Abstract
Background
Infrared thermographic imaging (IRTG) is a safe and reliable technology used to monitor skin temperature. The main aim of our study was to evaluate the relationship between skin temperature changes and muscle fatigue in order to answer the main research question if IRTG can be used to monitor muscle fatigue.
Methods
This was a case study performed on a 23-year-old trained middle distance runner. After warm-up the subject was exercising on the dynamometer for 7.5 min at 120°/s performing only concentric contractions of quadriceps. At the same time IRTG recording of both (exercising and non-exercising) quadriceps was performed.
Results
A correlational analysis that was performed in order to quantify the relationship between power and temperature change over time has shown that there is a significant negative correlation between skin temperature increase and power decrease (r = −0.543, p = 0.036) of exercising quadriceps. In linear regression model the exercising quadriceps power could be predicted from skin temperature. No such relationships were noted for the non-exercising limb that served as a control.
Conclusion
We believe that correlation between skin temperature change and muscle power output as described in this case study deserves further analysis on the larger sample including subjects of the different ages, health status, and physical abilities in order to create a new tool for monitoring the muscle fatigue.
Keywords: Correlation, Fatigue, Isokinetic, Quadriceps, Strength, Thermographic imaging
1. Introduction
Infrared thermographic imaging (IRTG) is a non-radiating and contact-free technology used to monitor skin temperature. The efficiency, safety, and low cost of IRTG make it a useful tool for detecting and locating thermal changes characterized by increases or decreases in skin surface temperature.1 During exercise human body is challenged to regulate the core temperature in order to prevent overheating due to heat production of contracting muscles. At the beginning of the exercise there is a cutaneous vasoconstriction2 due to increase of blood flow in the contracting muscle, but as exercise is prolonged and core temperature increases the central regulatory mechanisms causes the vasodilation and heat dissipation through the skin.3 Concomitantly with this process the muscle force output decreases during prolonged exercise leading to muscle fatigue.4
Muscle fatigue may be defined as a reversible decrease in contractile strength that occurs after longlasting or repeated muscular activity.5 By definition this is a condition of the muscle in which its capacity to produce maximum voluntary action, or to perform a series of repetitive actions, is reduced. Following the fatigue the subject's performance decreases6 as well as the injury risk.7 Monitoring the presence and magnitude of fatigue to maximize performance and training adaptation is an important consideration for applied sports scientists.8 Although the most commonly used method to monitor fatigue in sport science is electromyographic (EMG), there is an ongoing search for new tools to identify and quantify fatigue objectively and IRTG imaging could be one of such tools.9
In one of the recent studies authors10 have investigated the possibility of using IRTG for assessing muscle fatigue during low isometric effort. They investigated the temperature and EMG changes of biceps brachii muscle at loads equivalent to 5%, 15%, and 30% of maximal voluntary contraction in 10 healthy men. The results showed that isometric contraction at above-mentioned loads has resulted in an increase of skin temperature overlaying the biceps brachii muscle and that those changes over time in the values of all analyzed EMG parameters were significantly correlated with changes in the temperature. In another study3 authors have investigated thermoregulation of a local muscle area (muscle–tendon unit) involved in a localized steady-load exercise (2 min of standing heels raise) using IRTG in 7 trained females and 7 untrained female controls. The results showed that the skin temperature following the dynamic exercise protocol increased by 1.0°C ± 0.2°C and 0.4°C ± 0.1°C in trained and untrained females, respectively.
To our best knowledge, none of the previous studies has investigated how the muscle's torque (and power) output and skin temperature changes over the time during the concentric isokinetic exercise. The main aim of our study was to record skin temperature changes while registering how the torque output changes over the time in order to investigate the relationship between these 2 parameters, as it is known that heat dissipation during sport exercise is an important physiological mechanism that may influence athletic performance. The muscle of choice for this case study was quadriceps as dynamic activity of a significant muscle mass is required for initial vasoconstrictor response,2 as small muscle groups or isometric exercises are ineffective for such response.
2. Methods
2.1. Study design and subjects
This was a case study performed on a trained volunteer. The subject was a 23-year-old middle distance runner with 12-year training history (body height = 178.5 cm, body weight = 68 kg). Testing was performed at the Laboratory for Isokinetic Testing at the Faculty of Sport in Ljubljana. The environmental temperature in the laboratory during the tests was constant at 23.5°C (±2%). Before the measurements, the subject was in the laboratory for at least 15 min to acclimatize. The Ethic Board of the Faculty of Sport in Ljubljana approved the study, and written informed consent was obtained from the participant.
2.2. Exercise fatigue protocol
Each exercise session started with a warm-up consisting of cycling for 6 min on an ergometer (Ergo bike premium 8; Daum electronic GmbH, Fürth, Germany) at a constant pace (100 W), followed by a 10-s stretch of quadriceps (Q) and hamstrings (H). The dynamometer (iMoment, SMM, Maribor, Slovenia) was set into continuous passive motion (CPM) mode at the velocity 120°/s (moderate isokinetic speed). The session was to be ended by time and time limit was set at 7.5 min. Subject was in a sitting position where forward sliding on the seat was prevented with the use of proper belts that were pushing pelvis downward and backward but were not uncomfortable for the participants. Trunk movement was also prevented using comfortable strapping over the chest region. The thighs of both legs were secured using special straps. The subject was allowed to hold the handles during the protocol. The axis of rotation of knee joint was identified through the lateral femoral condyle and aligned with the dynamometer axis. A range of motion was 80° from 10° to 90° knee flexion (full extension considered 0°). As our primary goal was to assess the changes in skin temperature over quadriceps muscle in respect to changes in quadriceps torque we used a CPM at 120°/s. Subject was instructed to push the dynamometer handle as fast and hard as they can from 90° flexion to the 10° flexion and then relax until CPM returns the leg to the starting position in 90° flexion. The dynamometer was set to demand the full (80°) range of motion for each repetition over the given time period. By using this approach we prevented hamstrings to play any role in the heat production during the exercise protocol while the quadriceps was fully loaded through predetermined range of motion. The left quadriceps served as a control for the right leg in the terms of temperature change during the exercise protocol. Following the exercise protocol we have exported raw quadriceps torque data including time, torque, angle, and velocity information. From the data we calculated the power as a product of torque and angular velocity that was calculated as the change of angle over the change in time. Following this we calculated 30 s power average intervals and plotted them on the diagram against the temperature.
2.3. Thermographic imaging
An IR camera (FLIR T425; FLIR Systems, Täby, Sweden) was used to measure quadriceps temperature. It had a focal plane array (FPA) of uncooled microbolometer detectors that gave a resolution of 320 × 240 pixels.
The spectral range of matrix detectors was 7.5–13 µm. The precision of determining a temperature increase was 0.1°C. Thermal emissivity of the camera was adjusted at 0.98, which is suitable for human skin. The camera supported a 256 grayscale technique with MPEG4 video compression. The video was taken from 1 m distance at the rate of 8 pictures/s. Although cameras with better sampling frequency and better resolution are available at the market, the chosen camera was properly calibrated and the area from which the mean temperature was calculated was large enough, that camera resolution could not affect the results. The same is also true for the sampling frequency, as the results were averaged for 30 s intervals in which there are 240 pictures.
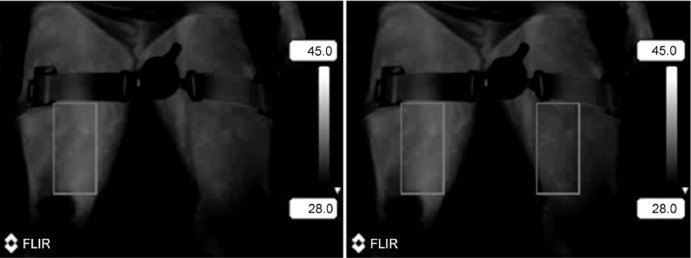
Thermogram sequences were registered and analyzed with ThermaCam Researcher 2001 software (FLIR Systems). Each thermogram (Fig. 1) contained digital information on the temperature values for each of the 76,800 pixels (320 × 240). Sequence of pictures was extracted from the video and based on the grayscale and temperature scale the mean temperature was calculated on the medial aspect of the quadriceps muscle (Fig. 1). Thirty seconds temperature average intervals were calculated and plotted on the diagram against the power.
Fig. 1.
The area for thermographic measurement (rectangle) on left (non-exercising) and right (exercising) quadriceps.
2.4. Statistical analysis
Diagram was plotted on synchronized time scale with 30 s intervals to show the relationship between power and temperature changes of quadriceps muscle. Temperature change was shown for both quadriceps muscles (exercising and control). Furthermore, correlational analysis was performed in order to quantify the relationship between power change and temperature change over time. All statistical analyses were performed using SPSS Statistics for Windows (Version 21.0; IBM Corp., Armonk, NY, USA). The significance threshold was set at 0.05.
3. Results
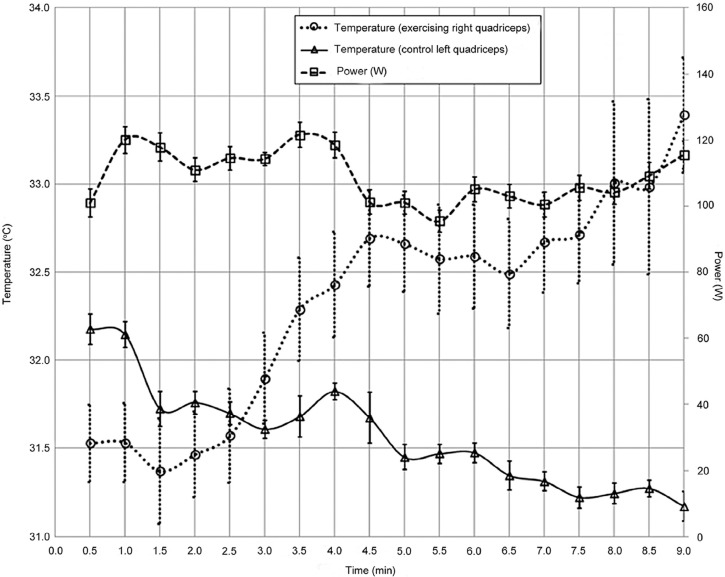
The results are depicted on Fig. 2. The mean temperature of the exercising vs. non-exercising limb was 32.2°C vs. 31.7°C, (mean difference 0.5°C, p = 0.018). The correlational analysis has shown that there is a significant negative correlation between skin temperature increase and power decrease (r = −0.543, p = 0.036). In linear regression model (R2 = 0.30; F = 5.438, p = 0.036) the quadriceps power could be predicted from skin temperature by Eq. (1).
| (1) |
Fig. 2.
Diagram of 30 s average temperature and power changes with 95% confidence intervals during the course of exercise.
4. Discussion
The main finding of this case study indicates that there is a significant correlation between quadriceps skin temperature and quadriceps power. The temperature of the skin overlying quadriceps has increased for 1.1°C during the course of exercise while quadriceps power has decreased for 7.9%. This is true when average of first 2 min was compared to last 2 min of exercise bout. At the same time the control (non-exercising) quadriceps did not show such temperature changes as overlying skin temperature has decreased for 0.7°C as there was no exercise induced heat production. Our results are in concordance with Formenti et al.3 who also reported skin temperature increase of 1°C and Al-Nakhli et al.11 who reported a post-exercise temperature increase of 1.17°C.
One of the possible physiological explanations of our findings may be the fact that an increase in muscle temperature per se increases muscle glycogen utilization during submaximal exercise12 leading to the decrease in power output. The curve of the 30 s average temperature of the control leg depicts the decrease in temperature over the 7.5 min period that was probably a result of the vasodilation13 that occurred as a general response to the exercise of the contralateral limb and was sustained over the whole period as the muscle was neither contracting nor producing heat.
Previous studies have shown that elderly subjects present with lower resting temperature and slower heat dissipation in comparison to young subjects14 and that thermoregulatory response differs among trained and untrained participants15 and among healthy and injured athletes.1 In the light of such findings we believe that correlation between skin temperature change and muscle power output as described in this case study deserves further analysis on the larger sample including subjects of the different age, health status, and physical abilities and also including the monitoring of the subject's average body temperature at the start of the specific activity, as this parameter could theoretically influence the observed relationship between skin temperature and muscle power.
5. Conclusion
The results of this case study are pointing to the possible relationship between muscle skin temperature change and muscle fatigue. As muscle skin temperature is much easier to monitor than muscle fatigue a further research in this area could give us a new tool to easily monitor muscle fatigue.
Authors' contributions
VH carried out isokinetic measurements and was involved in data analysis and presentation as well as manuscript drafting; BŠ was involved in study design and was advising regarding the analysis of thermographic measurements; AM carried out all thermographic measurements and was involved in data analysis and presentation; MČ carried out the study design and protocol and helped to draft the manuscript. All authors have read and approved the final version of the manuscript, and agree with the order of presentation of the authors.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Peer review under responsibility of Shanghai University of Sport.
References
- 1.Hildebrandt C., Zeilberger K., Francis E., Ring J., Raschner C. The application of medical infrared thermography in sports medicine. In: Zaslav K.R., editor. An international perspective on topics in sports medicine and sports injury. InTech; Rijeka: 2012. [Google Scholar]
- 2.Johnson J.M. Exercise and the cutaneous circulation. Exerc Sport Sci Rev. 1992;20:59–97. [PubMed] [Google Scholar]
- 3.Formenti D., Ludwig N., Gargano M., Gondola M., Dellerma N., Caumo A. Thermal imaging of exercise-associated skin temperature changes in trained and untrained female subjects. Ann Biomed Eng. 2013;41:863–871. doi: 10.1007/s10439-012-0718-x. [DOI] [PubMed] [Google Scholar]
- 4.Abbiss C.R., Burnett A., Nosaka K., Green J.P., Foster J.K., Laursen P.B. Effect of hot versus cold climates on power output, muscle activation, and perceived fatigue during a dynamic 100-km cycling trial. J Sports Sci. 2010;28:117–125. doi: 10.1080/02640410903406216. [DOI] [PubMed] [Google Scholar]
- 5.Komi P.V. Wiley-Blackwell; Oxford: 2002. Strength and power in sport. [Google Scholar]
- 6.Sesboüé B., Guincestre J.Y. Muscular fatigue. Ann Readapt Med Phys. 2006;49:257–264. doi: 10.1016/j.annrmp.2006.04.021. [DOI] [PubMed] [Google Scholar]
- 7.Opar D.A., Williams M.D., Shield A.J. Hamstring strain injuries: factors that lead to injury and re-injury. Sports Med. 2012;42:209–226. doi: 10.2165/11594800-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 8.Twist C., Highton J. Monitoring fatigue and recovery in rugby league players. Int J Sports Physiol Perform. 2013;8:467–474. doi: 10.1123/ijspp.8.5.467. [DOI] [PubMed] [Google Scholar]
- 9.Bertmaring I., Babski-Reeves K., Nussbaum M.A. Infrared imaging of the anterior deltoid during overhead static exertions. Ergonomics. 2008;51:1606–1619. doi: 10.1080/00140130802216933. [DOI] [PubMed] [Google Scholar]
- 10.Bartuzi P., Roman-Liu D., Wiśniewski T. The influence of fatigue on muscle temperature. Int J Occup Saf Ergon. 2012;18:233–243. doi: 10.1080/10803548.2012.11076931. [DOI] [PubMed] [Google Scholar]
- 11.Al-Nakhli H.H., Petrofsky J.S., Laymon M.S., Berk L.S. The use of thermal infra-red imaging to detect delayed onset muscle soreness. J Vis Exp. 2012;59:3551. doi: 10.3791/3551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Starkie R.L., Hargreaves M., Lambert D.L., Proietto J., Febbraio M.A. Effect of temperature on muscle metabolism during submaximal exercise in humans. Exp Physiol. 1999;84:775–784. [PubMed] [Google Scholar]
- 13.Torii M., Yamasaki M., Sasaki T., Nakayama H. Fall in skin temperature of exercising man. Br J Sports Med. 1992;26:29–32. doi: 10.1136/bjsm.26.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ferreira J.J., Mendonça L.C., Nunes L.A., Andrade Filho A.C., Rebelatto J.R., Salvini T.F. Exercise-associated thermographic changes in young and elderly subjects. Ann Biomed Eng. 2008;36:1420–1427. doi: 10.1007/s10439-008-9512-1. [DOI] [PubMed] [Google Scholar]
- 15.Abate M., Di Carlo L., Di Donato L., Romani G.L., Merla A. Comparison of cutaneous termic response to a standardised warm up in trained and untrained individuals. J Sports Med Phys Fitness. 2013;53:209–215. [PubMed] [Google Scholar]