Abstract
Purpose
To compare the significance of the tibio-femoral geometrical indices (notch width index, medial and lateral tibial slopes) and patellar tendon- tibial shaft angle in predicting non-contact ACL injuries and to compare these factors between genders.
Methods
Retrospective case control study evaluating 66 MRI knee of patients of age group of 18–60 years with 33 cases of noncontact ACL injury and 33 age matched controls. Notch width index, medial and lateral tibial slopes and patellar tendon tibial shaft angles were calculated and compared for statistical significance and was also compared between the genders. ROC curve was for plotted for the significant factors.
Results
Statistically significant difference was seen in notch width index and patellar tendon tibial shaft angles with cases showing a narrow notch width index and an increased patellar tendon tibial shaft angle. Gender comparative results showed no statistically significant differences. ROC curve plotted for NWI showed an optimal cut off value of 0.263 with a sensitivity of 88% and a specificity of 52%. ROC curve plotted for PTTS angle showed a cut off value of 26.7 degrees with a sensitivity of 67% and a specificity of 49%.
Conclusion
Narrow Notch width index and increased Patellar tendon tibial shaft angle are predictors of ACL injury. PTTS angle which has been studied as a function of knee flexion angle, can itself be an independent predictor of ACL injury (at a constant knee flexion angle).
Keywords: Notch width, Tibial slope, Patellar tendon angle
1. Introduction
High frequency of noncontact injury to the anterior cruciate ligament (ACL) has prompted considerable investigation into the potential anatomic, environmental, hormonal and biomechanical risk factors.1 Anatomical factors have been extensively studied by various researchers with subject of considerable debate being morphology of the femoral intercondylar notch and slopes of tibial condyles.
Role of morphology of intercondylar notch in ACL injury has received considerable attention in literature. A narrow intercondylar notch may place the ACL prone for injury, as the ligament gets stretched over the medial edge of the lateral femoral condyle.2 It has also been postulated that a smaller ACL would be present in a narrow notch with a greater tendency to rupture. On the contrary, a narrow notch with a normal-sized ACL would provide reduced space for ACL function.
The tibial plateau morphology affects load transmission across the knee joint and hence has been implicated in ACL injury. Tibial slope, defined as the angle between the posterior tibial inclination and the line perpendicular to tibial axis has been measured on lateral and medial tibial condyles. Increased tibial slope causes larger anterior tibial translation, which could lead to ACL injury.
Patellar tendon- tibial shaft angle as a function of knee flexion angle has been studied under weight bearing and non-weight bearing conditions in association with ACL injury.3 It is well known that decreasing the knee flexion angle would result in increase of patellar tendon- tibial shaft angle and increase in the anterior shear forces at the proximal end of tibia with greater ACL loading. With flexion angle being constant in sagittal MRI images, the variations in patellar tendon- tibial shaft angle could reflect alteration in anterior shear forces with predilection for ACL injury.
The aim of the study was to assess and compare the significance of anatomical risk factors in predicting non-contact ACL injuries and to compare these factors between genders. The objective was to study the notch width index, medial and lateral tibial slope and patellar tendon- tibial shaft angle in MRI studies and determine the association of these factors with ACL injury using a case control design.
2. Materials and methods
The present study is a retrospective case control study evaluating MRI knee of patients of age group of 18- 60 years performed during the period of January 2015 to December 2016. A sample size of 66 cases was calculated based on an earlier study 4 with the confidence level of 95% and a confidence interval of 5%. These included 33 cases of noncontact ACL injury and 33 controls, with segregation of the two groups based on MRI findings. MRI studies without any ligament/meniscal/retinacular injuries were included as controls. Knee MRI with history of contact injury, previous surgical history and medical conditions associated with ligamentous laxity were excluded from the study, based on clinical details. Retrospectively evaluated studies included MRI images from 1.5 T MRI system (Magnetom Siemens Avanto, Tim (76 × 18), Erlangen, Germany) at a tertiary care hospital. Imaging protocol included T1 weighted, T2 weighted and Proton Density FATSAT sequences, among which T2 weighted sequences were used for image interpretation. The imaging parameters for T2W sequences included FOV of 160/180 mm, slice thickness of 3 mm, TR of 4000ms and TE OF 74ms. The image interpretation was by done by two radiologists independently and the average of the two readings were taken into consideration. The study was approved by the Institutional review board.
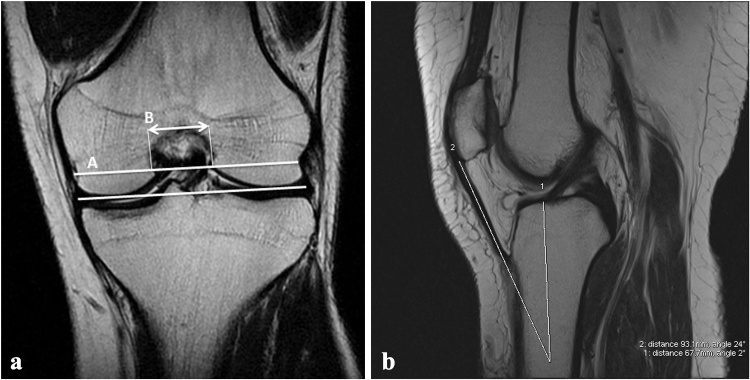
Notch width index (NWI) was measured as the ratio of the intercondylar notch width to the bicondylar width.5 The bicondylar width is measured at the level of the popliteal groove in the lateral condyle of the femur, parallel to the joint line as formed by the distal femoral condyles. Then, on the same line, most interior margins of the femoral condyles at the borders of the intercondylar notch represents the intercondylar notch width (Fig. 1).
Fig. 1.
(a) A is the Bicondylar width parallel to the joint line at the level of popliteal groove. B represents the notch width, the line joining the innermost margins of the femoral condyles at the borders of the intercondylar notch at the level of popliteal groove. B/A gives the notch width index. (b) PTTS angle is measured as the angle between PTAA (Proximal tibial anatomical axis) and patellar tendon axis in the mid-sagittal section. PTAA is obtained by extrapolating the line joining the midpoints of tibial shaft at 5 cms and 6 cms from the articular surface.
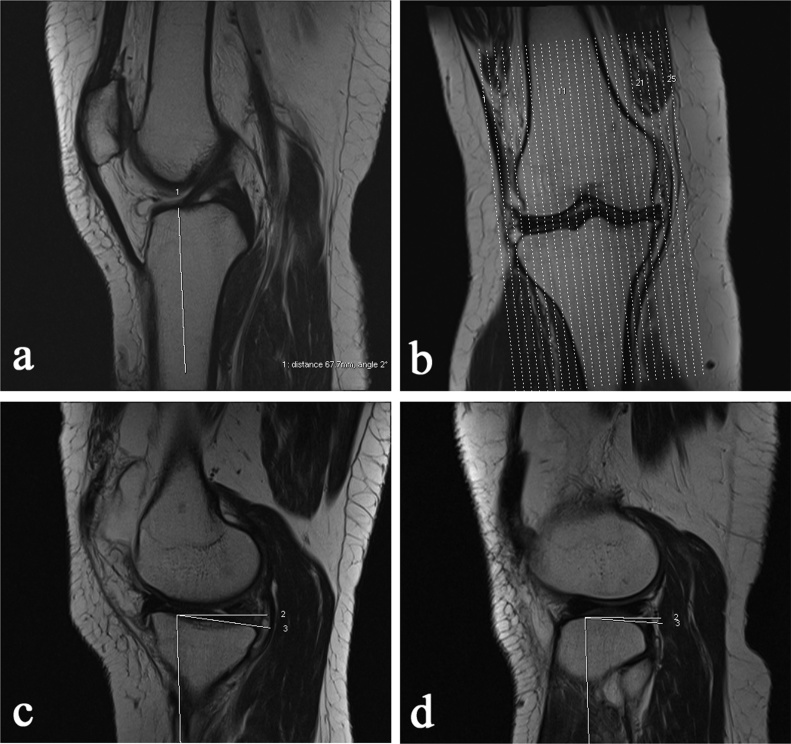
Medial and lateral tibial slopes (MTS and LTS) are measured as the angle between a line joining the peak points on the medial and lateral tibial plateau and the line perpendicular to the tibial longitudinal axis.6 Longitudinal axis of proximal tibia was obtained by extrapolating a line joining the midpoints of tibial shaft at 5 cm and 6 cms from the tibial articular surface at mid sagittal sections. Sagittal sections corresponding to midpoint of medial tibial tubercle and the medial tibial margin and corresponding to the mid-point of lateral tibial tubercle and the lateral tibial margin were located. The longitudinal axis was extrapolated to these sections. Line joining the peak anterior and posterior points on the medial and lateral tibial plateau represented the tibial slopes (medial and lateral).The angle was then measured between the tibial slope on the medial and lateral condyle and the perpendicular to the longitudinal axis (Fig. 2).
Fig. 2.
(a) PTAA (Proximal tibial anatomical axis): Midpoints of tibial shaft are marked at 5 cms and 6 cms from the articular surface. Line joining these two midpoints is extrapolated superiorly. This gives the Proximal tibial anatomical axis. (b) Sagittal section corresponding to midpoint of medial tibial tubercle and medial articular margin is located for measurement of MTS. Similarly, sagittal section corresponding to midpoint of lateral tibial tubercle and lateral articular margin is located for measurement of LTS. A coronal localizer image is used for this purpose. (c) measurement of medial tibial slope: the angle between PTAA and the line joining the peak points on the medial tibial plateau in the sagittal section located gives the medial tibial slope. (d) measurement of lateral tibial slope- the angle between PTAA and the line joining the peak points on the lateral tibial plateau in the sagittal section located gives the lateral tibial slope..
Patellar tendon − tibial shaft (PTTS) angle is measured as the angle between the patellar tendon axis and the tibial shaft axis.7 Tibial shaft axis was obtained as described earlier, by extrapolating a line joining the midpoints of tibial shaft at 5 cm and 6 cms from the tibial articular surface in the mid −sagittal section where the patellar tendon is visualized (Fig. 1). Knee flexion angle was maintained at an angle of 10°.
2.1. Statistical analysis
Analysis of data was by SPSS 16 for windows (IBM- SPSS, Armonk, NY). Age and sex matching between the control group and the cases were evaluated for statistical significance using chi-square test. The anatomical risk factors were studied using the independent samples T test. ROC (Receiver operator characteristics) curves were plotted for the factors which showed statistically significant difference between the two groups for determination of cut off values. p value <0.05 was considered to be statistically significant.
3. Results
Review of 66 MRI knee studies included 33 cases with non-contact ACL injury and 33 control subjects. There was no statistically significant differences in the age and sex distribution among the controls and cases (Table 1). The mean age group of cases was 34.18 years with a standard deviation of 11.56 years and that of controls was 30.24 years with a standard deviation of 8.42 years. No statistically significant difference was seen between the mean age groups (p = 0.119).
Table 1.
Age and sex distribution in cases and controls.
| Parameter | Cases (n = 33) | Controls (n = 33) | p value | |
|---|---|---|---|---|
| Age | < 20 years | 4 (12.12%) | 5 (15.15%) | 0.92 |
| 21–30 years | 9 (27.28%) | 10(30.30%) | ||
| 31–40 years | 13(39.39%) | 13(39.40%) | ||
| >40 years | 7 (21.21%) | 5 (15.15%) | ||
| Sex | Male | 15(45.45%) | 14 (42.42%) | 0.31 |
| Female | 18(54.55%) | 19 (57.58%) |
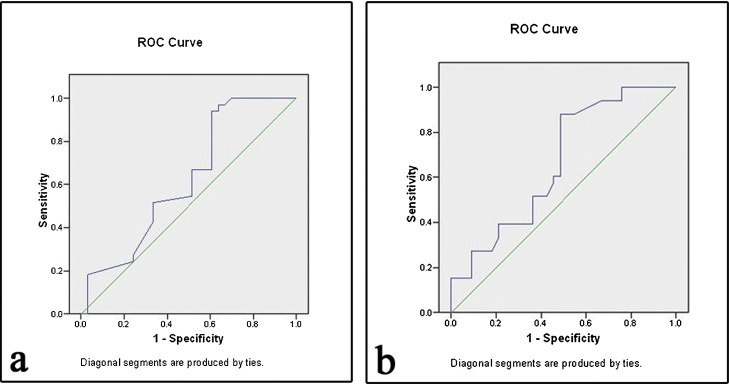
Comparison of the anatomical factors between the cases and controls showed a statistically significant difference in notch width index and patellar tendon tibial shaft angles (Table 2). Mean notch width index (standard deviation) in cases of ACL injury was 0.26 (0.04) whereas the controls showed a NWI of 0.28(0.02). The mean Patellar tendon tibial shaft angle was found to be 27.5° in cases and 25.7° in control subjects. Gender comparative results showed no statistically significant differences (Table 3). ROC curve plotted for NWI showed an optimal cut off value of 0.263 with a sensitivity of 88% and a specificity of 52% (Fig 3). ROC curve plotted for PTTS angle showed a cut off value of 26.7° with a sensitivity of 67% and a specificity of 49% (Fig 3).
Table 2.
Comparison of Notch Width Index, Medial and lateral tibial slope and Patellar tendon tibial shaft angle between cases and controls.
| Parameter | Group | Mean | Std. Deviation | p value |
|---|---|---|---|---|
| Notch Width Index | Cases (n = 33) | 0.26164 | 0.036568 | 0.009 |
| Controls (n = 33) | 0.28232 | 0.024784 | ||
| Medial Tibial Slope | Cases (n = 33) | 4.958 | 1.5548 | 0.818 |
| Controls (n = 33) | 5.042 | 1.4193 | ||
| Lateral Tibial Slope | Cases (n = 33) | 4.491 | 1.4150 | 0.707 |
| Controls (n = 33) | 4.364 | 1.3259 | ||
| Patellar Tendon Tibial Shaft Angle | Cases (n = 33) | 27.542 | 2.3175 | 0.015 |
| Controls (n = 33) | 25.724 | 3.4560 |
Table 3.
Comparison of Notch Width Index, Medial and lateral tibial slope and Patellar tendon tibial shaft angle between genders.
| Parameter | Sex | Mean | Std. Deviation | p value |
|---|---|---|---|---|
| Notch Width Index | Males(n = 16) | 0.26338 | 0.035189 | 0.796 |
| Females (n = 17) | 0.26000 | 0.038830 | ||
| Medial Tibial Slope | Males(n = 16) | 5.100 | 1.6054 | 0.617 |
| Females (n = 17) | 4.824 | 1.5425 | ||
| Lateral Tibial Slope | Males(n = 16) | 4.950 | 1.3948 | 0.070 |
| Females (n = 17) | 4.059 | 1.3309 | ||
| Patellar Tendon Tibial Shaft Angle | Males(n = 16) | 27.225 | 1.6503 | 0.448 |
| Females (n = 17) | 27.841 | 2.8271 |
Fig. 3.
(a) Receiver operating characteristics curve for PTTS angle to analyse the optimal cut off point (b) Receiver operating characteristics curve for NWI angle to analyse the optimal cut off point.
4. Discussion
Anthropometric factors related to tibio-femoral geometry have been extensively studied in western literature with few Indian studies evaluating the role of tibial plateau slope. PTTS angle is another factor determining the anterior shear force at the proximal tibia and hence implicated in ACL injury. Comparison of these factors in noncontact ACL injury and in control subjects showed statistically significant differences in the NWI and PTTS angle. Contrary to many previous studies,8, 9 MTS and LTS did not show a statistically significant difference between the two groups. This could be secondary to inaccuracy in determining the proximal tibial anatomic axis (PTAA) due to short sagittal sections of MRI.8 A minimum of 150 mm has to be covered below the articular surface to accurately determine the PTAA 10. However, in the present study distance upto 6 cm (60 mm) was considered due to incomplete coverage of tibia in MRI knee images. Also, the measurement of small angles in cases of lateral and medial tibial slopes could lead to observer related variations. Stijak et al. 8 found greater LTS in patients with ACL rupture and a greater MTS in ACL intact population indicating opposing effects of the LTS and MTS on the ACL lesion.
Female athletes are more prone to incur non‐contact ACL injury than their male counterparts, according to previous studies 11, 12 Gender comparison of the anatomical factors have showed a narrow femoral notch,13 increased tibial slope 6, 14 and increased PTTS angle 3 in females. However, in our study, there was no statistically significant differences in NWI, MTS, LTS and PTTS angle between the genders. Although the notch width index is lower and PTTS angle is larger in females, the differences are not statistically significant. Similar findings regarding notch width index between genders was also observed by Teitz et al.15 Tillman et al. 16 also did not find any significant differences in NWI between male and female cadaver femora. Higher rate of ACL injury in women has also been attributed to various other factors. Zelisko et al. [17] proposed a higher quadriceps angle due to a wider pelvis in women as a contributing factor for ACL injury. Presence of estrogen and progesterone receptors on ACL with hormonal influences on ACL injury has also been proposed.17 Further studies with larger sample size and incorporating these factors are required to study the gender differences in Indian population.
PTTS angle varies inversely with knee flexion angle with higher angles increasing the anterior shear force at the proximal end of tibia. Previous studies have evaluated the PTTS angle at varying degrees of knee flexion with weight bearing and non-weight bearing conditions. Nunley et al. 3 found that there was an inverse relationship between PTTS angle and knee flexion angle on lateral radiographs with weight bearing. However, in our study, the knee flexion angle is at a constant of 10° with PTTS angle being evaluated in cases and controls, which showed a statistically significant difference. ROC curve constructed showed cut off points at 26.7 with a sensitivity of 67% and a specificity of 49%.
NWI has been studied in cadavers,18 radiographs 13, 19, 20 and MRI.21 Significantly narrower notch width index in cases of non contact injury as compared to controls found in our study is in agreement to previous studies.13, 19, 21 La Parde and Burnett et al.22 in a two year prospective study found ACL rupture in six knees among 40 knees with stenosis of intercondylar notch, whereas a single ACL tear was seen in 375 knees with normal notch size. A review of literature regarding the risk factors for ACL injury by Smith et al. has observed that the majority of studies have found a relationship between NWI or notch width and ACL injury.23 Wada et al. 18 found a significant correlation between NWI, ACL tear and the severity of osteoarthritis. The higher rate of ACL tear in patients with narrow femoral notch is not seen in the reconstructed knee, which could suggest the presence of a smaller ACL in narrow notches.20 A reduced NWI was measured on MRI in skeletally immature patients with ACL injury.5 The mean value of NWI is higher in our study as compared to previous studies. Souryal et al. 19 found a mean notch width index of 0.23 in cases of anterior cruciate ligament injury on radiographs, where as in our study the mean NWI was seen to be 0.26. This could be secondary to racial differences and variation in imaging modality. Various other indices like Notch shape index, Notch area index and other distal femoral morphometric parameters like intercondylar height, medial and lateral condylar width, epicondylar width have been studied.2, 16 However, NWI is the most commonly studied distal femoral morphometric parameter. ROC curve for NWI showed an optimal cut off value of 0.263 with a sensitivity of 88% and a specificity of 52%.
The role of studying these anatomical risk factors is predominantly in preventing re-injury in a patient with ACL tear and in preventing ACL injury in the contralateral knee. Patients with NWI less than 0.263 and PTTS angle of greater than 26.7° could undergo lifestyle modification with avoidance of specific at-risk positions and motions. Role of knee braces is controversial. Control of obesity and physiotherapy also plays an important role. Exercises preventing quadriceps dominance (in relation to hamstring strength) are used in ACL injury prevention training programmes. Conditioning programmes increasing muscular flexibility, restoring normal range of motion are also used in physiotherapy.
Studies have shown a statistically significant correlation between the patient height and femoral bicondylar width.20 In our study, controls and cases were age and sex matched, however they were not matched for other factors which could be implicated in ACL injury like height, weight, body mass index. This could be a limitation of the study. Other limitations were smaller sample size and lack of correlation with corresponding radiographs.
5. Conclusion
We found that a narrow Notch width index and increased Patellar tendon tibial shaft angle are predictors of ACL injury. PTTS angle which has been studied as a function of knee flexion angle, can itself be an independent predictor of ACL injury (at a constant knee flexion angle) and this has been a novel addition by the study. We found the lateral tibial slope and medial tibial slope measurements on MRI less accurate with 2 dimensional imaging and could be offset with the emerging 3 dimensional tools. Future research with larger sample size and multi-centric coordination with involvement of various departments is necessary in Indian population comparing the risk factors contributing to the complex clinical problem of ACL injury.
Authors contributions
SK contributed for the concept of the study, data collection, drafting and revising the article and final approval. CT and AK contributed for data collection, drafting of the article and final approval.
Funding
None.
Conflict of interest
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
References
- 1.Griffin Letha Y., Agel Julie, Albohm Marjorie J. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000;8:141–150. doi: 10.5435/00124635-200005000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Murshed K.A., Ciçekcibaşi A.E., Karabacakoğlu A., Seker M., Ziylan T. Distal femur morphometry: a gender and bilateral comparative study using magnetic resonance imaging. Surg Radiol Anat. 2005;27(April (2)):108–112. doi: 10.1007/s00276-004-0295-2. [DOI] [PubMed] [Google Scholar]
- 3.Nunley Ryan M., Wright Donna, Renner Jordan B., Yu Bing, Garrett William E. Gender comparison of patellar tendon tibial shaft angle with weight bearing. Res Sports Med. 2003;11:173–185. [Google Scholar]
- 4.Bisson L.J., Gurske-DePerio J. Axial and sagittal knee geometry as a risk factor for noncontact anterior cruciate ligament tear: a case-Control study. Arthrosc J Arthrosc Relat Surg. 2010;26(July (7)):901–906. doi: 10.1016/j.arthro.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 5.Domzalski Marcin, Grzelak Piotr, Gabos Peter. Risk factors for Anterior Cruciate Ligament injury in skeletally immature patients: analysis of intercondylar notch width using Magnetic Resonance Imaging. Int Orthop. 2010;34(5):703–707. doi: 10.1007/s00264-010-0987-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hashemi J., Chandrasekhar N., Gill B. The geometry of the tibial plateau and its influence on the biomechanics of the tibiofemoral joint. J Bone Joint Surg. 2008;90(12):2724–2734. doi: 10.2106/JBJS.G.01358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yu Bing, Garrett William E. Mechanisms of non-contact ACL injuries. Br J Sports Med. 2007;4(August):i47–i51. doi: 10.1136/bjsm.2007.037192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stijak L., Herzog R.F., Schai P. Is there an influence of the tibial slope of the lateral condyle on the ACL lesion? A case-control study. Knee Surg Sports Traumatol Arthrosc. 2008;16(February (2)):112–117. doi: 10.1007/s00167-007-0438-1. [DOI] [PubMed] [Google Scholar]
- 9.Dare D.M., Fabricant P.D., McCarthy M.M. Increased lateral tibial slope is a risk factor for pediatric anterior cruciate ligament injury: an MRI-based case-control study of 152 patients. Am J Sports Med. 2015;43(July (7)):1632–1639. doi: 10.1177/0363546515579182. [DOI] [PubMed] [Google Scholar]
- 10.Brazier J., Migaud H., Gougeon F., Cotten A., Fontaine C., Duquennoy A. Evaluation of methods for radiographic measurement of the tibial slope: a study of 83 healthy knees. Rev Chir Orthop Reparatrice Appar Mot. 1996;82(3):195–200. [PubMed] [Google Scholar]
- 11.Arendt E., Dick R. Knee injury patterns among men and women in collegiate basketball and soccer: NCAA data and review of literature. Am J Sports Med. 1995;23(6):694–701. doi: 10.1177/036354659502300611. [DOI] [PubMed] [Google Scholar]
- 12.Lindenfeld T.N., Schmitt D.J., Hendy M.P., Mangine R.E., Noyes F.R. Incidence of injury in indoor soccer. Am J Sports Med. 1994;22:354–371. doi: 10.1177/036354659402200312. [DOI] [PubMed] [Google Scholar]
- 13.Uhorchak J.M., Scoville C.R., Williams G.N. Risk factors associated with noncontact injury of the anterior cruciate ligament: a prospective four-year evaluation of 859 West Point cadets. Am J Sports Med. 2003;31(6):831–842. doi: 10.1177/03635465030310061801. [DOI] [PubMed] [Google Scholar]
- 14.Beynnon B.D., Hall J.S., Sturnick D.R. Increased slope of the lateral tibial plateau subchondral bone is associated with greater risk of noncontact ACL injury in females but not in males: a prospective cohort study with a nested, matched case-control analysis. Am J Sports Med. 2014;42(May (5)):1039–1048. doi: 10.1177/0363546514523721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Teitz C.C., Lind B.K., Sacks B.M. Symmetry of the femoral notch width index. Am J Sports Med. 1997;25(September–October (5)):687–690. doi: 10.1177/036354659702500517. [DOI] [PubMed] [Google Scholar]
- 16.Tillman M.D., Smith K.R., Bauer J.A., Cauraugh J.H., Falsetti A.B., Pattishall J.L. Differences in three intercondylar notch geometry indices between males and females: a cadaver study. Knee. 2002;9(February (1)):41–46. doi: 10.1016/s0968-0160(01)00135-1. [DOI] [PubMed] [Google Scholar]
- 17.Zelisko J.A., Noble H.B., Porter M. A. comparison of men's and women's professional basketball injuries. Am J Sports Med. 1982;10(September–October (5)):297–299. doi: 10.1177/036354658201000507. [DOI] [PubMed] [Google Scholar]
- 18.Wada M., Tatsuo H., Baba H., Asamoto K., Nojyo Y. Femoral intercondylar notch measurements in osteoarthritic knees. Rheumatology. 1999;38(June (6)):554–558. doi: 10.1093/rheumatology/38.6.554. [DOI] [PubMed] [Google Scholar]
- 19.Souryal T.O., Freeman T.R. Intercondylar notch size and anterior cruciate ligament injuries in athletes. A prospective study. Am J Sports Med. 1993;21(July–August (4)):535–539. doi: 10.1177/036354659302100410. [DOI] [PubMed] [Google Scholar]
- 20.Shelbourne K.D., Davis T.J., Klootwyk T.E. The relationship between intercondylar notch width of the femur and the incidence of anterior cruciate ligament tears. A prospective study. Am J Sports Med. 1998;26(3):402–408. doi: 10.1177/03635465980260031001. [DOI] [PubMed] [Google Scholar]
- 21.Domzalski M., Grzelak P., Gabos P. Risk factors for Anterior Cruciate Ligament injury in skeletally immature patients: analysis of intercondylar notch width using Magnetic Resonance Imaging. Int Orthop. 2010;34(5):703–707. doi: 10.1007/s00264-010-0987-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.LaPrade R.F., Burnett Q.M. Femoral intercondylar notch stenosis and correlation to anterior cruciate ligament injuries. A prospective study. Am J Sports Med. 1994;22(March–April (2)):198–203. doi: 10.1177/036354659402200208. [DOI] [PubMed] [Google Scholar]
- 23.Smith Helen C., Vacek Pamela, Johnson Robert J., Beynnon Bruce D. Risk factors for anterior cruciate ligament injury. a review of the literature — part 1: neuromuscular and anatomic risk. Sports Health. 2012;4(January (1)):69–78. doi: 10.1177/1941738111428281. [DOI] [PMC free article] [PubMed] [Google Scholar]