Abstract
Purpose
Procedures such as Periodontally Accelerated Osteogenic Orthodontics (PAOO) support the use of osteotomy to aid tooth movement and rapid distraction of the periodontal ligament by utilizing tissue engineering principles with periodontal regenerative surgery. The aim of this study was to evaluate and compare the amount of tooth movement and the associated changes in buccal bone morphology between corticotomy and flapless Micro-Osteoperforation (MOP) assisted orthodontic treatment.
Material and methods
A total of ten healthy patients between 18 and 25 years of age requiring orthodontic treatment were recruited for this clinical trial with a split mouth design. After orthodontic and periodontal examinations, Cone Beam Computed Tomography scans (CBCT) were done pre- (T1) and post- (T2) operatively for each patient to evaluate radiographic parameters such as buccal bone thickness, root resorption and dehiscence. Amount of tooth movement was also evaluated and compared.
Results
The canine-premolar distance, measured in a time interval of 3 months and over a follow-up period of 6 months, reduced significantly from T1 to T2 at both corticotomy and MOP sites. At the corticotomy site, there was a mean increase in bone thickness of 1.15 ± 0.3 mm at coronal region, 0.48 ± 0.1 mm at mid-root region and 0.15 ± 0.0 mm at apical region. This increase in bone thickness was statistically significant at coronal level (p = 0.001) and mid-root level (p = 0.02). Significant increase in bone thickness was observed at MOP site. While on intergroup comparison, the difference was statistically significant at coronal level (p = 0.01).
Conclusion
Both the techniques cause an increase in canine retraction in short period of time with almost no harm to periodontal structures. MOP being a flapless procedure allow clinicians to deliver an efficient orthodontic care.
Keywords: Tooth movement, Cone beam computed tomography, Orthodontics
1. Introduction
Orthodontic tooth movement is considered a ‘periodontal phenomenon’, as conventional orthodontic movements lead to periodontal ligament compression, thereby activating the dynamics of crestal bone resorption and apposition. Many patients with malocclusions are reluctant for orthodontic treatment because of its drawn out treatment time, which may precipitate into an increased risk of root resorption, dental caries, decalcification and gingival inflammation. In order to meet the constant demand of short treatment time while preserving the integrity of periodontal structures, an alternate treatment approach has been popularized known as corticotomy facilitated orthodontics. This technique was proposed by Kole in 1959, who suggested that performing surgical osteotomies in the alveolar process, weakens the cortical bone and facilitates orthodontic tooth movement (bony block movement). Later on Harold Frost in 1983 identified that, the molecular dynamics of osteogenesis in stressed bone is based on Regional Acceleratory Phenomenon (RAP) and not on the bony block movement. He recognized that surgical wounding of osseous hard tissues results in striking reorganization activity adjacent to the site of injury in osseous and soft tissue surgery. These physiologic healing events were further described by Yaffe et al. (1994). RAP results in a decrease in regional bone densities (osteopenia) in healthy tissues, whereas the volume of bone matrix remains constant. Based on this phenomenon, Wilcko et al. (2001) suggested a novel surgical technique called Periodontally Accelerated Osteogenic Orthodontics (PAOO). The authors assumed that the local osteopenia caused by the surgical trauma will reduce the resistance of bone to tooth movement and allow for the acceleration of such movement. Moreover, when tooth movement is combined with selective decortication, RAP is maximized. Thus, the PAOO technique was claimed to increase the range of tooth movement outside the original bony envelope by creating an additional space for the buccal movement of roots during orthodontic expansion with minimal root resorption and dehiscence as compared to conventional orthodontic tooth movement.
The only problem encountered with PAOO is its invasiveness and the accompanied post- operative pain and discomfort. To minimize this, Alikhani et al. (2015), proposed a simple and safe method i.e Micro-Osteoperforations (MOP’s) to accelerate tooth movement that harnesses and amplifies the patient’s normal biological response to orthodontic forces. In recent years, many studies have been carried out to evaluate the efficiency of corticototomy and MOP, on an individual basis, as adjunctive procedures along with fixed orthodontic treatment to accelerate the rate of tooth movement. But there have been no comparative studies evaluating the effectiveness of both the procedures. Also, there is paucity of literature about the buccal bone morphologic changes associated with these procedures.
So, the purpose of this prospective clinical trial was to evaluate and compare the amount of tooth movement between corticotomy and flapless MOP and to evaluate the associated buccal bone morphologic changes.
2. Material and methods
In this split mouth interventional study, a total of ten systemically and periodontally healthy patients between 18 and 25 years of age requiring orthodontic treatment were recruited. The sample was set up to use each patient as his own control, thereby increasing the power of small sample (Evans and Ildstad, 2001). The patients with Angle’s Class I and Class II molar relation and indicated for first premolar extraction with adequate width of attached gingiva were included in the study while the patients with periodontal destruction (as assessed by PPD ≥3mm and presence of CAL), severe craniofacial disorder such as cleft palate, those on anti-inflammatory drugs (over 2 months), uncontrolled diabetes, bleeding disorders and other systemic diseases were excluded from the study.
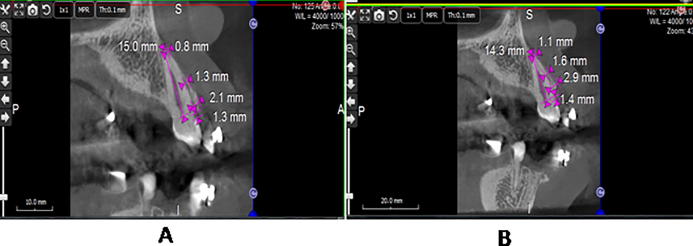
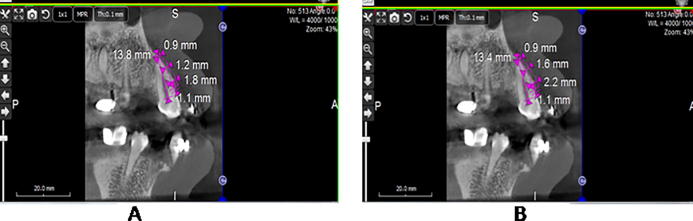
After recruitment, patients were examined by an Orthodontist (VV). Data collection included study casts, cephalometric and panoramic radiographs and clinical photographs. After the orthodontic examinations and investigations, a Periodontist (AA) carried out the periodontal examination and CBCT (KODAK 9000C and KODAK 9000C 3D Extraoral Imaging System, Carestream Health, Inc., France) was done for each patient to evaluate the buccal bone thickness, root resorption, dehiscence, before and after surgery (Fig. 1, Fig. 2). The patients were taken up for oral prophylaxis and oral hygiene maintenance instructions were given to them. The research protocol was accepted by the Institutional Ethics Committee and adhered to the provision of Helsinki declaration 1975, as revised in 2013. A written informed consent was procured from every patient after they were explained the study design and protocol.
Fig. 1.
CBCT Scans of Corticotomy site. A. Pre-operative (T1). B. Post-operative (T2).
Fig. 2.
CBCT Scans of Micro-osteoperforation site. A. Pre-operative (T1). B. Post-operative (T2).
2.1. Surgical procedure
Corticotomy site and MOP’s site (in total 20 sites) were assigned randomly by envelope method in each patient and all surgical procedures were performed by an experienced Periodontist (AK).
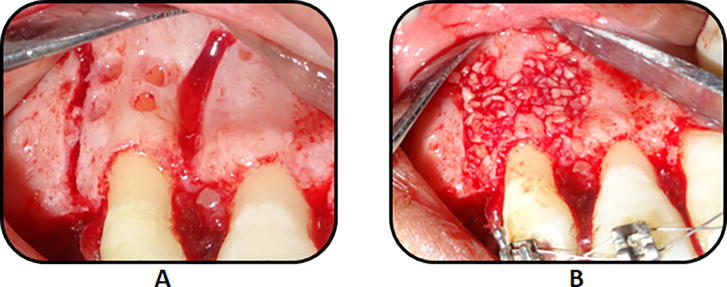
2.1.1. Corticotomy site (Fig. 3)
Fig. 3.
Surgical Pictures of corticotomy site. A. Corticotomy cuts. B. DFDBA graft placement.
After profound anesthesia, a full thickness mucoperiosteal flap was elevated extending 3–4 mm beyond the mucogingival junction. With the help of a surgical carbide bur no. 2, under proper irrigation with cold saline, vertical grooves were placed in the interradicular space, midway between the root prominences in the alveolar bone on the mesial and distal side of canine. These grooves extended from a point 2–3 mm away from the crest of the bone to a point approximately 4 mm beyond the apices of the roots. Semilunar corticotomy cuts were made joining these vertical cuts beyond the apices of the roots. After the placement of the corticotomy cuts, Demineralized Freeze Dried Bone Allograft (DFDBA)1 of particle size 500–1040 μm was placed with an effort not to place an excess amount, as it might interfere with flap replacement. Small round perforations of about 2 mm were made in between the corticotomy cuts which helped retain the graft material. The flap was adapted to normal position without tension and suturing was done. The sutures were left in place for 7–8 days and the patients were prescribed antibiotics for 7 days. No NSAID’s were prescribed post-operatively. The participants were instructed to rinse the oral cavity twice a day with chlorhexidine (0.12%) mouthwash and not to brush the operated area for 1 week.
2.1.2. Micro-Osteoperforation’s site (MOP’s) site (Fig. 4)
Fig. 4.
Surgical Pictures of micro-osteoperforation site. A. Micro-implants placed through the stent. B. Bleeding spots post implant removal.
After the corticotomy procedure, MOP was performed on the contralateral side. To determine exact location of MOP’s, a stent was prepared in 0.016 × 0.022 S.S wire extending from the molar tube to canine bracket of the side where MOP’s were to be performed and a RVG was taken. Local anesthetic spray was used prior to starting MOPs. Also a small puncture was made with a probe through the stent at the implant placement site until bone was felt and the depth of soft tissue (gums) was then measured with a periodontal probe. Accordingly, the length of implant was selected i.e. 6 mm, 7 mm or 8 mm long micro-implants which created MOP at least 3–4 mm deep and 1.5 mm wide. After proper micro-implant selection, proper position of stent was assured and the implants were inserted through the stent. Inserting all the three implants together assured proper site of implant placement, avoided excessive bleeding in between placements and consumed lesser time. The patient was asked to rinse with chlorhexidine solution (0.12%) and relax for 5min. The implants were then carefully removed by turning them in an anticlockwise direction, followed by stent removal. Bleeding spots were seen post implant removal. Bleeding was stopped by applying a pressure pack in that area. Similar procedure was carried out mesial to the canine between the roots of lateral incisor and canine but the number of MOP’s was dependent on the interdental space available between roots. Patient was again asked to rinse with chlorhexidine solution. Orthodontic retraction was then started 2 weeks after surgery; appliance activation was done every 2 weeks for 3 months. Clinical parameters (probing pocket depth, gingival recession) and radiographic parameters (buccal bone thickness, root resorption and dehiscence) were recorded pre- (T1) and post- (T2) treatment. Overall satisfaction of patient was also evaluated post-operatively by Visual Analogue Scale (VAS). Amount of canine distalization was estimated on study models at T1 and T2.
The CBCT scan was performed using a specific protocol in which the pixel size, slice increment and slice thickness were 0.2 mm for accurate 3D analysis. The DICOM files from the CBCT scan as shown in Fig. 1, Fig. 2 were used for all measurements which included:
-
(a)
Buccal bone thickness – Measured from the buccal bone up to the root at three levels i.e coronal, mid-root and apical level (Both at T1 and T2).
-
(b)
Root resorption – Difference in the distance from cemento-enamel junction up to root apex at T1 and T2.
-
(c)
Dehiscence – Measured from cemento-enamel junction up to the bone crest.
3. Statistical analysis
The statistical analysis was done using the Statistical Package for the Social Science (SPSS version 22, Armonk, NY: IBM Corp).The mean values of buccal bone thickness at coronal, mid-root, apical level at both the sites were calculated and compared using independent samples t-test. By using one way ANOVA, the difference in buccal bone thickness at all the three levels (coronal, mid-root and apical) on both the sites was estimated. The change in distance and angle were also compared between two groups from study models using t-test for independent samples.
4. Results
A total of ten patients, including 8 females and 2 males, with a mean age range of 21.9 ± 2.13 years, were recruited for this trial. In each patient one site was considered as corticotomy site and the contralateral as MOP site. Both the groups revealed that the procedures were well tolerated without any complication. The mean orthodontic treatment time at corticotomy sites was 5.75 ± 1.75 months, whereas for MOP sites, it was 6.50 ± 0.75 months. Slight discomfort was experienced by some patients within the first week after the procedure which was on expected lines especially on the corticotomy treated site. The patient satisfaction with the overall treatment was 9 on a VAS ranging from 1 (not pleased) to 10 (very pleased). Table 1a, Table1b shows the buccal bone thickness at pre- (T1) and post- (T2) treatment time in both the groups. The bone thickness increased significantly after performing corticotomy as well as after performing MOP.
Table 1a.
Comparison of level of buccal bone thickness pre- (T1) and post- (T2) treatment in both the groups.
| Level of buccal bone thickness | Pre (T1) Mean ± SD (in mm) |
Post (T2) Mean ± SD(in mm) |
T2-T1 (in mm) |
p value | |
|---|---|---|---|---|---|
| Corticotomy (n = 10) |
Coronal | 1.42 ± 1.0 | 2.57 ± 0.7 | 1.15 ± 0.3 | 0.001* |
| Mid-root | 1.06 ± 0.4 | 1.54 ± 0.5 | 0.48 ± 0.1 | 0.02† | |
| Apical | 0.9 ± 0.3 | 1.05 ± 0.3 | 0.15 ± 0 | 0.30‡ | |
| MOP (n = 10) |
Coronal | 1.35 ± 0.4 | 1.8 ± 0.5 | 0.45 ± 0.1 | 0.01† |
| Mid-root | 0.97 ± 0.2 | 1.32 ± 0.3 | 0.35 ± 0.1 | 0.03† | |
| ‘Apical | 0.88 ± 0.2 | 1.0 ± 0.4 | 0.12 ± 0.2 | 0.40‡ | |
p ≤ 0.001 statistically highly significant.
p ≤ 0.05 statistically significant.
Non significant.
Table1b.
Comparison of level of buccal bone thickness post-treatment (T2).
| Level of buccal bone thickness | Groups (Mean ± SD) |
p value | |
|---|---|---|---|
| Corticotomy (n = 10) (in mm) |
MOP (n = 10) (in mm) |
||
| Coronal | 2.57 ± 0.7 | 1.8 ± 0.5 | 0.01† |
| Mid-root | 1.54 ± 0.5 | 1.32 ± 0.3 | 0.2‡ |
| Apical | 1.05 ± 0.3 | 1.0 ± 0.4 | 0.7‡ |
| p value | 0.02† | 0.001* | |
p≤0.001 statistically highly significant.
p≤0.05 statistically significant.
Non significant.
Table 1a shows that at the corticotomy site, there was a mean increase in bone thickness of 1.15 ± 0.3 mm at coronal region, 0.48 ± 0.1 mm at mid-root region and 0.15 ± 0.0 mm at apical region. This increase in bone thickness was statistically highly significant at coronal level (p = 0.001) and mid-root level (p = 0.02) as calculated using paired samples t-test. At the MOP site, there was a mean increase in bone thickness of 0.45 ± 0.1 mm at coronal region, 0.35 ± 0.1 mm at mid-root region and 0.12 ± 0.2 mm at apical region. This increase in bone thickness was statistically significant at coronal level (p = 0.01) and mid-root level (p = 0.03) as calculated using paired samples t-test. On inter-group comparison, the post-treatment buccal bone thickness at corticotmy treated sites at coronal, mid-root, and apical levels were 2.57 ± 0.7 mm, 1.54 ± 0.5 mm and 1.05 ± 0.3 mm, while those at MOP treated sites were 1.8 ± 0.5 mm, 1.32 ± 0.3 mm and 1.0 ± 0.4 mm, respectively. The differences were statistically significant at coronal level and non-significant at the mid-root and apical levels (Table 1b).
Table 2 shows the comparison of canine–premolar distance between the two groups at pre- and post treatment. The distance reduced significantly from 6.31 ± 0.9 mm (T1) to 3.55 ± 0.7 mm (T2) at the corticotomy site which was a highly significant difference. At the MOP site, the distance reduced from 6.21 ± 0.8 mm (T1) to 3.84 ± 0.7 mm (T2) which was also a statistically significant difference.
Table 2.
Comparison of canine–premolar distance between the two groups at pre- and post- treatment.
| Time | Corticotomy (n = 10) (in mm) |
MOP (n = 10) (in mm) |
p value |
|---|---|---|---|
| Pre-treatment (T1) | 6.31 ± 0.9 | 6.21 ± 0.8 | 0.8‡ |
| Post-treatment (T2) | 3.55 ± 0.7 | 3.84 ± 0.7 | 0.4‡ |
| p value | 0.001* | 0.001* |
p≤0.001 statistically highly significant.
Non significant.
Table 3 depicts that root length reduced post-operatively in both the groups, although there was no significant difference pre-operatively and post-operatively in both the groups. Table 4 shows that 40% of sample had root dehiscence after corticotomy while 30% had root dehiscence after MOP.
Table 3.
Comparison of root length between the two groups at pre- and post-treatment.
| Time | Corticotomy (n = 10) (in mm) |
MOP (n = 10) (in mm) |
p value |
|---|---|---|---|
| Pre-treatment (T1) | 13.31 ± 1.7 | 13.48 ± 2.3 | 0.5‡ |
| Post-treatment (T2) | 13.17 ± 1.6 | 13.28 ± 1.9 | 0.9‡ |
| p value | 0.32‡ | 0.08‡ |
Non significant.
Table 4.
Distribution of dehiscence proportion wise among both the groups.
| Time | Corticotomy (n = 10)% | MOP (n = 10)% |
|---|---|---|
| >3 | >3 | |
| Pre-treatment (T1) | 1 (10%) | 2 (20%) |
| Post-treatment (T2) | 4 (40%) | 3 (30%) |
5. Discussion
The bone biologic phenomenon called coupling causes migration of teeth via orthodontic appliances, which suggests that the resorptive changes in the bone are accompanied by the formative process in healthy tissues (Proff and Romer, 2009). While the basic mechanism underlying the selective alveolar decortication was the coupling between osteoblasts and osteoclasts initiated at the same time window after the mechanical injury, wherein it bypasses the lag phase and initiates the tooth movement earlier in comparison with the traditional tooth movement (Iino et al., 2007). The procedure comprises of selective alveolar decortications of bone, a form of periodontal tissue engineering that results in an increased turnover of trabecular bone along with areas of alveolar demineralization (Frost, 1989). Besides, MOP intensifies the naturally coupled bone remodeling pathways that are activated by orthodontic forces (Alikhani et al., 2015).
With the slight differences in the underlying mechanisms of conventional orthodontic treatment and those facilitated by PAOO (Corticotomy and MOP’s), there are evidences supporting the acceleration of tooth movement by using corticotomy facilitated osteogenic orthodontics as compared to conventional orthodontics (Fischer, 2007, Aboul-Ela et al., 2011, Al-Naoum et al., 2014). However, this is the first study comparing the corticotomy facilitated osteogenic orthodontics with the minimally invasive MOP’s technique on the contralateral side.
Conventional technique results in canine retraction rate of 0.5–1 mm per month, so it can be estimated that tooth movement achieved in 2 months should be in the range of 1.5–2 mm (Abbas et al., 2016). In the present study, at the corticotomy site, the mean difference in the canine-premolar distance pre- and post-surgery was 2.76 ± 0.2 mm while at the MOP site it was 2.37 ± 0.1 mm which is suggestive of accelerated canine distalization in a short period of time at both the sites as compared to conventional orthodontics, with more distance being covered by canine at the corticotomy site as compared to the MOP site. The increase in canine distalization in short period by using MOP’s is similar to that reported by Alikhani et al., 2015. The significant increase in tooth movement at the corticotomy site could be due to the vertical cuts given on the cortical bone unlike mere small perforations at the MOP’s site. Since these vertical cuts pierced through the cortical bone, less amount of resistance was offered during application of orthodontic forces, which was not the case with MOP site. Though MOP’s also exhibited higher rate of tooth movement as compared to conventional orthodontic treatment, (Alikhani et al., 2015, Escobar and Samper, 2017), it was lesser but not significantly different as compared to that at corticotomy sites in this study.
With respect to the treatment time, the canine retraction is the most time consuming phase thus increasing the total orthodontic treatment time (Alikhani et al., 2015). There are some case reports that claim comprehensive orthodontic treatment can be completed in 4–9 months by application of a single stage corticotomy, whereas conventional orthodontics takes 1.5–2.5 years. (Suya, 1991, Wilcko et al., 2001). However in our study, by using PAOO techniques (Corticotomy and MOP’s) total completion of orthodontic treatment time was reduced to an average of 6–8 months suggestive of almost 50% reduction in treatment time. The possible reason for this could be the transient demineralization-remineralization phenomenon in the bony alveolar housing initiated on giving corticotomy cuts along with the heavy orthodontic forces consistent with that of the RAP.
The protracted treatment time not only refrains the patient from conventional orthodontic treatment, but is also associated with the damage to the periodontium (Fuhrmann, 1996, Slutzkey and Levin, 2008). Several reports (Hassan et al., 2010, Spena et al., 2007, Wilcko et al., 2009) mentioned the effects of corticotomy on periodontium which were ranging from no problems to slight interdental bone loss, loss of attached gingiva, but no such changes were observed in the present study other than the little difference in the pocket depth and gingival recession. These findings are in accordance with the results of the study conducted by Wilcko et al. (2008). The reason for no significant changes in the periodontal parameters post-operatively in the present study could be because the corticotomy cuts were given 2 mm away from the alveolar crest and only the patients with good oral hygiene and compliance were selected. However, Bell and Levy, 1972 reported a damaging effect to the periodontium around the incisors after corticotomy cuts at the premolar and incisor regions in four rhesus monkeys. According to those authors, alteration of the circulation could reduce the viability of the bone and teeth, affect the healing capacity of the mobilized bone, and have a destructive effect on the periodontium.
External root resorption is a known phenomenon associated with orthodontic treatment (Jiang et al., 2017, Segal et al., 2004). Significant root resorption and post operative discomfort was not observed in the present study on either side. This goes in accordance with the findings of Alikhani et al., 2015 who reported no post operative pain and external root resorption after MOP’s. Forty percent corticotomy sites while thirty percent MOP’s sites showed dehiscence in the present study which might be due to thin buccal bone and thus is an anatomical consideration.
In addition to the reduced patient discomfort and periodontal concerns, the PAOO provides an additional benefit of increased buccal bone thickness. In one of the previous studies, the authors concluded that a combination of decortications and buccal augmentation with orthodontic movements enables extensive tooth movement at an accelerated rate with minimal clinical periodontal damage (Bhattacharya et al., 2014, Chackartchi et al., 2017, Wilcko et al., 2001). Chackartchi et al., 2017, Yodthong et al., 2013 demonstrated a significant increase in the labial bone thickness at the crestal level during maxillary incisor retraction. The findings of their studies are similar to the findings of the present study wherein there is in an increase in buccal bone thickness at the corticotomy site. This is one of the first studies evaluating the changes in buccal bone thickness after MOP’s and also comparing it with the contralateral corticotomy site. Significant increase in buccal bone thickness was found at two levels (coronal, mid-root) at the MOP site. Moreover, when comparing the same with that on the contralateral site, the thickness of buccal bone was significantly more at the coronal level of the corticotomy site as compared to that at the MOPs site. This increase in buccal bone thickness on the corticotomy site could be attributed to the augmentation achieved through bone graft and the RAP which is seen in such type of induced injuries. The present study supports the findings of Bhattacharya et al., 2014 who concluded that orthodontic therapy facilitated with corticotomy surgery and grafting improved alveolar bony support and resulted in a permanent increase in alveolar process width. In the present study, only buccal corticotomies were performed to minimize the invasiveness as no significant difference was observed in retraction time, as reported in some of the recent studies (Addanki et al., 2017, Jahanbakhshi et al., 2016).
However, there are a few limitations to the present study including a small sample size and a short evaluation period. The results may differ with a larger sample size and the type of malocclusion being treated. So, further investigations are necessary to confirm the findings of our study. The effect of both the procedures on tooth vitality, root resorption, treatment stability and retention could not be studied as it requires long-term evaluation. Future investigations are desired in this direction.
6. Conclusion
The realms of interdisciplinary alliance in the dental profession has changed traditional orthodontic tooth movement conventions and synthesized periodontal tissue engineering and regenerative surgery, not only as a method of rapid orthodontic tooth movement but has also contributed in evolving refined protocols that reduce side effects like gingival recession, root resorption, dehiscence and relapse. PAOO is a creditable approach as compared to conventional orthodontic treatment with respect to accelerated tooth movement. Both the techniques cause increase in canine retraction in a short period of time with almost no harm to periodontal structures. The corticotomy procedure provides an added advantage of gaining increased buccal bone thickness, while MOP’s being a flapless procedure allow clinicians to deliver an efficient orthodontic care. However, longitudinal studies with larger sample size are desirable to further substantiate these observations.
Conflict of interest
The authors declared that there is no conflict of interest.
Ethical statement
The work has been approved by the appropriate ethical committees of VSPM Dental College and Research Centre, Nagpur.
Informed consent
All the subjects participating in the clinical trial were informed about the procedure and materials to be used and a written informed consent was obtained.
Footnotes
TATA Memorial Cancer Research Hospital, Mumbai.
References
- Abbas N.H., Sabet N.E., Hassan I.T. Evaluation of corticotomy-facilitated orthodontics and piezocision in rapid canine retraction. Am. J. Orthod. Dentofacial Orthop. 2016;149:473–480. doi: 10.1016/j.ajodo.2015.09.029. [DOI] [PubMed] [Google Scholar]
- Aboul-Ela S.M., El-Beialy A.R., El-Sayed K.M., Selim E.M., El-Mangoury N.H., Mostafa Y.A. Miniscrew implant-supported maxillary canine retraction with and without corticotomy-facilitated orthodontics. Am. J. Orthod. Dentofacial Orthop. 2011;139:252–259. doi: 10.1016/j.ajodo.2009.04.028. [DOI] [PubMed] [Google Scholar]
- Addanki P., Gooty J.R., Palaparthy R. Clinical and radiographic comparative evaluation of buccal and palatal corticotomy with buccal corticotomy in periodontally accelerated osteogenic orthodontics with surgical bur. Contemp. Clin. Dent. 2017;8:321–326. doi: 10.4103/ccd.ccd_846_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Naoum F., Hajeer M.Y., Al-Jundi A. Does alveolar corticotomy accelerate orthodontic tooth movement when retracting upper canines? A split-mouth design randomized controlled trial. J. Oral Maxillofac. Surg. 2014;72:1880–1889. doi: 10.1016/j.joms.2014.05.003. [DOI] [PubMed] [Google Scholar]
- Alikhani M., Alansari S., Sangsuwon C., Alikhani M., Chou M.Y., Alyami B. Micro-osteoperforations: minimally invasive accelerated tooth movement. Semin. Orthod. 2015;21(3):162–169. [Google Scholar]
- Bell W.H., Levy B.M. Revascularization and bone healing after maxillary corticotomies. J. Oral Surg. 1972;30:640–648. [PubMed] [Google Scholar]
- Bhattacharya P., Bhattacharya H., Anjum A., Bhandari R., Agarwal D.K., Gupta A. Assessment of corticotomy facilitated tooth movement and changes in alveolar bone thickness – A CT scan study. J. Clin. Diagn. Res. 2014;8 doi: 10.7860/JCDR/2014/9448.4954. ZC26–ZC30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chackartchi T., Barkana I., Klinger A. Alveolar bone morphology following periodontally accelerated osteogenic orthodontics: a clinical and radiographic analysis. Int. J. Periodontics Restorative Dent. 2017;37:203–208. doi: 10.11607/prd.2723. [DOI] [PubMed] [Google Scholar]
- Escobar Y., Samper F. Micro-osteoperforations for accelerating tooth movement during canine distalization, split-mouth study. Case report. Revista Mexicana de Ortodoncia. 2017;5:e201–e209. [Google Scholar]
- Evans, C.H., Ildstad, S.T., 2001. Small Clinical Trials: Issues and Challenges. Washington DC, National Academy Press. Available online: books.nap.edu/catalog/10078.html. [PubMed]
- Fischer T.J. Orthodontic treatment acceleration with corticotomy-assisted exposure of palatally impacted canines: a preliminary study. Angle Orthod. 2007;77:417–420. doi: 10.2319/0003-3219(2007)077[0417:OTAWCE]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Frost H.M. The regional acceleratory phenomenon: a review. Henry Ford Hosp. Med. J. 1983;31:3–9. [PubMed] [Google Scholar]
- Frost H.M. The biology of fracture healing. An overview for clinicians. Part I. Clin. Orthop. Relat. Res. 1989;248:283–293. [PubMed] [Google Scholar]
- Fuhrmann R. Three-dimensional interpretation of periodontal lesions and remodelling during orthodontic treatment. Part III. J. Orofac. Orthop. 1996;57:224–237. doi: 10.1007/BF02190235. [DOI] [PubMed] [Google Scholar]
- Hassan A.H., Al-Fraidi A.A., Al-Saeed S.H. Corticotomy-assisted orthodontic treatment: review. Open Dent. J. 2010;4:159–164. doi: 10.2174/1874210601004010159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iino S., Sakoda S., Ito G., Nishimori T., Ikeda T., Miyawaki S. Acceleration of orthodontic tooth movement by alveolar corticotomy in the dog. Am. J. Orthod. Dentofacial. Orthop. 2007;131 doi: 10.1016/j.ajodo.2006.08.014. 448.e1 8. [DOI] [PubMed] [Google Scholar]
- Jahanbakhshi M.R., Motamedi A.M., Feizbakhsh M., Mogharehabed A. The effect of buccal corticotomy on accelerating orthodontic tooth movement of maxillary canine. Dent. Res. J. (Isfahan) 2016;13:303–308. doi: 10.4103/1735-3327.187875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang F., Chen J., Kula K., Gu H., Du Y., Eckert G. Root resorptions associated with canine retraction treatment. Am. J. Orthod. Dentofacial Orthop. 2017;152:348–354. doi: 10.1016/j.ajodo.2017.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kole H. Surgical operations on the alveolar ridge to correct occlusal abnormalities. Oral Surg. Oral Med. Oral Pathol. 1959;12:515–529. doi: 10.1016/0030-4220(59)90153-7. [DOI] [PubMed] [Google Scholar]
- Proff P., Romer P. The molecular mechanism behind bone remodelling: a review. Clin. Oral Investig. 2009;13:355–362. doi: 10.1007/s00784-009-0268-2. [DOI] [PubMed] [Google Scholar]
- Segal G.R., Schiffman P.H., Tuncay O.C. Meta analysis of the treatment-related factors of external apical root resorption. Orthod. Craniofac. Res. 2004;7:71–78. doi: 10.1111/j.1601-6343.2004.00286.x. [DOI] [PubMed] [Google Scholar]
- Slutzkey S., Levin L. Gingival recession in young adults: occurrence, severity, and relationship to past orthodontic treatment and oral piercing. Am. J. Orthod. Dentofacial Orthop. 2008;134:652–656. doi: 10.1016/j.ajodo.2007.02.054. [DOI] [PubMed] [Google Scholar]
- Spena R., Caiazzo A., Gracco A., Siciliani G. The use of segmental corticotomy to enhance molar distalization. J. Clin. Orthod. 2007;41:693–699. [PubMed] [Google Scholar]
- Suya H. Corticotomy in orthodontics. In: Hosl E., Baldauf A., editors. Mechanical and Biologic Basis in Orthodontic Therapy. Verlagsgruppe Hüthig Jehle Rehm GmbH; Heidelberg, Germany: 1991. pp. 207–226. [Google Scholar]
- Wilcko M.T., Wilcko W.M., Pulver J.J., Bissada N.F. An evidence-based analysis of periodontally accelerated orthodontic and osteogenic techniques: a synthesis of scientific perspectives. Semin. Orthod. 2008;14:305–316. [Google Scholar]
- Wilcko M.T., Wilcko W.M., Bissada N.F., Bouquot J.E. Accelerated osteogenic orthodontics technique: a 1-stage surgically facilitated rapid orthodontic technique with alveolar augmentation. J. Oral Maxillofac. Surg. 2009;67:2149–2159. doi: 10.1016/j.joms.2009.04.095. [DOI] [PubMed] [Google Scholar]
- Wilcko W.M., Wilcko M.T., Bouquot J.E., Ferguson D.J. Rapid orthodontics with alveolar reshaping: two case reports of decrowding. Int. J. Periodontics Restorative Dent. 2001;21:9–19. [PubMed] [Google Scholar]
- Yaffe A., Fine N., Binderman I. Regional accelerated phenomenon in the mandible following mucoperiosteal flap surgery. J. Periodontol. 1994;65:79–83. doi: 10.1902/jop.1994.65.1.79. [DOI] [PubMed] [Google Scholar]
- Yodthong N., Charoemratrote C., Leethanakul C. Factors related to alveolar bone thickness during upper incisor retraction. Angle Orthod. 2013;83:394–401. doi: 10.2319/062912-534.1. [DOI] [PMC free article] [PubMed] [Google Scholar]