Abstract
Numerous factors have been shown to increase sexual risk-taking—especially among gay and bisexual men (GBM), who remain disproportionately affected by HIV and STIs. We present three lines of evidence that highlight the need to consider a previously under-explored situational factor in sexual risk-taking: tiredness. While tiredness has been shown, in sleep science literature, to impair cognition, emotional functioning, and decision-making in a wide range of behaviors, it has yet to be considered in-depth as a risk factor in sexual behavior. Counter to the common-sense assumption that being tired should impede the performance of active, effortful behaviors such as sex, we propose that tiredness may actually increase sexual risk-taking. Analyzing data from an online survey of 1,113 HIV-negative GBM, we found that sex with casual partners most commonly occurred at night, especially among younger GBM and those with an evening chronotype, and that sex without condoms more often occurred at or later than one’s usual time of feeling tired (as was reported by 44.2% of men) than did sex with condoms (reported by 36.6%). We also found that tiredness can increase sexual desire in many GBM (endorsed by 29.9%), and increases the likelihood of engaging in receptive positioning in anal sex (endorsed by almost 40% of men with a versatile sexual positioning identity). These findings highlight the importance of considering tiredness as a situational risk factor in sexual health—especially among younger GBM—and of counting sex among the behaviors that can be adversely impacted by poor or overdue sleep.
Keywords: sleep, sex, men who have sex with men (MSM), HIV, sexually-transmitted infections (STIs)
Introduction
Tiredness— whether due to needing sleep or feeling fatigued, worn out, or less-than-alert—has complex implications for the study of risk-taking behaviors. Whether arising as a result of sleep deprivation, poor quality or inadequate sleep, or the fluctuations in energy and alertness that occur throughout the day and night according to one’s circadian preference or chronotype (i.e., being a morning person vs. being more of a “night owl” or evening person), tiredness has the potential either: (1) to decrease engagement in active, effortful behaviors (Engle-Friedman, 2014) and thus lower the odds of encountering risk-taking situations, or (2) to decrease the ability and motivation to self-regulate when a choice or temptation is presented, and thus raise the odds of risk-taking. Applying this to sexual risk-taking, tiredness may, on the one hand, dissuade the individual from engaging in sex (the “too tired to have sex” phenomenon), or alternatively, tiredness may lead to riskier decisions when sex does occur, such as not using condoms, not communicating with a partner about sexual health, or not utilizing other strategies to minimize health risks in-the-moment (the “not too tired to have sex, but too tired to be proactive and vigilant about sexual health” phenomenon). The current paper focuses on exploring the latter of these two.
A wealth of sleep deprivation studies have shown that when faced with a choice or task—such as gambling (Venkatraman, Chuah, Huettel, & Chee, 2007), deciding between health and unhealthy foods (Greer, Goldstein, & Walker, 2013), choosing the quick-and-easy option in a complex task (Engle-Friedman et al., 2003), cheating (Gunia, Barnes, & Sah, 2014)—the tired individual is less likely to successfully self-regulate, given deficits in the performance of brain regions involving top-down cognitive control or executive functioning (see Durmer & Dinges, 2005; Palmer & Alfano, 2017; Schmidt, Collette, Cajochen, & Peigneux, 2007; van der Helm & Walker, 2012, for reviews). At the same time, tiredness also exacerbates emotional reactivity (see Kahn, Sheppes, & Sadeh, 2013; Perogamvros & Schwartz, 2015, for reviews) and various physical or visceral desires (e.g., Pejovic et al., 2010). Situating this within a dual processes framework of self-regulation (e.g., Metcalfe & Mischel, 1999), we argue that tiredness situationally compromises self-regulatory success—here, related to sexual behavior—by impairing the cognitive, rational, higher-order capacities involved in “cool” processing and by exacerbating the desires or urges which fuel more emotion-laden, “hot” processing.
Indeed, the role of tiredness in risk-taking has been substantiated by a meta-analysis in which 23 of 28 studies linked sleep deprivation with increased risk-taking (Womack, Hook, Reyna, & Ramos, 2013)—and accordingly, poor sleep has recently gained recognition as a risk factor in models of health behavior (e.g., Barber, 2014; Hagger, 2014; Terre, 2014). However, tiredness has rarely been considered in research regarding sexual risk-taking, whether focused on heterosexuals or on sexual minorities—and here, the current study will focus on gay and bisexual men (GBM), as they face disproportionately high rates of HIV and sexually-transmitted infections (STIs; Centers for Disease Control & Prevention, CDC, 2016).
Leaving aside clinical studies linking chronic sleep disorders with reduced sexual functioning (e.g., Allen & Desille, 2017; Kling et al., 2017; Budweiser et al., 2009; Lin et al., 2015), we are aware of only five studies that have considered tiredness or poor sleep in connection with increased sexual interest, behavior, and/or risk-taking. Two experimental studies have shown that sleep deprivation led men to pay greater attention to images of attractive women (Zarcone, de la Pena, & Dement, 1974), and that poorer overall sleep quality in women was associated with greater sexual arousal after an induced sexual fantasy exercise (Costa & Oliveira, 2016). In three survey studies, poor sleep health in adolescents was connected to a range of risk-taking behaviors including sex (McKnight-Eily et al., 2011), shorter sleep duration in young adults was associated with having less restricted views on sociosexual attitudes and desire (Randler, Jankowski, Rahafar, & Diaz-Morales, 2016), and in the only study to focus on GBM, poor overall sleep quality was associated with higher rates of receptive condomless anal sex (Duncan et al., 2016).
Relatedly, the need for further exploration of the role of tiredness in sexual behavior and risk-taking is in part heightened by evidence that sex might often be occurring in the context of tiredness, insofar as it typically happens late at night when tiredness is more likely to be impairing self-regulation and decision-making. Sex as primarily—though not strictly—a late-night activity is indicated by a small number of studies focusing mostly on heterosexuals and sex with main partners. One survey of young heterosexual married couples in North Carolina found that roughly two-thirds of sex events occurred between 10pm and 1am (Palmer, Udry, & Morris, 1982). An Israeli study found that first sexual experiences occurred in the evening or night for 87% of the 108 women surveyed (Barak, Stein, Ring, Ticher, & Elizur, 1997). A study surveying college students in South Carolina and California found that sex most often occurred between 11pm and 1am, with a secondary peak occurring in the morning between 6–8am (Refinetti, 2005)—and more recently, a Polish study found that the usual time of sex peaked between 6pm and midnight, and even later for men with an evening chronotype (9pm-3am; Jankowski, Díaz-Morales, & Randler, 2014). The only study, to our knowledge, that has partly approached the issue of time of sex among GBM and with casual partners looked at timings of men’s usage of a popular mobile app for sex hook-ups (Goedel & Duncan, 2015), and found that the majority of these men were most active on the app late at night (40%) or in the evening (35%), compared to daytime (25%).
Considering the above studies, we surmise that sex is, for many people, a behavior that typically occurs at night—and often late at night just before going to sleep. We argue that the lateness of the hour may be important for sexual risk-taking if people are also affected by tiredness in the moment of making sexual decisions. However, these studies were not focused on risk-taking and thus did not address the question of whether condoms were used. They also did not specifically ask about sex with casual partners, which may involve higher risk for HIV and STI transmission, assuming that the health status of casual partners may be less thoroughly known than that of one’s main partner. Research on the timing of actual sex events among GBM with casual partners and with reference to condom use is lacking—and the importance of addressing this lack was emphasized by Millar (2017) who argued that, as tiredness generally increases towards the end of the waking day (Manly, Lewis, Robertson, Watson, & Datta, 2002), generally peaking just before bed-time (Watson, Wiese, Vaidya, & Tellegen, 1999), then researchers should consider the effects of tiredness on a given health behavior if it tends to occur late at night.
Accordingly, our first aim in the current study was to extend the existing literature by focusing on a comparatively large sample of GBM across a wider range of ages, gathering information on their timing of sex with casual partners, and exploring whether sex without condoms (here, condomless anal sex; CAS) tends to occur later at night than sex with condoms (SWC). Given the well-established association between tiredness and general risk-taking (Womack et al., 2013), we hypothesized that sex (both CAS and SWC) with casual partners would most often occur late at night and often later than one’s usual time of becoming tired (Hypothesis 1) and further, that CAS would more commonly occur when men are more likely to be tired than would SWC (Hypothesis 2). Considering Jankowski et al.’s (2014) finding of later times of sex for men with an evening chronotype, we also explored whether these times shifted according to chronotype. Indeed, the current study is among the first to consider whether the principle of “circadian misalignment” (i.e., the mismatch between an individual’s chronotype, or preferred time of day for being “in one’s prime” or “at one’s peak,” and the timing of when activities are encountered and attempted; Schmidt, Collette, Cajochen, & Peigneux, 2007; Curtis, Burkley, & Burkley, 2014) might be applied to sex. Circadian misalignment is often applied to morning-related domains such as early start-times for school, work, or sports/exercising, typically to the detriment of evening types in terms of impaired performance and/or self-regulation. However, we argue that it might also apply at the other end of the waking day—i.e., night-time activities—with impairments in self-regulation expected to occur sooner in the night for morning types and later in the night for evening types, when navigating health decisions later than their usual time of becoming tired.
The second line of evidence to be explored, aside from the timing of sex, is the question of whether tiredness uniformly decreases the desire for sex, or whether it might actually increase desire among some men. In light of the five studies described earlier which connected tiredness with increased sexual desire and/or activity (e.g., Zarcone et al., 1974)—along with studies connecting tiredness with other visceral desires (e.g., Pejovic et al., 2010)—we aimed to explore the effect of tiredness on sexual desire. We hypothesized that, for a substantial proportion of GBM, tiredness would not necessarily decrease their desire for sex and may, in fact, increase their felt desire. We also explored whether these proportions differed according to chronotype (Hypothesis 3).
Finally, our third line of enquiry returns more directly to the issue of risk for HIV and STI transmission, by considering sexual positioning in anal sex between GBM—as being the receptive partner is associated with increased risk (CDC, 2012). Anal sex between two men generally allows either man to decide on whether to be the insertive (i.e., “top”) or receptive (i.e., “bottom”) partner, and the majority of GBM are versatile in their sexual positioning (Lyons et al., 2011), whereas positioning in heterosexual sex is typically more predetermined. As such, GBM are tasked with an additional risk-related decision to make in the moment of having sex which is usually already settled in other couplings—and this decision-making for GBM may also be subject to the effects of situational tiredness. Accordingly, our final aim was to explore the effect of tiredness on the odds of being the receptive partner. We hypothesized that tiredness would increase the likelihood of being the receptive partner (Hypothesis 4), informed by research connecting tiredness with decreased expenditure of energy (Engle-Friedman, 2014)—although the question of which position requires more effort may not be unanimously agreed upon. We anticipated, however, that this may less applicable for those who strictly identify as tops or bottoms—i.e., those whose positioning identity makes it unlikely that they would change their positioning preference even when tired. We therefore explored differences with respect to usual sexual positioning identity, but did not advance any hypotheses regarding chronotype, as there was no reason to expect that positioning would differ according to chronotype. Taken together, the three lines of enquiry (and the four hypotheses they generated) described above aimed to explore the effects of tiredness on sexual risk-taking among GBM.
Method
Participants and procedure
Cross-sectional data were drawn from the 24-month assessment of One Thousand Strong, a longitudinal study following a national cohort of HIV-negative GBM over a period of three years (for more details, see Grov et al., 2016). Participants were identified via Community Marketing and Insight’s (CMI) panel of over 22,000 GBM throughout the USA and were eligible if they: were at least 18 years of age; were biologically male and currently identified as male and as gay or bisexual; self-reported an HIV-negative status, and; were able to complete online surveys in English and at-home self-administered testing for HIV (oral) and STIs. Participants also needed to report having sex with a man within the past year, have an address to receive mail that was not a P.O. Box, and have not moved more than twice in the past six months prior (i.e., residential stability). Of the 1,071 men who joined the study at baseline, 985 (92.0%) completed the 24-month assessment and were included in the current study. In the third year of the project, an additional 128 GBM of color were recruited and received the 24-month assessment as their first assessment. This brought the full sample for the current study to 1,113 HIV-negative GBM. Participants completed the online survey via a unique emailed link and were compensated with a $25 Amazon gift card for survey completion. All protocols were approved by the Hunter College Institutional Review Board.
Measures
Demographics.
Participants reported their birthdate, race and ethnicity, relationship status, sexual orientation, education, and annual income.
Chronotype.
Chronotype was measured using the widely-used 5-item version of Horne and Östberg’s (1975) Morningness-Eveningness Questionnaire (MEQ-R; Adan & Almirall, 1991). Response items to each of the five items vary and are weighted in their scoring. In accordance with Adan and Almirall’s recommendation, the following five groups can be classified: definitely morning type (22–25); moderately morning type (18–21); intermediate type (12–17); moderately evening type (8–11), and; definitely evening type (4–7). These groups were combined into three categories—morning types, intermediate types, and evening types—that have been commonly used in the literature (see Adan et al., 2012, for review).
Usual time of becoming tired.
Participants indicated the time (rounded to the nearest hour) when they typically begin to feel tired on a weeknight. This variable was used to determine whether the most recent event of sex had occurred later than the participant’s usual time of becoming tired, although it could not be determined whether the sex event had occurred on a weeknight or weekend. For example, a participant who reports generally becoming tired at 9pm, but who last had CAS at 11pm and last had SWC at 7pm was coded as a 1 for CAS (being at or later than one’s usual time of tiredness) and a 0 for SWC (being earlier than one’s usual time of tiredness). Each of the following items were created by the investigative team, as no other existing studies have asked questions about time-of-day, anal sex, and condom use.
Timing of most recent sex with a casual partner.
Participants indicated the time of day when their most recent event of CAS with a casual partner had occurred—and separately, the time when their most recent event of SWC had occurred. In response to the stem “Thinking back to the last time you had anal sex with a casual partner, WITHOUT [or WITH] a condom, was it during the day or during the night?”, participants indicated whether: 1 (It was during the day), 2 (It was during the night), or 3 (Not applicable, I have never had anal sex with a casual partner WITHOUT a condom). If participants answered 1 or 2, they were then asked to recall the approximate time of that event from a drop-down menu to the closest half-hour. These times were grouped into: daytime (from 6am up to 5pm), evening (from 5pm up to 9pm), night (from 9pm up to midnight), and midnight or later (from midnight to 6am).
Tiredness on sexual desire.
In response to the stem “After I’ve had a long day…”, participants chose the answer that best describes the effect of tiredness on their level of sexual desire and/or arousal, from among the following options: 1 (Being tired doesn’t reduce my libido/sex-drive at all [i.e., it has no effect on my ability to become sexually aroused]), 2 (Being tired reduces my libido/sex-drive a little bit), 3 (Being tired reduces my libido/sex-drive a lot), or 4 (Being tired reduces my libido/sex drive-completely [i.e., I will not become aroused if I am tired]). In response to a second item, participants answered true or false to the statement: “Sometimes, being tired actually increases my libido/sex-drive” (“false” coded as 0). This second item allowed for participants to indicate that tiredness has a range of effects on their sexual desire.
Usual sexual positioning identity.
Participants indicated whether they generally consider themselves to be a “top” (the insertive partner in anal sex), a “bottom” (the receptive partner), or “versatile” on the following scale: 1 (Top), 2 (Versatile/Top), 3 (Versatile), 4 (Versatile/Bottom), or 5 (Bottom).
Tiredness on positioning in anal sex.
In response to the stem “If I am tired but am still wanting to have anal sex…”, participants chose one of the following options: 1 (Being tired would not change my preference for being a “top” or a “bottom”), 2 (Being tired would probably make me more likely to “bottom”), or 3 (Being tired would probably make me more likely to “top”).
Analytic Plan
Although the full sample was asked about the timing of their last events of CAS and SWC, comparisons for Hypotheses 1 and 2 regarding time of sex events were limited to only those who reported having had both CAS and SWC with casual partners within the past year in order to maximize the extent to which age, chronotype, and other covariates (e.g., relationship status) would be contemporaneous with the event. We checked for differences between the subsample (i.e., those reporting both CAS and SWC in the past year) and those not included in these analyses. Bivariate comparisons among the subsample by chronotype and age were conducted for the four different times of day. At the multivariable level, binary logistic regressions were run to predict the odds of reporting a “later-than-9pm” time of last sex event, separately for CAS and SWC (where we grouped both 9pm-midnight and midnight-6am as “later-than-9pm”, compared to “earlier-than-9pm” or daytime and evening grouped together). In a separate model, we also tested whether the event occurred at or later than the participant’s usual time of becoming tired (testing Hypothesis 1). In Step 1 of each model, age was entered alongside the following covariates: race/ethnicity (White as the referent), relationship status (partnered as the referent), education (less than college degree as the referent) and income ($50K or less as the referent). In Step 2, chronotype (morning type as the referent) was entered. Improvement in model fit was indicated by Model and Step χ2 statistics and inspection of the Hosmer and Lemeshow χ2 (where a p<0.05 result indicates that the covariance matrix implied by the specified model deviates significantly from that observed in the data).
The full sample was included in analyses for Hypotheses 3 and 4. We tested for differences in frequencies of whether being tired reduces or increases sexual desire or increases odds of receptive sex by chronotype, age, and usual sexual positioning identity. Binary logistic regression predicting endorsement of the statement that “being tired can sometimes increase my libido/sex drive” included the predictors of age and chronotype (in the three groupings) in a stepwise progression. Finally, binary logistic regression predicting endorsement of the statement that “being tired would probably make me more likely to bottom” (vs. the other two responses combined) included age and usual sexual positioning identity (in the five groupings as described above) in stepwise progression. The covariates of race/ethnicity, relationship status, income, and education were included in analyses for Hypotheses 1 and 2, as we reasoned that sociodemographic factors might affect the times when people’s schedules may allow them to have sex. However, these covariates were not included for Hypotheses 3 and 4 as there was no reason to expect they would affect desire or positioning.
Results
As displayed in Table 1, the full sample of 1113 HIV-negative GBM (utilized for Hypotheses 3 and 4) had a mean age of 41.3 (SD = 13.6), was mostly White (62.8%), and was evenly split by relationship status and income. Most participants identified as gay (95.3%) whereas 4.7% identified as bisexual. Chronotype distributions were morning types (21.6%), intermediate types (49.9%), and evening types (28.6%). Age differences by chronotype emerged, F(2, 1110) = 63.7, p < 0.001—on average, evening types were significantly younger (M = 36.7, SD = 12.3) than morning types (M = 49.0, SD = 13.0; t(556) = −11.39, p < 0.001) and intermediate types (M = 40.7, SD = 13.2; t(871) = −4.34, p < 0.001). Of the 1113 men, 344 reported having had both CAS and SWC with casual partners in the last year and these men constituted the analytic sample for Hypotheses 1 and 2. Men in this group were, on average, younger and were more likely to be single and Black, compared to those who did not report both CAS and SWC in the last year. However, the two groups did not differ on income, sexual orientation, chronotype, or the reported times of their last CAS or SWC.
Table 1.
Total Sample (for Aims 3 & 4) and Subsample with Recent CAS and SWC with Casual Partners (for Aims 1 & 2)
| Demographics | Total | Recent CAS+SWC |
No recent CAS+SWC |
Test Statistic |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Overall | 1113 (100) | 344 (30.9) | 769 (69.1) | |
| Race and Ethnicity | ||||
| Black | 135 (12.1) | 59 (17.2)a | 76 (9.9)b |
χ2(3) = 18.03*** |
| Latino | 177 (15.9) | 59 (17.2) | 118 (15.3) | |
| White | 699 (62.8) | 188 (54.7)a | 511 (66.4)b | |
| Multiracial/Other | 102 (9.2) | 38 (11.0) | 64 (8.3) | |
| Sexual Identity | ||||
| Gay | 1061 (95.3) | 325 (94.5) | 736 (95.7) | χ2(1) = 0.81 |
| Bisexual | 52 (4.7) | 19 (5.5) | 33(4.3) | |
| Relationship Status | ||||
| Single | 542 (48.7) | 235 (68.3) | 307 (39.9) |
χ2(1) = 76.69*** |
| Partnered | 571 (51.3) | 109 (31.7) | 462 (60.1) | |
| Income | ||||
| Below $50K | 557 (50.0) | 176 (51.2) | 381 (49.5) | χ2(1) = 0.25 |
| $50K or above | 556 (50.0) | 168 (48.8) | 388 (50.5) | |
| Education | ||||
| Less than college deg. | 443 (39.8) | 128 (37.2) | 315 (41.0) | χ2(3) = 1.60 |
| 4-year college degree | 338 (30.4) | 107 (31.1) | 231 (30.0) | |
| Graduate degree | 332 (29.8) | 109 (31.7) | 223 (29.0) | |
| Chronotype | ||||
| Morning Type | 240 (21.6) | 62 (18.0) | 173 (23.1) | χ2(2) = 3.70 |
| Intermediate Type | 555 (49.9) | 180 (52.3) | 375 (48.8) | |
| Evening Type | 318 (28.6) | 102 (29.7) | 216 (28.1) | |
| M (SD) | M (SD) | M (SD) | ||
| Age (years) | 41.4 (13.6) | 38.3 (12.4) | 42.7 (13.9) | t(1111) = 5.04*** |
Note. CAS = condomless anal sex; SWC = sex with condoms. Within rows within variables, cells with different superscripts differ significantly.
p ≤ 0.001.
Timing of sex with a casual partner
Both among the full sample and the analytic sample of 344 men, the majority reported that their most recent CAS and SWC events with casual partners had occurred at night. As shown in the upper section of Table 2, of the 344 men with past-year CAS and SWC, more than two-thirds (68.6%) indicated that their last CAS event had occurred in the evening, night, or late night—most commonly from midnight onwards (25.9%), followed by 9pm-midnight (23.5%), and 5–9pm (19.2%). The remaining 31.4% of CAS events occurred during the 11-hour period during the day (6am-5pm). Bivariate analyses revealed that men who reported later times of last CAS (especially after midnight) were, on average, younger but did not differ by chronotype.
Table 2.
Bivariate Comparisons Between Chronotype and Age of Timing of Last CAS and SWC with Casual Partners
| Total | Daytime, 6am to 5pm |
Evening, 5–9pm |
From 9pm to midnight |
Midnight or later |
Test Statistic | |
|---|---|---|---|---|---|---|
| Last CAS with casual partner | n | n (%) | n (%) | n (%) | n (%) | |
| Overall | 344 | 108 (31.4) | 66 (19.2) | 81 (23.5) | 89 (25.9) | |
| Chronotype | ||||||
| Morning Type | 62 | 25 (40.3) | 15 (24.2) | 10 (16.1) | 12 (19.4) | χ2(6) = 10.20 |
| Intermediate Type | 180 | 55 (30.6) | 34 (18.9) | 49 (27.2) | 42 (23.3) | |
| Evening Type | 102 | 28 (27.5) | 17 (16.7) | 22 (21.6) | 35 (34.3) | |
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | ||
| Age (years) | 38.3 (12.4) | 40.7 (12.8)a | 41.1 (12.8)ab | 36.3 (11.5)bc | 35.1 (11.5)c | F(3,340) = 5.44** |
| Last SWC with casual partner | n | n (%) | n (%) | n (%) | n (%) | |
| Overall | 344 | 119 (34.6) | 65 (18.9) | 91 (26.5) | 69 (20.1) | |
| Chronotype | ||||||
| Morning Type | 62 | 30 (48.4)a | 10 (16.1) | 15 (24.2) | 7 (11.3)a | χ2(6) = 16.78** |
| Intermediate Type | 180 | 66 (36.7)b | 38 (21.1) | 42 (23.3) | 34 (18.9)b | |
| Evening Type | 102 | 23 (22.5)c | 17 (16.7) | 34 (33.3) | 28 (27.5)c | |
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | ||
| Age (years) | 38.3 (12.4) | 39.2 (12.4) | 39.0 (10.9) | 38.2 (12.6) | 36.2 (12.6) | F(3,340) = 0.97 |
Note. CAS = condomless anal sex; SWC = sex with condoms. Within rows within continuous variables, cells with different superscripts differ significantly. Within columns within categorical variables, different superscripts signify that proportions among groups differ significantly.
p ≤ 0.01.
The lower section of Table 2 shows the frequencies of timings for most recent event of SWC with a casual partner. Almost as many men (65.4%) reported that their most recent event of SWC had occurred at night as did those reporting on CAS—most commonly, between 9pm and midnight (26.5%), followed by midnight onwards (20.1%), and between 5–9pm (18.9%). In contrast to the CAS results above, bivariate analyses revealed that the frequencies of these timings of SWC differed by chronotype but not by age. A greater proportion of morning types (48.4%) reported SWC during the day than did those with an evening (22.5%) or intermediate (36.7%) chronotype. Only 11.3% of morning types reported that their most recent SWC occurred after midnight, whereas 19.4% had reported that their most recent CAS occurred after midnight. These distributions are depicted in Figure 1.
Figure 1.
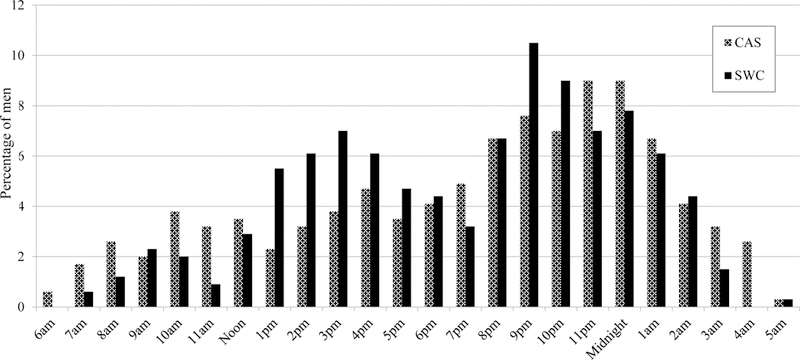
Percentage of men reporting times of last CAS and SWC with a casual partner, N = 344.
In multivariable analyses displayed in Table 3, younger age was significantly associated with greater odds of last CAS occurring from 9pm onwards (vs. during the day/evening), while chronotype was not, when adjusting for age and covariates. The addition of chronotype in the second step of the model for CAS did not improve model fit. Conversely chronotype, but not age, was significantly associated with odds of last SWC occurring from 9pm onwards (vs. during the day/evening). After adjusting for age and covariates, morning types were less likely to report that SWC occurred from 9pm onwards than were evening types. The addition of chronotype in the second step of the model for SWC did contribute significantly to improved model fit.
Table 3.
Logistic Regressions Predicting CAS and SWC from 9pm onwards (vs. Day/Evening), N = 344
| Step 1 | Step 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Time of Last CAS | B | AOR | p | 95% CI | B | AOR | p | 95% CI |
| Constant | 0.12 | 1.13 | 0.56 | −0.19 | 0.83 | 0.57 | ||
| Race and Ethnicity (ref. White) | ||||||||
| Men of Color | 0.17 | 1.19 | 0.50 | [0.73, 1.93] | 0.14 | 1.15 | 0.58 | [0.70, 1.88] |
| Relationship Status (ref. partnered) | ||||||||
| Single | −0.05 | 0.96 | 0.85 | [0.59, 1.54] | −0.03 | 0.97 | 0.91 | [0.60, 1.57] |
| Education (ref. < college degree) | ||||||||
| 4-year college degree | −0.33 | 0.72 | 0.23 | [0.42, 1.23] | −0.34 | 0.71 | 0.22 | [0.41, 1.23] |
| Graduate degree | −0.49 | 0.61 | 0.09 | [0.35, 1.08] | −0.48 | 0.62 | 0.10 | [0.35, 1.10] |
| Income (ref. less than $50K) | ||||||||
| $50K or more | 0.05 | 1.05 | 0.83 | [0.65, 1.70] | 0.05 | 1.05 | 0.83 | [0.65, 1.70] |
| Age | −0.03 | 0.97 | <0.001 | [0.95, 0.99] | −0.03 | 0.97 | <0.01 | [0.95, 0.99] |
| Chronotype (ref. Morning Type) | ||||||||
| Intermediate Type | 0.37 | 1.44 | 0.26 | [0.77, 2.71] | ||||
| Evening Type | 0.43 | 1.53 | 0.24 | [0.76, 3.09] | ||||
| Model Statistics: | Model χ2(6) = 19.39, p <0.01 | Step χ2(2) = 1.58, p = 0.45 | ||||||
| Hosmer & Lemeshow χ2(8) = 8.53, p = 0.38 | Hosmer & Lemeshow χ2(8) = 3.92, p = 0.87 | |||||||
| Time of Last SWC | B | AOR | p | 95% CI | B | AOR | p | 95% CI |
| Constant | −0.01 | 0.99 | 0.97 | −0.42 | 0.66 | 0.20 | ||
| Race and Ethnicity (ref. White) | ||||||||
| Men of Color | 0.15 | 1.16 | 0.56 | [0.71, 1.87] | 0.07 | 1.07 | 0.79 | [0.65, 1.75] |
| Relationship Status (ref. partnered) | ||||||||
| Single | −0.32 | 0.73 | 0.19 | [0.46, 1.17] | −0.30 | 0.74 | 0.22 | [0.46, 1.19] |
| Education (ref. < college degree) | ||||||||
| 4-year college degree | 0.22 | 1.25 | 0.42 | [0.73, 2.12] | 0.30 | 1.34 | 0.29 | [0.78, 2.31] |
| Graduate degree | 0.09 | 1.09 | 0.77 | [0.62, 1.91] | 0.13 | 1.14 | 0.65 | [0.65, 2.02] |
| Income (ref. less than $50K) | ||||||||
| $50K or more | −0.37 | 0.69 | 0.12 | [0.43, 1.11] | −0.36 | 0.70 | 0.14 | [0.43, 1.12] |
| Age | −0.01 | 0.99 | 0.44 | [0.98, 1.01] | 0.00 | 1.00 | 0.99 | [0.98, 1.02] |
| Chronotype (ref. Morning Type) | ||||||||
| Intermediate Type | 0.21 | 1.23 | 0.51 | [0.66, 2.32] | ||||
| Evening Type | 0.96 | 2.61 | <0.01 | [1.29, 5.27] | ||||
| Model Statistics: | Model χ2(6) = 7.47, p = 0.28 | Step χ2(2) = 10.57, p <0.01 | ||||||
| Hosmer & Lemeshow χ2(8) = 7.97, p = 0.44 | Hosmer & Lemeshow χ2(8) = 3.19, p = 0.92 | |||||||
Note. CAS = condomless anal sex; SWC = sex with condoms; AOR = adjusted odds ratio; CI = confidence interval; ref. = referent.
Comparing times of CAS and SWC against one’s usual time of feeling tired, 152 (44.2%) last had CAS with a casual partner at or later than their usual time of feeling tired—and this differed significantly by age, t(342) = −3.59, p < 0.001. Indeed, this was reported by 56.1% of GBM under 30 but by only 41.9% of men aged 30–49 and 31.4% of men aged 50 or older. These distributions are depicted in Figure 2. However, having last CAS at or later than one’s usual time of feeling tired did not vary by chronotype, χ2(2) = 3.29, p = 0.19. In a binary logistic regression, younger age significantly predicted having CAS at or later than one’s usual time of being tired (AOR = 0.97, p = 0.01), adjusting for chronotype (which was non-significant) and the covariates included in regressions above. In contrast, only 126 men (36.6%) last had SWC at or later than their usual time of feeling tired, and this did not differ significantly by age, t(342) = 1.03, p = 0.31. This was reported by 41.1% of GBM under 30, by 35.3% of men aged 30–49, and 32.9% of men aged 50 or older. This also did not differ by chronotype, χ2(2) = 0.38, p = 0.83. Neither age or chronotype were significant predictors in a regression adjusting for the above covariates.
Figure 2.
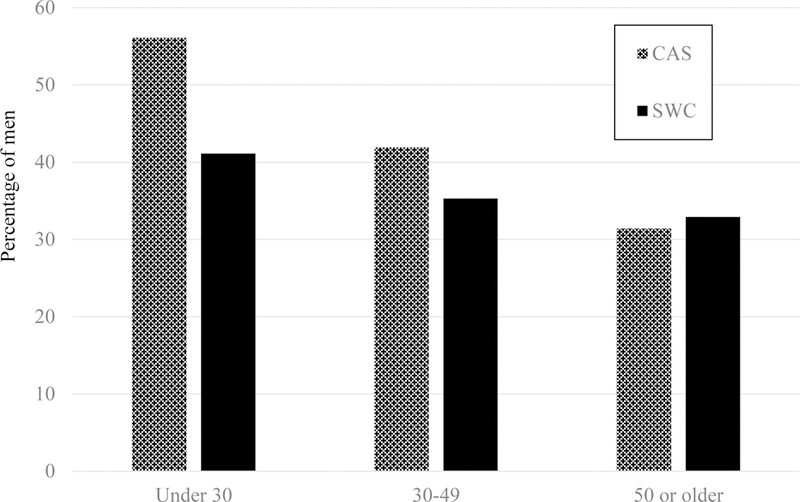
Percentage of men, separated by age, reporting last CAS and SWC with a casual partner at or later than their usual time of feeling tired, N = 344.
Tiredness and desire
Regarding the effect of tiredness on sexual desire, more than two-thirds (67.2%) of the 1113 men reported little (43.8%) or no (23.5%) reduction in sexual desire as a result of being tired. Less than one-third (32.8%) reported a substantial (27.5%) or complete (5.3%) reduction in desire. Further, as displayed in Table 4, 325 men (29.2%) indicated that being tired can increase their sexual desire. These 325 men were, on average, younger than those for whom tiredness does not increase desire. Indeed, 38.2% of GBM aged below 30 endorsed this statement, whereas only 28.2% of men aged 30–49 and 23.1% of men aged 50 or older did so. Endorsement of this statement did not differ according to chronotype or usual sexual positioning identity. In the upper section of Table 6, binary logistic regression showed that younger age predicted greater odds of reporting that being tired can increase sexual desire, adjusting for chronotype.
Table 4.
Bivariate Associations Between Age, Chronotype, and Sexual Position Identity with Whether Tiredness Increases Sexual Desire
| Total | Tiredness does not increase desire |
Tiredness can increase desire |
Test Statistic | |
|---|---|---|---|---|
| n | n (%) | n (%) | ||
| Overall | 1113 | 788 (70.8) | 325 (29.2) | |
| Chronotype | ||||
| Morning Type | 240 | 180 (75.0) | 60 (25.0) | χ2(2) = 5.76 |
| Intermediate Type | 555 | 398 (71.7) | 157 (28.3) | |
| Evening Type | 318 | 210 (66.0) | 108 (34.0) | |
| Sexual Position Identity | ||||
| Top | 221 | 167 (75.6) | 54 (24.4) | χ2(4) = 3.65 |
| Versatile/Top | 251 | 172 (68.5) | 79 (31.5) | |
| Versatile | 235 | 164 (69.8) | 71 (30.2) | |
| Versatile/Bottom | 261 | 186 (71.3) | 75 (28.7) | |
| Bottom | 145 | 99 (68.3) | 46 (31.7) | |
| M (SD) | M (SD) | M (SD) | ||
| Age (years) | 41.3 (13.6) | 42.4 (13.5) | 38.6 (13.5) | t(1111) = 4.28*** |
Note.
p < 0.001.
Table 6.
Logistic Regressions Predicting Whether Tiredness Increases Sexual Desire and Odds of Bottoming, N = 1113
| Step 1 | Step 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Sexual Desire: | B | AOR | P | 95% CI | B | AOR | p | 95% CI |
| Constant | −0.90 | 0.41 | <0.001 | −0.96 | 0.38 | <0.001 | ||
| Age | −0.02 | 0.98 | <0.001 | [0.97 0.99] | −0.02 | 0.98 | <0.001 | [0.97, 0.99] |
| Chronotype (ref. Morning Type) | ||||||||
| Intermediate Type | 0.02 | 1.00 | 0.99 | [0.70, 1.43] | ||||
| Evening Type | 0.19 | 1.21 | 0.34 | [0.82, 1.80] | ||||
| Model Statistics: | Model χ2(1) = 18.47, p <0.001 | Step χ2(2) = 1.70, p = 0.43 | ||||||
| Hosmer & Lemeshow χ2(8) = 15.65, p = 0.05 | Hosmer & Lemeshow χ2(8) = 8.40, p = 0.40 | |||||||
| Odds of Bottoming: | B | AOR | P | 95% CI | B | AOR | p | 95% CI |
| Constant | −1.06 | 0.35 | <0.001 | -3.26 | 0.04 | <0.001 | ||
| Age | −0.02 | 0.99 | <0.01 | [0.98 1.00] | -0.01 | 0.99 | 0.07 | [0.98, 1.00] |
| Positioning Identity (ref. Top) | ||||||||
| Top/Versatile | 1.94 | 6.93 | <0.001 | [3.21, 14.95] | ||||
| Versatile | 2.73 | 15.39 | <0.001 | [7.23, 32.73] | ||||
| Bottom/Versatile | 2.71 | 15.01 | <0.001 | [7.08, 31.81] | ||||
| Bottom | 2.39 | 10.90 | <0.001 | [4.94, 24.06] | ||||
| Model χ2(1) = 9.20, p <0.01 | Step χ2(4) = 109.86, p <0.001 | |||||||
| Hosmer & Lemeshow χ2(8) = 8.79, p = 0.36 | Hosmer & Lemeshow χ2(8) = 8.66, p = 0.37 | |||||||
Note. AOR = adjusted odds ratio; CI = confidence interval; ref. = referent
Tiredness and sexual positioning
As displayed in Table 5, more than one-quarter (26.0%) of the 1113 men reported that being tired would make them more likely to be the receptive partner or the “bottom” in anal sex. This was more commonly reported by younger GBM—indeed, more than one-third (33.5%) of men aged below 30 endorsed this option whereas only 24.4% of men aged 30–49 and 22.1% of men aged 50 or older did so. No differences were observed according to chronotype—however, differences did emerge depending on sexual positioning identity. A greater proportion of those reporting a versatile positioning identity (37.4%) indicated that being tired would make them more likely to bottom, compared to those who identify as the insertive partner or “the top” in anal sex (3.6%) and those who identify as a “versatile/top” (21.1%). As displayed in Table 6, binary logistic regression analyses showed that younger age predicted greater odds that tiredness increases bottoming (compared to the other two responses combined), when entered in the first step of the model. The addition of sexual positioning identity in the second step of the analysis substantially improved model fit.
Table 5.
Bivariate Associations Between Age, Chronotype, and Sexual Position Identity with the Effect of Tiredness on Sexual Positioning
| Total | Would not change |
More likely to top |
More likely to bottom |
Test Statistic | |
|---|---|---|---|---|---|
| n | n (%) | n (%) | n (%) | ||
| Overall | 1113 | 757 (68.0) | 67 (6.0) | 289 (26.0) | |
| Chronotype | |||||
| Morning Type | 240 | 174 (72.5) | 8 (3.3) | 58 (24.2) | χ2(4) = 5.67 |
| Intermediate Type | 555 | 374 (67.4) | 39 (7.0) | 142 (25.6) | |
| Evening Type | 318 | 209 (65.7) | 20 (6.3) | 89 (28.0) | |
| Sexual Position Identity | |||||
| Top | 221 | 197 (89.1) | 16 (7.2) | 8 (3.6)a | χ2(8) = 107.14*** |
| Versatile/Top | 251 | 176 (70.1) | 22 (8.8) | 53 (21.1)b | |
| Versatile | 235 | 131 (55.7) | 16 (6.8) | 88 (37.4)c | |
| Versatile/Bottom | 261 | 151 (57.9) | 13 (5.0) | 97 (37.2)c | |
| Bottom | 145 | 102 (70.3) | 0 (0) | 43 (29.7)bc | |
| M (SD) | M (SD) | M (SD) | M (SD) | ||
| Age (years) | 41.3 (13.6) | 42.5 (13.4)a | 37.5 (14.4)b | 39.3 (13.6)b | F(2,1110) = 8.67*** |
Note. Within the ‘more likely to bottom’ column within variables, different superscripts signify that proportions among groups differ significantly. Within rows within continuous variables, cells with different superscripts differ significantly
p < 0.001.
Discussion
Tiredness has been implicated elsewhere in a range of adverse health outcomes (related to lapsed self-regulation in eating, exercise, substance use, smoking, and injury), such that insufficient sleep has been declared a “public health epidemic” (CDC, 2015). Our findings have provided preliminary, yet compelling, evidence highlighting three reasons why tiredness should be considered an important factor in relation to sexual behavior—here among GBM, but potentially among other populations as well. First, we showed that two-thirds of recent anal sex events with casual partners (whether without or with condoms) occurred at night, and frequently late at night, in a national sample of GBM. Later times for sex with casual partners were more commonly reported by younger GBM and by evening types—however, a substantial number of morning types also reported that their most recent event had occurred late at night, when they are generally expected to be experiencing substantial levels of tiredness. We also found that CAS more often occurred at or later than the individual’s usual time for becoming tired than did SWC (44.2% vs. 36.6%), and more commonly so among younger GBM (56.1% vs. 41.1%). Drawing particular emphasis to the latter statistic: more than half of GBM under 30 reported that their most recent event of CAS with a causal partner occurred at or later at night than their usual time of feeling tired—and substantially fewer of these men reported that SWC did so.
These findings that sex—especially CAS—with casual partners most often occurs late in one’s waking day become particularly important when considered alongside the findings of our final two aims. We found that, for many GBM, tiredness does not substantially diminish the desire for sex and can actually increase desire, especially among younger GBM. Furthermore, we found that, for many GBM, tiredness increases their odds of being the receptive partner in anal sex, especially among younger GBM and among those with a versatile positioning identity.
It should be noted that men in our sample with an evening chronotype were significantly younger than those with an earlier chronotype, which is consistent with chronobiology research showing that younger men tend to have later chronotypes than older men (Duarte et al., 2014; Randler, 2016; Roenneberg et al., 2007). However, in terms of timing of sex with casual partners, our analyses showed that the influence of chronotype only persisted when adjusting for age in relation to SWC, and not CAS. In combination with the finding that CAS more often occurred at or later than an individual’s usual time of feeling tired, this suggests that CAS with casual partners may be an act that tends to be more affected by the mismatch with men’s circadian preference, at least more so than SWC. In other words, tiredness from circadian misalignment may have played some role in the level of risk in the given event, however the current study design cannot confirm this. This is generally in line with circadian misalignment research in fields outside of sex (e.g., Curtis et al., 2014), whereby people tend to make better decisions in their optimal time or “circadian peak” vs their off-time or “circadian trough.”
Contrary to the common-sense assumption that being tired diminishes desire for sex, we found that, for many men, undiminished or increased levels of sexual desire can be experienced at the same time as tiredness, and more commonly among younger GBM. This has implications for GBM and anal sex, given the potential in male-male sex for each partner to switch positioning according to fluctuations in energy and effort. This potential, insofar as it relates to risk for HIV and STI infection, is not a feature typically shared by heterosexual or female-female sexual contact. Our finding that tiredness can situationally heighten a GBM’s risk for HIV infection via sexual positioning decisions further highlights the need for sexual health researchers to consider tiredness and poor sleep health as important factors in HIV and STI prevention for GBM.
This study is among the first to connect two aspects of the human experience that are not often considered together: tiredness and sex. To our knowledge, ours is the first attempt to gather data on when GBM have sex with casual partners, and is also the first study about timing of sex to differentiate between sex with and without condoms more generally. The only study that has explored timing of sex-related activity among GBM, although not actual sex per se, is Goedel and Duncan’s (2015) study of peak usage of a sexual networking app on which 75% of GBM were most often active late at night or in the evening. This is consistent with our findings that almost 70% of our GBM reported that recent casual sex occurred at night. Our findings regarding GBM also roughly accord with the few studies that have looked at timing of sex among heterosexuals (Barak et al., 1997; Jankowski et al., 2014; Palmer et al., 1982; Refinetti, 2005), providing further evidence that sex can be generally considered a “nighttime” activity. We are aware of only one other sleep-related study of GBM (Duncan et al., 2016), in which both poorer overall sleep quality and shorter average sleep duration were positively associated with having CAS with a greater number of recent partners—and notably, the association was stronger for receptive CAS, which aligns with our findings about tiredness influencing sexual positioning.
In sum, this is important given what is known from the sleep science literature about the impairing effects of tiredness and/or continued wakefulness on cognition, emotion, and risk-taking (see Womack et al., 2013 for review), and is in line with a dual processes view of self-regulation, as tiredness can increase sexual desire at the same time as decreasing the self-regulatory capacities involved in managing or minimizing attendant risks. Our findings resonate with other studies showing that lapses in self-regulation commonly occur at night in other health behaviors such as dieting (Forman et al., 2017; McKee, Ntoumanis, & Taylor, 2014) and trying to quit smoking (Fillo, Alfano, Paulus, & Baird, 2016). One implication of our findings is that, in order to maximize ecological validity, future lab-based research on sexual response and decision-making (e.g., the effects of arousal on behavior) should be conducted at times of day or in states of tiredness that more closely match the real-world conditions in which sexual decisions are commonly being made. Our findings also highlight the need for studies utilizing intensive longitudinal assessment, such as daily diaries, to gather details on time of day when sexual activity begins and on levels of concomitant tiredness, antecedent sleep quality, and co-occurring substance use, in order to better capture person-by-situation interactions regarding sex (Cooper, 2010; Rendina, 2015). Finally, research could also explore indirect pathways from tiredness to sexual behavior via intervening factors such as impaired emotion regulation or increased negative affect.
In terms of interventions, efforts to increase people’s awareness of their sleep health and of how tiredness may impair their decision-making regarding sex could help to increase self-efficacy and minimize adverse outcomes of risky sexual behavior. Interventions for younger adults and adolescents, via sex education programs and HIV prevention efforts regarding sleep health and its benefits, could be particularly well-timed in a developmental sense if delivered during this vulnerable life-stage. Such psychoeducation could be delivered in cost-effective, engaging, and wide-reaching ways using internet and mobile technologies, in a public health campaign. Further, for people with more problematic patterns of sexual behavior, more personalized intervention could be delivered in one-on-one counselling. Addressing sleep health in a discrete module within existing counselling interventions—whether within a cognitive-behavioral therapy (CBT) approach, a mindfulness approach, or a motivational interviewing approach—could be especially beneficial to those for whom tiredness is particularly debilitating and/or prevalent in their daily lives.
Among the limitations of this largely exploratory work is the issue of the generalizability of our cohort of HIV-negative GBM participating in online research, having residential stability and relatively high levels of education and income. Also, the day of the week when last CAS or SWC occurred was not reliably established and may be influential, especially for people who become tired later on a weekend night than they do on a weeknight. Further, our originally-derived questions about sexual desire and positioning behavior did not actually ask about implications for their condom use, or whether responses would differ for sex with main vs. casual partners. Future studies could explore whether tiredness affects GBM’s attitudes and self-efficacy regarding condom use and/or use of other risk reduction strategies. The item regarding desire included reference to both sexual desire and sexual arousal, and future research should consider exploring these two constructs separately. Our questions also did not ask about antecedent or concurrent substance use with sex when tired, or whether the lateness of the sex event/s was enabled by substance use. More detailed information on lifestyle factors for these men might be relevant, such as whether they are shift-workers or live by nocturnal schedules, and could be more precisely gleaned by use of ecological momentary assessment (e.g., daily diaries or activity monitoring). Further, the relationship status item may not have covered the full 12-month period assessed. Finally, the classification of sexual risk here did not account for the individual’s PrEP status nor the HIV status of the casual partner with respect to viral load detectability or PrEP usage. Finally, we did not assess for clinical sleep problems or other physical conditions which may be associated with reduced sexual activity (e.g., Allen & Desille, 2017; Budweiser et al., 2009; Lin et al., 2015).
Conclusions
Previous research has identified other sources (e.g., alcohol, drugs, sexual arousal, strong negative affect) that can situationally impair self-regulation in relation to sex. Our findings have highlighted tiredness as an additional factor that warrants similar attention in the sexual health literature, by exploring some of the contexts (e.g., mostly nighttime, and often at or later than one’s usual time of feeling tired) and motivators (e.g., undiminished or increased desire, and increased odds of receptive positioning) involved in the sexual behaviors of many GBM. It is especially concerning for younger GBM that tiredness may increase sexual desire as well as odds of riskier positioning in anal sex, given that younger adults in general tend to have poorer sleep health in general (Brown, Buboltz Jr, & Soper, 2002) and also that younger GBM are at elevated risk for HIV infection (CDC, 2016). Additionally, similar dynamics regarding the effects of tiredness on substance use behavior could also be influential in combination with sex occurring at night (e.g., Millar et al., 2018). Accordingly, future research should explore connections between tiredness, sex, and the use of alcohol and drugs before and/or during sex when feeling tired. Interventions should aim to increase the individual’s self-awareness of how their tiredness might be affecting their sexual decision-making, and may also target related outcomes such as medication adherence (whether HIV medication for HIV-positive men or PrEP for HIV-negative men), emotion regulation strategies, and substance use reduction. Our findings indicate the need for future research to further explore the role of tiredness in sexual behaviors in order to improve overall health in GBM and in other populations.
ACKNOWLEDGEMENTS:
The authors would like to acknowledge the contributions of the other members of the One Thousand Strong Study Team (Dr. Christian Grov, Demetria Cain, Mark Pawson, Ruben Jimenez, Chloe Mirzayi, Raymond Moody, and Thomas Whitfield) and other staff from the Center for HIV/AIDS Educational Studies and Training (Chris Hietikko, Brian Salfas, Kendell Doyle, and Carlos Ponton). Thank you to Dr. Cheryl Carmichael and Dr. Dustin Duncan. We would also like to thank the staff at Community Marketing Inc (David Paisley, Heather Torch, and Thomas Roth). Finally, we thank Jeffrey Schulden at NIDA and all of our participants in the One Thousand Strong study.
FUNDING: The One Thousand Strong study was funded by a research grant from the National Institute on Drug Abuse (R01 DA036466: Jeffrey T. Parsons & Christian Grov, MPIs). H. Jonathon Rendina was funded in part by a Career Development Award from the National Institute on Drug Abuse (K01-DA039030; H. Jonathon Rendina, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
CONFLICT OF INTEREST: The authors declare that they have no conflicts of interest.
References
- Adan A, & Almirall H (1991). Horne & Östberg morningness-eveningness questionnaire: A reduced scale. Personality and Individual Differences, 12(3), 241–253. [Google Scholar]
- Adan A, Archer SN, Hidalgo MP, Di Milia L, Natale V, & Randler C (2012). Circadian typology: A comprehensive review. Chronobiology International, 29(9), 1153–1175. [DOI] [PubMed] [Google Scholar]
- Allen MS, & Desille AE (2017). Health-related lifestyle factors and sexual functioning and behavior in older adults. International Journal of Sexual Health, 29(3), 273–277. [Google Scholar]
- Barak Y, Stein D, Ring A, Ticher A, & Elizur A (1997). Patterns of first intercourse: A survey among Israeli women. Biological Rhythm Research, 28(1), 36–41. [Google Scholar]
- Barber LK (2014). Conceptualizations of sleep in stress theory: Exciting new directions. Stress and Health, 30(5), 431–432. [DOI] [PubMed] [Google Scholar]
- Brown FC, Buboltz WC Jr, & Soper B (2002). Relationship of sleep hygiene awareness, sleep hygiene practices, and sleep quality in university students. Behavioral Medicine, 28(1), 33–38. [DOI] [PubMed] [Google Scholar]
- Budweiser S, Enderlein S, Jörres RA, Hitzl AP, Wieland WF, Pfeifer M, & Arzt M (2009). Men’s sexual health: Sleep apnea is an independent correlate of erectile and sexual dysfunction. The Journal of Sexual Medicine, 6(11), 3147–3157. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2012). HIV transmission risk, 2012 Available at: http://www.cdc.gov/hiv/law/pdf/Hivtranmsmision.pdf. Published July 2012. Accessed May 1, 2016.
- Centers for Disease Control and Prevention (2015). Insufficient sleep is a public health epidemic Available at: https://www.cdc.gov/features/dssleep/index.html. Published September 2015. Accessed June 1, 2017.
- Centers for Disease Control and Prevention (2016). HIV Surveillance Report, 2015; vol. 27 Available at http://www.cdc.gov/hiv/library/reports/surveillance/html. Published November 2016. Accessed 15 June 2017.
- Cooper ML (2010). Toward a person×situation model of sexual risk-taking behaviors: Illuminating the conditional effects of traits across sexual situations and relationship contexts. Journal of Personality and Social Psychology, 98(2), 319–341. [DOI] [PubMed] [Google Scholar]
- Costa RM, & Oliveira TF (2016). Poorer subjective sleep quality is related to higher fantasy-induced sexual arousal in women of reproductive age. Journal of Sex & Marital Therapy, 42(8), 740–748. [DOI] [PubMed] [Google Scholar]
- Curtis J, Burkley E, & Burkley M (2014). The rhythm is gonna get you: The influence of circadian rhythm synchrony on self-control outcomes. Social and Personality Psychology Compass, 8(11), 609–625. [Google Scholar]
- Duarte LL, Menna-Barreto L, Miguel MAL, Louzada F, Araújo J, Alam M, … & Pedrazzoli M (2014). Chronotype ontogeny related to gender. Brazilian Journal of Medical and Biological Research, 47(4), 316–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan DT, Goedel WC, Mayer KH, Safren SA, Palamar JJ, Hagen D, & Jean-Louis G (2016). Poor sleep health and its association with mental health, substance use, and condomless anal intercourse among gay, bisexual, and other men who have sex with men. Sleep Health, 2(4), 316–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durmer JS, & Dinges DF (2005). Neurocognitive consequences of sleep deprivation. Seminars in Neurology, 25(1), 117–129. [DOI] [PubMed] [Google Scholar]
- Engle-Friedman M, Riela S, Golan R, Ventuneac AM, Davis CM, Jefferson AD, & Major D (2003). The effect of sleep loss on next day effort. Journal of Sleep Research, 12(2), 113–124. [DOI] [PubMed] [Google Scholar]
- Engle-Friedman M (2014). The effects of sleep loss on capacity and effort. Sleep Science, 7(4), 213–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fillo J, Alfano CA, Paulus DJ, Smits JA, Davis ML, Rosenfield D,…Baird SO (2016). Emotion dysregulation explains relations between sleep disturbance and smoking quit-related cognition and behaviour. Addictive Behaviors, 57, 6–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman EM, Schumacher LM, Crosby R, Manasse SM, Goldstein SP, Butryn ML, … & Thomas JG (2017). Ecological momentary assessment of dietary lapses across behavioral weight loss treatment: Characteristics, predictors, and relationships with weight change. Annals of Behavioral Medicine, 1–13. [DOI] [PMC free article] [PubMed]
- Goedel WC, & Duncan DT (2015). Geosocial-networking app usage patterns of gay, bisexual, and other men who have sex with men: Survey among users of Grindr, a mobile dating app. JMIR, Public Health & Surveillance, 1(1), e4–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greer SM, Goldstein AN, & Walker MP (2013). The impact of sleep deprivation on food desire in the human brain. Nature Communications, 4(1), ncomms3259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Cain D, Whitfield TH, Rendina HJ, Pawson M, Ventuneac A, & Parsons JT (2016). Recruiting a US national sample of HIV-negative gay and bisexual men to complete at-home self-administered HIV/STI testing and surveys: Challenges and opportunities. Sexuality Research and Social Policy, 13(1), 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunia BC, Barnes CM, & Sah S (2014). The morality of larks and owls: Unethical behavior depends on chronotype as well as time of day. Psychological Science, 25(12), 2272–2274. [DOI] [PubMed] [Google Scholar]
- Hagger MS (2014). Where does sleep fit in models of self-control and health behaviour. Stress Health, 30, 425–30. [DOI] [PubMed] [Google Scholar]
- Horne JA, & Östberg O (1975). A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. International Journal of Chronobiology, 4(2), 97–110. [PubMed] [Google Scholar]
- Jankowski KS, Díaz-Morales JF, & Randler C (2014). Chronotype, gender, and time for sex. Chronobiology International, 31(8), 911–916. [DOI] [PubMed] [Google Scholar]
- Kahn M, Sheppes G, & Sadeh A (2013). Sleep and emotions: Bidirectional links and underlying mechanisms. International Journal of Psychophysiology, 89(2), 218–228. [DOI] [PubMed] [Google Scholar]
- Kling JM, Manson JE, Naughton MJ, Temkit MH, Sullivan SD, Gower EW, … & Crandall CJ (2017). Association of sleep disturbance and sexual function in postmenopausal women. Menopause, 24(6), 604–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin HH, Ho FM, Chen YF, Tseng CM, Ho CC, & Chung WS (2015). Increased risk of erectile dysfunction among patients with sleep disorders: A nationwide population‐based cohort study. International Journal of Clinical Practice, 69(8), 846–852. [DOI] [PubMed] [Google Scholar]
- Lyons A, Pitts M, Smith G, Grierson J, Smith A, McNally S, & Couch M (2011). Versatility and HIV vulnerability: Investigating the proportion of Australian gay men having both insertive and receptive anal intercourse. The Journal of Sexual Medicine, 8(8), 2164–2171. [DOI] [PubMed] [Google Scholar]
- Manly T, Lewis GH, Robertson IH, Watson PC, & Datta AK (2002). Coffee in the cornflakes: Time-of-day as a modulator of executive response control. Neuropsychologia, 40(1), 1–6. [DOI] [PubMed] [Google Scholar]
- McKee HC, Ntoumanis N, & Taylor IM (2014). An ecological momentary assessment of lapse occurrences in dieters. Annals of Behavioral Medicine, 48(3), 300–310. [DOI] [PubMed] [Google Scholar]
- McKnight-Eily LR, Eaton DK, Lowry R, Croft JB, Presley-Cantrell L, & Perry GS (2011). Relationships between hours of sleep and health-risk behaviors in US adolescent students. Preventive Medicine, 53(4), 271–273. [DOI] [PubMed] [Google Scholar]
- Metcalfe J, & Mischel W (1999). A hot/cool system analysis of delay of gratification: Dynamics of willpower. Psychological Review, 106, 3–19. [DOI] [PubMed] [Google Scholar]
- Millar BM (2017). Clocking self-regulation: Why time of day matters for health psychology. Health Psychology Review, 11(4), 345–357. [DOI] [PubMed] [Google Scholar]
- Millar BM, Rendina HJ, Starks TJ, Grov C, & Parsons JT (2018). The role of chronotype, circadian misalignment, and tiredness in the substance use behaviors of gay and bisexual men. Psychology of Sexual Orientation and Gender Diversity, online first. [DOI] [PMC free article] [PubMed]
- Palmer CA, & Alfano CA (2017). Sleep and emotion regulation: An organizing, integrative review. Sleep Medicine Reviews, 31, 6–16. [DOI] [PubMed] [Google Scholar]
- Palmer JD, Udry JR, & Morris NM (1982). Diurnal and weekly, but no lunar rhythms in human copulation. Human Biology, 54(1), 111–121. [PubMed] [Google Scholar]
- Pejovic S, Vgontzas AN, Basta M, Tsaoussoglou M, Zoumakis E, Vgontzas A, … & Chrousos GP (2010). Leptin and hunger levels in young healthy adults after one night of sleep loss. Journal of Sleep Research, 19(4), 552–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perogamvros L, & Schwartz S (2015). Sleep and emotional functions. Current Topics in Behavioral Neurosciences, 25, 411–431. [DOI] [PubMed] [Google Scholar]
- Randler C (2016). Ontogeny of morningness–eveningness across the adult human lifespan. The Science of Nature, 103(1–2), 3–6. [DOI] [PubMed] [Google Scholar]
- Randler C, Jankowski KS, Rahafar A, & Díaz-Morales JF (2016). Sociosexuality, morningness–eveningness, and sleep duration. SAGE Open, 6(1), 1–8. [Google Scholar]
- Refinetti R (2005). Time for sex: Nycthemeral distribution of human sexual behavior. Journal of Circadian Rhythms, 3(1), 4–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendina HJ (2015). When parsimony is not enough: Considering dual processes and dual levels of influence in sexual decision making. Archives of Sexual Behavior, 44(7), 1937–1947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roenneberg T, Kuehnle T, Juda M, Kantermann T, Allebrandt K, Gordijn M, & Merrow M (2007). Epidemiology of the human circadian clock. Sleep Medicine Reviews, 11(6), 429–438. [DOI] [PubMed] [Google Scholar]
- Schmidt C, Collette F, Cajochen C, & Peigneux P (2007). A time to think: Circadian rhythms in human cognition. Cognitive Neuropsychology, 24(7), 755–789. [DOI] [PubMed] [Google Scholar]
- Terre L (2014). Clinical implications of impaired sleep. American Journal of Lifestyle Medicine, 8(6), 352–370. [Google Scholar]
- Van der Helm E, & Walker MP (2012). Sleep and affective brain regulation. Social and Personality Psychology Compass, 6(11), 773–791. [Google Scholar]
- Venkatraman V, Chuah YL, Huettel SA, & Chee MW (2007). Sleep deprivation elevates expectation of gains and attenuates response to losses following risky decisions. Sleep, 30(5), 603–609. [DOI] [PubMed] [Google Scholar]
- Watson D, Wiese D, Vaidya J, & Tellegen A (1999). The two general activation systems of affect: Structural findings, evolutionary considerations, and psychobiological evidence. Journal of Personality and Social Psychology, 76(5), 820–838. [Google Scholar]
- Womack SD, Hook JN, Reyna SH, & Ramos M (2013). Sleep loss and risk-taking behavior: A review of the literature. Behavioral Sleep Medicine, 11(5), 343–359. [DOI] [PubMed] [Google Scholar]
- Zarcone V, De La Pena A, & Dement WC (1974). Heightened sexual interest and sleep disturbance. Perceptual and Motor Skills, 39(3), 1135–1141. [Google Scholar]


