Abstract
Insecure attachment is a predisposing risk factor for the development of Functional Neurological Disorder (FND). Limited research has been conducted investigating connections between attachment styles, other predisposing vulnerabilities and symptom severity in patients with motor FND. Using a within-group design with prospective data collection, we performed univariate tests followed by multivariate linear regressions to investigate neuropsychiatric factors associated with four attachment styles (secure, fearful, pre-occupied, and dismissing) in 56 patients with motor FND (mean age 40.2±13.0; 41 women, 15 men). In univariate analyses, fearful attachment style was associated with self-reported adverse life event burden, alexithymia, dissociation, depression, anxiety, impaired stress coping, functional neurologic symptom severity and marital status. In a multivariate stepwise linear regression analysis, childhood abuse, alexithymia, depression and not being married independently predicted fearful attachment. In a post-hoc analysis, childhood sexual and emotional abuse were each independently associated with fearful attachment tendencies. There were no independent predictors of secure, preoccupied or dismissing attachment styles in this study population. Future studies with larger cohorts are needed to investigate nuanced relationships among predisposing vulnerabilities for the development of FND, as well as potential links between risk factors, functional neurologic symptom severity and clinical outcomes.
Keywords: conversion disorder, psychogenic nonepileptic seizures, functional movement disorders, attachment styles
Introduction
Interpersonal conflicts and other relational difficulties are important predisposing vulnerabilities or perpetuating factors affecting patients with Functional Neurological Disorder (FND, a.k.a. Conversion Disorder), a common neuropsychiatric condition characterized by unexplained limb weakness, gait difficulties, non-epileptic seizures, abnormal movements, and/or sensory deficits{1-3}. According to attachment theory, interpersonal difficulties may arise throughout the lifespan in part from insecure attachment tendencies based on childhood maltreatment and poor caregiver relationships{1}. While individuals with secure attachment generally enjoy more consistent nurturance in childhood and exhibit a positive view of the self and others{4, 5}, adults with insecure attachment experience interpersonal challenges. Those with dismissing attachment are thought to have had early childhood experiences marked by emotionally unresponsive caregiving, resulting in overcompensated self-reliance combined with discomfort in closeness to others{1, 4}. Adults with preoccupied attachment are more likely to have had inconsistently responsive caregiving, resulting in over-vigilance, poor self-esteem, and a dependence on the approval of others{6, 7}. Fearfully attached individuals often experience affectionless, critical, and rejecting caregiving, thus leaving them with a negative view of the self and others. Adults with a fearful attachment crave social attachments, but are frequently stymied by their fears of intimacy and rejection, resulting in an urge to flee{8}. Although insecure attachment styles have been linked to somatization and emotional dysregulation{7, 9}, few studies in FND populations have examined neuropsychiatric factors associated with attachment styles, which are also important considerations affecting doctor-patient encounters{8}.
While two studies found no differences in attachment styles between patients with epilepsy and those with psychogenic non-epileptic seizures (PNES, a.k.a. dissociative seizures){10, 11}, another revealed higher levels of fearful attachment in individuals with PNES{12}. In the latter study, abuse and neglect correlated with insecure attachment{12}. Furthermore, in patients with PNES, depression and anxiety have been linked to avoidant/anxious attachment styles, relationship conflicts and lack of relationship depth, indicating a role for attachment in the development of concurrent psychopathology{11}. In pediatric FND populations, distinct attachment styles may be linked to specific symptom profiles, implying an interplay between relationship difficulties and functional neurological symptoms{13}. The heterogeneity of group-level differences also highlights the importance of considering individual differences in FND populations using a neurobio-psycho-social perspective{14, 15}. Additionally, very few studies have investigated attachment styles in other motor FND sub-populations, such as functional movement disorders (FMD) or functional weakness.
In this prospective cohort study, we used a within-group design to investigate relationships between attachment styles, demographic variables, motor subtypes, and other neuropsychiatric factors, including self-reported symptom severity, adverse life event burden, affective symptoms, resilience, and personality dimensions in 56 patients with motor FND. We hypothesized that insecure attachment styles would relate to functional neurological symptom severity and several predisposing vulnerabilities for the development of FND including trauma burden, affective symptoms, maladaptive personality traits, and impaired stress coping.
Methods
56 patients with motor FND (mean age=40.2±13.0; 41 women, 15 men; illness duration=3.3±3.7 years) were recruited from the Massachusetts General Hospital FND Clinic{16}. Patients met criteria for clinically-established functional movement disorders (n=29), psychogenic non-epileptic seizures (21 documented; 1 clinically-established; 2 probable), and/or functional limb weakness (20 with positive exam findings, 1 with probable paroxysmal functional weakness based on history and longitudinal follow-up). 17 of 56 had mixed-motor FND, 16 also showed functional speech symptoms, and 12 exhibited splitting-of-the-midline sensory deficits (See Supplemental Table 1). Patients with major neurologic comorbidities (n=7) and/or co-morbid epileptic seizures (n=4) were also included. Exclusion criteria included illiteracy, history of mania/psychosis, active suicidality, and current illicit drug abuse or alcohol dependence. Subjects provided written informed consent as approved by the Institutional Review Board of Partners HealthCare.
All subjects completed the Relationship Scales Questionnaire (RSQ){5} as the primary study measure. In addition, self-report measures characterizing functional neurologic symptom severity and the spectrum of common predisposing vulnerabilities and perpetuating factors were also obtained: Patient Health Questionnaire-15 (PHQ-15){17}, Screening for Somatoform Symptoms Conversion Disorder Subscale (SOMS:CD){18}, Dissociative Experience Scale (DES){19}, Somatoform Dissociation Questionnaire-20 (SDQ-20){20}, Short Form Health Survey (SF-36){21}, Beck Depression Inventory-II (BDI){22}, Spielberger State-Trait Anxiety Inventory (STAI-T){23}, NEO Five-Factor Inventory-3 (NEO){24}, Toronto Alexithymia Scale (TAS){25}, Barrett Impulsivity Scale (BIS){26}, Connor-Davidson Resilience Scale (CD-RISC){27}, Childhood Trauma Questionnaire (CTQ){28}, Life Events Checklist-5 (LEC){29}, and Post-traumatic Stress Disorder (PTSD) Checklist-5 (PTSD-CL5){30}. All individuals also underwent a Structured Clinical Interview for DSM-IV-TR Axis I Disorders (SCID).
The RSQ is a 30-item continuous measure of attachment with four established dimensions: secure, fearful, dismissing, and preoccupied{5}. The PHQ-15 and the SOMS:CD denote functional neurological symptom severity. The DES and SDQ-20 are measures of psychological and somatoform dissociation, respectively. The SF-36 assesses mental and physical health status. The STAI-T, BDI, and PTSD-CL5 scales record state-trait anxiety, depression, and PTSD symptom severity, respectively. The TAS evaluates alexithymia, and the NEO assesses five validated personality dimensions. To measure childhood/adolescent and lifetime trauma burden, the CTQ and LEC-5 “happened to me” indices were used. Lastly, the CD-RISC and BIS evaluate resilience and impulsivity, respectively.
Dependent variables included RSQ sub-scores for secure, fearful, dismissing, and preoccupied attachment styles. Pearson correlations for continuous variables and independent sample two-tailed t-tests for dichotomous variables were performed for univariate screenings. Clinical and psychometric variables that showed a statistically significant relationship with any of the RSQ sub-scores (p < 0.05) were entered into separate multivariate linear regression analyses. For any regression models demonstrating collinearity (tolerance < 0.20), automated stepwise linear regressions were performed. All analyses were performed in IBM SPSSv23 (Chicago).
Results
In univariate tests, secure attachment positively correlated with NEO-extraversion (r=0.47, p<0.001), SF-36 mental health (r=0.30, p=0.03), FMD subtype (t=2.27, p=0.03) and CD-RISC scores (r=0.47, p<0.001); secure attachment negatively correlated with NEO-neuroticism (r=−0.44, p=0.001), TAS (r=−0.47, p<0.001), STAI-T (r=−0.42, p=0.001), and PTSD-CL5 (r=−0.30, p=0.03) scores (See Supplemental Table 2). In a multivariate linear regression analysis, there were no statistically significant variables independently associated with secure attachment.
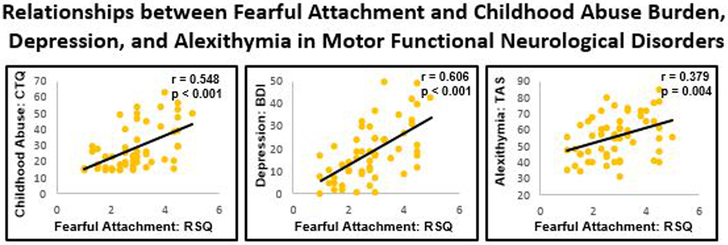
Fearful attachment positively correlated with PHQ-15 (r=0.35, p=0.009), SDQ-20 (r=0.43, p=0.001), DES (r=0.57, p<0.001), LEC ‘happened to me’ (r=0.37, p=0.005), CTQ-abuse (r=0.55, p<0.001), CTQ-neglect (r=0.34, p=0.01), TAS (r=0.38, p=0.004), BDI (r=0.61, p<0.001), STAI-T (r=0.56, p<0.001), PTSD-CL5 (r=0.49, p<0.001), PCS (r=0.51, p<0.001), and NEO-neuroticism (r=0.48, p<0.001) scores. Additionally, fearful attachment negatively correlated with being married (t=−2.09, p=0.04), NEO-extraversion (r=−0.40, p=0.003), CD-RISC (r=−0.30, p=0.03), and SF-36 mental health (r=−0.48, p<0.001) scores. Collinearity testing, as measured by tolerance scores less than 0.20, showed that STAI-T was collinear with several psychometric variables. Therefore, we performed an automated stepwise linear regression using all statistically significant univariate variables, which identified CTQ-abuse (standardized beta=0.39, p<0.001), BDI (standardized beta=0.39, p<0.001), TAS (standardized beta=0.22, p=0.03), and not being married (standardized beta=−0.25, p=0.009) to be significantly associated with fearful attachment (See Figure 1 and Table 1). This model explained 60.9% of the variance in fearful attachment style scores.
Figure 1. Scatterplots of the associations between fearful attachment (RSQ), childhood trauma, depression, and alexithymia in motor functional neurological disorders.
RSQ, Relationship Scales Questionnaire; FND, Functional Neurological Disorder; CTQ, Childhood Trauma Questionnaire; BDI-II, Beck Depression Inventory-II; TAS, Toronto Alexithymia Score.
Table 1. Stepwise linear regression predictors of fearful attachment (RSQ) in motor functional neurological disorders.
RSQ, Relationship Scales Questionnaire; FND, Functional Neurological Disorder; CTQ, Childhood Trauma Questionnaire; BDI-II, Beck Depression Inventory-II; TAS, Toronto Alexithymia Score.
| Independent Variables | Standardized Beta |
95% Confidence Interval |
P-Value |
|---|---|---|---|
| CTQ-Abuse | 0.39 | 0.02-0.05 | <0.001 |
| BDI-II | 0.39 | 0.02-0.05 | <0.001 |
| TAS | 0.22 | 0.002-0.03 | 0.03 |
| Being Married | −0.25 | −0.93- −0.14 | 0.009 |
Given the robust relationship between fearful attachment style and childhood abuse burden, we performed a post-hoc analysis to evaluate the relationships between fearful attachment and CTQ-abuse subscales (sexual, emotional, and physical). Performing a single linear regression with fearful attachment scores as the dependent variable and all three CTQ-abuse subscales as independent variables, the magnitude of sexual abuse (standardized beta=0.29, p=0.03) and emotional abuse (standardized beta=0.49, p=0.002) independently correlated with fearful attachment. This model explained 37.0% of the variance in fearful attachment style scores.
In univariate tests, preoccupied attachment positively correlated with DES (r=0.38, p=0.004), NEO-neuroticism (r=0.34, p=0.01), STAI-T (r=0.28, p=0.04), BIS (r=0.28, p=0.04), and PCS (r=0.32, p=0.02) scores; preoccupied attachment was negatively associated with NEO-conscientiousness (r=−0.32, p=0.02). In a multivariate linear regression analysis, no variables independently correlated with preoccupied attachment.
Dismissing attachment was negatively associated with being married (t=−2.41, p=0.02) and white ethnicity (t=−2.13, p=0.04) in univariate analyses. Neither variable remained statistically significant in a multivariate linear regression analysis. Also, across all univariate analyses, there were no statistically significant differences in attachment subscale scores between patients with isolated FND (n=45) and the 11 individuals with FND and co-morbid major neurologic conditions.
Discussion
The positive correlation between fearful attachment tendencies and childhood traumatic experiences across motor FND subtypes reinforces the notion that early-life maltreatment is connected to insecure attachment in adulthood. While not all individuals with FND endorse adverse early life events, childhood trauma is a well-documented risk factor for FND{31} and has been linked to functional neurologic symptom severity{32-34}. Our findings extend prior evidence of relationships between fearful attachment and early traumatic experiences in PNES{12}, demonstrating overlapping trauma-attachment relationships across the spectrum of motor FND. Studies have also observed higher incidence of insecure attachment and childhood trauma in patients with somatic symptom disorders{35}. Our post-hoc analyses demonstrate that sexual and emotional abuse each independently contribute to the development of fearful attachment in patients with motor FND. As noted by Wearden and colleagues, fearful attachment, which combines a negative view of the self with a negative view of others, can arise from past rejection or caregiver maltreatment, resulting in abandonment anxiety and a fear of intimacy in interpersonal relationships{9}. This phenomenon may explain why patients with FND who were married reported lower fearful attachment tendencies, though this study only examined marital status, as opposed to marital quality or relationship stability, which may be potential topics for future research.
In patients with FND, fearful attachment also positively correlated with alexithymia and depression, factors that we have previously linked to decreased self-reported resilience in a recently published study from our lab in this same cohort{14}. Alexithymia, or difficulty identifying and expressing emotions, has been associated with insecure attachment in patients with somatoform disorders and constitutes an obstacle to healthy emotional and personal interactions{36}. Alexithymia is commonly identified as an important predisposing vulnerability in patients with FND{10, 37, 38} and may partially explain the misattribution of emotional states as physical phenomena given nuanced connections between stressful life events, affective dysregulation, and physical symptoms. This explanation may be in line with alexithymia-related somatosensory amplification, which attributes increased interoceptive arousal and somatic misattribution to alexithymic patients{39}. Additionally, depression is a common comorbidity in FND{16, 40, 41}, and links between depression, health-related quality of life and prognosis have been well described in FND populations{42, 43}. In the context of recognized associations between fearful attachment and depression{44}, PTSD{45} and dissociation{46}, our finding suggests that links between negative affective symptoms and fearful attachment are present across multiple psychopathologies.
Across attachment styles, personality traits, resilience, and anxiety appear to also be important factors connected to patients’ approaches to interpersonal relationships based on our preliminary univariate analyses. We have previously linked adaptive and maladaptive personality traits to self-reported stress coping (resilience) in patients with FND{14}, and personality traits may influence concurrent pathophysiology, symptom profiles, and prognosis in FND populations{43, 47}. Furthermore, self-reported resilience was closely linked to secure attachment and inversely associated with fearful attachment in univariate analyses, suggesting that healthy interpersonal relationships are an important component of adaptive stress coping. In this study, secure, fearful, and preoccupied attachment styles related to neuroticism, a factor that plays a role in the development of mood and affective disorders more broadly{48}. Additionally, anxiety, another common comorbidity in FND{16, 40, 41}, positively correlated with fearful and preoccupied attachment styles and negatively correlated with secure attachment. The lack of clear connections related to symptom severity and health status indicate that further studies of attachment with larger sample sizes are needed to investigate potential indirect links between attachment styles and symptom severity.
While this study aimed to examine relationships between attachment styles and other neuropsychiatric factors in FND, we did not obtain attachment data in healthy controls or other clinical populations, preventing analyses of group-level differences. We were also limited by a reliance on self-report measures and did not use gold standard structured attachment interviews{13}, leaving unaddressed potential differences between self-perceived interpersonal styles and more objective measures. Additionally, we included 11 FND subjects with major neurological comorbidities to ensure that the study sample was representative of the overall FND population{14}. Lastly, we recruited patients across the motor spectrum of FND given the many similarities among these sub-populations{14, 32}, though this approach remains debated{49}. We only had one univariate association between a motor FND subtype and an attachment style (those with FMD reported higher secure attachment tendencies compared to other motor FND subtypes), implying that insecure attachment styles were similar across motor FND sub-populations.
In conclusion, fearful attachment related to the magnitude of childhood abuse burden, alexithymia, depression, and marital status in patients across the spectrum of motor FND. These findings identify links between fearful attachment tendencies and several other risk factors for the development of FND. Future research is needed to determine the influence of insecure attachment styles on symptom onset and severity, as well as clinical outcomes in FND.
Supplementary Material
Supplemental Table 1. Clinical characteristics of patients with motor functional neurological disorders. †Indicates that these patients had splitting of the midline functional numbness. ††Indicates that patient also had a functional cognitive disorder. *Indicates that these patients also had functional voice symptoms. **Psychiatric diagnoses made by chart review, as structured psychiatric interview not performed. M, male; F, female; PNES, Psychogenic Nonepileptic Seizures; FW, Functional Weakness; FMD, Functional Movement Disorders; NOS, not otherwise specified; MDD, Major Depressive Disorder; PD_Ag+, Panic Disorder with Agoraphobia; PD_Ag-, Panic Disorder without Agoraphobia; GAD, Generalized Anxiety Disorder; Undiff Somatoform, Undifferentiated Somatoform Disorder; PTSD, Post-Traumatic Stress Disorder; OCD, Obsessive Compulsive Disorder; Ag, Agoraphobia without Panic Disorder; LOC, Loss of Consciousness; AMD, Amantadine; APM, Amphetamine; APZ, Aripiprazole; ATP, Amitriptyline; BSP, Buspirone; BUP, Bupropion; BZP, Benztropine; CLN, Clonidine; CLP, Clonazepam; CTP, Citalopram; CZP, Carbamazepine; DLX, Duloxetine; DNZ, donepezil; DOX, Doxepin; DVX, Desvenlafaxine; DXAM, Dextroamphetamine; DZP, Diazepam; ECP, Escitalopram; FLX, Fluoxetine; GBP, Gabapentin; LRZ, Lorazepam; LSD, Lysergic Acid Diethylamide; LTG, Lamotrigine; LXAM, Lisdexamfetamine; MIR, Mirtazapine; NRT, Nortriptyline; PGN, Pregabalin; PZN, Prazosin; QTP, Quetiapine; ROP, Ropinirole; SERT, Sertraline; THP, Trihexyphenidyl; TPM, Topiramate; TZD, Trazodone; VEN, Venlafaxine; VPA, Valproic Acid; VTX, Vortioxetine; ZLP, Zolpidem.
Supplemental Table 2. Demographic characteristics and within group univariate associations with self-reported attachment styles (RSQ) in motor functional neurological disorders. Test statistic refers to independent sample t-test for dichotomous group comparisons or Pearson correlation coefficient for continuous variables. *Indicates that one subject had missing data for the PTSD-CL5 and another subject had missing data for the PCS. RSQ, Relationship Scales Questionnaire; FND, Functional Neurological Disorder; PNES, psychogenic non-epileptic seizures; FMD, functional movement disorders; FW, functional weakness; SD, standard deviation; SOMS: CD, Conversion Disorder Subscale of the Screening for Somatoform Symptoms-7 scale; PHQ-15, Patient Health Questionnaire-15; SDQ-20, Somatoform Dissociation Questionnaire-20; SF-36; Short Form Health Survey-36; DES, Dissociative Experience Scale; PTSD-CL5, Post-Traumatic Stress Disorder Checklist for DSM-5; LEC, Life Events Checklist; CTQ, Childhood Trauma Questionnaire; BDI-II, Beck Depression Inventory-II; STAI-T, Spielberger State-Trait Anxiety Inventory Total Score; CD-RISC, Connor-Davidson Resilience Scale; TAS, Toronto Alexithymia Score; NEO, NEO Five-Factor Inventory-3; BIS, Barrett Impulsivity Scale; PCS, Pain Catastrophizing Scale.
Acknowledgments
Funding:
D.L.P. was funded by the Sidney R. Baer Jr. Foundation and the Massachusetts General Hospital Physician-Scientist Development Award.
Footnotes
Conflicts of Interest/Disclosures:
None
References
- 1.Bowlby J: Developmental psychiatry comes of age. Am J Psychiatry 1988; 145:1–10 [DOI] [PubMed] [Google Scholar]
- 2.Edwards MJ, Bhatia KP: Functional (psychogenic) movement disorders: merging mind and brain. The Lancet Neurology 2012; 11:250–260 [DOI] [PubMed] [Google Scholar]
- 3.Reuber M, Howlett S, Khan A, et al. : Non-epileptic seizures and other functional neurological symptoms: predisposing, precipitating, and perpetuating factors. Psychosomatics 2007; 48:230–238 [DOI] [PubMed] [Google Scholar]
- 4.Ainsworth MDS, Blehar MC, Waters E, et al. : Patterns of attachment: A psychological study of the strange situation, Psychology Press, 2015 [Google Scholar]
- 5.Griffin DW, Bartholomew K: The metaphysics of measurement: The case of adult attachment. 1994; [Google Scholar]
- 6.Bartholomew K: Avoidance of intimacy: An attachment perspective. Journal of Social and Personal Relationships 1990; 7:147–178 [Google Scholar]
- 7.Waldinger RJ, Schulz MS, Barsky AJ, et al. : Mapping the road from childhood trauma to adult somatization: the role of attachment. Psychosom Med 2006; 68:129–135 [DOI] [PubMed] [Google Scholar]
- 8.Fricchione G: Compassion and healing in medicine and society : on the nature and use of attachment solutions to separation challenges, Baltimore, Johns Hopkins University Press, 2011 [Google Scholar]
- 9.Wearden AJ, Lamberton N, Crook N, et al. : Adult attachment, alexithymia, and symptom reporting: An extension to the four category model of attachment. J Psychosom Res 2005; 58:279–288 [DOI] [PubMed] [Google Scholar]
- 10.Brown RJ, Bouska JF, Frow A, et al. : Emotional dysregulation, alexithymia, and attachment in psychogenic nonepileptic seizures. Epilepsy Behav 2013; 29:178–183 [DOI] [PubMed] [Google Scholar]
- 11.Green B, Norman P, Reuber M: Attachment style, relationship quality, and psychological distress in patients with psychogenic non-epileptic seizures versus epilepsy. Epilepsy Behav 2017; 66:120–126 [DOI] [PubMed] [Google Scholar]
- 12.Holman N, Kirkby A, Duncan S, et al. : Adult attachment style and childhood interpersonal trauma in non-epileptic attack disorder. Epilepsy Res 2008; 79:84–89 [DOI] [PubMed] [Google Scholar]
- 13.Kozlowska K, Scher S, Williams LM: Patterns of emotional-cognitive functioning in pediatric conversion patients: implications for the conceptualization of conversion disorders. Psychosom Med 2011; 73:775–788 [DOI] [PubMed] [Google Scholar]
- 14.Jalilianhasanpour R, Williams B, Gilman I, et al. : Resilience linked to personality dimensions, alexithymia and affective symptoms in motor functional neurological disorders. J Psychosom Res 2018; 107:55–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McKee K, Glass S, Adams C, et al. : The Inpatient Assessment and Management of Motor Functional Neurological Disorders: An Interdisciplinary Perspective. Psychosomatics 2018; Epub Ahead of Print [DOI] [PubMed] [Google Scholar]
- 16.Matin N, Young SS, Williams B, et al. : Neuropsychiatric Associations with Gender, Illness Duration, Work Disability and Motor Subtype in a US Functional Neurological Disorders Clinic Population J Neuropsychiatry Clin Neurosci 2017; 29:375–382 [DOI] [PubMed] [Google Scholar]
- 17.Kroenke K, Spitzer RL, Williams JB: The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med 2002; 64:258–266 [DOI] [PubMed] [Google Scholar]
- 18.Rief W, Hiller W: A new approach to the assessment of the treatment effects of somatoform disorders. Psychosomatics 2003; 44:492–498 [DOI] [PubMed] [Google Scholar]
- 19.Bernstein EM, Putnam FW: Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis 1986; 174:727–735 [DOI] [PubMed] [Google Scholar]
- 20.Nijenhuis ER, Spinhoven P, Van Dyck R, et al. : The development and psychometric characteristics of the Somatoform Dissociation Questionnaire (SDQ-20). J Nerv Ment Dis 1996; 184:688–694 [DOI] [PubMed] [Google Scholar]
- 21.Ware JE Jr., Sherbourne CD: The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992; 30:473–483 [PubMed] [Google Scholar]
- 22.Beck AT, Ward CH, Mendelson M, et al. : An inventory for measuring depression. Arch Gen Psychiatry 1961; 4:561–571 [DOI] [PubMed] [Google Scholar]
- 23.Spielberger CD, Gorsuch RL, Lushene RE: Manual for the state-trait anxiety inventory. 1970 [Google Scholar]
- 24.Costa P Jr, McRae R: Revised NEO Personality Inventory (NEO-PI-R) and NEO Five-Factor Inventory (NEO-FFI) professional manual. Psychological Assessment Resources. Inc; 1992 [Google Scholar]
- 25.Bagby M, Taylor GJ, Ryan D: Toronto Alexithymia Scale: Relationship with personality and psychopathology measures. Psychotherapy and Psychosomatics 1986; 45:207–215 [DOI] [PubMed] [Google Scholar]
- 26.Barratt ES, Patton J, Stanford M: Barratt Impulsiveness Scale, Barratt-Psychiatry Medical Branch, University of Texas; Texas, 1975 [Google Scholar]
- 27.Connor KM, Davidson JR: Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety 2003; 18:76–82 [DOI] [PubMed] [Google Scholar]
- 28.Bernstein DP, Fink L, Handelsman J, et al. : Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry 1994; 151:1132–1136 [DOI] [PubMed] [Google Scholar]
- 29.Weathers FW, Blake DD, Schnurr PP, et al. : The Life Events Checklist for DSM-5 (LEC-5). 2013 [Google Scholar]
- 30.Blevins CA, Weathers FW, Davis MT, et al. : The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress 2015; 489–498 [DOI] [PubMed] [Google Scholar]
- 31.Ludwig L, Pasman JA, Nicholson T, et al. : Stressful life events and maltreatment in conversion (functional neurological) disorder: systematic review and meta-analysis of case-control studies. The Lancet Psychiatry 2018; 5:307–320 [DOI] [PubMed] [Google Scholar]
- 32.Perez DL, Matin N, Barsky A, et al. : Cingulo-insular structural alterations associated with psychogenic symptoms, childhood abuse and PTSD in functional neurological disorders. J Neurol Neurosurg Psychiatry 2017; 88:491–497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Roelofs K, Keijsers GP, Hoogduin KA, et al. : Childhood abuse in patients with conversion disorder. Am J Psychiatry 2002; 159:1908–1913 [DOI] [PubMed] [Google Scholar]
- 34.Selkirk M, Duncan R, Oto M, et al. : Clinical differences between patients with nonepileptic seizures who report antecedent sexual abuse and those who do not. Epilepsia 2008; 49:1446–1450 [DOI] [PubMed] [Google Scholar]
- 35.Nacak Y, Morawa E, Tuffner D, et al. : Insecure attachment style and cumulative traumatic life events in patients with somatoform pain disorder: A cross-sectional study. J Psychosom Res 2017; 103:77–82 [DOI] [PubMed] [Google Scholar]
- 36.Koelen JA, Eurelings-Bontekoe EH, Stuke F, et al. : Insecure attachment strategies are associated with cognitive alexithymia in patients with severe somatoform disorder. Int J Psychiatry Med 2015; 49:264–278 [DOI] [PubMed] [Google Scholar]
- 37.Kaplan MJ, Dwivedi AK, Privitera MD, et al. : Comparisons of childhood trauma, alexithymia, and defensive styles in patients with psychogenic non-epileptic seizures vs. epilepsy: implications for the etiology of conversion disorder. J Psychosom Res 2013; 75:142–146 [DOI] [PubMed] [Google Scholar]
- 38.Demartini B, Petrochilos P, Ricciardi L, et al. : The role of alexithymia in the development of functional motor symptoms (conversion disorder). J Neurol Neurosurg Psychiatry 2014:jnnp-2013-307203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Perez DL, Barsky AJ, Vago DR, et al. : A neural circuit framework for somatosensory amplification in somatoform disorders. J Neuropsychiatry Clin Neurosci 2015; 27:e40–50 [DOI] [PubMed] [Google Scholar]
- 40.Sar V, Akyuz G, Kundakci T, et al. : Childhood trauma, dissociation, and psychiatric comorbidity in patients with conversion disorder. Am J Psychiatry 2004; 161:2271–2276 [DOI] [PubMed] [Google Scholar]
- 41.Stone J, Warlow C, Sharpe M: The symptom of functional weakness: a controlled study of 107 patients. Brain 2010; 133:1537–1551 [DOI] [PubMed] [Google Scholar]
- 42.Jones B, Reuber M, Norman P: Correlates of health‐related quality of life in adults with psychogenic nonepileptic seizures: A systematic review. Epilepsia 2016; 57:171–181 [DOI] [PubMed] [Google Scholar]
- 43.Gelauff J, Stone J, Edwards M, et al. : The prognosis of functional (psychogenic) motor symptoms: a systematic review. J Neurol Neurosurg Psychiatry 2014; 85:220–226 [DOI] [PubMed] [Google Scholar]
- 44.Reis S, Grenyer BF: Fear of intimacy in women: Relationship between attachment styles and depressive symptoms. Psychopathology 2004; 37:299–303 [DOI] [PubMed] [Google Scholar]
- 45.Woodhouse S, Ayers S, Field AP: The relationship between adult attachment style and post-traumatic stress symptoms: A meta-analysis. J Anxiety Disord 2015; 35:103–117 [DOI] [PubMed] [Google Scholar]
- 46.Pearce J, Simpson J, Berry K, et al. : Attachment and dissociation as mediators of the link between childhood trauma and psychotic experiences. Clin Psychol Psychother 2017; 24:1304–1312 [DOI] [PubMed] [Google Scholar]
- 47.Ekanayake V, Kranick S, LaFaver K, et al. : Personality traits in psychogenic nonepileptic seizures (PNES) and psychogenic movement disorder (PMD): Neuroticism and perfectionism. J Psychosom Res 2017; 97:23–29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ormel J, Jeronimus BF, Kotov R, et al. : Neuroticism and common mental disorders: meaning and utility of a complex relationship. Clin Psychol Rev 2013; 33:686–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kanaan RA, Duncan R, Goldstein LH, et al. : Are psychogenic non-epileptic seizures just another symptom of conversion disorder? J Neurol Neurosurg Psychiatry 2017; 88:425–429 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1. Clinical characteristics of patients with motor functional neurological disorders. †Indicates that these patients had splitting of the midline functional numbness. ††Indicates that patient also had a functional cognitive disorder. *Indicates that these patients also had functional voice symptoms. **Psychiatric diagnoses made by chart review, as structured psychiatric interview not performed. M, male; F, female; PNES, Psychogenic Nonepileptic Seizures; FW, Functional Weakness; FMD, Functional Movement Disorders; NOS, not otherwise specified; MDD, Major Depressive Disorder; PD_Ag+, Panic Disorder with Agoraphobia; PD_Ag-, Panic Disorder without Agoraphobia; GAD, Generalized Anxiety Disorder; Undiff Somatoform, Undifferentiated Somatoform Disorder; PTSD, Post-Traumatic Stress Disorder; OCD, Obsessive Compulsive Disorder; Ag, Agoraphobia without Panic Disorder; LOC, Loss of Consciousness; AMD, Amantadine; APM, Amphetamine; APZ, Aripiprazole; ATP, Amitriptyline; BSP, Buspirone; BUP, Bupropion; BZP, Benztropine; CLN, Clonidine; CLP, Clonazepam; CTP, Citalopram; CZP, Carbamazepine; DLX, Duloxetine; DNZ, donepezil; DOX, Doxepin; DVX, Desvenlafaxine; DXAM, Dextroamphetamine; DZP, Diazepam; ECP, Escitalopram; FLX, Fluoxetine; GBP, Gabapentin; LRZ, Lorazepam; LSD, Lysergic Acid Diethylamide; LTG, Lamotrigine; LXAM, Lisdexamfetamine; MIR, Mirtazapine; NRT, Nortriptyline; PGN, Pregabalin; PZN, Prazosin; QTP, Quetiapine; ROP, Ropinirole; SERT, Sertraline; THP, Trihexyphenidyl; TPM, Topiramate; TZD, Trazodone; VEN, Venlafaxine; VPA, Valproic Acid; VTX, Vortioxetine; ZLP, Zolpidem.
Supplemental Table 2. Demographic characteristics and within group univariate associations with self-reported attachment styles (RSQ) in motor functional neurological disorders. Test statistic refers to independent sample t-test for dichotomous group comparisons or Pearson correlation coefficient for continuous variables. *Indicates that one subject had missing data for the PTSD-CL5 and another subject had missing data for the PCS. RSQ, Relationship Scales Questionnaire; FND, Functional Neurological Disorder; PNES, psychogenic non-epileptic seizures; FMD, functional movement disorders; FW, functional weakness; SD, standard deviation; SOMS: CD, Conversion Disorder Subscale of the Screening for Somatoform Symptoms-7 scale; PHQ-15, Patient Health Questionnaire-15; SDQ-20, Somatoform Dissociation Questionnaire-20; SF-36; Short Form Health Survey-36; DES, Dissociative Experience Scale; PTSD-CL5, Post-Traumatic Stress Disorder Checklist for DSM-5; LEC, Life Events Checklist; CTQ, Childhood Trauma Questionnaire; BDI-II, Beck Depression Inventory-II; STAI-T, Spielberger State-Trait Anxiety Inventory Total Score; CD-RISC, Connor-Davidson Resilience Scale; TAS, Toronto Alexithymia Score; NEO, NEO Five-Factor Inventory-3; BIS, Barrett Impulsivity Scale; PCS, Pain Catastrophizing Scale.