Abstract
Objectives
To investigate the effect of cementation, cement type and vent-holes on the marginal and internal fit of Zirconia (Zr) Copings.
Materials and methods
Extracted premolars (N = 100) were mounted in resin and prepared for Zr crowns. Samples were randomly divided into 5 groups (n = 20); A: No Cementation; B: Cementation with Glass-Ionomer (GI); C: GI + Vent-Holes; D: Cementation with Resin Cement (RC); E: RC + Vent-Holes. The copings were fabricated using semi sintered Zr Blocks with a standardized cement space of 20 µm. Groups C & E were designed to have 0.5 mm of Vent-Holes on the Buccal and Lingual Cusp Tips. The copings were tried, cemented, thermocycled, re-embedded in resin and cross sectioned into two halves. The copings were examined with 3D-Digital Microscope (HIROX, KH-7700, Tokyo, Japan) at 50-200X. The gaps were recorded at 9 predetermined points.
Results
The non-cemented groups showed statistically better fit compared to the cemented groups P < 0.05 except vs Group E (RC plus vent holes). No significance was found between the cemented groups P > 0.05. Copings with vent-holes showed statistically better fit than copings without holes P < 0.05.
Conclusion
Marginal and Internal gap values designed in the software programs differed than the actual values measured for the non-cemented copings. Cementation process also influenced the fit of the Zr copings, the resin cement being the more accurate. The addition of vent-holes on the occlusal surface improved the fit.
Keywords: Zirconia copings, Marginal fit, Internal fit, Zirconia cementation, Vent-holes
1. Introduction
All ceramic restorations have gained popularity due to the improvements in digital technologies and ceramic materials (Quintas et al., 2004). Often clinical situation dictates the selection of ceramic material, its design and fabrication method, and luting agent (Rosenstiel et al., 1998). Marginal and internal fit of a restoration is an important factor that is essential for the long term prognosis of any restoration. It decreases the associated risks of periodontal disease, secondary caries, pulpal sensitivity, and necrosis (Grenade et al., 2011, Kohorst et al., 2011) The literature recommends a cement space of 30 μm and 40 μm for the resin cements and zinc phosphate cements respectively. But in reality this space varies considerably (Abduo et al., 2010). Many factors had been described in the literature (Quintas et al., 2004, Rosenstiel et al., 1998, Grenade et al., 2011, Kohorst et al., 2011, Abduo et al., 2010) about this variation of cement space or marginal discrepancies. Probable reasons for marginal and internal misfit can be due to cementation technique, cement type, occlusal pressure applied during cementation, preparation angles, laboratory errors and absence of escape channels for the cement on the occlusal surface (Colpani et al., 2013, Wassell et al., 2002).
In previous studies, different cementation techniques had been evaluated to improve the fit of cast restorations like venting, escape channels, etching, die spacer application, cement application site and cement volume (Schwedhelm et al., 2003, Harrison et al., 1991, Cordoso et al., 2008). All these factors and techniques were reported to have improved the fit and adaptation of the restorations. Using vent-hole or escape channel should allow to minimize the hydrostatic pressure created by the luting agent between the intaglio surface of crown and coronal portion of tooth and thus improve the overall fit of the crown (Sallustio et al., 1992, Clark et al., 1995, Lindquist and Connolly, 2001).
The computer aided designing/computer aided manufacturing (CAD/CAM) focuses on precision and consistent fabrication of Zr crowns. Designing and manufacturing Zr crowns with CAD/CAM compensates for shrinkage due to sintering, it is reproducible and relatively economical (Kohorst et al., 2011, Lindquist and Connolly, 2001). However, studies reported on the marginal discrepancies and leakage in these restorations are scarce (Grenade et al., 2011, Kohorst et al., 2011, Abduo et al., 2010, Lindquist and Connolly, 2001, Beuer et al., 2009). Studies had been done on effects of preparation angles (Beuer et al., 2009), fabrication methods (Grenade et al., 2011), different luting materials and methods (Quintas et al., 2004), differences in the depths of preparations (Azar et al., 2011), common errors during preparations (Renne et al., 2012) and effect of different occlusal schemes for the fit of Zr copings (Habib et al., 2014). However, it is still important to identify and explore more factors such as occlusal vent-holes that can possibly improve the fit of Zr copings as well as techniques to improve this misfit.
Hence, the aim of this in-vitro research study was to investigate and compare the marginal and internal fit of zirconia copings both before and after cementation with two types of luting cements; and to investigate the effect of occlusal vent-holes on the overall fit of Zr copings. The Null Hypothesis was that there is no difference in the marginal and internal fit of Zr copings before and after cementation, with or without occlusal vent holes and for different types of cements used.
2. Materials and methods
A total sample of 100 minimally restored or sound extracted permanent upper premolar teeth with similar dimension in size were collected, stored in water containing 0.05% thymol to simulate the intra-oral condition and used as samples within thirty days after the extraction. The teeth were randomly divided into five groups of 20 in each group; Group A: copings with no cementation; Group B: copings with glass ionomer cementation; Group C: copings with glass ionomer cementation plus vent-holes; Group D: copings with resin cementation and Group E: copings with resin cementation plus vent-holes. Sample size for each group calculated was to be 20 with significance level of 0.05 and power calculation of 0.96 and also keeping in view the sample sizes used in various studies (Abduo et al., 2010, Colpani et al., 2013, Habib et al., 2014). Each tooth was embedded in self-curing resin (Ortho-Resin, DeguDent GmbH, Germany) to have a 3 cm diameter circular base, exposing the full crown with 2 mm of the coronal portion of root. Teeth were prepared with standard reduction (Shillingburg et al., 1997, Rosenstiel et al., 2006) by one experienced prosthodontist for all ceramic Zr crown, hence were similar in preparation design and reduction amount. An index made of silicone putty (Virtual Putty Regular, Ivoclar, Vivadent Inc.) of each tooth was fabricated before commencing the tooth reduction to be used for verification of the amount of reduction by sectioning it mesiodistally.
All the prepared teeth were scanned using digital scanner (Wieland Zenotec S107 Scanner, Dental Wings Inc., Canada). Designing of the copings was carried out with ZENOTEC CAD 4.3 software (Wieland Dental + Technik GmbH & Co. KG) to have thickness of 0.6 mm. For the Groups C and E, the design of the copings also incorporated vent-holes of 0.5 mm diameter on the tips of buccal and lingual cusps. The incorporation of the vent-holes during the designing of the coping was carried out to avoid breakage/fracture of the copings in case if the vent-holes were to be drilled after the fabrication. All the copings were designed to have a cement gap of 20 μm between fitting surface of the coping and prepared teeth except margins. Copings were then milled in Wieland Zenotec select hybrid (5-axis) (Wieland Dental + Technik-GmbH & Co. KG, Germany). Sintered in a furnace (Zenotec fire P1, Wieland Dental + Technik GmbH & Co. KG, Germany) by an experienced CAD/CAM technician.
Before placing the copings on the corresponding prepared teeth, they were checked by visual criteria for any discrepancies/impurities and steam cleaned. Marginal fit was then verified by visual and tactical methods with the tip of a sharp explorer. A fit checker (Occlude, Pascal Company, Inc., Washington USA) was used for further verification of fit and adjustments carried out with a high speed rotary (Diamond bur #BR31, Mani, Inc., Tochigi, Japan) under copious water supply. The fit checking process was carried out three times.
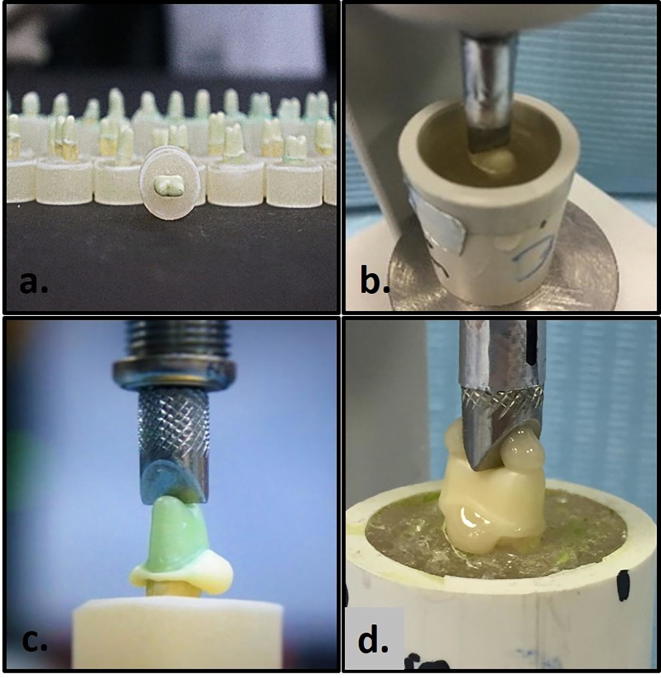
For Group A, the copings were placed under a constant load of 20 Newtons using a surveyor (Dentalfarm Manual Surveyor, A3005, Italy) without cementation and re-embedded in self-curing resin (Ortho-Resin, DeguDent GmbH, Germany) to facilitate sectioning afterwards. For the other groups the copings were cemented with GIC (KetacCem; 3M ESPE., Minnesota, USA) and resin cement (RelyX Unicem; 3M ESPE., Minnesota, USA) under 20 Newtons applied for 7 and 5 min respectively following manufacturer’s instructions and protocols as described by Quintas et al., 2004, Habib et al., 2014 (see Fig. 1).
Fig. 1.
(a) Prepared samples. (b) Re-Embedding of Group A (No Cementation) copings. (c) Cementation without vent holes. (d) Cementation with occlusal vent holes.
These copings were then thermocycled for 24 hrs in a thermocycling machine (Huber, SD Mechatronik Thermocycler, Germany) for 1500 cycles there by simulated approximately two months’ intraoral service (Gale and Darvell, 1999) and then re-embedded in resin to avoid the dislodgement during sectioning. Samples were then cross-sectioned into equal mesial and distal halves using precision saw (Isomet-2000, Precision saw, Buehler, USA). Two of the samples were excluded because of distortion.
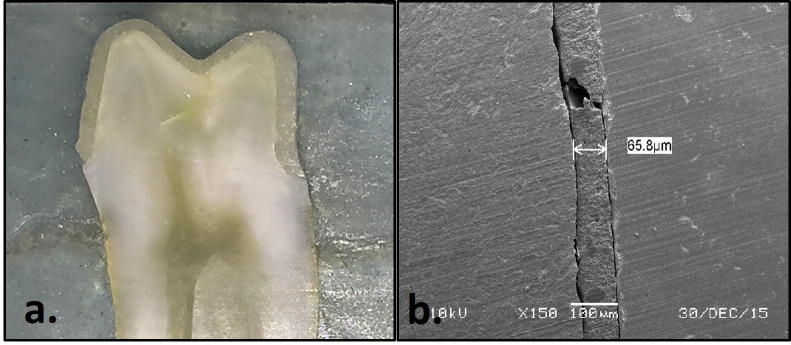
Each half of the sectioned specimen labeled a and b. 3D digital microscope (HIROX, KH 7700, Tokyo, Japan) was used for examining the sectioned halves with the exposed surfaces parallel to the examination table of the microscope. Cement space and thickness between the fitting area of a coping and the coronal portion of the tooth was measured at 50-200X at 9 points for each of the sectioned half as described by Habib et al. (2014) (see Figs. 2, 3 and Table 1).
Fig. 2.
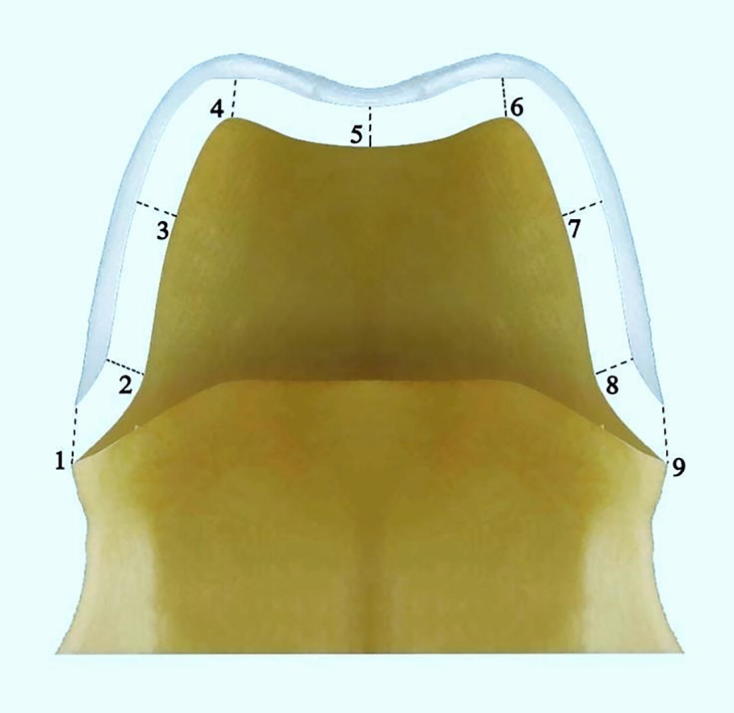
9 predetermined areas for measurements.
Fig. 3.
(a) Sectioned specimen half. (b) Digital Microscopic Reading.
Table 1.
Details of 9 areas of measurements for Zirconia copings.
| Point | Abbreviation | Description |
|---|---|---|
| 1 | BMG | Buccal Marginal Gap. The perpendicular distance from the edge of the coping to the buccal finish line |
| 2 | MBC | Mid-buccal chamfer. The perpendicular distance from the internal surface of the coping to the line angle formed between the buccal axial wall and floor of the crown margin |
| 3 | MBAW | Mid-buccal axial wall. The perpendicular distance from the internal surface of the coping to the mid-point of the buccal axial wall |
| 4 | BCT | Buccal cusp tip. The perpendicular distance from the internal surface of the coping to the mid-point of the buccal cusp tip |
| 5 | CG | Central groove. The perpendicular distance from the internal surface of the coping to the mid-point of the occlusal central groove |
| 6 | PCT | Palatal cusp tip. The perpendicular distance from the internal surface of the coping to the mid-point of the palatal cusp tip |
| 7 | MPAW | Mid-palatal axial wall. The perpendicular distance from the internal surface of the coping to the mid-point of the palatal axial wall |
| 8 | MPC | Mid-palatal chamfer. The perpendicular distance from the internal surface of the coping to the mid-point of the palatal chamfer |
| 9 | PMG | Palatal marginal gap. The perpendicular distance from the edge of the coping to the palatal finish line |
2.1. Statistical tests
All the data was analyzed with SPSS V20.0.1 software package (SPSS, Inc., Chicago, IL, USA) with predetermined significance level at p < 0.05. Mean of the two measurements for each sectioned sample was taken as final reading for each sample. Descriptive statistics of the 9 measured areas for all groups were completed and analyses carried out using ANOVA, Scheffe and Post Hoc Tukeys tests.
3. Results
Table 2 describes the descriptive statistics for all the experimental groups. The lowest mean gap was recorded for no cementation (group A 126.11 ± 67.95 µm). Among the (cemented groups) resin with vent hole showed the least gap (group E 135.54 ± 63.31 µm) and GI without vent holes exhibited the most gap (group B 164.63 ± 79.51 µm).
Table 2.
Mean values (standard deviation) of the marginal and internal gaps for the Five experimental groups (n = 100).
| Group | Description | *Overall mean | Standard deviation | 95% Confidence interval for mean |
Minimum | Maximum | |
|---|---|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||||
| A (n = 20) | No cement | 126.11 | 67.95 | 116.11 | 136.10 | 29 | 336 |
| B (n = 20) | GIC without holes | 164.63 | 79.51 | 152.93 | 176.32 | 27 | 435 |
| C (n = 18) | Resin without holes | 143.04 | 57.52 | 134.11 | 151.96 | 39 | 269 |
| D (n = 20) | GIC with holes | 159.58 | 66.84 | 149.74 | 169.40 | 12 | 294 |
| E (n = 20) | Resin with holes | 135.54 | 63.31 | 126.23 | 144.85 | 36 | 336 |
| Total (n = 98) | 145.84 | 69.01 | 141.27 | 150.39 | 12 | 435 | |
Mean gap was measured in micrometers (µm).
Generally, samples cemented with resin cement showed smaller gap than the (GI groups) for both with and without vent-holes copings (Table 2). Similarly, the samples with the vent holes showed least gap for both cements, however, statistically no significance was observed (Table 2, Table 3).
Table 3.
Multiple comparisons of the means of gap between 5 groups by *Post Hoc Tukey test.
| Groups | A | B | C | D | E |
|---|---|---|---|---|---|
| A | _ | 0.000 | 0.009 | 0.000 | 0.325 |
| B | 0.000 | _ | 0.000 | 0.851 | 0.000 |
| C | 0.009 | 0.000 | _ | 0.012 | 0.590 |
| D | 0.000 | 0.851 | 0.012 | _ | 0.000 |
| E | 0.325 | 0.000 | 0.590 | 0.000 | _ |
p value was significant at p < 0.05.
Group A had significantly lower mean values than the mean values of all the other groups. However, with Post Hoc Tukeys test this difference was significant (p < 0.05) only for groups B, C, D and not for group E (p = 0.325) (Table 3). A statistically significant difference (p < 0.05) was found between the Group B (GIC) Vs Group C (Resin) and Group D (GIC + vent-holes) Vs Group E (Resin + vent-holes). However, no significant difference was found within the same type of cement, with or without vent-holes, though the mean marginal gap values were less for the groups with vent-holes (147.56 ± 65.07 µm) in comparison to the groups without vent-holes (153.83 ± 68.51 µm).
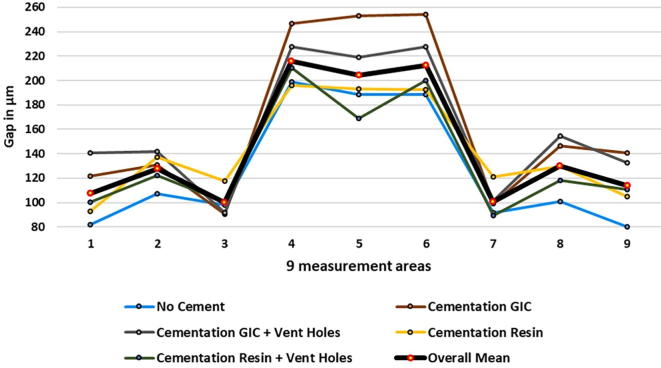
The least gap resulted at buccal axial wall (Area 3) not at the margins (Areas 1 and 9) (Fig. 4). The greatest gap was observed at the buccal cusp tip (Area 4). The Post-Hoc Tukey’s analysis revealed significant difference (p < 0.05) between areas 4, 5 6 and the rest of the areas. The gaps recorded for the copings having vent-holes were generally less than the copings without vent-holes if the same kind of cement was used. However, between the groups for with in areas 4, 5 and 6 showed non-significant differences between the cementation groups for GIC with or with our vent-holes and Resin with or without vent-holes (Table 4).
Fig. 4.
Comparison of the mean values of gaps for the five groups at 9 measured areas.
Table 4.
Multiple comparisons with Scheffe Test between 4, 5, and 6 areas for the groups with and without vent holes.
| Areas | GIC without holes (N = 20) | Resin without holes (N = 18) | GIC with holes (N = 20) | Resin with holes (N = 20) | |
|---|---|---|---|---|---|
| 4 | Resin without holes | 0.018 | – | 0.235 | 0.809 |
| GIC with holes | 0.684 | 0.235 | – | 0.733 | |
| Resin with holes | 0.145 | 0.809 | 0.733 | – | |
| 5 | Resin without holes | 0.043 | – | 0.682 | 0.687 |
| GIC with holes | 0.389 | 0.682 | – | 0.107 | |
| Resin with holes | 0.001 | 0.687 | 0.107 | – | |
| 6 | Resin without holes | 0.002 | – | 0.158 | 0.952 |
| GIC with holes | 0.418 | 0.158 | – | 0.374 | |
| Resin with holes | 0.010 | 0.952 | 0.374 | – | |
4. Discussion
Based on the results of this study, the mean gap for the cemented groups was found to be greater than the non-cemented group therefore, the null hypothesis was rejected. The cement thickness was also greater than 30 µm as reported by Kious et al. (2009) where they measured the film thickness of luting cements between two glass cylinders. This increased cement thickness may be a result of hydraulic pressure being developed during cementation procedure. The 145.84 ± 69.01 µm overall mean value of the groups is similar to those reported previously (Moldovan et al., 2011, Wakabayashi et al., 2005, Gonzalo et al., 2009).
In this study the non-cemented copings showed considerably larger average gap of 126 µm (range of 29–336) than 20 µm (default gap set in the software). In a clinical situation the crowns are always cemented, however, this group was included to evaluate the effect of cementing procedure and to see whether the default gap in the CAD-CAM software was produced accurately in the manufactured copings or not. The results indicate that the digital systems currently available needs improvements in their reproducibility and accuracy of fabricating prostheses and therefore some clinical adjustments are still needed to improve their fit. However, this must be noted that clinically this difference between the actual gap and the default gap in the software in microns is almost undetectable.
The current study results showed that the marginal and internal misfit was generally greater for the cemented groups as compare to the non-cemented copings confirming the fact that the cementation procedure could cause incomplete seating of prostheses. As expected the resin cement due to its less viscosity exhibited better adaptation than the GI cement. This result is in agreement with Clark et al. (1995) who reported better seating of crowns with resin cement than zinc phosphate cement.
Due to the chemical structure of resin cements they are more resistant to dissolution by oral fluids and subsequently offer resistance to plaque and microbial colonization. The commonly used resin cements are Bis-GMA, urethane dimethycrylate and PMMA based cements (Petropoulou et al., 2015). In the current study RelyX™ Unicem resin cement (phosphoric acid modified methacrylate monomers) was used. It is a dual-curing, self-adhesive universal resin luting cement with higher moisture tolerance, releases fluoride ions, high dimensional stability and a high degree of adhesion to the tooth structure (Giti et al., 2016). Besides it is the most commonly used self-adhesive resin cement (Ferracane et al., 2011).
In this study the least gap was observed at the buccal axial wall (99.80 µm) and maximum gap was measured under the buccal cusp (215.83 µm). The marginal gap, most important aspect of crown acceptability recorded in this study was on average 107.48 µm buccally (point 1) and 113.86 µm lingually (point 9) which is in the range of clinical acceptance as reported by various studies (Abduo et al., 2010, Colpani et al., 2013, Habib et al., 2014). However, the maximum gap recoded was 228 µm and 297 µm respectively which is twice the accepted values. Generally, lower values were recorded for the copings with vent holes. This observation is in line with earlier results by Harrison et al. (1991) who used Dicor crowns cemented with Zn phosphate cement. Similar findings were reported by Tjan and Sarkissin (1984) for placing internal escape channel for gold crowns.
An increased misfit was noticed under the occlusal surface (Areas 4, 5, 6). The presence of vent-holes should reduce the hydraulic pressure build up and should result in better adaptation of the copings (Schwedhelm et al., 2003, Sallustio et al., 1992, Clark et al., 1995). The results of this study supported this believe as gaps recorded for the copings having vent holes were generally less than the copings without vents, however, the difference was not statistically significant. The vent holes do appear to improve the seating of the crown and should be considered where clinical situation allows their use, especially in non-esthetic areas.
Some limitations of the current study that could have affected the results include the human variations in the preparation of the specimen teeth, designing of the copings with the digital software and digital microscopic measurements. The routine clinical procedure (static seating) for cementing a crown was adhered to during this study. However, the results of this study should be applied cautiously as different cements may behave differently due to their flow dynamics (Wadhwani et al., 2016) as well as various combinations of seating techniques like static seating, non-static seating (tapping) and dynamic seating (Cruz et al., 2008, Chan and Setchell, 1997) may also affect the flow of the cements used in the study. For the future scope of the current study, various resin cements can be evaluated and compared for their luting and adaptation properties when used for cementation of Zr crowns.
5. Conclusions
In this study, the marginal and internal gap values designed in the CAD/CAM software differed considerably from the actual values between the copings and the prepared teeth as measured with microscope. Cementation influenced the overall marginal and internal gap values and thus affected the fit of the Zr copings. The addition of vent-holes on the occlusal surface improved the marginal and internal fit though it was not statistically significant. Cementation with resin cement showed better fit of the Zr copings than GIC.
Conflict of interest
We have no conflict of interest to declare.
Acknowledgements
The authors are thankful to Mr. Bong for assistance with Digital Microscopic measurements and Mr. Nassr Maflehi for his help in the statistical analysis. The research project was approved and supported by the College of Dentistry Research Center (Registration # IR0163) and Deanship of Scientific Research at King Saud University.
Footnotes
Peer review under responsibility of King Saud University.
References
- Abduo J., Lyons K., Swain M. Fit of zirconia fixed partial denture: a systematic review. J. Oral. Rehabil. 2010;37:866–876. doi: 10.1111/j.1365-2842.2010.02113.x. [DOI] [PubMed] [Google Scholar]
- Azar M.S., Lehmann K.M., Dietrich H. Effect of preparation depth differences on the marginal fit of zirconia crown copings: an in-vitro study. Int. J. Prosthodont. 2011;24(3):264–266. [PubMed] [Google Scholar]
- Beuer F., Aggstaller H., Richter J. Influence of preparation angle on marginal and internal fit of CAD/CAM-fabricated zirconia crown copings. Quintessence. Int. 2009;40:243–250. [PubMed] [Google Scholar]
- Chan N.C., Setchell D.J. Die relief, seating methods and fit of full crowns. Singapore. Dent. J. 1997;22:29–34. [PubMed] [Google Scholar]
- Clark M.T., Richards M.W., Meiers J.C. Seating accuracy and fracture strength of vented and nonvented ceramic crowns luted with three cements. J. Prosthet. Dent. 1995;74:18–24. doi: 10.1016/s0022-3913(05)80223-9. [DOI] [PubMed] [Google Scholar]
- Colpani J.T., Borba M., DellaBona A. Evaluation of marginal and internal fit of ceramic crown copings. Dent. Mater. 2013;29:174–180. doi: 10.1016/j.dental.2012.10.012. [DOI] [PubMed] [Google Scholar]
- Cordoso M., Torres M.F., Rego M.R. Influence of application site of provisional cement on the marginal adaptation of provisional crowns. J. Appl. Oral. Sci. 2008;16:214–218. doi: 10.1590/S1678-77572008000300010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz M.A., Sorenson J.A., Johnson W.K. Effect of venting and seating techniques on the cementation of complete coverage restorations. Oper. Dent. 2008;33:690–695. doi: 10.2341/08-19. [DOI] [PubMed] [Google Scholar]
- Ferracane J.L., Stansbury J.W., Burke F.J. Self-adhesive resin cements—Chemistry, properties and clinical considerations. J. Oral. Rehabil. 2011;38:295–314. doi: 10.1111/j.1365-2842.2010.02148.x. [DOI] [PubMed] [Google Scholar]
- Gale M.S., Darvell B.W. Thermal cycling procedures for laboratory testing of dental restorations. J. Dent. 1999;27:89–99. doi: 10.1016/s0300-5712(98)00037-2. [DOI] [PubMed] [Google Scholar]
- Giti R., Vojdani M., Abduo J., Bagheri R. The comparison of sorption and solubility behavior of four different resin luting cements in different storage media. J. Dent. (Shiraz) 2016;17:91–97. [PMC free article] [PubMed] [Google Scholar]
- Gonzalo E., Suarez M.J., Serrano B. A comparison of the marginal vertical discrepancies of zirconium and metal ceramic posterior fixed dental prostheses before and after cementation. J. Prosthet. Dent. 2009;102:378–384. doi: 10.1016/S0022-3913(09)60198-0. [DOI] [PubMed] [Google Scholar]
- Grenade C., Mainjot A., Vanheusden A. Fit of single tooth zirconia copings: comparison between various manufacturing processes. J. Prosthet. Dent. 2011;105:249–255. doi: 10.1016/S0022-3913(11)60040-1. [DOI] [PubMed] [Google Scholar]
- Habib S.R., Asiri W., Hefne M.J. Effect of anatomic, semi-anatomic and non-anatomic occlusal surface tooth preparations on the adaptation of zirconia copings. J. Adv. Prosthodont. 2014;6:444–450. doi: 10.4047/jap.2014.6.6.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison K.M., Billy E.J., Pelleu G.B. Effects of an internal escape channel on a castable ceramic crown. J. Prosthet Dent. 1991;65:622–627. doi: 10.1016/0022-3913(91)90195-3. [DOI] [PubMed] [Google Scholar]
- Kious A.R., Roberts H.W., Brackett W.W. Film thickness of recently introduced luting cements. J. Prosthet. Dent. 2009;101:189–192. doi: 10.1016/S0022-3913(09)60026-3. [DOI] [PubMed] [Google Scholar]
- Kohorst P., Junghanns J., Dittmer M.P. Different CAD/CAM-processing routes for zirconia restorations: influence on fitting accuracy. Clin. Oral. Investig. 2011;15:527–536. doi: 10.1007/s00784-010-0415-9. [DOI] [PubMed] [Google Scholar]
- Lindquist T.J., Connolly J. In vitro microleakage of luting cements and crown foundation material. J. Prosthet. Dent. 2001;85:292–298. doi: 10.1067/mpr.2001.113705. [DOI] [PubMed] [Google Scholar]
- Moldovan O., Luthardt R.G., Corcodel N. Three-dimensional fit of CAD/CAM-made zirconia copings. Dent. Mater. 2011;27:1273–1278. doi: 10.1016/j.dental.2011.09.006. [DOI] [PubMed] [Google Scholar]
- Petropoulou A., Vrochari A.D., Hellwig E. Water sorption and water solubility of self-etching and self-adhesive resin cements. J. Prosthet. Dent. 2015;114:674–679. doi: 10.1016/j.prosdent.2015.06.002. [DOI] [PubMed] [Google Scholar]
- Quintas A.F., Oliveira F., Bottino M.A. Vertical marginal discrepancy of ceramic copings with different ceramic materials, finish lines, and luting agents: an in vitro evaluation. J. Prosthet. Dent. 2004;92:250–257. doi: 10.1016/j.prosdent.2004.06.023. [DOI] [PubMed] [Google Scholar]
- Renne W., McGill S.T., Forshee K.V. Predicting marginal fit of CAD/CAM crowns based on the presence or absence of common preparation errors. J. Prosthet. Dent. 2012;108:310–315. doi: 10.1016/S0022-3913(12)60183-8. [DOI] [PubMed] [Google Scholar]
- Rosenstiel S., Land M., Fujimoto J. Mosby Elsevier; St Louis: 2006. Contemporary Fixed Prosthodontics. [Google Scholar]
- Rosenstiel S.F., Land M.F., Crispin B.J. Dental luting agents: a review of the current literature. J. Prosthet. Dent. 1998;80:280–301. doi: 10.1016/s0022-3913(98)70128-3. [DOI] [PubMed] [Google Scholar]
- Sallustio F.W., Waskewicz G.A., Billy E.J. The effect of venting on the strength of Dicor and Hi-Ceram ceramic crowns. Int. J. Prosthodont. 1992;5:463–468. [PubMed] [Google Scholar]
- Schwedhelm E.R., Lepe X., Aw T.C. A crown venting technique for the cementation of implant supported crowns. J. Prosthet. Dent. 2003;89:89–90. doi: 10.1067/mpr.2003.66. [DOI] [PubMed] [Google Scholar]
- Shillingburg, H.T. Jr, Hobo, S., Whitsett, L.D., 1997. Principles of tooth preparations. In: Shillingburg, H.T. Jr, Hobo, S., Whitsett, L.D. (Eds.): Fundamentals of Fixed Prosthodontics third ed. Chicago, Quintessence, pp. 119–154.
- Tjan A.H.L., Sarkissian R. Internal escape channel: an alternative to venting complete crowns. J. Prosthet. Dent. 1984;52:50–56. doi: 10.1016/0022-3913(84)90181-1. [DOI] [PubMed] [Google Scholar]
- Wadhwani C., Goodwin S., Chung K.H. Cementing an implant crown: a novel measurement system using computational fluid dynamics approach. Clin. Implant. Dent. Relat. Res. 2016;18:97–106. doi: 10.1111/cid.12258. [DOI] [PubMed] [Google Scholar]
- Wakabayashi K., Sohmura T., Nakamura T. New evaluation method by microfocus radiograph CT for 3D assessment of internal adaptation of all ceramic crowns. Dent. Mater. J. 2005;24:362–367. doi: 10.4012/dmj.24.362. [DOI] [PubMed] [Google Scholar]
- Wassell R.W., Barker D., Steele J.G. Crowns and other coronal restorations: Try in and cementation of crowns. B.D.J. 2002;193:17–28. doi: 10.1038/sj.bdj.4801473. [DOI] [PubMed] [Google Scholar]