Abstract
Background
Global elimination of vaccine preventable diseases, such as measles, mumps and rubella is a priority. Many countries have reported diminishing of antibody titres against these diseases among young population as immunization coverage of adolescents and adults in not monitored. The objective of this study was to determine the susceptibility against measles, mumps and rubella among young adults.
Methods
In this cross-sectional study serological evidence of susceptibility to measles, mumps and rubella was determined by qualitative detection of IgG antibody titres by commercially available enzyme linked florescence assay (VIDAS, bioMerieux) in serum samples young adults.
Results
A total of 335 young individuals (mean age: 20.54 ± 1.37 years) participated voluntarily between May 2017 to September 2018, of which 183 (54.63%) were males. Seroprotection against measles, mumps and rubella were 87.16%, 82.69% and 79.10% respectively.
Conclusion
Serological surveillance is important to monitor immune status in population. Susceptibility of young adults to measles, mumps, and rubella indicates need for booster vaccination. With the recent launch of measles-rubella vaccination campaign in India, country specific data will be required to plan periodicity of such campaign, which in turn would be based on accumulation of susceptible individuals in a community. Lastly, inclusion of mumps vaccine in the national universal immunization program needs consideration.
Keywords: Measles, Mumps, Rubella, Vaccination, Immune response
Introduction
Global eradication of smallpox about five decades back laid a stepping stone for elimination of vaccine-preventable diseases. Launched in 1985, the Universal Immunization Programme in India provides vaccination against childhood tuberculosis, hepatitis B, diphtheria, pertussis, tetanus, poliomyelitis, Haemophilus influenza type B, and measles.1 Introduction of vaccines against rotavirus (2016) and rubella, as a part of measles-rubella vaccine (2017), has been implemented in a phased manner in certain states. Also, Japanese encephalitis has been rolled out in certain endemic states.1
Measles, mumps, and rubella are highly infectious acute febrile viral illnesses. The causative agent of measles is a single-stranded, negatively sensed RNA virus of the genus Morbillivirus and family Paramyxoviridae. Although availability of efficacious vaccine has resulted in 80% reduction in total deaths due to measles since 2000, 110,000 children, mostly younger than 5 years, died in the year 2017.2 An estimated 88% and 77% coverage for the first and second dose of measles vaccination, respectively, was reported by the World Health Organization and United Nations International Children's Emergency Fund survey in 2017.3
Mumps, which mainly affects salivary glands, is caused by a single-stranded, negatively sensed RNA virus of the genus Rubulavirus in the family Paramyxoviridae. Mumps infection spreads by droplet infection similar to measles and rubella. The disease peaks in winter, and several outbreaks have been reported across India.4, 5
Rubella or German measles is also caused by an enveloped, single-stranded positively sensed RNA virus of the genus Rubivirus in the family Togaviridae. It causes a self-limiting illness in children; however, if contracted by the expectant mother, it may lead to congenital defects in the fetus.
Global elimination of vaccine-preventable diseases such as measles, mumps and rubella is a priority. Many countries have reported diminishing of antibody titers against these diseases among young population.6, 7 A recent study has confirmed a total of 94 outbreaks of measles and rubella in the year 2013 in the state of Maharashtra, India, necessitating the need for serosurveillance of susceptible population and strengthening of vaccine coverage program.8 As immunization effectiveness in adolescents and young adults are not monitored, the objective of this study was to determine the susceptibility against measles, mumps and rubella among young adults.
Material and methods
A minimum sample size of 307 was calculated, assuming prevalence of measles, mumps, and rubella IgG seronegativity in young population to be 15%, absolute precision of 4%, and level of confidence to be 95%. The study population included young adults. The study was carried out in a microbiology laboratory of a tertiary care teaching institute. Five milliliters of whole blood sample was collected in a serum separator Vacutainer under aseptic conditions. The serum was separated and stored at −70 °C. In this cross-sectional study design, serological evidence of immunity to measles, mumps and rubella was determined by qualitative detection IgG antibodies by commercially available two-step enzyme-linked fluorescence assay (VIDAS, bioMerieux) on serum samples. The intensity of fluorescence was proportional to the concentration of IgG antibodies in the sample. The study results were reported as positive, negative, or equivocal based on the assay value or relative fluorescence value generated by the instrument on analysis.
Results
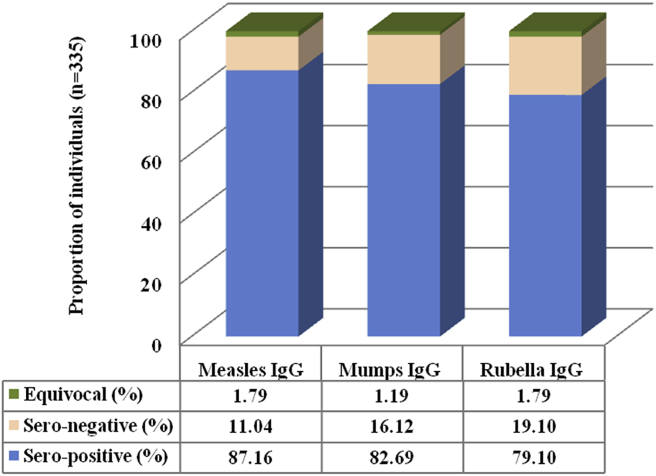
A total of 335 young adults participated voluntarily between May 2017 and September 2018, of which 183 (54.63%) were male, and the mean age of the participants was 20.54 (±1.37) years. IgG seropositivity to measles, mumps and rubella was 87.16%, 82.69%, and 79.10%, respectively. The proportion of individuals with positive, negative, and equivocal IgG antibodies against measles, mumps and rubella is shown in Fig. 1.
Fig. 1.
The proportion of study participants (n = 335) with positive, negative, and equivocal IgG antibodies against measles, mumps, and rubella.
Discussion
Measles, mumps and rubella are contagious diseases that spread by droplet infection. In India, more than 1.3 million children acquire these diseases, contributing nearly 36% to the global figures. Measles, mumps and rubella are a public health concern in developing countries, and breaking the chain of indigenous transmission is a priority. Monitoring of serological status of young adults against these vaccine-preventable infections is important, especially in women of reproductive age group as waning immunity is documented in this age group.7 The present study investigated susceptibility to measles, mumps and rubella in young adults by estimating IgG antibody levels. Our data revealed that 19.10% of individuals were susceptible to rubella. The seronegativity to measles and mumps were 16.12% and 11.4%, respectively. Gohil et al9 have earlier reported higher seronegativity to rubella-specific antibodies (12%) among college-going students in Mumbai than to measles (9%) and mumps (3%).
Recently, the European Centre for Disease Prevention and Control identified gaps in vaccination of teenagers and young adults as the surveillance data indicated that 80% of individuals of these age groups who contracted measles in 2017 were not vaccinated.10 Seroprotection against measles is lower when vaccine is received at 9 months than at 12 months.11 Furthermore, rubella vaccination in childhood is associated with lower rubella seroprevalence and shift of disease to adolescence and young adults.12, 13 A seroprevalence study conducted by Vaidya et al14 among 790 health science students demonstrated 32% susceptibility to mumps. Further to this, Vashishtha et al15 analyzed three studies of mumps surveillance in India and reported susceptibility rates between 32% and 80% in young children and adolescents. Combined measles, mumps, rubella (MMR) vaccine is recommended for adults by the Advisory Committee on Immunization Practices, USA.16
To tackle measles and rubella, the Government of India has initiated massive Measles-Rubella Vaccination Campaign in a phased manner in 2017, targeting children aged between 9 months and 15 years, with the aim to eliminate measles and control rubella/congenital rubella syndrome by 2020.17 Country-specific data are needed to ascertain periodicity of such a campaign, which would be based on accumulation of susceptible individuals in a community. Regarding seroprotection against mumps, the gaps continue to remain. Mumps vaccination is currently not included in our national Universal Immunization Programme. Worldwide, most mumps outbreaks, of late, have been reported in MMR-vaccinated young people.18 It is pertinent to note that severe complications such as orchitis, meningitis, and deafness occur in 10% of mumps-infected adolescents and young adults, as compared to less severe clinical manifestations such as fever and parotid swelling which are seen in children.19, 20
This study's results should be considered in the light of certain limitations. First, the study design was cross sectional, and the study was conducted among urban educated youth, who may not be representative of the rest of India. Although a prospective study would have been ideal to determine the efficacy of the vaccination strategy, our objective was to estimate the susceptibility to measles, mumps, and rubella among young persons. It would be difficult to comment whether protective antibody levels were due to vaccination or past infection. The history of MMR vaccination in the absence of individual participant vaccination records was difficult to elicit correctly in study participants because of recall bias. Nevertheless, the study highlights the existence of a considerable proportion of susceptible young adults, which may hinder the goal of elimination and/or control of vaccine-preventable diseases, namely, measles, mumps, and rubella.
In conclusion, serological monitoring of susceptibility to vaccine-preventable diseases is an essential tool to monitor immune status in general population. Susceptibility of young adults to measles, mumps, and rubella, as indicated by our study, reinforces need for multicentric serosurveillance and booster vaccination against these vaccine-preventable diseases.
Conflicts of interest
The authors have none to declare.
Acknowledgments
The authors acknowledge the technical support of Sub/LT IP Singh, Department of Microbiology, Armed Forces Medical College, Pune, and Sub/LT Indrajit Kumar, Command Hospital (SC), Pune.
References
- 1.Universal immunization program. National Health Portal, Government of India. Available online at: https://www.nhp.gov.in/universal-immunisation-programme_pg. Last assessed on 20 Dec 2018.
- 2.Measles factsheet, World Health Organization, Geneva. Available online at: https://www.who.int/news-room/fact-sheets/detail/measles.
- 3.India: WHO and UNICEF estimates of immunization coverage: 2017 revision. Available online at: www.who.int/immunization/monitoring_surveillance/data/ind.pdf.
- 4.Paul S., Mahajan P.B., Sahoo J., Bhatia V., Subba S.H. Investigating mumps outbreak in Odisha, India: an opportunity to assess the health system by utilizing the essential public health services framework. Am J Trop Med Hyg. 2017;96(5):1215–1221. doi: 10.4269/ajtmh.15-0593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Raut C.G., Sinha D.P., Jayaprakash H., Hanumiah H., Manjunatha M.J. Mumps disease outbreak in Davangere district of Karnataka, India. Indian J Med Microbiol. 2015;33(3):378–382. doi: 10.4103/0255-0857.158558. [DOI] [PubMed] [Google Scholar]
- 6.Gidding H.F., Quinn H.E., Hueston L., Dwyer D.E., McIntyre P.B. Declining measles antibodies in the era of elimination: Australia's experience. Vaccine. 2018;36(4):507–513. doi: 10.1016/j.vaccine.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 7.Gallone M.S., Gallone M.F., Larocca A.M.V., Germinario C., Tafuri S. Lack of immunity against rubella among Italian young adults. BMC Infect Dis. 2017;17(1):199. doi: 10.1186/s12879-017-2295-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vaidya S.R., Kamble M.B., Chowdhury D.T., Kumbhar N.S. Measles & rubella outbreaks in Maharashtra State, India. Indian J Med Res. 2016;143(2):227–231. doi: 10.4103/0971-5916.180214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gohil D.J., Kothari S.T., Chaudhari A.B. Seroprevalence of measles, mumps, and rubella antibodies in college students in Mumbai, India. Viral Immunol. 2016;29(3):159–163. doi: 10.1089/vim.2015.0070. [DOI] [PubMed] [Google Scholar]
- 10.European Centre for Disease Prevention and Control . ECDC; Stockholm: 2018. Measles and Rubella Surveillance – 2017.https://ecdc.europa.eu/en/publications-data/annual-measles-and-rubella-monitoring-report-2017 Available online at: [Google Scholar]
- 11.Singh R., John T.J., Cherian T., Raghupathy P. Immune response to measles, mumps & rubella vaccine at 9, 12 & 15 months of age. Indian J Med Microbiol. 1994;100:155–159. [PubMed] [Google Scholar]
- 12.Panagiotopoulos T., Antoniadou I., Valassi-Adam E. Increase in congenital rubella occurrence after immunisation in Greece: retrospective survey and systematic review. BMJ. 1999;319(7223):1462–1467. doi: 10.1136/bmj.319.7223.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang Z., Yan R., He H. Difficulties in eliminating measles and controlling rubella and mumps: a cross-sectional study of a first measles and rubella vaccination and a second measles, mumps, and rubella vaccination. PLoS One. 2014;9(2) doi: 10.1371/journal.pone.0089361. Published 2014 Feb 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vaidya S.R., Hamde V.S. Is it right time to introduce mumps vaccine in India's universal immunization program? Indian Pediatr. 2016;53(6):469–473. doi: 10.1007/s13312-016-0874-4. [DOI] [PubMed] [Google Scholar]
- 15.Vashishtha V.M., Yadav S., Dabas A. IAP position paper on burden of mumps in India and vaccination strategies. Indian Pediatr. 2015;52(6):505–514. doi: 10.1007/s13312-015-0666-2. [DOI] [PubMed] [Google Scholar]
- 16.Kim D.K., Riley L.E., Hunter P. Advisory committee on immunization Practices recommended immunization schedule for adults aged 19 Years or Older - United States, 2018. MMWR Morb Mortal Wkly Rep. 2018;67(5):158–160. doi: 10.15585/mmwr.mm6705e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Government of India DoH, Ministry of Health and Family Welfare, National Operational Guidelines 2017 . 2017. Introduction of Measles Rubella Vaccine (Campaign and Routine Immunization)http://www.nccmis.org/document/measles_rubella_vaccine_guidelines.pdf Available online at: [Google Scholar]
- 18.Gouma S., Koopmans M.P., van Binnendijk R.S. Mumps virus pathogenesis: insights and knowledge gaps. Hum Vaccines Immunother. 2016;12(12):3110–3112. doi: 10.1080/21645515.2016.1210745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Anderson R.M., Crombie J.A., Grenfell B.T. The epidemiology of mumps in the UK: a preliminary study of virus transmission, herd immunity and the potential impact of immunization. Epidemiol Infect. 1987;99(1):65–84. doi: 10.1017/s0950268800066875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Orlikova H., Maly M., Lexova P. Protective effect of vaccination against mumps complications, Czech Republic, 2007–2012. BMC Public Health. 2016;16:293. doi: 10.1186/s12889-016-2958-4. [DOI] [PMC free article] [PubMed] [Google Scholar]