Abstract
Background
Limb amputations are responsible for disability. We studied the outcomes of lower limb amputees in our daily practice.
Methods
This prospective analytical study over 7 years (January 2009–December 2015) included 70 amputees of lower limb. They were mainly male (73%), aged on average of 42.4 ± 18.8 years. The mean time of follow- up was 3.2 ± 1.9 years. We assessed disability on balance, walking, disability in daily life for patients with prosthesis, and the socio-economic impact of the amputation. Statistical analysis was performed with Chi2 and Mann-Whitney tests; a p-value ≤ 0.05 was considered statistically significant.
Results
The average Timed Up and Go Test was 18.5 s. Class II of Pohjolainen subjects were the most recovered (37%). The mean Houghton score in the 17 fitted patients was 6.2 ± 2.0. Socially, 90% of the patients no longer practiced leisure activities, and 4/53 patients were no longer in a couple. At the economic level, 87% of patients had a decreased monthly income. Factors that bear direct correlation to functional outcome of patients were the level of amputation, and the prosthesis fitting.
Conclusion
Lower limbs amputations entail adverse consequences at the functional and socio-economic level. Our country must review its policy on prosthetic fittings for amputees, and vote laws that involve private firms and government in socio-economic reintegration, and empowerment of these subjects.
Keywords: Lower limb amputation, Outcomes, Social reintegration
1. Introduction
A Limb amputation is a mutilating surgery and a public health problem.1,2 Its history is intimately linked to that of disability. Perceived as a failure by the surgeon, it leads to an alteration of the body image, chronic pain, psycho-affective disorders which lead to marital conflicts.2, 3, 4 Moreover, the possibilities of prosthetic fittings for amputees and their acceptance are often low in the low-income countries.5 Although a lot of studies have been conducted on the epidemiology and characteristics of limb amputations.5, 6, 7, 8, very few have been interested in the outcomes of amputees in their daily life in Africa. The aim of this study was to evaluate the functional, social and economic outcomes of lower limb amputees and to find associated factors to functional outcomes.
2. Patients and methods
2.1. Study design and population
This was a prospective, analytical study from January 2009 to December 2015, on lower limb amputees in orthopedic-traumatology department of Cotonou National Teaching hospital. This hospital is the level-1 referral hospital of Benin, a low-income country in West Africa. The health system of this country is third-level pyramid: the peripheral level (District or Communal health centers, supported by a regional referral hospital), the departmental level (departmental hospitals) and the national level (Cotonou National Teaching hospital, and mother and child hospital). In this country, the guaranteed minimum wage is 61.0 Euros monthly and the rate of poverty was 36.2%. There is limited rate of social coverage. All care services must be prepaid by the victim’s family outside the hospitalization fees. The cost of a daily hospitalization is 9.90 Euros for a common ward. The hospital has a rehabilitation department near the trauma unit, what facilitates rehabilitation of patients.
The inclusion criteria was patient aged of 15 years or most, with a lower limb amputation and a minimal follow-up of six months, who consent to participate to the study. For teenagers, their parents also gave their consent. Patients with a lower limb amputation before the period of the study and those with limb agenesis were excluded.
2.2. Variables
We appreciated the rate of prosthesis fitting, the functional, social and economic fate of the patients. Functionally, disability on balance was evaluated with the Timed ‘Up and Go' Test (TUGT).9 The disability on the walking was evaluate with the classification of Pohjolainen (Table 1).10 Houghton's score was used to assess disability in daily life.11 Patients were classified as patients with unsatisfactory rehabilitation (score <9) and patients with satisfactory rehabilitation (score ≥9).11 The social impact was assessed on the resumption of driving and work, adjustment of post, leisure activities practice, divorce, and dismissal. On the economic level we appreciated the monthly income after amputation (decreased, normal or increased).
Table 1.
Classification of Pohjolainen.
| Characteristics of the class | |
|---|---|
| Class I | Ambulating with a prosthesis but without other walking aids. |
| Class II | Independent at home, ambulating with a prosthesis but requiring one walking stick or crutch for outdoor activities |
| Class III | Independent indoors, ambulating with a prosthesis and one stick or crutch, but requiring two crutches outdoors and occasionally a wheelchair. |
| Class IV | Walking indoors with a prosthesis and two crutches or a walker, but requiring a wheelchair for outdoor activities. |
| Class V | Walking indoors only short distances, ambulating mostly with a wheelchair. |
| Class VI | Walking with aids but without a prosthesis |
| Class VII | Non ambulatory except in a wheelchair |
2.3. Ethical statement
This survey was conducted in compliance with the protocol Good Clinical Practices and Declaration of Helsinki principles. All included patients gave written informed consent to participate in the study after being informed about the purpose of study. We also received parental permission and the written consent of the parents about teenagers. Investigators guaranteed the total anonymity of the information derived from the research.
2.4. Statistical analysis
Statistical analysis was performed with EPI Info 7.1.5.0. Qualitative variables are expressed as frequencies. Quantitative variables are expressed as means ± standard deviation. The Chi2 of Pearson and the Mann-Whitney test were used to search correlation between the variables. A p-value ≤ 0.05 was considered statistically significant. The confidence interval was set at 95%.
3. Results
3.1. Sociodemographic and clinical characteristics
The study involved 70 patients, including 51 males and 19 females (male to female ratio = 2.7). They were mean aged of 42.4 ± 18.8 years (15–85 years). Laborers (40%) were most interested. The mean follow-up was 3.2 ± 1.9 years. The sociodemographic and clinical characteristics of these patients are summarized in Table 2, Table 3.
Table 2.
Sociodemographic characteristics of the patients (N = 70).
| Number of cases | Percentage | |
|---|---|---|
| Sex | ||
| Male | 51 | 73% |
| Female | 19 | 27% |
| Age group | ||
| [15–30 years [ | 29 | 42% |
| [30–45 years [ | 17 | 24% |
| [45–60 years [ | 10 | 14% |
| [60–75 years [ | 11 | 16% |
| [75–90 years [ | 3 | 4% |
| Matrimonial situation | ||
| Married | 53 | 76% |
| Single | 17 | 24% |
| Profession | ||
| Laborer | 28 | 40% |
| Craftsman | 14 | 20% |
| Civil servant | 12 | 17% |
| Trader | 8 | 12% |
| Student | 3 | 4% |
| Farmer | 2 | 3% |
| Driver of “Taxicab-Motorcycle” | 2 | 3% |
| Housewife | 1 | 1% |
Table 3.
Clinical characteristics of amputations (N = 70).
| Number of cases | Percentage | |
|---|---|---|
| Cause of amputation | ||
| Traumatic etiology | 48 | 70% |
| Diabetic foot | 15 | 21% |
| Peripheral vascular disease | 4 | 5% |
| Malignant bone tumor | 3 | 4% |
| Level of amputation | ||
| Transfemoral amputation | 35 | 50% |
| Transtibial amputation | 30 | 43% |
| Chopart amputation | 3 | 4% |
| Metatarsophalangeal disarticulation | 2 | 3% |
3.2. Prosthesis fitting and using of walking aids
Seventeen patients (24%) had a prosthesis fitting; they were 11 transfemoral amputees and 06 transtibial amputees. The mean delay between amputation and prosthesis fitting was 7.2 ± 2.1 months (4–12 months). Fifty two patients (70%) had a walking aids: 38 were using walking stick (54%), 11(16%), crutch and 3 (4%), wheelchair.
3.3. Functional outcomes
3.3.1. Disability on balance
The mean Timed ‘Up and Go' Test (TUGT) was 18.5 ± 5.0 s (10–34 s). The lower the amputation level was, the lower the TUGT was (p-value = 0.0001). Similarly, subjects with prosthesis had a longer TUGT than those without prosthesis (p-value = 0.03). But, there was no statistically significant relationship between the TUGT and sex, age, cause of amputation (p-value respectively of 0.4, 0.6, and 0.9)
3.3.2. Disability on walking
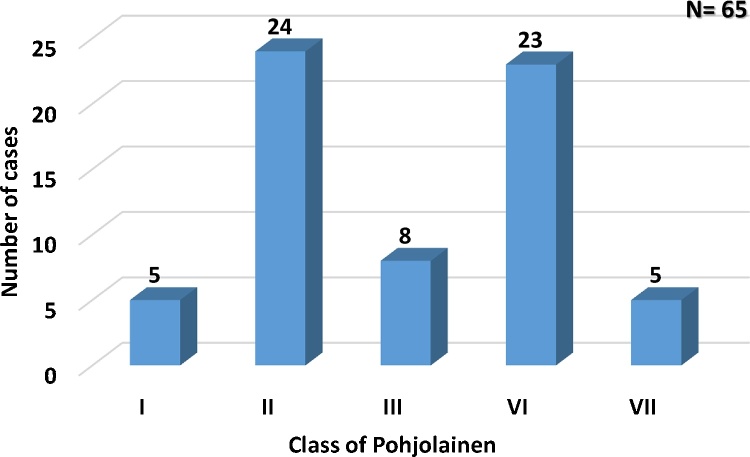
Among the 70 patients, five were completely autonomous and 65 could be classified according to Pohjolainen. Subjects of class II followed by those of class VI, were most found (Fig. 1)
Fig. 1.
Distribution of patients according to Class of Pohjolainen.
Male were predominantly class VI (21/47) while female were predominantly class II of Pohjolainen (8/18). But there was no significant relationship between theses variables (Chi2 = 7.4; p-value = 0.1). Similarly there wasn’t any link between the class of Pohjolainen and age (Chi2 = 17.7; p-value = 0.6), cause of the amputation (Chi2 = 3.3; p-valu = 0.5) and level of amputation (Chi2 = 8.1; p-value = 0.9). However, there was a statistically significant relationship between the fitting prosthesis and the disability on walking (p-value = 0.03; Chi2 = 10.8): fitted prosthesis patients were more autonomous on walking than unfitted subjects
3.3.3. Disability in daily life for fitted prosthesis patients
The mean Houghton score was 6.2 ± 2.0 (3–11). Rehabilitation was unsatisfactory in 14/17 patients. All those fitted after transfemoral amputation (11/11) had unsatisfactory rehabilitation; 3/6 fitted after a transtibial amputation had satisfactory rehabilitation. There was a statistically significant relationship between the amputation level and the Houghton score (Chi2 = 6.7; p-value = 0.009): the higher the level of amputation was, the greater was the risk of unsatisfactory rehabilitation. Fitting prosthesis wasn’t linked to the sex (Chi2 = 1.6; p-valu = 0.2), the age (Chi2 = 1.7; p-valu = 0.6), the cause of amputation (Chi2 = 1.2; p-valu = 0.3)
3.3.4. Social impact
Lower limb amputations had a negative impact on patient’s social life with disruption of all social parameters evaluated (Fig. 2).
Fig. 2.
Distribution of patients according to social parameters.
3.3.5. Economic impact
The monthly income of 61 patients (87%) has decreased. Eight (12%) have a monthly income equal to that before the limb loss and one (1%) has an increasing this monthly income after a post adjustment.
4. Discussion
The monocentric characteristic of the study is a weakness. Furthermore, there is a bias in assessing the functional outcomes of patients due to the lack of functional evaluation scales validated in our local languages, while most of the population is out of school. However, the sample size obtained by comprehensive survey of all adult lower limb amputees in the national referral hospital of our country is sufficient to allow statistical analysis and conclusive results. It’s therefore a beginning for another studies on this field in our country. This study is relevant because its provides data until then unavailable, about lower limb amputees outcomes in a sub-Saharan low-income country. It also permits us to compare our experience to those of other countries among the world, in order to improve our management of this kind of persons.
4.1. Fitting prosthesis
In this study, 17 patients (24%) had been fitted. This rate is above that of 9% reported by Tobomè et al. 6 in North Benin. Souna et al., and Tiandaza et al. reported respectively 6.97% and 20% of prosthesis fitting.11, 12 In developed countries, the prosthesis fitting is 100% covered by social security.13, 14 This explains that 60–80% of limb amputees are fitted.13, 14 In our context, prosthesis is still a luxury, reserved only for patients who can buy it either by their own, or after petty annoyances with insurance for those who are victims of road traffic accidents involving an insured car. Tibial prostheses cost 512.1–1250.7 Euros, which means 8.4–20.5 times the value of the guaranteed minimum wage in Benin (61.0 Euros). Femoral prostheses cost 709.3–1555.4 Euros, or 11.6–25.5 times, the guaranteed minimum wage in Benin. These prostheses are therefore not accessible to everyone, especially for our patients who were mainly laborers (40%). Moreover, the unavailability of prosthesis for all level of amputations in our practice obliges us to avoid some levels, especially around the knee (disarticulation or amputation of Gritti). To permit fitting prosthesis of most of amputees, some countries as India, made the choice of the ″Jaipur leg″ and ″Jaipur foot″, which are inexpensive to manufacture prostheses, and most suitable option for many patients in their experience. They also have social act, which helps amputees on their rehabilitation and socio-economic reintegration.15 However, it should be emphasized, that prosthesis fitting is not systematic; its opportunity is discussed depending on the case, in particular according to the comorbidities of the patient, his clinical state after the amputation, the functional results that one can expect and the motivation of the patient.16, 17, 18, 19, 20
4.2. Functional outcome
The balance of the lower limb amputees was correlated with the level of amputation (p-value = 0.0001) and the existence of a prosthesis (p-value = 0.03). For the latter parameter, the fitted subjects had a lower capacity for equilibrium than the unfitted subjects. This could be explained by unsatisfactory rehabilitation prior the fitting. Indeed, most patients had an unsatisfactory rehabilitation according to the Houghton score. Furthermore, when one looks better at the patients, all those fitted after transfemoral amputation had unsatisfactory rehabilitation. While, half of fitted after a transtibial amputation had satisfactory rehabilitation. Burger et al. 18 noted with transfemoral amputations, lower TUGT performance and less walking distance in 9 min compared to transtibial amputations. Similarly, Sansam et al. 16 identified the level of amputation as a very significant predictive factor (p < 0.001) of the mobility level evaluated 6 months after the amputation. The level of amputation is therefore a major predictive factor of the functional abilities, which could be expected after prosthesis fitting.16, 17 Moreover, this level is directly related to the energetic cost of walking with the prosthesis. The use of the prosthesis will be easier and its comfort greater, because the level of amputation is low.17 This is one of the reasons why some countries, such as the United States of America, have chosen to select patients requiring prosthetic fitting using the Medicare Functional Classification Levels.19
The class of Pohjolainen was statistically significantly related to the existence of prosthesis, with the fitted patients being more autonomous in their walking than the unfitted (p-value = 0.03). Above all, the prosthesis would allow an autonomy for the pelvic limb amputee, by facilitating his movements in a certain way.
The higher the level of amputation was, the greater the risk of unsatisfactory rehabilitation in case of prosthesis fitting was (p- value = 0.009). These results are in agreement with those of the literature and confirm the specificity of this simple clinical test for the evaluation of fitted patients after a lower limb amputation.21
4.3. Socio-economic impact
All the social parameters which were studied were disrupted, and most of the respondents had a decreased monthly income. According to the forensic assessment scale used in France and on which is based the insurance code used in Benin, permanent partial disability after lower limb amputation for unfitted patients varies from 8% to 70%.22 In this study, the population was predominantly young. It can be seen that the functional capacities and productivity of the most active age groups are greatly reduced by these amputations. The lower limb amputation thus affects not only the autonomy of the subject, but also contributes to increasing impoverishment in the low-income countries by striking mainly the active subjects.
5. Conclusion
Lower limb amputations are characterized in our context by a low rate of prosthesis fitting, disability and significant handicap with negative consequences on the functional, and socio-economic outcomes of the patients. A better policy on prosthetic fittings choice, with laws voting to involve everyone in socio-economic reintegration, and empowerment of these amputees is necessary in our country. The prevention of the main causes of these amputations and the application of the rules of their realization when indicated must always be the objectives aimed by traumatologists.
Conflict of interest
None.
Acknowledgments
The authors want to thank to Ahomadégbé B, Agonvenon E, Agossou B, Adon F, Awanou G, Dossou S, Ekpinsou C, Kanhonou C, Nakpan N, Sessou A, and Zoumenou H who helped to review the patients.
References
- 1.Menais P. Difficultés d'inclusion pour des usagers devant bénéficier d'appareillages au Togo. Kinesither Rev. 2015;15(161):45–50. [Google Scholar]
- 2.Muzembo Ndundu J., Motumbe Likita B. Prise en charge des amputés des membres inférieurs au centre orthopédique de Kalembe-lembe (Kinshasa):étude rétrospective sur six ans. J réadapt méd. 2012;32:114–118. [Google Scholar]
- 3.Luchetti M., Montebarocci O., Rossi N., Cutti A.G., Sutin A.R. Autobiographical memory and psychological distress in a sample of upper limb amputees. PLoS One. 2014;9(6):e99803. doi: 10.1371/journal.pone.0099803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karami G.R., Ahmadi Kh, Nejati V., Masumi M. Better mental component of quality of life in amputee. Iran J Publ Health. 2012;41(7):53–58. [PMC free article] [PubMed] [Google Scholar]
- 5.Chalya P.L., Mabula J.B., Dass R.M., Ngayomela I.H., Chandika A.B., Mbelenge N. Major limb amputations: a tertiary hospital experience in northwestern Tanzania. J Orthop Surg Res. 2012;7:18. doi: 10.1186/1749-799X-7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tobomè S.R., Hodonou A.M., Dadjo A.Y., Ahononga B.C., Haoudou R., Gayito R.C. Amputations de membres dans un hôpital de zone du Nord- Bénin: à propos de 122 cas. Med Afr Noire. 2015;62(3):165–172. [Google Scholar]
- 7.Sarvestani A.S., Azam A.T. Amputation: a Ten-Year survey. Trauma Mon. 2013;18(3):126–129. doi: 10.5812/traumamon.11693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sié Essoh J.B., Kodo M., Djè Bi Djè V.L. Limb amputations in adults in an Ivorian Teaching Hospital. Nig J Clin Pract . 2009;12(3):245–247. [PubMed] [Google Scholar]
- 9.Shoppen T. The Timed Up and Go Test: Reliability and Validity in Persons With Unilateral Lower Limb Amputation. Arch Phys Med Rehabil. 1999;80:825–828. doi: 10.1016/s0003-9993(99)90234-4. [DOI] [PubMed] [Google Scholar]
- 10.Pohjolainen T., Alaranta H., Karkkäinen M. Prosthetic Use and Functional and Social Outcome Following Major Lower Limb Amputation. Prosth Ortho Int. 1990;14:75–79. doi: 10.3109/03093649009080326. [DOI] [PubMed] [Google Scholar]
- 11.Souna B.S., Mamoudou A., Guigma A.Y., Ouhou N.H. Les causes des amputations des membres : Etude rétrospective et prospective de 87 cas d’amputations de membres. Mali Méd. 2009;24(4):11–16. [Google Scholar]
- 12.Tiandaza D.O., Randrianirina J.B., Ralison F., Ramadany A., Ravolamanana L. Vol. 1. 2010. pp. 35–41. (Amputation Majeure Des Membres (à Propos De 40 Cas Observés Au CHU De Mahajanga- Madagascar). e-Santé). [Google Scholar]
- 13.Calmels P., Béthoux F., Le-Quang B., Chagnon P.Y., Rigal F. Échelles d’évaluation fonctionnelle et amputation du membre inférieur. Ann Réadapt Méd Phys. 2001;44:499–507. doi: 10.1016/s0168-6054(01)00147-7. [DOI] [PubMed] [Google Scholar]
- 14.Menager D. Amputations du membre inférieur et appareillage. Encycl Méd Chir, Appareil locomoteur. 2002:15. 15–896-A-10. [Google Scholar]
- 15.Mysore H. The Jaipur Foot: India’s most popular prosthetic for amputees is not the latest in technology, but it's still the most suitable option for many patients almost 50 years after its development. IEEE Pulse. 2016;7(3):30–33. doi: 10.1109/MPUL.2016.2539798. [DOI] [PubMed] [Google Scholar]
- 16.Sansam K., Vera N., Rory C. Predicting walking ability following lower limb amputation: a systematic review of the literature. J Rehabil Med. 2009;41:593–603. doi: 10.2340/16501977-0393. [DOI] [PubMed] [Google Scholar]
- 17.Esquenazi A., DiGiacomo R. Rehabilitation after amputation. J Am Podiatr Med Assoc. 2001;91(1):13–22. doi: 10.7547/87507315-91-1-13. [DOI] [PubMed] [Google Scholar]
- 18.Burger H., Marincek C. Functional testing of elderly subjects after lower limb amputation. Prosthet Orthot Int. 2001;25(2):102–107. doi: 10.1080/03093640108726582. [DOI] [PubMed] [Google Scholar]
- 19.Twillert V.S., Geertzen J., Hemminga T., Postema K., Lettinga A. Reconsidering evidence-based practice in prosthetic rehabilitation: a shared enterprise. Prosthet Orthot Int. 2013;37(3):203–211. doi: 10.1177/0309364612459541. [DOI] [PubMed] [Google Scholar]
- 20.Roffman C.E., Buchanan J., Allison G.T. Predictors of non-use of prostheses by people with lower limb amputation after discharge from rehabilitation: development and validation of clinical prediction rules. J Physiother. 2014;60:224–231. doi: 10.1016/j.jphys.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 21.Devlin M., Pauley T., Head K., Garfinkel S. Houghton scale of prosthetic use in people with lower-extremity amputations: reliability, validity and responsiveness to change. Arch Phys Med;1. Rehabil. 2004;85(8):1339–1344. doi: 10.1016/j.apmr.2003.09.025. [DOI] [PubMed] [Google Scholar]
- 22.Association des Médecins Experts en Dommage corporel. Barème d’évaluation médicolégale; Paris: 2000. Société De Médecine légale Et De Criminologie De France, Association Des Médecins Experts En Dommage Corporel. Chapitre 2, Fonction Motrice. In: Société De Médecine légale Et De Criminologie De France; pp. 35–68. [Editions ESKA] [Google Scholar]