Telemedicine may improve access to specialty care, particularly in underserved, rural areas.1 To promote telemedicine adoption, “parity” laws, which mandate coverage and/or reimbursement for telemedicine, have passed in 32 (64%) U.S. states as of 2016.2 However, little is known about telemedicine adoption nationally among the commercially insured. To address this gap, we examined trends in telemedicine use and its association with regional factors (parity legislation and physician supply) within a large commercial health plan.
METHODS
We used 2005–2017 data from OptumLabs™ Data Warehouse, a de-identified claims database for privately insured and Medicare Advantage enrollees in a large, private U.S. health plan. Database enrollees are younger and more concentrated in the South compared to the overall US population. Telemedicine visits were identified using Medicare criteria3 and grouped into 3 categories: telemental health (visits with mental health clinicians, mental health-specific CPT codes, or primary mental health diagnoses), primary care telemedicine (non-telemental health visits with primary care clinicians), and other telemedicine (all remaining specialist visits).
We estimated growth in telemedicine use from 2005–2017 using a regression model with a linear variable for time and log-transformed telemedicine visit volume as the dependent variable. We examined trends in telemedicine use stratified by state parity laws4 and county-level physician supply. Using separate multivariable regression with the dependent variable of telemedicine visits per 1,000 enrollees, we examined linear indicators for time interacted with presence of parity law and level of physician supply to estimate differences in trends between categories. All statistical analyses were performed in R (version 3.5.0), with 2-sided P values <0.05 considered significant. The Harvard Medical School institutional review board exempted this study from review.
RESULTS
From 2005–2017, there were 383,565 telemedicine visits by 217,851 patients. From 2015–2017, telemedicine users had an average age of 38.3 years, were 63.0% female and 83.3% resided in urban areas. Users of primary care telemedicine were younger on average than telemental health users (38.0 vs, 39.7 years, respectively) and were more likely to reside in urban areas (87.1% vs. 75.2%, respectively).
Annual telemedicine visits among all members increased from 206 in 2005 (0.020 per 1,000, 95% CI 0.018–0.021) to 202,374 in 2017 (6.57 per 1,000, 95% CI 6.54–6.60), an average annual compound growth rate of 49% (95% CI 41–58) (38%, 95% CI [33–43], from 2005–2014 and 260%, 95% CI [205–328] from 2015–2017; Figure 1). Most telemedicine visits were either telemental health (53%) or primary care telemedicine (39%). Primary care telemedicine visits grew 26% annually before 2016 and then rose sharply to 136,366 visits in 2017, while telemental health grew 47% annually to 57,095 visits in 2017. By 2017, primary care telemedicine was the most frequently used form of telemedicine.
Figure :
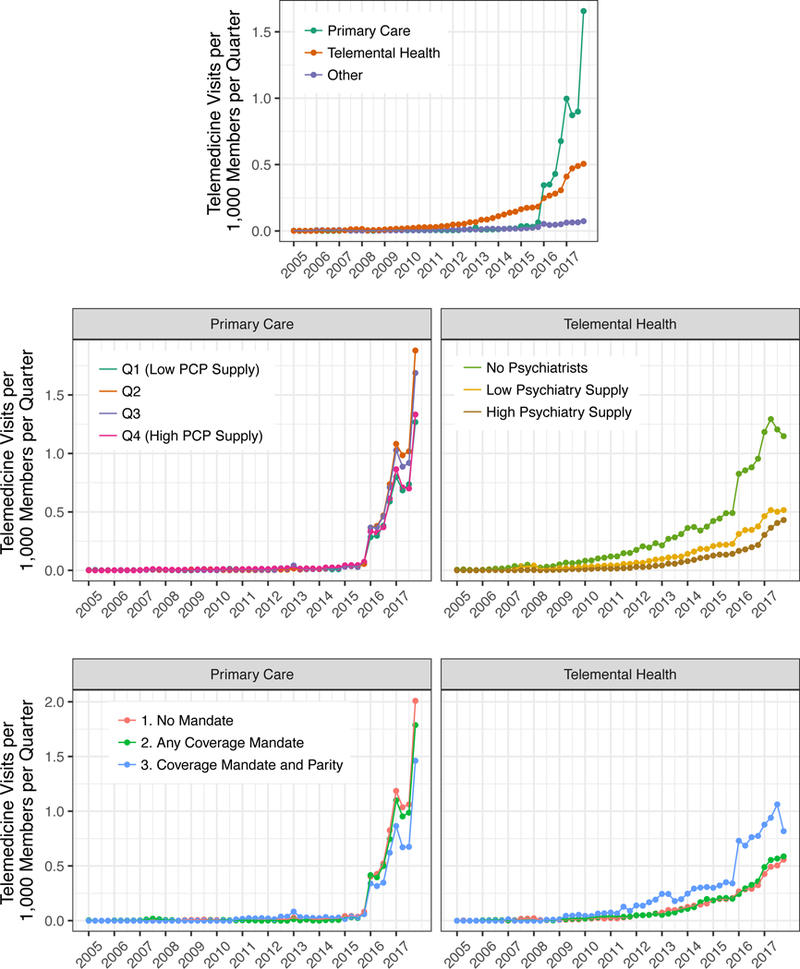
Trends in Total Telemedicine Visits by Specialty, 2005–2017
Abbreviations: primary care physician (PCP)Top row: Rate of telemedicine visits per 1,000 members per quarter (right panel) are shown. Telemedicine use is stratified by primary care telemedicine (green), telemental health (orange), and other specialties (purple, 10% of total volume).
Middle row: Unadjusted trends in the rate of telemedicine visits per 1,000 members per quarter are shown, stratified by county-level characteristics in physician supply. In the left panel, rates of primary care telemedicine are stratified by quartiles of county-level supply of primary care physicians (PCPs) per capita, with varying percentages of total enrollees in each (10% of enrollees in Q1 [low], 39% in Q2, 33% in Q3 and 18% in Q4 [high]). In the right panel, rates of telemedicine mental health care (telemental health) are stratified according to whether a county had no psychiatrists (7% of enrollees), low supply (below average among counties with any supply, ≤6.2 psychiatrists per 100,000; 25% of enrollees), or high supply (above average among counties with any supply, >6.2 psychiatrists per 100,000; 67% of enrollees).
Bottom row: Unadjusted trends in the rate of telemedicine visits per 1,000 members per quarter are shown, stratified by state-level telemedicine parity and coverage laws. We defined three levels of parity/coverage laws, no mandate for coverage or parity (red; 68% of enrollees), any mandate for insurer coverage of telemedicine (green; 26% of enrollees) and full mandate of coverage and reimbursement parity (blue; 6% of enrollees). In the left panel, rates of primary care telemedicine and shown and in the right panel, rates of telemedicine mental health care (telemental health) are shown.
Telemental health growth was significantly faster in counties with no psychiatrists (p<0.001, Figure 1) and in states with comprehensive parity mandates (p=0.02). In contrast, primary care telemedicine growth was not associated with primary care physician supply (p=0.76) and there was a small negative association with comprehensive parity laws (p=0.04).
DISCUSSION
Although telemedicine grew substantially from 2005–2017, use was still uncommon by 2017. Telemental health use grew steadily over this period. In contrast, there was a rapid increase in growth for primary care telemedicine in 2016 and 2017 after coverage for direct-to-consumer telemedicine expanded.5,6 An important limitation is that these data are from one insurer whose population and policies may not generalize to other populations.
In this sample, telemedicine for subspecialty care beyond mental health was uncommon and despite the attention given to telemedicine for rural settings, most telemedicine users lived in urban areas. Physician supply appears to be influential for telemental health, but not for primary care telemedicine, whose brisk adoption may reflect consumers seeking convenience rather than low primary care supply. There is widespread belief that the key barrier to telemedicine adoption is reimbursement. This evidence suggests local reimbursement regulations may have influenced telemental care, but not primary care telemedicine growth.
ACKNOWLEDGEMENTS
MLB had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Supported by a gift from Melvin Hall and a grant from the NIH (R01MH112829). Dr. Barnett was supported by a career development award from the National Institute on Aging (K23AG058806). Dr. Ray was also supported by a career development award from the NIH (NICHD K23HD088642).
Contributor Information
Michael L. Barnett, Department of Health Policy and Management, Harvard T. H. Chan School of Public Health, Pittsburgh, PA.
Kristin N. Ray, Department of Pediatrics, University of Pittsburgh School of Medicine, Pittsburgh, PA.
Jeff Souza, Department of Health Care Policy, Harvard Medical School, Pittsburgh, PA.
Ateev Mehrotra, Department of Health Care Policy, Harvard Medical School, Pittsburgh, PA.
REFERENCES
- 1.Dorsey ER, Topol EJ. State of Telehealth. N Engl J Med 2016;375(2):154–61. [DOI] [PubMed] [Google Scholar]
- 2.Telehealth Parity Laws. Health Aff. - Health Policy Briefs. (Accessed Jul 30, 2018 at http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=162)
- 3.Center for Medicare and Medicaid Services. Telehealth Services. 2016;(Accessed Aug 29, 2017 at https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/TelehealthSrvcsfctsht.pdf)
- 4.Trout KE, Rampa S, Wilson FA, Stimpson JP. Legal Mapping Analysis of State Telehealth Reimbursement Policies. Telemed J E-Health Off J Am Telemed Assoc 2017;23(10):805–14. [DOI] [PubMed] [Google Scholar]
- 5.Pittman D Major insurer adds telemedicine in Medicare Advantage plans. POLITICO. (Accessed May 1, 2018 at https://www.politico.com/tipsheets/morning-ehealth/2016/01/politicos-morning-ehealth-telemedicines-use-in-medicare-advantage-biden-talks-tumor-sequencing-and-data-onc-faca-talks-ehr-tool-212103)
- 6.UnitedHealthcare now covers Doctor On Demand, American Well video visits too. MobiHealthNews. 2015;(Accessed May 1, 2018 at http://www.mobihealthnews.com/43052/unitedhealthcare-now-covers-doctor-on-demand-american-well-video-visits-too) )


