatment.
As is often the case in community-based research, women also described how they learned of other women’s situations that differed from their own along with resources that these women could tap into, so they not only had a mental resource map for themselves but also others. Some of the women have indicated that they have become a sort of navigator for other women because of this experience. These findings suggest that developing effective interventions for complex problems like treatment delay requires true stakeholder engagement. Further, this work is also serving as a tool to voice involvements of women in developing effective interventions for breast cancer diagnosis and early treatment initiation.
Over the last decade, little advancement has been made in eliminating cancer disparities in society, and some have increased rather than decreased (Siegel et al., 2017). It is clear from our findings that to address the continuing issue regarding health disparities, and to successfully understand and develop effective interventions to improve cancer outcomes, dynamic approaches are needed that not only identify determinants but also importantly help us to understand how they interact to fuel cancer disparities. System dynamics is one such approach (Homer & Hirsch, 2006; Luke & Stamatakis, 2012). Improving disparities in breast cancer outcomes can be a daunting task, but the present project has laid a foundation by adding a new approach to stakeholder involvement. It has identified non-linear factors and feedback loops responsible for breast cancer disparities as well as leverage strategies needed to improve survival outcomes between African American and white women in St. Louis.
ACKNOWLEDGEMENTS
The authors wish to thank all women who participated, Nancy Zoellner, Maisha Flannel, Lailea Noel, David Habif, Jr., and Linda Talley.
FUNDING SOURCE
This project was supported by the Transdisciplinary Research on Energetics and Cancer (TREC) Center at Washington University in St. Louis. The National Cancer Institute at NIH (U54 CA155496), Washington University School of Medicine in St. Louis, and the Alvin J. Siteman Cancer Center fund the TREC Center
Contributor Information
Faustine Williams, East Tennessee State University.
Graham A. Colditz, Washington University in St. Louis.
Peter Hovmand, University in St Louis.
Sarah Gehlert, Washington University in St Louis.
REFERENCES
- Adler NE, & Newman K (2002). Socioeconomic disparities in health: pathways and policies. Health affairs, 21(2), 60–76. [DOI] [PubMed] [Google Scholar]
- Andersen DF, Richardson GP, & Vennix JA (1997). Group model building: adding more science to the craft. [Google Scholar]
- Baquet CR, & Commiskey P (2000). Socioeconomic factors and breast carcinoma in multicultural women. Cancer, 88(5 Suppl), 1256–1264. [DOI] [PubMed] [Google Scholar]
- Bone L, Edington K, Rosenberg J, Wenzel J, Garza MA, Klein C, … Ford JG (2013). Building a Navigation System to Reduce Cancer Disparities in Urban Black Older Adults. Prog Community Health Partnersh, 7(2), 209–218. doi: 10.1353/cpr.2013.0018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley CJ, Given CW, & Roberts C (2002). Race, Socioeconomic Status, and Breast Cancer Treatment and Survival. J Natl Cancer Inst, 94(7), 490–496. doi: 10.1093/jnci/94.7.490 [DOI] [PubMed] [Google Scholar]
- Clegg LX, Reichman ME, Miller BA, Hankey BF, Singh GK, Lin YD, … Edwards BK (2009). Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control, 20. doi: 10.1007/sl0552-008-9256-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clow B (2001). Who’s afraid of Susan Sontag? Or, the myths and metaphors of cancer reconsidered. Social History of Medicine, 14(2), 293–312. [DOI] [PubMed] [Google Scholar]
- Commission, S. L. R. H. (2012). Decade Review of Health Status for St. Louis City and County 2000–2010: An Update to Building a Healthier St. Louis: Saint Louis Regional Health Commission. [Google Scholar]
- Commission, S. L. R. H. (2012). Towards Building a Healthier St. Louis [Google Scholar]
- Copson E, Maishman T, Gerty S, Eccles B, Stanton L, Cutress R, … Jones L (2014). Ethnicity and outcome of young breast cancer patients in the United Kingdom: the POSH study. Br J Cancer, 110(1), 230–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corner J, Hopkinson J, & Roffe L (2006). Experience of health changes and reasons for delay in seeking care: a UK study of the months prior to the diagnosis of lung cancer. Social Science & Medicim, 62(6), 1381–1391. [DOI] [PubMed] [Google Scholar]
- Dai D (2010). Black residential segregation, disparities in spatial access to health care facilities, and late-stage breast cancer diagnosis in metropolitan Detroit. Health Place,16. doi: 10.1016/j.healthplace.2010.06.012 [DOI] [PubMed] [Google Scholar]
- DeSantis CE, Fedewa SA, Goding Sauer A, Kramer JL, Smith RA, & Jemal A (2016). Breast cancer statistics, 2015: Convergence of incidence rates between black and white women. CA: a cancer journal for clinicians, 66(1), 31–42. [DOI] [PubMed] [Google Scholar]
- DeSantis CE, Siegel RL, Sauer AG, Miller KD, Fedewa SA, Alcaraz KI, & Jemal A (2016). Cancer statistics for African Americans, 2016: Progress and opportunities in reducing racial disparities. CA: A Cancer Journal for Clinicians. [DOI] [PubMed] [Google Scholar]
- Dunn LB, Langford DJ, Paul SM, Berman MB, Shumay DM, Kober K,… Miaskowski C (2015). Trajectories of fear of recurrence in women with breast cancer. Supportive Care in Cancer, 23(7), 2033–2043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feinglass J, Rydzewski N, & Yang A (2015). The socioeconomic gradient in all-cause mortality for women with breast cancer: findings from the 1998 to 2006 National Cancer Data Base with follow-up through 2011. Ann Epidemiol, 25(8), 549–555. doi: 10.1016/i.annepidem.2015.02.006 [DOI] [PubMed] [Google Scholar]
- Gehlert S, & Colditz GA (2011). Cancer disparities: unmet challenges in the elimination of disparities. Cancer Epidemiology and Prevention Biomarkers, 20(9), 1809–1814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall AG, Khoury AJ, Lopez ED, Lisovicz N, Avis-Williams A, & Mitra A (2008). Breast cancer fatalism: the role of women’s perceptions of the health care system. J Health Care Poor Underserved, 19(4), 1321–1335. [DOI] [PubMed] [Google Scholar]
- Homer JB, & Hirsch GB (2006). System Dynamics Modeling for Public Health: Background and Opportunities. Am J Public Health, 96(3), 452–458. doi: 10.2105/AJPH.2005.062059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovmand PS (2014). Community based system dynamics. New York: Springer. [Google Scholar]
- Hunt BR, Whitman S, & Hurlbert MS (2014). Increasing Black: White disparities in breast cancer mortality in the 50 largest cities in the United States. Cancer EpideMiol 38(2), 118–123. [DOI] [PubMed] [Google Scholar]
- Iqbal J, Ginsburg O, Rochon PA, Sun P, & Narod SA (2015). Differences in breast cancer stage at diagnosis and cancer-specific survival by race and ethnicity in the United States. Jama, 313(2), 165–173. doi: 10.1001/jama.2014.17322 [DOI] [PubMed] [Google Scholar]
- Lengacher CA, Reich RR, Paterson CL, Jim HS, Ramesar S, Alinat CB,… Moscoso MS (2015). The effects of mindfulness-based stress reduction on objective and subjective sleep parameters in women with breast cancer: a randomized controlled trial. Psycho-Oncology, 24(4), 424–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leyva B, Allen JD, Tom LS, Ospino H, Torres MI, & Abraido-Lanza AF (2014). Religion, fatalism, and cancer control:a qualitative study among Hispanic Catholics. American journal of health behavior, 38(6), 839–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luke DA, & Stamatakis KA (2012). Systems Science Methods in Public Health: Dynamics, Networks, and Agents. Annual review of public health, 33, 357–376. doi: 10.1146/annurev-publhealth-031210-101222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGee SA, Durham DD, Tse C-K, & Millikan RC (2013). Determinants of breast cancer treatment delay differ for African American and White women. Cancer epidemiology, biomarkers & prevention: a publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology, 22(7), 1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty HL, Small BJ, Laronga C, & Jacobsen PB (2016). Predictors and patterns of fear of cancer recurrence in breast cancer survivors. Health Psychology, 35(1),1. [DOI] [PubMed] [Google Scholar]
- Metropolitan Chicago Breast Cancer Task Force, (2014). How far have we come? Improving access to and quality of breast health services in Chicago, Chicago, IL. Retrieved from http://www.chicagobreastcancer.org/site/files/904/93199/353837/718237/State_of_Breast_Cancer_Disparties_Report_Final_11.pdf
- Passmore SR, Williams-Parry KF, Casper E, & Thomas SB (2017). Message received: African American women and breast cancer screening. Health promotion practice, 1524839917696714. doi: 10.1177/1524839917696714 [DOI] [PubMed] [Google Scholar]
- Polite BN, Cipriano-Steffens T, Hlubocky F, Dignam J, Ray M, Smith D,… Daugherty C (2017). An evaluation of psychosocial and religious belief differences in a diverse racial and socioeconomic urban cancer population. Journal of Racial and Ethnic Health Disparities, 4(2), 140–148. [DOI] [PubMed] [Google Scholar]
- Pronk NP (2013). An integrated framework for assessing the value of community-based prevention: a report of the Institute of Medicine. Prev Chronic Dis,10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeder-Hayes KE, Wheeler SB, & Mayer DK (2015). Health disparities across the breast cancer continuum. Semin Oncol Nurs, 31(2), 170–177. doi: 10.1016/j.soncn.2015.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salant T, & Gehlert S (2008). Collective memory, candidacy, and victimisation: community epidemiologies of breast cancer risk. Sociology of Health & Illness, 30(4), 599–615. [DOI] [PubMed] [Google Scholar]
- Shavers VL, & Brown ML (2002). Racial and ethnic disparities in the receipt of cancer treatment. J Natl Cancer Inst, 94(5), 334–357. [DOI] [PubMed] [Google Scholar]
- Siegel RL, Miller KD, & Jemal A (2017). Cancer Statistics, 2017. CA: A Cancer Journal for Clinicians, 67(1), 7–30. doi: 10.3322/caac.21387 [DOI] [PubMed] [Google Scholar]
- State Cancer Profiles, (2017). State Cancer Profiles Retrieved from https://statecancerprofiles.cancer.gov/cgi-bin/deathrates/deathrates.pl?29&055&02&2&001&0&1&1&1#results
- St. Louis Susan G. Komen Project, (2014). Addressing the African American and white breast cancer mortality disparities in St. Louis [Google Scholar]
- Sturtz LA, Melley J, Mamula K, Shriver CD, & Ellsworth RE (2014). Outcome disparities in African American women with triple negative breast cancer: a comparison of epidemiological and molecular factors between African American and Caucasian women with triple negative breast cancer. BMC Cancer,14, 62. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talbert PY (2008). The relationship of fear and fatalism with breast cancer screening among a selected target population of African American middle class women. Journal of Social, Behavioral, and Health Sciences, 2(1),7. [Google Scholar]
- Trani J-F, Ballard E, Bakhshi P, & Hovmand P (2016).Community based system dynamic as an approach for understanding and acting on messy problems: a case study for global mental health intervention in Afghanistan. Conflict and health, 10(1),25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vennix JAM(1999). Group model-building: tackling messy problems. System Dynamics Review, 15(4), 379–401. doi: [DOI] [Google Scholar]
- Ward E, Jemal A, Cokkinides V, Singh GK, Cardinez C, Ghafoor A, & Thun M (2004). Cancer disparities by race/ethnicity and socioeconomic status. CA Cancer J Clin, 54(2), 78–93. [DOI] [PubMed] [Google Scholar]
- Warnecke RB, Oh A, Breen N, Gehlert S, Paskett E, Tucker KL, … Hiatt RA (2008). Approaching health disparities from a population perspective: The National Institutes of Health Centers for Population Health and Health Disparities. Am J Public Health, 98(9), 1608–1615. doi: 10.2105/AJPH.2006.102525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheeler SB, Reeder-Hayes KE, & Carey LA (2013). Disparities in breast cancer treatment and outcomes: biological, social, and health system determinants and opportunities for research. Oncologist, 18(9), 986–993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DL, Tortu S, & Thomson J (2010). Factors associated with delays to diagnosis and treatment of breast cancer in women in a Louisiana urban safety net hospital. Women Health, 50(8), 705–718. doi: 10.1080/03630242.2010.530928 [DOI] [PubMed] [Google Scholar]
- Williams F, & Jeanetta SC, (2016).Lived experiences of breast cancer survivors after diagnosis, treatment and beyond. Health Expectations, 19(3), 631–642. doi: 10.1111/hex.12372 [DOI] [PMC free article] [PubMed] [Google Scholar]