Abstract
Objective
The purpose of this study was to evaluate the effects of high-intensity interval training (HIIT) and moderate-intensity continuous training (MICT) on cardiovascular disease (CVD) risk factors in adults with overweight and obesity.
Methods
Twenty-two articles were included by searching six databases, the total number of subjects was 620 in these articles. Outcomes were synthesised using a random-effects meta-analysis of the Standardized mean difference (SMD) in CVD risk factors.
Results
HIIT and MICT resulted in statistically significant reductions in Weight, BMI, fat%, total cholesterol(TC), and improvement in VO2max. Compared with MICT, subgroup of durations of HIIT training interval ≥2 min can significantly increase VO2max (SMD = 0.444, 95% CI:0.037~0.851,P = 0.032), subgroup of energy expenditure of HIIT equal to MICT can significantly increase VO2max (SMD = 0.399, 95% CI:0.106~0.692,P = 0.008).
Conclusions
HIIT appears to provide similar benefits to MICT for improving body composition, VO2maxand TC, but HIIT spent less time than MICT by 9.7 min on one session. HIIT is superior to MICT in improving cardiopulmonary fitness when durations of HIIT training interval ≥2 min or energy expenditure of HIIT same as MICT. PROSPERO ID: CRD42016045835.
Introduction
According to epidemiological data, cardiovascular disease (CVD) is the leading cause of death and disability[1, 2]. People who develop CVD not only bear extreme suffering leading to declines in quality of life but also pose a heavy economic burden to their families and the society. BMI and waist circumference are correlated with risk for CVD, its risk factors, and overall mortality,additionallyweight loss medications, but not behavior-based interventions, were associated with higher rates of harms[3]. Therefore, it is of practical importance to identify an appropriate method, especially an no-drug method, of improving the risk factors of CVD and reducing its incidence. Moderate-intensity continuous training (MICT) is often considered an effective way to reduce risk factors of CVD [4, 5]. However, in recent years, a popular protocol calledhigh-intensity interval training (HIIT) which involved brief high-intensity by rest or brief but slightly longer bouts of very low-intensity exercise, is one of the most effective means of improving cardiorespiratory and reducing risk factors of CVD [6–8]. Therefore, a body of experimental studies have been conducted to compare the effects between HIIT and MICT, but their results are inconsistent and inconclusive. Indeed, some experimental studies reported HIIT were more effective than MICT in reducing risks of CVD[9–11], but other studies did not find this result[12]. Although previous meta-analyses have been conducted to compare the effects between two training methods in adolescents with abnormal glucose and lipid metabolism[13, 14], the results HIIT vs. MICT for reducing risk factors of CVD are inconsistent[11, 15–19]. Therefore, we aimed to quantitatively combine data from experimental studies compare the effect between HIIT and MICT in reducing risk factors of CVD in adults with overweight and/or obesity. Findings from this study may serve important evidence for prevention CVD in adults with overweight and/or obesity.
Methods
Literature search
This research program has been registered on the PROSPERO System Evaluation Registration Platform, registration number: CRD42016045835. This study has been reported according to the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines. The searched databases included PubMed, Embase, Cochrane, CENTRAL, PEDro and CNKI. The search strategy comprised key phrases ’interval training’ OR ’interval exercise’ OR ’intermittent exercise’ OR’ intermittent training’ ADN ’overweight’ OR ’obesity’ OR ’obese’ to identify relevant trials, the search strategy was limited to adults, and not animals, adolescent, child. The publication dates of the articles were restricted to the period between the year when the database was built to July 20, 2018.
Study inclusion and exclusion criteria
Inclusion criteria were as follows: (a) randomized controlled trial (RCT) or controlled clinical trial (CCT); (b) healthy participants ≥ 18 years old, BMI ≥ 25; (c) HIIT intervention and MICT intervention,HIIT defined as activities with intermittent bouts of activity that were performed at maximal effort, ≥75% VO2max, ≥75% HR reserve or the relative intensity of at least 85% HR max, The study included a HIIT session lasting ≤4 min/set interspersed with an interval of rest or active recovery; (d) ≥ 4 weeks with intervention; (e) outcome indicators included at least one of the following: weight, body mass index (BMI), fat mass% (fat%), VO2max, triglyceride (TG), total cholesterol (TC), low-density lipoprotein (LDL), high-density lipoprotein (HDL), fasting blood glucose (FBG) and insulin; (f) the study reported that baseline BMI of HIIT participants or baseline BMI could be calculated from the provided data; (g) the article was written in English or Chinese. Exclusion criteria were as follows: (a) participants with chronic diseases, such as diabetes, hypertension, or other diseases constituting a special population; (b) studies on one-time acute exercise; (c) interventions including strength training, diet or medicine; (d) HIIT without supervision.
Data collection
Two authors independently screened titles and abstracts of potentially eligible studies and downloaded the full texts. Discrepancies between the two authors during the literatures exclusion were solved through reaching consensus with each other. Another way of obtaining eligible studies was through examining the references of relevant studies.
Literature quality evaluation
The quality of the literature was evaluated according to the risk bias evaluation method adopted by Costigan et al. [14] in a meta-analysis of HIIT-related research. The eight evaluation items were as follows: (a) inclusion criteria; (b) randomized grouping; (c) baseline similarity; (d) rater-masked; (e) intentional analysis; (f) participants’ withdrawal proportion was less than 20%; (g) the sample quantity met the requirements; (h) accurate results were reported. The two researchers used ’’√’’ (with clear description), "×" (without description) and "?" (unknown or inadequate description) to evaluate each included article. The inconsistent results were solved through discussion among the research group, and each article with a ’’√’’ was counted.
Statistical treatment
Given the consistency of variable units between the same outcome indicator among the continuous variables in the included studies, we compare the changes from baseline to end-point data between groups. Some SD of change is sometimes not supplied, based on Cochrane Handbook for Systematic Reviews of Interventions, we calculate the correlation coefficients using a complete report of the study, and use the correlation coefficients to estimate the SD of the changes from baseline to end-point. Within-group meta-analyses were completed for continuous data using the baseline and post-intervention values. Random-effects models were used in this study for the meta-analysis of included studies. Standardized mean difference(SMD)and 95% CI were calculated in this study for statistical analysis. According to the characteristics of the literature, the factors of durations of HIIT training interval and energy expenditure were analyzed to test the effects of different subgroups. The statistical heterogeneity was examined using I2 between included studies and Cochran’s Q-test. It was defined as non-existent, low, medium and high heterogeneity when I2 values were < 25%, 25 ~ < 50%, 50 ~ < 75%, and ≥ 75%, respectively[19]. Egger test was adopted to detect publication bias. When there was a significant Egger test for publication bias (P <0.05), the trim and fill method was performed to estimate the impact of publication bias on the results[20]. Furthermore, to test the reliability of the results of this study, the following two methods were used to conduct a sensitivity analysis: one article was removed each time to examine whether each article had a significant influence on the effect. Level of significance was set at P< 0.05 and 95% confidence intervals. Magnitude of effect was categorized as large (SMD > 0.8), medium (SMD 0.5~0.8), small (SMD 0.2~0.5) or trivial(SMD < 0.2)[21]. All statistical calculations were performed by statistical software STATA 14.1 (Release 14.1 College Station, TX, USA); P < 0.05 was defined as a significant difference.
Subgroup moderator analysis
HIIT must be applied appropriately by manipulating key programming variables (frequency, intensity, training interval, recovery interval). There are difference contributions of the anaerobic energy systems during events of differing training interval and intensities. The phosphagen and fast glycolytic are the primary energy systems when durations of HIIT training interval < 2 min (DHTI < 2 min), the fast glycolytic energy systems will be gradually depleted when durations of HIIT training interval ≥ 2 min (DHTI ≥2 min)[22]. HIIT programmes were divided into the following subgroups: DHTI ≥ 2 min and DHTI < 2 min. Energy expenditure values were included if reported in the manuscript or were calculated using reported data for group mean VO2max and protocol intensity/duration assuming a 21 kJ min-1 energy expenditure during exercise at a VO2 of 1 L min-1[19]. When exercise energy expenditure (EE) was reported or can be estimated by reported data, the studies were classified as HIIT equal to MICT (H = M), HIIT less than MICT (H<M) or HIIT more than MICT (H>M). On the contrary, when exercise EE was not reported and cannot be estimated, such as sprint interval protocols that have a large anaerobic component, the studies were classified as Not Clear (?). AZ-test was performed to compare the mean effect across subgroups.
Results
Literature search and selection
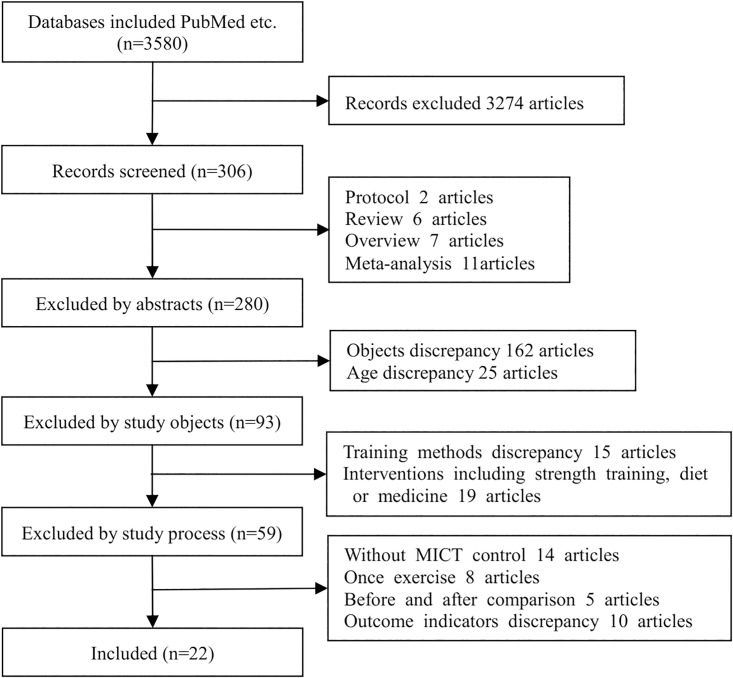
A total of 3580 articles were searched from each database; 3274 articles were excluded according to the inclusion and exclusion criteria, and 22 articles were included[23–44]. The literature screening process is shown in Fig 1.
Fig 1. Study selection process.
Literature characteristics
There were 620participants in the 22 articles examined in this study. A total of 310subjects were in the HIIT group, with 6 ~ 29 subjects in each group; a total of 310 subjects were in the MICT group, with 7 ~ 29 subjects in each group. The training frequency was 3 ~ 5 times a week, and the cycle was 4 ~ 12 weeks. The participants included in this study were trained by ergometry cycle [24, 26, 28, 31–34, 36–38, 41], walking, jogging and running [18, 25, 27, 29, 30, 35, 39, 40, 42–44]. The following target intensity was used in the MICT group: 60 ~ 75% HRmax[23, 26, 31, 32, 35], 50 ~ 60% VO2max[25, 30, 36, 41–43], 10% below the individual anaerobic threshold (IAT) intensity [24], 400% MET (metabolic equivalent of energy) [29], 60 ~ 80 VO2peak [26, 28, 33, 34], 50 ~ 75% HRpeak[40, 44]and 55 ~ 70%HRR[5, 38]. The following target intensity was used in HIIT group: 85 ~ 95%HRmax [23, 27, 29, 31, 35], 85 ~ 90% VO2max [25, 30, 36, 41–44], all out[27, 32, 34, 37–39, 41], 85% peak power [28], 85 ~ 95% HRpeak[40], 20% above the IAT intensity[24], 200% Wmax[33]and 120% VO2peak [26]. VO2max was determined by the method of the stepwise increasing load test combined with gas metabolic analysis. The standards of the end of exercise were that the respiratory quotient was more than 1.05 [23, 32], 1.1 [34, 38, 40]or 1.15 [25, 27, 30], combined with subjective consciousness and the exhaustion of willpower[29, 31, 36]. Blood collection after fasting 8 ~ 12 hours was needed for biochemical index detection. The methods adopted for the body composition test included the following: dual X-ray[23, 25, 26, 28, 31–33, 36, 37], bioelectrical impedance [24, 30, 34, 40–44], air displacement plethysmography with measured thoracic gas volume[38], and skin fold calculation[29]. The outcome indexes included body composition (weight, BMI, fat%), VO2max and glycolipid metabolism indicators (TG, TC, LDL, HDL, FBG, insulin). Total duration of HIIT and MICT were 10.3±3.0 weeks, one session of HIIT and MICT was 30.0±10.2min and 39.7±15.5min respectively, The included studies’ characteristics are shown in Table 1.
Table 1. Summary of included studies.
| Study | Age | BMI | Modality | Energy expenditure | Duration | MICT group | HIIT group | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Intensity | Time(min) | Frequency | n | High intensity | Recovery intensity | Time(min) | Frequency | ||||||
| Schjerve et al.[23] | 46.9 | 36.7 | walking and running | H<M | 12w | 13 | 60–70% HRmax | 47 | 3/w | 14 | 4×4-min 85–95% HRmax | 3 min 50–60% HRmax | 28 | 3/w |
| Moreira et al.[24] | 40 | 28.3 | cycle | H = M | 12w | 8 | 10% lower than IAT | 60 | 3/w | 8 | 2 min intensity was 20% above IAT | 1 min 20% lower than IAT | 60 | 3/w |
| Sijie et al.[25] | 19.8 | 27.7 | walking and jogging | H = M | 12w | 16 | 50% VO2max | 40 | 5/w | 17 | 5×3 min 85% VO2max | 3 min 50% VO2max | 30 | 5/w |
| Keating et al.[26] | 41.8 | 28.2 | cycle | ? | 12w | 13 | 65% VO2peak | 45 | 3/w | 13 | 6×60s 120% VO2peak | 120s low intensity | 18 | 3/w |
| Lunt et al.-1[27] | 48.2 | 32.1 | walking and jogging | H = M | 12w | 7 | 65–75% HRmax | 33 | 3/w | 9 | 4×4-min 85–95% HRmax | 3 min 65–75% HRmax | 28 | 3/w |
| Lunt et al.-2[27] | 50.3 | 32.4 | walking and jogging | ? | 12w | 7 | 65–75% HRmax | 33 | 3/w | 9 | 3×30sce all out | 4 min low intensity | 13.5 | 3/w |
| Wang et al.[40] | 21 | 25.8 | walking and jogging | H = M | 12w | 12 | 60–70% HRpeak | 33 | 4/w | 12 | 4×4 min 85–95% HRpeak | 3 min 50–60% HRpeak+7 min pacing rest | 28 | 4/w |
| Fisher et al.[28] | 20 | 29 | cycle | H<M | 6w | 10 | 55–65% VO2peak,138±13w | 60 | 5/w | 13 | 4×30s 85% peak power,810±250w | 4 min 15% peak power,140±20w | 20 | 3/w |
| Cheema et al.[29] | 43 | 32 | walking | H = M | 12w | 6 | 4 MET | 50 | 4/w | 6 | 10×2 min >75% HRmax | 1 min, standing or pacing | 30 | 4/w |
| Ahmadizad et al.[30]# | 25 | 27.6 | walking and jogging | ? | 6w | 10 | 50–60% VO2max | 60 | 3/w | 10 | 8×2–3 min (rest/intensity = 2:1), intensity: 90% VO2max | 24 | 3/w | |
| Sawyer et al.[31] | 35.1 | 37.4 | cycle | H<M | 8w | 9 | 70–75% HRmax | 30 | 3/w | 9 | 10×1 min 90–95% HRmax | 1 min low intensity | 20 | 3/w |
| Martins et al.-1[32] | 34.4 | 32.4 | cycle | H = M | 12w | 7 | 70% HRmax | 250Kcal deficit time | 3/w | 16 | 8sce all out | 12s low intensity | 250Kcal deficit time | 3/w |
| Martins et al.-2[32] | 34.4 | 32.4 | cycle | H<M | 12w | 7 | 70% HRmax | 250Kcal deficit time | 3/w | 16 | 8sce all out | 12s low intensity | 125Kcal deficit time | 3/w |
| Cocks et al.[33] | 25 | 35.8 | cycle | ? | 4w | 8 | 65% VO2peak | 60 | 5/w | 8 | 4–7×30s 200%Wmax | 120s 30 W | 30 | 3/w |
| Kong et al.[34] | 21 | 25.8 | cycle | H<M | 5w | 13 | 60–80% VO2peak | 40 | 4/w | 13 | 60×8s all out | 12s passive rest | 20 | 5/w |
| Gerosa-Neto et al.[35] | 46.4 | 31.8 | walking and running | H<M | 16w | 11 | 70% HRmax | 30 | 5/w | 11 | 4×4 min90%HRmax | 3 min 75% HRmax | 28 | 3/w |
| Zhang et al.[36] | 18–22 | 38.1% (fat%) | cycle | H = M | 12w | 15 | 60% VO2max | 62.6 | 3-4/w | 15 | 4–6×4 min 90% VO2max | 3 min passive rest | 34 | 3-4/w |
| Liu et al.[41] | 20–23 | 28.8 | cycle | H = M | 12w | 20 | 50% VO2max | 30 | 4/w | 20 | 15×1 min 90% VO2max | 1 min 20% VO2max | 30 | 4/w |
| Zhang et al.[39] | 21 | 25.8 | running | H = M | 12w | 12 | 60–70% HRpeak | 33 | 4/w | 12 | 4×4 min 85–95% HRpeak | 3-min 50–60% HRpeak | 28 | 4/w |
| Higgins et al.[37] | 20.4 | 30.3 | cycle | H = M | 6w | 20 | 60%–70% HRR | 20 | 3/w | 29 | (3–7)30s all out | 4 min of active recovery | 16 | 3/w |
| Vella et al.[38] | 26.2 | 31.6 | treadmill, cycle, elliptical | H = M | 8w | 9 | 55–59% HRR | 20 | 4/w | 8 | 10×1min 75–80% HRR | 1min 35–40% HRR | 20 | 4/w |
| Wang et al.[42] | 18–21 | 28.7 | treadmill, cycle | H = M | 12w | 16 | 60% VO2max | 45 | 4/w | 18 | 7×3min 80–90% VO2max | 3min 50–60% VO2max+1min rest | 36 | 4/w |
| Gao et al.[43] | 21.6 | 27.1 | treadmill | H = M | 12w | 17 | 60% VO2max | 55 | 5/w | 17 | 5×4min 85% VO2max | 2min 50%VO2max+5min rest | 55 | 5/w |
| Eimarieskandari et al.[44] | 22.1 | 29.6 | treadmill | H = M | 8w | 7 | 50–70% HRpeak | 41 | 3/w | 7 | 4×4min80-90%VO2peak | 3min50-60%VO2peak | 33 | 3/w |
MICT:moderate-intensity continuous training; HIIT:high-intensity interval training; IAT: individual anaerobic threshold; MET: Metabolic Equivalent; HR:heart rate; HRR:heart rate reserve. Lunt et al.-1 and Lunt et al.-2 were two different HIIT methods were used in one article. Martinset al.-1 and Martins et al.-2 were two different HIIT methods were used in one article. H = M: Energy expenditure of HIIT equal to MICT; H<M: Energy expenditure of HIIT less than MICT; ?:Not Clear; #: the study is controlled clinical trial and non-randomised trials, unmarked studies arerandomized controlled trial.
Bias and sensitivity analysis
Of the 22 articles, 5 articles were classified as low risk (risk of bias assessment ranging from 7 ~ 8), 16 articles were classified as moderate risk (risk of bias assessment ranging from 4 ~ 6), and one article was classified as high risk (risk of bias assessment ranging from 0 ~ 3), Risk of bias assessment of included studies are presented in Table 2. According to the sensitivity analysis of the 22 articles, if statistical models were replaced and one article was removed each time to perform a meta-analysis again, the results of effect would not change meaningfully, indicating that the results of the meta-analysis in this study were reliable. Egger test for fat% and Insulin determined indication of publication bias, the trim and fill method was proformed to fat% and the rusults suggested that 5 studies were missing, before trim and fill(SMD:-0.159, 95%CI: -0.509~0.191), after trim and fill(SMD: 0.642, 95%CI: 0.443~0.930), these values were changed after using the trim and fill method under the random-effects model, it suggestes that publication bias has great influence on the stability of fat%. The same method suggests that 2 studies were missing to Insulin, these values were unchanged using the trim and fill method under the random-effects model, it suggestes that the effect of publication bias on Insulin can be ignored. Egger test show no significant publication bias for other of the outcome variables(Table 3).
Table 2. Risk of bias assessment of included studies.
| Article | Evaluation items | Score | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Inclusion criteria | Randomized grouping | Baseline similarity | Rater-masked | Intentional analysis | Withdrawal proportion is less than 20% | Sample quantity meets the requirements | Accurate results report | ||
| Schjerve et al.[23] | √ | √ | √ | √ | ? | √ | × | √ | 6 |
| Moreira et al.[24] | √ | √ | √ | ? | ? | √ | × | √ | 5 |
| Sijie et al.[25] | √ | √ | √ | ? | ? | √ | × | √ | 5 |
| Keating et al.[26] | √ | √ | √ | √ | √ | √ | × | √ | 7 |
| Lunt et al.[27] | √ | √ | √ | √ | √ | √ | √ | √ | 7 |
| Wang et al.[40] | √ | √ | √ | ? | ? | ? | × | × | 3 |
| Fisher et al.[28] | √ | √ | √ | √ | √ | √ | × | √ | 7 |
| Cheema et al.[29] | √ | √ | √ | √ | √ | √ | × | √ | 7 |
| Ahmadizad et al.[30] | √ | ? | √ | ? | ? | √ | × | √ | 4 |
| Sawyer et al.[31] | √ | √ | √ | √ | ? | √ | √ | √ | 7 |
| Martins et al.[32] | √ | √ | √ | ? | ? | √ | × | √ | 5 |
| Cocks et al.[33] | √ | √ | √ | ? | ? | √ | × | √ | 5 |
| Kong et al.[34] | √ | √ | √ | ? | ? | √ | √ | √ | 6 |
| Gerosa-Neto et al.[35] | √ | √ | √ | ? | ? | √ | × | √ | 5 |
| Zhang et al.[36] | √ | √ | √ | ? | ? | √ | × | √ | 5 |
| Liu et al.[41] | √ | √ | √ | ? | ? | √ | × | × | 4 |
| Zhang et al.[39] | √ | √ | √ | √ | × | √ | × | √ | 6 |
| Higgins et al.[37] | √ | √ | √ | ? | × | √ | √ | √ | 6 |
| Vella et al.[38] | √ | √ | √ | ? | ? | √ | × | √ | 5 |
| Wang et al.[42] | √ | √ | √ | ? | × | √ | × | √ | 5 |
| Gao et al.[43] | √ | √ | √ | ? | × | √ | × | √ | 5 |
| Eimarieskandari et al.[44] | √ | √ | √ | ? | × | √ | × | √ | 5 |
√: with clear description; ×: without description; ?: unknown or inadequate description.
Table 3. Effects of HIIT vs. MICT on body composition, aerobic capacity, lipid metabolism, glucose metabolism.
| Category | Index | Study (n) | Within-group effects | Between-group effects | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| HIIT | MICT | |||||||||
| SMD (95% CI) | P | SMD (95% CI) | P | SMD (95% CI) | P | I2(%) | Egger test P | |||
| Body composition | Weight, kg | 20 | 0.305(0.117, 0.494) | 0.002* | 0.319(0.129, 0.508) | 0.001* | -0.039(-0.346, 0.268) | 0.803 | 64.2 | 0.529 |
| BMI, kg/m2 | 16 | 0.591(0.139, 1.044) | 0.010* | 0.727(0.272, 1.182) | 0.002* | 0.017(-0.415, 0.449) | 0.938 | 74.9 | 0.614 | |
| fat% | 18 | 0.609(0.248, 0.971) | 0.001* | 0.647(0.315, 0.979) | 0.000* | -0.159(-0.509, 0.191) | 0.374 | 68.4 | 0.016§ | |
| Aerobic capacity | VO2max, ml/kg/min | 16 | -0.966(-1.290, -0.642) | 0.000* | -0.690(-1.037-, 0.343) | 0.000* | 0.256(-0.019, 0.531) | 0.068 | 43.9 | 0.990 |
| Lipid metabolism index | TG, mg/dl | 12 | 0.146(-0.098, 0.390) | 0.241 | 0.068(-0.180, 0.317) | 0.589 | -0.099(-0.489, 0.291) | 0.619 | 60.4 | 0.536 |
| TC, mg/dl | 12 | 0.467(0.157, 0.777) | 0.003* | 0.488(0.176, 0.800) | 0.002* | 0.121(-0.203, 0.445) | 0.464 | 43.1 | 0.279 | |
| LDL, mg/dl | 8 | 0.445(0.092, 0.797) | 0.013* | 0.287(-0.086, 0.661) | 0.132 | -0.101(-0.376, 0.173) | 0.470 | 0.0 | 0.274 | |
| HDL, mg/dl | 19 | 0.129(-0.204, 0.462) | 0.447 | 0.031(-0.276, 0.339) | 0.842 | -0.092(-0.515, 0.332) | 0.671 | 59.9 | 0.079 | |
| Glucose metabolism index | FBG, mmol/l | 10 | 0.372(-0.401, 1.145) | 0.345 | 0.344(-0.246, 0.934) | 0.253 | -0.139(-0.803, 0.524) | 0.681 | 81.4 | 0.476 |
| Insulin, mU/l | 7 | 0.585(-0.318, 1.488) | 0.204 | 0.779(-0.063, 1.621) | 0.070 | 0.348(-0.105, 0.801) | 0.132 | 43.3 | 0.039§ | |
*P<0.05 was defined as a significant difference;
§P<0.05 was defined as publication bias
MICT: moderate-intensity continuous training; HIIT: high-intensity interval training; SMD: Standardized mean difference; BMI: Body Mass Index; TG: triglyceride; TC: Total Cholesterol; LDL: Low-density lipoprotein; HDL: High-density lipoprotein; FBG: fasting blood glucose.
Results of meta-analysis
Within-group analyses are showed in Table 3. Both HIIT and MICT resulted in statistically significant reductions in Weight (SMD: 0.305 and 0.319 for HIIT and MICT, respectively), BMI(SMD:0.591 and 0.727 for HIIT and MICT, respectively), fat%(SMD:0.609 and 0.647 for HIIT and MICT, respectively), TC(SMD:0.467 and 0.488 for HIIT and MICT, respectively), and improvement in VO2max(SMD:-0.966 and -0.690 for HIIT and MICT, respectively), additionally, HIIT can reduce LDL(SMD:0.445 and 0.287 for HIIT and MICT, respectively) but not find in MICT. There was no significant effect of HIIT or MICT on TG, HDL, FBG and Insulin. Comparisons of HIIT and MICT interventions revealed no significant differences in their effects on any measure of body composition, aerobic capacity, lipid and glucose metabolism index(Table 3).
Subgroup analysis
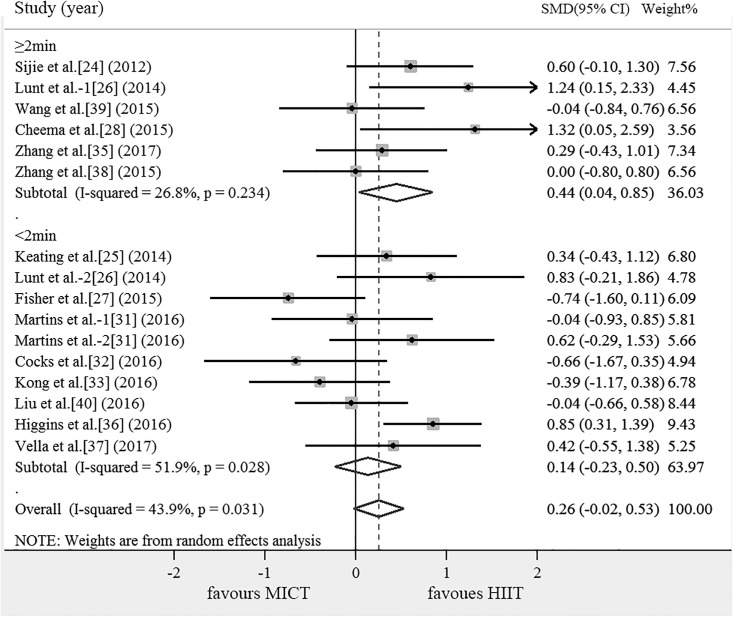
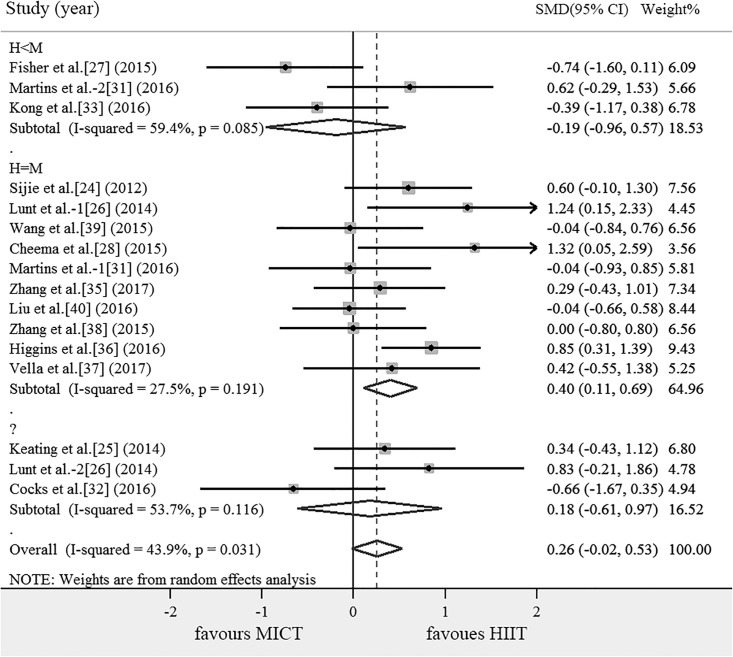
The results of the subgroup analysis of the effects on outcomes are shown in Table 4. Compared with MICT, subgroup of DHTI ≥ 2 min can significantly increase VO2max (SMD = 0.444, 95% CI: 0.037 ~ 0.851, P = 0.032). According to the energy consumption, HIIT were divided into the following subgroups: H = M, H<M, H>M and ?, there are no articles including the subgroup of H>M. Compared with MICT, subgroup of H = M can significantly increase VO2max (SMD = 0.399, 95% CI: 0.106 ~ 0.692, P = 0.008). There was no significant difference across subgroups in the mean effect (Table 4).
Table 4. Results of subgroup analysis.
| Outcome index | Subgroup | Study (n) | SMD (95% CI) | P | Weight% | I2% | Compare across subgroups (P-Value) | |
|---|---|---|---|---|---|---|---|---|
| Weight | DHTI | <2 min | 9 | 0.064(-0.317, 0.445) | 0.741 | 46.46 | 52.5 | 0.817 |
| ≥2 min | 11 | -0.140(-0.630, 0.349) | 0.574 | 53.54 | 72.0 | |||
| Energy expenditure |
H = M | 11 | -0.219(-0.667, 0.228) | 0.337 | 55.68 | 71.1 | 0.693 | |
| H<M | 6 | 0.101(-0.382, 0.584) | 0.682 | 29.90 | 48.9 | |||
| ? | 3 | 0.393(-0.128, 0.913) | 0.139 | 14.42 | 4.6 | |||
| BMI | DHTI | <2 min | 6 | 0.092(-0.634, 0.818) | 0.938 | 37.74 | 76.4 | 0.909 |
| ≥2 min | 10 | -0.028(-0.598, 0.542) | 0.924 | 62.26 | 76.6 | |||
| Energy expenditure |
H = M | 10 | -0.108(-0.730, 0.513) | 0.732 | 62.90 | 81.4 | 0.742 | |
| H<M | 3 | 0.193(-0.503, 0.890) | 0.587 | 25.42 | 62.1 | |||
| ? | 2 | 0.316(-0.390, 1.022) | 0.380 | 11.68 | 0 | |||
| Fat% | DHTI | <2 min | 7 | -0.147(-0.527, 0.232) | 0.447 | 40.95 | 39.6 | 0.998 |
| ≥2 min | 11 | -0.145(-0.699, 0.408) | 0.607 | 59.05 | 77.1 | |||
| Energy expenditure |
H = M | 11 | -0.320(-0.818, 0.178) | 0.208 | 61.20 | 75.7 | 0.516 | |
| H<M | 4 | 0.189(-0.219, 0.597) | 0.363 | 23.18 | 0 | |||
| ? | 3 | 0.095(-0.454, 0.645) | 0.374 | 15.63 | 0 | |||
| VO2 max | DHTI | <2 min | 10 | 0.135(-0.233, 0.504) | 0.472 | 63.97 | 51.9 | 0.632 |
| ≥2 min | 6 | 0.444(0.037, 0.851) | 0.032* | 36.03 | 26.8 | |||
| Energy expenditure |
H = M | 10 | 0.399(0.106, 0.692) | 0.008* | 64.96 | 27.5 | 0.249 | |
| H<M | 3 | -0.192(-0.957, 0.574) | 0.623 | 18.53 | 59.4 | |||
| ? | 3 | 0.179(-0.613, 0.971) | 0.657 | 16.52 | 53.7 | |||
| TG | DHTI | <2 min | 7 | -0.057(-0.565, 0.451) | 0.827 | 58.45 | 60.2 | 0.893 |
| ≥2 min | 5 | -0.162(-0.846, 0.522) | 0.643 | 41.55 | 68.2 | |||
| Energy expenditure |
H = M | 7 | -0.087(-0.548, 0.374) | 0.711 | 59.63 | 53.8 | 0.372 | |
| H<M | 3 | -0.621(-1.443, 0.201) | 0.139 | 24.53 | 61.5 | |||
| ? | 2 | 0.662(-0.246, 1.570) | 0.153 | 15.84 | 47.8 | |||
| TC | DHTI | <2 min | 7 | -0.098(-0.453, 0.258) | 0.590 | 59.47 | 22.4 | 0.334 |
| ≥2 min | 5 | 0.472(-0.084, 1.029) | 0.096 | 40.53 | 50.8 | |||
| Energy expenditure |
H = M | 7 | 0.203(-0.326, 0.733) | 0.451 | 58.41 | 63.6 | 0.372 | |
| H<M | 3 | 0.061(-0.419, 0.542) | 0.802 | 25.59 | 0.0 | |||
| ? | 2 | 0.009(-0.967, 0.985) | 0.986 | 16.00 | 57.8 | |||
| LDL | DHTI | <2 min | 6 | -0.161(-0.495, 0.174) | 0.346 | 71.59 | 5.4 | 0.531 |
| ≥2 min | 2 | 0.042(-0.473, 0.557) | 0.872 | 28.41 | 0.0 | |||
| Energy expenditure |
H = M | 4 | -0.101(-0.480, 0.278) | 0.601 | 55.37 | 4.5 | 0.525 | |
| H<M | 3 | 0.094(-0.386, 0.575) | 0.700 | 32.57 | 0.0 | |||
| ? | 1 | -0.646(-1.436, 0.144) | 0.109 | 12.06 | \ | |||
| HDL | DHTI | <2 min | 7 | -0.200(-0.807, 0.408) | 0.520 | 68.46 | 70.8 | 0.778 |
| ≥2 min | 3 | -0.008(-0.468, 0.452) | 0.973 | 31.54 | 0.0 | |||
| Energy expenditure |
H = M | 5 | 0.156(-0.326, 0.639) | 0.342 | 30.86 | 80.9 | 0.269 | |
| H<M | 3 | -0.423(-1.295, 0.449) | 0.525 | 49.19 | 0.0 | |||
| ? | 2 | 0.000(-0.607, 0.607) | 1.000 | 19.96 | 0.0 | |||
| FBG | DHTI | <2 min | 6 | 0.183(-0.605, 0.972) | 0.649 | 61.08 | 79.2 | 0.422 |
| ≥2 min | 4 | -0.726(-2.071, 0.620) | 0.290 | 38.92 | 87.0 | |||
| Energy expenditure |
H = M | 6 | 0.302(-0.238, 0.842) | 0.273 | 61.64 | 57.7 | 0.560 | |
| H<M | 2 | 0.009(-1.945, 1.963) | 0.993 | 19.97 | 87.9 | |||
| ? | 2 | -2.135(-5.104, 0.834) | 0.159 | 18.39 | 91.9 | |||
| Insulin | DHTI | <2 min | 5 | 0.377(-0.292, 1.046) | 0.269 | 69.88 | 62.0 | 0.962 |
| ≥2 min | 2 | 0.351(-0.259, 0.961) | 0.259 | 30.12 | 0.0 | |||
| Energy expenditure |
H = M | 2 | 0.792(-1.472, 3.056) | 0.493 | 24.61 | 89.2 | 0.054 | |
| H<M | 2 | 0.294(-0.218, 0.806) | 0.261 | 43.78 | 0.0 | |||
| ? | 2 | 0.202(-0.378, 0.783) | 0.494 | 31.61 | 0.0 | |||
*P<0.05 was defined as a significant difference;
<DHTI: Durations of HIIT training interval; SMD: Standardized mean difference; BMI: Body Mass Index; TG: Triglyceride; TC: Total Cholesterol; LDL: Low-density lipoprotein; HDL: High-density lipoprotein; FBG: Fasting blood glucose. ?:Not Clear; \:There is only one article and I2% cannot be calculated.
Discussion
Different exercise modes produce different training effects on body[45]. HIIT and MICT can induce significant improvements in body composition, VO2max and TC. Both HIIT and MICT appear to be similarly effective on risk factors of CVD, however HIIT(30.0±10.2min) save 9.7min compared with MICT(39.7±15.5min) in one session. HIIT is superior to MICT in improving VO2max when durations of HIIT training interval ≥ 2 min or energy expenditure of HIIT same as MICT. Each of these findings has major implications for reducing the risk of CVD management interventions.
Effects of HIIT and MICT on body composition
The results showed that there were no significant differences between HIIT and MICT in reducing fat%, BMI and weight. Currently, the researches support the idea that HIIT has greater effectiveness on weight loss than MICT[25, 29, 46], indicating that exercise intensity plays an important role in regulation of body composition and local fat consumption [29, 47]. HIIT is superior to MICT in promoting the secretion of catecholamines, epinephrine [48], norepinephrine[49] and growth hormone [50], which promote fat decomposition [51, 52] to achieve effective weight loss. Nevertheless, there is still debate about the effectiveness of HIIT for weight loss and the fat burning mechanism of HIIT[53] because improvement in body composition is affected by exercise intensity, frequency, diet and lifestyle et al[54]. Energy balance is critical in the influence of exercise on body composition, Martins et al.[32] adopted HIIT and MICT in interventions for volunteers with overweight or obese under the same total energy consumption and found no significant differences between HIIT and MICT in reducing fat% and weight, but the exercise time of HIIT was much less than that of MICT. As a result, the consumption of total energy plays a more critical role in weight loss relative to the exercise intensity[55], yet it can also consume large amount of total energy to achieve weight loss through a longer period of MICT [56]. In our study, the duration time of one session of the MICT(39.7±15.5 min) programs is more than that of HIIT(30.0±10.2 min). This review indicates that HIIT may provide similar benefits of improving body composition in less energy expenditure compared with MICT, the benefits of HIIT on fat loss have been proposed to reflect changes in appetite responses and an augmented excess post-exercise oxygen consumption (EPOC)[53], additionally, HIIT has greater potential for muscle glycogen depletion than MICT[19]. However, weight loss management is along-term process, the Institute of Medicine defined weight loss maintenance as losing at least 5% of body weight, or reducing body mass index (BMI) by at least 1 unit, and keeping weight below this minimum amount for at least 1 year[57], either HIIT or MICT implemented in long-term is likely to produce clinically meaningful fat loss. Publication bias has great influence on the stability of fat%, thus more studies on the comparison of fat reduction effects between HIIT and MICT need to be studied in future.
Effects of HIIT and MICT on VO2max
In individuals with poor cardiorespiratory fitness, it is much easier to identify CVD than obesity[58]. The risk of CVD decreases by 15% as long as the aerobic capacity increases 1- Metabolic Equivalent of Energy (MET)[59]. Thus, improving cardiorespiratory fitness confers major health benefits for both individuals with obesity and the population with CVD [60]. VO2max is recognized as the important predictors of mortality among cardiac patients, several studies had shown that HIIT was safe in cardiac patients[61], HIIT also can improve VO2max for healthy subjects[62], patients with heart failure[63]. Some researches indicated that HIIT results in greater improvements in VO2max compared to MICT[64, 65], but the results of this review showed that there was no significant difference of HIIT and MICT on improving VO2max. Interestingly, subgroup analysis of this study found that DHTI ≥ 2 min had greater effectiveness than MICT, but the effect of DHTI < 2 min on improving cardiorespiratory fitness was similar to that of MICT, which indicates that DHTI ≥ 2 min obtain more advantage in improving VO2max(SMD = 0.444, 95% CI: 0.037 ~ 0.851, P = 0.032), partly because of DHTI≥ 2 min can keep the heart and lungs in a relatively high working state for a long time. It can be seen that it is necessary to maintain a certain period of time in a higher intensity in order to increase cardiopulmonary fitness. What is the relationship between energy consumption of different sports modes and cardiopulmonary fitness? When compared the energy consumption and the DHTI subgroup, we were surprised to find that 5 of the 6 articles in the DHTI ≥ 2 min subgroup were equal energy expenditure of HIIT and MICT(Figs 2 and 3). It can be seen that energy consumption plays an important role in improving VO2max, furthermore, subgroup analysis showed that HIIT (SMD = 0.399, 95% CI: 0.106 ~ 0.692, P = 0.008) had an advantage in improving cardiopulmonary fitness with the same energy expenditure as MICT(Fig 3). The possible mechanisms of HIIT to improve cardiorespiratory fitness are as follows: In work-matched comparisons, maximum stroke volume increased more following HIIT relative to MICT, HIIT programme elicited an significant increase in skeletal muscle mitochondrial respiration compared with MICT[66], stroke volume and skeletal muscle mitochondrial respiration enhanced the oxygen utilization rate in peripheral blood, thereby improving VO2max and cardiorespiratory fitness. However HIIT and MICT can achieve similar increases in muscle oxidative capacity, as reflected by the activity of cytochrome c oxidase (COX), COX subunits II, IV protein content[67] and 3-hydroxyacyl CoA dehydrogenase[68]. So both durations of training interval and total exercise load play an important role in improving cardiopulmonary fitness, and HIIT has an advantage in improving cardiopulmonary fitness when energy expenditure of HIIT equal to MICT.
Fig 2. Meta-analysis for the comparison of HIIT vs. MICT for VO2max with subgroup analyses for studies employing DHTI < 2 min, DHTI ≥2 min than MICT.
The positive value of X axis indicated that HIIT was more effective than MICT in improving VO2max. Lunt et al.-1 and Lunt et al.-2 were two different HIIT methods were used in one article. Martins et al.-1 and Martins et al.-2 were two different HIIT methods were used in one article. DHTI< 2 min: HIIT training interval < 2 min, DHTI ≥2 min: HIIT training interval ≥ 2 min.
Fig 3. Meta-analysis for the comparison of HIIT vs. MICT for VO2max with subgroup analyses for studies employing H = M, H<M and ? than MICT.
The positive value of X axis indicated that HIIT was more effective than MICT in improving VO2max. Lunt et al.-1 and Lunt et al.-2 were two different HIIT methods were used in one article. Martins et al.-1 and Martins et al.-2 were two different HIIT methods were used in one article. H = M: Energy expenditure of HIIT equal to MICT;H<M: Energy expenditure of HIIT less than MICT; ?:Not mentioned in the article and the results can not be used to calculate the energy consumption.
Effects of HIIT and MICT on lipid metabolism
Individuals with obesity often suffer from lipid metabolism disorder[69], which leads to increase risk of CVD[70]. Exercise is especially known as an economic and effective approach to reduce fat accumulation, however, the results of this review comparisons of HIIT and MICT interventions revealed no significant differences in their effects on TG, TC, LDL, HDL. There was no significant difference in the changes of TC[71], HDL[72], LDL[73], triglycerides[74], and C-reactive protein[75] between HIIT and MICT in the studies examining the improvement of lipid metabolism. The effects of exercise on blood lipid levels in individuals with overweight or obesity depend on blood lipid levels before exercise, exercise intensity, exercise duration, body composition, calorie intake, metabolic rate and lifestyle et al[76–78]. HIIT and MICT in improving TG, TC, LDL, and HDL in adults with overweight and/or obesity may be related to the abovementioned factors, which indicates that these factors should be fully considered in studies examining the influence of exercise mode on blood lipid levels. But the results of this study indicated that HIIT and MICT modes resulted in statistically significant reductions in TC(SMD:0.467 and 0.488 for HIIT and MICT, respectively). Several studies have shown that the decomposition and metabolism of fat have strong sensitivity to hormones[79], and exercise can significantly increase epinephrine, norepinephrine and growth hormone[80] and stimulate fat decomposition[81], the results of this study show that HIIT and MICT are effective approach to reduce TC. Accumulation of LDL inside the blood vessels serves as a major cause of arteriosclerosis, regular exercise enhances the heart and vessel functions and can thus prevent or delay the progress of CVD in part by improving cholesterol levels[82]. This study find that HIIT resulted instatistically significant reductions in LDL(SMD:0.445 and 0.287 for HIIT and MICT, respectively) but not in MICT. Our results suggest that HIIT can prevent LDL accumulation. Regular and continuous exercises especially HIIT help control obesity, reduces the risk of CVD, thus helping prevent or postpone the development of CVD in obese individuals.
Effects of HIIT and MICT on glucose metabolism
Exercise is an effective way to reduce insulin levels[83], insulin-dependent glucose disposal increases following exercise[84], HIIT tended to be superior in reduction FBG and insulin resistance compared with MICT[18, 85]. Some studies found that HIIT can induce higher expression and translocation of glucose transporter 4 (GLUT4) on skeletal muscle cell membrane surfaces in comparison with MICT[86, 87]. Metcalf et al.[88] noted in an observational study lasting 6 ~ 19 years that the effect of regulating insulin and improving insulin resistance will meaningfully weaken or even disappear without enough exercise intensity and suggested that intermittent exercise of sufficient intensity is needed. Improvement of insulin sensitivity is localized to contracting muscle, HIIT recruit a larger proportion of muscle fibres compared with MICT[89], thus HIIT can improve the efficiency of insulin transportation and insulin sensitivity, thereby reduce blood sugar and inhibiting excessive insulin secretion. However a meta-analysis reported no difference between HIIT and MICT[90]. Tjønna et al[91]. reported a reduction in the FBG of patients with metabolic syndrome after 16 weeks of either continuous exercise or intermittent exercise. Gayda et al.[92] reported that intermittent exercise is as effective as continuous exercise for reducing FBG in patients with chronic heart failure. This study found that there was no significant difference between HIIT and MICT in the improvement of FBG and insulin levels, partly because of the included subjects are overweight and/or obesity adults without metabolic diseases. It is noteworthy that the changes in glucose metabolism with either modality was small in terms of clinical meaningfulness, but, given the health benefits of exercise are fundamental in populations with obesity.
Limitations
A major limitation of this study is the heterogeneity of the included literature. Although the heterogeneity was reduced by subgroup analysis, some subgroups still had high heterogeneity, which may have affected the reliability of the results. However, this study used the random-effects model to avoid the adverse effects of high heterogeneity. Publication bias has great influence on the stability of fat%. Cardiovascular risk factors involve many aspects, this study was restricted to analyze the aspects of body composition, aerobic capacity and glycolipid metabolism. Hence, the conclusions may be limited.
Conclusions
HIIT appears to provide similar benefits to MICT for improving body composition, VO2max and TC, but HIIT spent less time than MICT by 9.7 min on one session of training, HIIT can be considered as a time-efficient exercise mode for managing overweight and obese individuals. HIIT resulted instatistically significant reductions in LDL but not in MICT. HIIT is superior to MICT in improving cardiopulmonary fitness when durations of HIIT training interval ≥ 2 min or energy expenditure of HIIT same as MICT.
Prospect: The HIIT mode includes manipulating key programming variables such as frequency, intensity, training interval, recovery interval, the different combinations of these variables will confer different benefits to physical function. Future research directions may include examining which training combinations are more advantageous to improving cardiovascular risk factors.
Supporting information
(DOCX)
(DOC)
(XLSX)
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This study was supported by the National Natural Science Foundation of China (81703252, to MingHui Quan).
References
- 1.Niiranen TJ, Vasan RS. Epidemiology of cardiovascular disease: recent novel outlooks on risk factors and clinical approaches. Expert Rev Cardiovasc Ther. 2016;14(7):855–69. 10.1080/14779072.2016.1176528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahluwalia A, Gladwin M, Coleman GD, Hord N, Howard G, Kim-Shapiro DB, et al. Dietary Nitrate and the Epidemiology of Cardiovascular Disease: Report From a National Heart, Lung, and Blood Institute Workshop. Journal of the American Heart Association. 2016;5(7). 10.1161/jaha.116.003402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.LeBlanc ES, Patnode CD, Webber EM, Redmond N, Rushkin M, O’Connor EA. Behavioral and Pharmacotherapy Weight Loss Interventions to Prevent Obesity-Related Morbidity and Mortality in Adults: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. Jama. 2018;320(11):1172–91. 10.1001/jama.2018.7777 [DOI] [PubMed] [Google Scholar]
- 4.Thompson PD, Arena R, Riebe D, Pescatello LS. ACSM’s new preparticipation health screening recommendations from ACSM’s guidelines for exercise testing and prescription, ninth edition. Current sports medicine reports. 2013;12(4):215–7. 10.1249/JSR.0b013e31829a68cf [DOI] [PubMed] [Google Scholar]
- 5.Hussain SR, Macaluso A, Pearson SJ. High-Intensity Interval Training Versus Moderate-Intensity Continuous Training in the Prevention/Management of Cardiovascular Disease. Cardiology in review. 2016;24(6):273–81. 10.1097/CRD.0000000000000124 [DOI] [PubMed] [Google Scholar]
- 6.Terada T, Friesen A, Chahal BS, Bell GJ, McCargar LJ, Boule NG. Feasibility and preliminary efficacy of high intensity interval training in type 2 diabetes. Diabetes research and clinical practice. 2013;99(2):120–9. 10.1016/j.diabres.2012.10.019 [DOI] [PubMed] [Google Scholar]
- 7.Weston KS, Wisloff U, Coombes JS. High-intensity interval training in patients with lifestyle-induced cardiometabolic disease: a systematic review and meta-analysis. British journal of sports medicine. 2014;48(16):1227–34. 10.1136/bjsports-2013-092576 [DOI] [PubMed] [Google Scholar]
- 8.Babraj JA, Vollaard NB, Keast C, Guppy FM, Cottrell G, Timmons JA. Extremely short duration high intensity interval training substantially improves insulin action in young healthy males. BMC endocrine disorders. 2009;9:3 10.1186/1472-6823-9-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gibala MJ, Little JP, Macdonald MJ, Hawley JA. Physiological adaptations to low-volume, high-intensity interval training in health and disease. The Journal of physiology. 2012;590(5):1077–84. 10.1113/jphysiol.2011.224725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ciolac EG. High-intensity interval training and hypertension: maximizing the benefits of exercise? American journal of cardiovascular disease. 2012;2(2):102–10. [PMC free article] [PubMed] [Google Scholar]
- 11.Wewege M, van den Berg R, Ward RE, Keech A. The effects of high-intensity interval training vs. moderate-intensity continuous training on body composition in overweight and obese adults: a systematic review and meta-analysis. Obesity reviews: an official journal of the International Association for the Study of Obesity. 2017;18(6):635–46. 10.1111/obr.12532 [DOI] [PubMed] [Google Scholar]
- 12.Aguilera Eguia R, Vergara Miranda C, Quezada Donoso R, Sepulveda Silva M, Coccio N, Cortes P, et al. High-intensity interval exercise therapy to reduce cardiovascular risk factors in people with the metabolic syndrome; systematic review with meta-analysis. Nutricion hospitalaria. 2015;32(6):2460–71. 10.3305/nh.2015.32.6.9776 [DOI] [PubMed] [Google Scholar]
- 13.Garcia-Hermoso A, Cerrillo-Urbina AJ, Herrera-Valenzuela T, Cristi-Montero C, Saavedra JM, Martinez-Vizcaino V. Is high-intensity interval training more effective on improving cardiometabolic risk and aerobic capacity than other forms of exercise in overweight and obese youth? A meta-analysis. Obesity reviews: an official journal of the International Association for the Study of Obesity. 2016;17(6):531–40. 10.1111/obr.12395 [DOI] [PubMed] [Google Scholar]
- 14.Costigan SA, Eather N, Plotnikoff RC, Taaffe DR, Lubans DR. High-intensity interval training for improving health-related fitness in adolescents: a systematic review and meta-analysis. British journal of sports medicine. 2015;49(19):1253–61. 10.1136/bjsports-2014-094490 [DOI] [PubMed] [Google Scholar]
- 15.Batacan RB Jr., Duncan MJ, Dalbo VJ, Tucker PS, Fenning AS. Effects of high-intensity interval training on cardiometabolic health: a systematic review and meta-analysis of intervention studies. British journal of sports medicine. 2017;51(6):494–503. 10.1136/bjsports-2015-095841 [DOI] [PubMed] [Google Scholar]
- 16.Weston M, Taylor KL, Batterham AM, Hopkins WG. Effects of low-volume high-intensity interval training (HIT) on fitness in adults: a meta-analysis of controlled and non-controlled trials. Sports medicine (Auckland, NZ). 2014;44(7):1005–17. 10.1007/s40279-014-0180-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ramos JS, Dalleck LC, Tjonna AE, Beetham KS, Coombes JS. The impact of high-intensity interval training versus moderate-intensity continuous training on vascular function: a systematic review and meta-analysis. Sports medicine (Auckland, NZ). 2015;45(5):679–92. 10.1007/s40279-015-0321-z [DOI] [PubMed] [Google Scholar]
- 18.Jelleyman C, Yates T, O’Donovan G, Gray LJ, King JA, Khunti K, et al. The effects of high-intensity interval training on glucose regulation and insulin resistance: a meta-analysis. Obesity reviews: an official journal of the International Association for the Study of Obesity. 2015;16(11):942–61. 10.1111/obr.12317 [DOI] [PubMed] [Google Scholar]
- 19.Keating SE, Johnson NA, Mielke GI, Coombes JS. A systematic review and meta-analysis of interval training versus moderate-intensity continuous training on body adiposity. Obesity reviews: an official journal of the International Association for the Study of Obesity. 2017;18(8):943–64. 10.1111/obr.12536 [DOI] [PubMed] [Google Scholar]
- 20.Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–63. 10.1111/j.0006-341X.2000.00455.x [DOI] [PubMed] [Google Scholar]
- 21.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Research synthesis methods. 2010;1(2):97–111. 10.1002/jrsm.12 [DOI] [PubMed] [Google Scholar]
- 22.Haff GG, Triplett NT. Essentials of strength training and conditioning 4th edition National Strength and Conditioning Association; 2016:53–6. [Google Scholar]
- 23.Schjerve IE, Tyldum GA, Tjonna AE, Stolen T, Loennechen JP, Hansen HE, et al. Both aerobic endurance and strength training programmes improve cardiovascular health in obese adults. Clinical science (London, England: 1979). 2008;115(9):283–93. 10.1042/cs20070332 [DOI] [PubMed] [Google Scholar]
- 24.Moreira MM, Souza HP, Schwingel PA, Sa CK, Zoppi CC. Effects of aerobic and anaerobic exercise on cardiac risk variables in overweight adults. Arquivos brasileiros de cardiologia. 2008;91(4):200–6, 19–26. 10.1590/S0066-782X2008001600003 [DOI] [PubMed] [Google Scholar]
- 25.Sijie T, Hainai Y, Fengying Y, Jianxiong W. High intensity interval exercise training in overweight young women. The Journal of sports medicine and physical fitness. 2012;52(3):255–62. [PubMed] [Google Scholar]
- 26.Keating SE, Machan EA, O’Connor HT, Gerofi JA, Sainsbury A, Caterson ID, et al. Continuous exercise but not high intensity interval training improves fat distribution in overweight adults. Journal of obesity. 2014;2014:834865 10.1155/2014/834865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lunt H, Draper N, Marshall HC, Logan FJ, Hamlin MJ, Shearman JP, et al. High intensity interval training in a real world setting: a randomized controlled feasibility study in overweight inactive adults, measuring change in maximal oxygen uptake. PloS one. 2014;9(1):e83256 10.1371/journal.pone.0083256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fisher G, Brown AW, Bohan Brown MM, Alcorn A, Noles C, Winwood L, et al. High Intensity Interval- vs Moderate Intensity- Training for Improving Cardiometabolic Health in Overweight or Obese Males: A Randomized Controlled Trial. PloS one. 2015;10(10):e0138853 10.1371/journal.pone.0138853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cheema BS, Davies TB, Stewart M, Papalia S, Atlantis E. The feasibility and effectiveness of high-intensity boxing training versus moderate-intensity brisk walking in adults with abdominal obesity: a pilot study. BMC sports science, medicine & rehabilitation. 2015;7:3 10.1186/2052-1847-7-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ahmadizad S, Avansar AS, Ebrahim K, Avandi M, Ghasemikaram M. The effects of short-term high-intensity interval training vs. moderate-intensity continuous training on plasma levels of nesfatin-1 and inflammatory markers. Hormone molecular biology and clinical investigation. 2015;21(3):165–73. 10.1515/hmbci-2014-0038 [DOI] [PubMed] [Google Scholar]
- 31.Sawyer BJ, Tucker WJ, Bhammar DM, Ryder JR, Sweazea KL, Gaesser GA. Effects of high-intensity interval training and moderate-intensity continuous training on endothelial function and cardiometabolic risk markers in obese adults. Journal of applied physiology (Bethesda, Md: 1985). 2016;121(1):279–88. 10.1152/japplphysiol.00024.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Martins C, Kazakova I, Ludviksen M, Mehus I, Wisloff U, Kulseng B, et al. High-Intensity Interval Training and Isocaloric Moderate-Intensity Continuous Training Result in Similar Improvements in Body Composition and Fitness in Obese Individuals. International journal of sport nutrition and exercise metabolism. 2016;26(3):197–204. 10.1123/ijsnem.2015-0078 [DOI] [PubMed] [Google Scholar]
- 33.Cocks M, Shaw CS, Shepherd SO, Fisher JP, Ranasinghe A, Barker TA, et al. Sprint interval and moderate-intensity continuous training have equal benefits on aerobic capacity, insulin sensitivity, muscle capillarisation and endothelial eNOS/NAD(P)Hoxidase protein ratio in obese men. The Journal of physiology. 2016;594(8):2307–21. 10.1113/jphysiol.2014.285254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kong Z, Fan X, Sun S, Song L, Shi Q, Nie J. Comparison of High-Intensity Interval Training and Moderate-to-Vigorous Continuous Training for Cardiometabolic Health and Exercise Enjoyment in Obese Young Women: A Randomized Controlled Trial. PloS one. 2016;11(7):e0158589 10.1371/journal.pone.0158589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gerosa-Neto J, Antunes BM, Campos EZ, Rodrigues J, Ferrari GD, Rosa Neto JC, et al. Impact of long-term high-intensity interval and moderate-intensity continuous training on subclinical inflammation in overweight/obese adults. Journal of exercise rehabilitation. 2016;12(6):575–80. 10.12965/jer.1632770.385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang H, Tong TK, Qiu W, Zhang X, Zhou S, Liu Y, et al. Comparable Effects of High-Intensity Interval Training and Prolonged Continuous Exercise Training on Abdominal Visceral Fat Reduction in Obese Young Women. Journal of diabetes research. 2017;2017:5071740 10.1155/2017/5071740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Higgins S, Fedewa MV, Hathaway ED, Schmidt MD, Evans EM. Sprint interval and moderate-intensity cycling training differentially affect adiposity and aerobic capacity in overweight young-adult women. Applied physiology, nutrition, and metabolism = Physiologie appliquee, nutrition et metabolisme. 2016;41(11):1177–83. 10.1139/apnm-2016-0240 [DOI] [PubMed] [Google Scholar]
- 38.Vella CA, Taylor K, Drummer D. High-intensity interval and moderate-intensity continuous training elicit similar enjoyment and adherence levels in overweight and obese adults. European journal of sport science. 2017;17(9):1203–11. 10.1080/17461391.2017.1359679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang H, Tong TK, Qiu W, Wang J, Nie J, He Y. Effect of high-intensity interval training protocol on abdominal fat reduction in overweight chinese women: a randomized controlled trial. Kinesiology. 2015;47(1):57–66. [Google Scholar]
- 40.Wang JJ, Han H, Zhang H. Effects of High-intensity Interval Training and Continuous Training on Abdominal Fat in ObeseYoung Women. Chinese J Sports Med. 2015;34(1):15–20. [Google Scholar]
- 41.Liu HF, Liu ZM, Wang CM. Effect of high intensity interval training on lose weight in obese young women. J Shandong Sport University. 2016;32(6):95–8. [Google Scholar]
- 42.Wang XM. The influence effect of HIIT and LIAT for simple obesity young men. J Guangzhou Sport University. 2017;37(1):100–6. 10.3969/j.issn.1007-323X.2017.01.024 [DOI] [Google Scholar]
- 43.Gao YM, Wang GM, Yang WL, Qiao XF. Effects of high intensity interval training and aerobic exercise on lipid metabolism and chronic inflammation in obese adolescents. Chinese J Sports Med. 2017;36(7):628–32. [Google Scholar]
- 44.Eimarieskandari R, Zilaeibouri S, Zilaeibouri M, Ahangarpour A. Comparing two modes of exercise training with different intensity on body composition in obese young girls. Ovidius University Annals, Series Physical Education & Sport/Science, Movement & Health. 2012;12(2):473–8. [Google Scholar]
- 45.Buchheit M, Laursen PB. High-intensity interval training, solutions to the programming puzzle: Part I: cardiopulmonary emphasis. Sports medicine (Auckland, NZ). 2013;43(5):313–38. 10.1007/s40279-013-0029-x [DOI] [PubMed] [Google Scholar]
- 46.Maillard F, Pereira B, Boisseau N. Effect of High-Intensity Interval Training on Total, Abdominal and Visceral Fat Mass: A Meta-Analysis. Sports medicine (Auckland, NZ). 2018;48(2):269–88. 10.1007/s40279-017-0807-y [DOI] [PubMed] [Google Scholar]
- 47.Lee S, Kuk JL, Davidson LE, Hudson R, Kilpatrick K, Graham TE, et al. Exercise without weight loss is an effective strategy for obesity reduction in obese individuals with and without Type 2 diabetes. Journal of applied physiology (Bethesda, Md: 1985). 2005;99(3):1220–5. 10.1152/japplphysiol.00053.2005 [DOI] [PubMed] [Google Scholar]
- 48.Williams CB, Zelt JG, Castellani LN, Little JP, Jung ME, Wright DC, et al. Changes in mechanisms proposed to mediate fat loss following an acute bout of high-intensity interval and endurance exercise. Applied physiology, nutrition, and metabolism = Physiologie appliquee, nutrition et metabolisme. 2013;38(12):1236–44. 10.1139/apnm-2013-0101 [DOI] [PubMed] [Google Scholar]
- 49.Peake JM, Tan SJ, Markworth JF, Broadbent JA, Skinner TL, Cameron-Smith D. Metabolic and hormonal responses to isoenergetic high-intensity interval exercise and continuous moderate-intensity exercise. American journal of physiology Endocrinology and metabolism. 2014;307(7):E539–52. 10.1152/ajpendo.00276.2014 [DOI] [PubMed] [Google Scholar]
- 50.Freda PU, Shen W, Heymsfield SB, Reyes-Vidal CM, Geer EB, Bruce JN, et al. Lower visceral and subcutaneous but higher intermuscular adipose tissue depots in patients with growth hormone and insulin-like growth factor I excess due to acromegaly. The Journal of clinical endocrinology and metabolism. 2008;93(6):2334–43. 10.1210/jc.2007-2780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bracken RM, Linnane DM, Brooks S. Plasma catecholamine and nephrine responses to brief intermittent maximal intensity exercise. Amino acids. 2009;36(2):209–17. 10.1007/s00726-008-0049-2 [DOI] [PubMed] [Google Scholar]
- 52.Zouhal H, Jacob C, Delamarche P, Gratas-Delamarche A. Catecholamines and the effects of exercise, training and gender. Sports medicine (Auckland, NZ). 2008;38(5):401–23. 10.2165/00007256-200838050-00004 [DOI] [PubMed] [Google Scholar]
- 53.Boutcher SH. High-intensity intermittent exercise and fat loss. Journal of obesity. 2011;2011:868305 10.1155/2011/868305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Must A, Tybor DJ. Physical activity and sedentary behavior: a review of longitudinal studies of weight and adiposity in youth. International journal of obesity (2005). 2005;29 Suppl 2:S84–96. [DOI] [PubMed] [Google Scholar]
- 55.Grediagin A, Cody M, Rupp J, Benardot D, Shern R. Exercise intensity does not effect body composition change in untrained, moderately overfat women. Journal of the American Dietetic Association. 1995;95(6):661–5. [DOI] [PubMed] [Google Scholar]
- 56.Hong HR, Jeong JO, Kong JY, Lee SH, Yang SH, Ha CD, et al. Effect of walking exercise on abdominal fat, insulin resistance and serum cytokines in obese women. Journal of exercise nutrition & biochemistry. 2014;18(3):277–85. 10.5717/jenb.2014.18.3.277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stevens J, Truesdale KP, McClain JE, Cai J. The definition of weight maintenance. International journal of obesity (2005). 2006;30(3):391–9. 10.1038/sj.ijo.0803175 [DOI] [PubMed] [Google Scholar]
- 58.Blair SN, Brodney S. Effects of physical inactivity and obesity on morbidity and mortality: current evidence and research issues. Medicine and science in sports and exercise. 1999;31(11 Suppl):S646–62. [DOI] [PubMed] [Google Scholar]
- 59.Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Asumi M, et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: a meta-analysis. Jama. 2009;301(19):2024–35. 10.1001/jama.2009.681 [DOI] [PubMed] [Google Scholar]
- 60.Katzmarzyk PT, Church TS, Blair SN. Cardiorespiratory fitness attenuates the effects of the metabolic syndrome on all-cause and cardiovascular disease mortality in men. Archives of internal medicine. 2004;164(10):1092–7. 10.1001/archinte.164.10.1092 [DOI] [PubMed] [Google Scholar]
- 61.Nilsson BB, Westheim A, Risberg MA. Effects of group-based high-intensity aerobic interval training in patients with chronic heart failure. The American journal of cardiology. 2008;102(10):1361–5. 10.1016/j.amjcard.2008.07.016 [DOI] [PubMed] [Google Scholar]
- 62.Helgerud J, Hoydal K, Wang E, Karlsen T, Berg P, Bjerkaas M, et al. Aerobic high-intensity intervals improve VO2max more than moderate training. Medicine and science in sports and exercise. 2007;39(4):665–71. 10.1249/mss.0b013e3180304570 [DOI] [PubMed] [Google Scholar]
- 63.Wisloff U, Stoylen A, Loennechen JP, Bruvold M, Rognmo O, Haram PM, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: a randomized study. Circulation. 2007;115(24):3086–94. 10.1161/CIRCULATIONAHA.106.675041 [DOI] [PubMed] [Google Scholar]
- 64.Rognmo O, Hetland E, Helgerud J, Hoff J, Slordahl SA. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. European journal of cardiovascular prevention and rehabilitation: official journal of the European Society of Cardiology, Working Groups on Epidemiology & Prevention and Cardiac Rehabilitation and Exercise Physiology. 2004;11(3):216–22. [DOI] [PubMed] [Google Scholar]
- 65.Cornish AK, Broadbent S, Cheema BS. Interval training for patients with coronary artery disease: a systematic review. European journal of applied physiology. 2011;111(4):579–89. 10.1007/s00421-010-1682-5 [DOI] [PubMed] [Google Scholar]
- 66.MacInnis MJ, Gibala MJ. Physiological adaptations to interval training and the role of exercise intensity. The Journal of physiology. 2017;595(9):2915–30. 10.1113/JP273196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gibala MJ, Little JP, van Essen M, Wilkin GP, Burgomaster KA, Safdar A, et al. Short-term sprint interval versus traditional endurance training: similar initial adaptations in human skeletal muscle and exercise performance. The Journal of physiology. 2006;575(Pt 3):901–11. 10.1113/jphysiol.2006.112094 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Burgomaster KA, Howarth KR, Phillips SM, Rakobowchuk M, Macdonald MJ, McGee SL, et al. Similar metabolic adaptations during exercise after low volume sprint interval and traditional endurance training in humans. The Journal of physiology. 2008;586(1):151–60. 10.1113/jphysiol.2007.142109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Smith-Ryan AE, Melvin MN, Wingfield HL. High-intensity interval training: Modulating interval duration in overweight/obese men. The Physician and sportsmedicine. 2015;43(2):107–13. 10.1080/00913847.2015.1037231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chang KT, Chen CH, Chuang HH, Tsao YC, Lin YA, Lin P, et al. Which obesity index is the best predictor for high cardiovascular disease risk in middle-aged and elderly population? Archives of gerontology and geriatrics. 2018;78:165–70. 10.1016/j.archger.2018.06.002 [DOI] [PubMed] [Google Scholar]
- 71.Ciolac EG, Bocchi EA, Bortolotto LA, Carvalho VO, Greve JM, Guimaraes GV. Effects of high-intensity aerobic interval training vs. moderate exercise on hemodynamic, metabolic and neuro-humoral abnormalities of young normotensive women at high familial risk for hypertension. Hypertension research: official journal of the Japanese Society of Hypertension. 2010;33(8):836–43. 10.1038/hr.2010.72 [DOI] [PubMed] [Google Scholar]
- 72.Wallman K, Plant LA, Rakimov B, Maiorana AJ. The effects of two modes of exercise on aerobic fitness and fat mass in an overweight population. Research in sports medicine (Print). 2009;17(3):156–70. 10.1080/15438620903120215 [DOI] [PubMed] [Google Scholar]
- 73.Mitranun W, Deerochanawong C, Tanaka H, Suksom D. Continuous vs interval training on glycemic control and macro- and microvascular reactivity in type 2 diabetic patients. Scandinavian journal of medicine & science in sports. 2014;24(2):e69–76. 10.1111/sms.12112 [DOI] [PubMed] [Google Scholar]
- 74.Kessler HS, Sisson SB, Short KR. The potential for high-intensity interval training to reduce cardiometabolic disease risk. Sports medicine (Auckland, NZ). 2012;42(6):489–509. 10.2165/11630910-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 75.Moholdt T, Aamot IL, Granoien I, Gjerde L, Myklebust G, Walderhaug L, et al. Aerobic interval training increases peak oxygen uptake more than usual care exercise training in myocardial infarction patients: a randomized controlled study. Clinical rehabilitation. 2012;26(1):33–44. 10.1177/0269215511405229 [DOI] [PubMed] [Google Scholar]
- 76.Durstine JL, Grandjean PW, Davis PG, Ferguson MA, Alderson NL, DuBose KD. Blood lipid and lipoprotein adaptations to exercise: a quantitative analysis. Sports medicine (Auckland, NZ). 2001;31(15):1033–62. [DOI] [PubMed] [Google Scholar]
- 77.Trejo-Gutierrez JF, Fletcher G. Impact of exercise on blood lipids and lipoproteins. Journal of clinical lipidology. 2007;1(3):175–81. 10.1016/j.jacl.2007.05.006 [DOI] [PubMed] [Google Scholar]
- 78.Adedeji OO. Diet, alcohol consumption, smoking and exercise as determinants of blood lipid levels of Nigerians. West African journal of medicine. 2000;19(4):283–5. [PubMed] [Google Scholar]
- 79.Arner P, Kriegholm E, Engfeldt P, Bolinder J. Adrenergic regulation of lipolysis in situ at rest and during exercise. The Journal of clinical investigation. 1990;85(3):893–8. 10.1172/JCI114516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pritzlaff CJ, Wideman L, Blumer J, Jensen M, Abbott RD, Gaesser GA, et al. Catecholamine release, growth hormone secretion, and energy expenditure during exercise vs. recovery in men. Journal of applied physiology (Bethesda, Md: 1985). 2000;89(3):937–46. 10.1152/jappl.2000.89.3.937 [DOI] [PubMed] [Google Scholar]
- 81.Irving BA, Davis CK, Brock DW, Weltman JY, Swift D, Barrett EJ, et al. Effect of exercise training intensity on abdominal visceral fat and body composition. Medicine and science in sports and exercise. 2008;40(11):1863–72. 10.1249/MSS.0b013e3181801d40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Chung J, Kim K, Hong J, Kong HJ. Effects of prolonged exercise versus multiple short exercise sessions on risk for metabolic syndrome and the atherogenic index in middle-aged obese women: a randomised controlled trial. BMC women’s health. 2017;17(1):65 10.1186/s12905-017-0421-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Suh S, Jeong IK, Kim MY, Kim YS, Shin S, Kim SS, et al. Effects of resistance training and aerobic exercise on insulin sensitivity in overweight korean adolescents: a controlled randomized trial. Diabetes & metabolism journal. 2011;35(4):418–26. 10.4093/dmj.2011.35.4.418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mikines KJ, Sonne B, Farrell PA, Tronier B, Galbo H. Effect of physical exercise on sensitivity and responsiveness to insulin in humans. The American journal of physiology. 1988;254(3 Pt 1):E248–59. 10.1152/ajpendo.1988.254.3.E248 [DOI] [PubMed] [Google Scholar]
- 85.Cassidy S, Thoma C, Houghton D, Trenell MI. High-intensity interval training: a review of its impact on glucose control and cardiometabolic health. Diabetologia. 2017;60(1):7–23. 10.1007/s00125-016-4106-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Whyte LJ, Gill JM, Cathcart AJ. Effect of 2 weeks of sprint interval training on health-related outcomes in sedentary overweight/obese men. Metabolism: clinical and experimental. 2010;59(10):1421–8. 10.1016/j.metabol.2010.01.002 [DOI] [PubMed] [Google Scholar]
- 87.Little JP, Jung ME, Wright AE, Wright W, Manders RJ. Effects of high-intensity interval exercise versus continuous moderate-intensity exercise on postprandial glycemic control assessed by continuous glucose monitoring in obese adults. Applied physiology, nutrition, and metabolism = Physiologieappliquee, nutrition et metabolisme. 2014;39(7):835–41. 10.1139/apnm-2013-0512 [DOI] [PubMed] [Google Scholar]
- 88.Metcalf BS, Hosking J, Henley WE, Jeffery AN, Mostazir M, Voss LD, et al. Erratum to: Physical activity attenuates the mid-adolescent peak in insulin resistance but by late adolescence the effect is lost: a longitudinal study with annual measures from 9–16 years (EarlyBird 66). Diabetologia. 2015;58(12):2900 10.1007/s00125-015-3753-y [DOI] [PubMed] [Google Scholar]
- 89.Gollnick PD, Piehl K, Saltin B. Selective glycogen depletion pattern in human muscle fibres after exercise of varying intensity and at varying pedalling rates. The Journal of physiology. 1974;241(1):45–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.De Nardi AT, Tolves T, Lenzi TL, Signori LU, Silva A. High-intensity interval training versus continuous training on physiological and metabolic variables in prediabetes and type 2 diabetes: A meta-analysis. Diabetes research and clinical practice. 2018;137:149–59. 10.1016/j.diabres.2017.12.017 [DOI] [PubMed] [Google Scholar]
- 91.Tjonna AE, Lee SJ, Rognmo O, Stolen TO, Bye A, Haram PM, et al. Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: a pilot study. Circulation. 2008;118(4):346–54. 10.1161/CIRCULATIONAHA.108.772822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gayda M, Normandin E, Meyer P, Juneau M, Nigam A. Comparison of carbohydrate and lipid oxidation during continuous and intermittent exercise in patients with chronic heart failure. The Canadian journal of cardiology. 2013;29(8):990–2. 10.1016/j.cjca.2012.11.005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOC)
(XLSX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.