Abstract
Cartilage defects of the patella are difficult to treat due to the complex anatomy of the patellofemoral joint. First-line treatment of chondral patellar defects often results in failure independent of the surgical technique. Moreover, there is no recommendation for second-line treatment of failed patellar defect treatment. Here, the case of a 48-year-old active patient with complex patellofemoral problems who had undergone multiple previous surgeries, including failed microfracture of a full-thickness cartilage defect on his patella, is presented. The patient was treated with a polymer-based implant in combination with microfracture and autologous platelet-rich fibrin glue. Post-surgical follow-up after 6 months with magnetic resonance imaging revealed complete defect filling, which was confirmed by second-look arthroscopy after 9 months, showing the formation of cartilage repair tissue. This procedure seems to be a viable and safe treatment option for patients suffering from full-thickness chondral lesions on the patella that have previously failed microfracture at the same location.
Keywords: Patella, cell-free implant, polyglycolic acid–hyaluronan, microfracture, biological glue
Introduction
Treatment of patellar cartilage defects is challenging due to the complex structure of the patellofemoral joint, with high compressive and shear forces combined with possible malalignment, abnormal morphology, and potential instability of the patella.
Lower success rates are reported for patella treatment compared to other locations in the knee, for example, the femoral condyles. Moreover, in the literature failure rates in the range of 7.7% up to 28.6% are reported for cartilage defects independent of the treatment approach.1,2
Individual strategies are necessary to treat previously failed chondral patellar repairs. A possible treatment option might be the microfracture technique combined with a biocompatible resorbable polyglycolic acid–hyaluronan (PGA–hyaluronan) scaffold that retains mesenchymal stem and progenitor cells released by microfracturing of the subchondral bone inside the cartilage defect. Thus, the scaffold provides a three-dimensional environment for cell adhesion and matrix development to support repair tissue formation while simultaneously protecting the exposed subchondral bone.3
Case report
Anamnesis
An active 48-year-old male patient with a body mass index of 21 presented with anterior knee pain. The patient suffered from Charcot Marie Tooth Type 1b and bilateral hip dysplasia, which had been treated with multiple surgeries. On first presentation, the patient was found to have patellar dysplasia and patella alta, but with normal patellar tracking, and there was a full-thickness chondral defect on the lateral facet of the patella. In addition, there was also an old complete tear of the anterior cruciate ligament (ACL), and the patient was complaining of intermittent instability.
The patient underwent an ACL reconstruction combined with a tibial tuberosity advancement osteotomy, to correct the patella alta. The chondral defect on the lateral facet of the patella was found to measure approximately 2 cm × 1 cm. The edges of this defect were stabilized by arthroscopic radiofrequency chondroplasty and the base was treated with microfracture.
The patient underwent slow and cautious rehabilitation, remaining non-weight-bearing for the first 6-week period followed by a gradual return to full-weight-bearing as comfort allowed, but avoiding any heavy patellofemoral loading until 6 months post-operatively.
The patient then reported that the knee felt stable and initially there was reduced anterior knee pain. However, over the course of the following 3–4 years, the patient once more began to complain of increasing anterior knee pain again, particularly with any activity that involved patellofemoral loading. A magnetic resonance imaging (MRI) scan at 4 years post-microfracture showed poor filling of the patellar lesion with minimal fibrocartilage (Figure 1(a)).
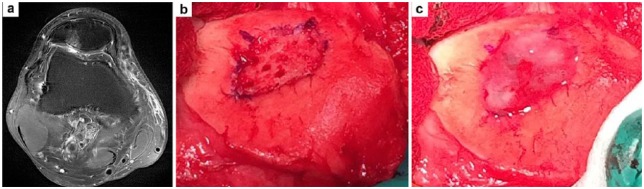
Figure 1.
Pre-operative MRI and surgical technique: (a) axial MRI at 4 years post-microfracture, showing poor filling of the patellar defect with minimal fibrocartilage, (b) chondral defect on lateral facet of patella with base microfractured and (c) polyglycolic acid scaffold fitted into the defect, fixed with two bioresorbable pins and covered with autologous platelet-rich fibrin glue.
Surgery
After a detailed discussion of the various potential options, the patient consented to further surgery. The knee was opened with a mini-medial parapatellar arthrotomy and the patella was everted. The base of the chondral defect on the lateral facet of the patella was curetted down to the subchondral bone plate and microfracture was performed according to the protocol of Steadman et al.4 A resorbable PGA–hyaluronan-based implant (chondrotissue®—BioTissue AG, Zurich, Switzerland) was cut to size, placed into the defect, and fixed in place with two bioabsorbable ActivaNail™ pins (Bioretec Ltd, Tampere, Finland) (Figure 1(b)). The implant was seen to immediately soak up the blood from the microfracture. Furthermore, platelet-rich autologous fibrin glue (Vivostat PRF®—Vivostat A/S, Alleroed, Denmark) was prepared from 120 mL of the patient’s blood used to cover the implant as additional sealing (Figure 1(c)).
Rehabilitation
Post-operatively, the patient was initially kept non-weight-bearing with his knee in a hinged brace locked in full extension for the first 2-week period followed by commencement of regular unloaded range of motion exercises. Weight-bearing was commenced at 6 weeks post-operatively, followed by a gradual return to light cardio fitness exercises, but excluding any heavy patellofemoral loading, such as squats, lunges, the leg press or loaded leg extensions.
Follow-up
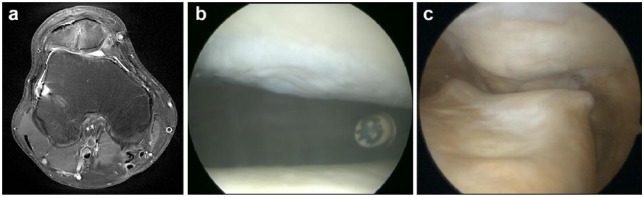
The treatment proceeded without any intra- or post-operative complications such as inflammatory reaction, swelling, infection, arthrofibrosis, or undue pain. To evaluate the cartilage repair, MRI was performed on a 3T scanner 6 months post-operatively. The MRI (Figure 2(a)) demonstrated good formation of new tissue on the lateral facet of the patella, with evidence of the biodegradable pins having partially dissolved and with what appeared to be growth of new articular cartilage. By this stage, the patient had reported a significant decrease in his anterior knee pain but he was complaining of a clunking sensation anteriorly with knee flexion. Second-look arthroscopy (Figure 2(b) and (c) performed 9 months after the patellar chondrotissue implantation, revealed the formation of new cartilage repair tissue filling the whole defect, which was stable and which exhibited normal cartilage-like texture on probing. Some scarring of the anterolateral aspect of the lining of the joint was indentified, and this required just a minor debridement. Six weeks after the second-look arthroscopy, the patient reported a reduction of the previous catching sensations that had been present beforehand and an overall significant improvement in his anterior knee symptoms that had been present prior to the PGA–hyaluronan scaffold implantation procedure. The patient reported satisfaction, with improved function and a return to regular non-impact exercise.
Figure 2.
MRI and second-look arthroscopy post-surgery: (a) MRI scan (axial view) 6 months post-op, showing the formation of a new layer of cartilage repair tissue in the defect on the lateral facet of the patella. (b, c) Intra-operative arthroscopic views of the new cartilage repair tissue on the lateral facet of the patella: (b) view looking up from the anterolateral portal and (c) view looking down from a superolateral portal.
Discussion
This case report shows for the first time the feasible and safe application of a resorbable PGA–hyaluronan implant together with a platelet-rich fibrin in combination with microfracture in a patient with several underlying diseases and a previous failed microfracture of a full-thickness chondral patellar defect.
Failure of chondral patellar defect treatment has been reported in 7.7% up to 28.6% of patients.1,2,5–7 There is no general recommendation for a second-line treatment, due to individual underlying diseases and previous treatment failure of the patients. Nevertheless, the most common approach reported for second-line treatment is total knee arthroplasty (TKA).2,6 A regenerative approach is favorable to preserve the joint and maintain the TKA as final option in case of progressive cartilage degeneration over time.
In the case of osteochondral allograft transplantation (OAT) as first- or second-line treatment, an osteochondral defect is created, although only a local cartilage defect is present.2 Defect filling with either autologous chondrocyte implantation (ACI) or matrix-assisted ACI (M-ACI) are two-step procedures that require biopsy harvest in a first surgery and implantation of the cells in a second surgery,1,5,6,7 which often lacks patient compliance.
In the presented case, no implant-related adverse events or complications were observed. The patient reported improvement in symptoms and complete defect filling was confirmed by MRI and second-look arthroscopy, which revealed formation of new cartilage repair tissue in the defect as early as 6 months post-surgery. In previous reports, the successful use of PGA-hyaluronan-based implants in combination with microfracture for cartilage defects of the patella was reported.8 None of these cases involved previous failed microfracture or a long history of cartilage defect treatment.
Conclusion
Microfracture in combination with a cell-free PGA-hyaluronan implant covered with a platelet-rich fibrin sealant is a feasible and safe second-line treatment option for chondral patellofemoral defects with an excellent clinical short-term outcome (Table 1). The case suggests that previous failed microfracture is not necessarily a contraindication for matrix-assisted microfracture treatment.
Table 1.
Literature review of failure rates in chondral patellar defect treatment.
| Reference | Treatment | Previous surgery (%) | Failure rate (%) |
|---|---|---|---|
| Kon et al.6 | M-ACI | 53.1 | 12.5 |
| Gracitelli et al.2 | OAT | 92.9 | 28.6 |
| Gomoll et al.7 | ACI | – | 8 |
| Vanlauwe et al.5 | ACI | 84.2 | 13.1 |
| Pascual-Garrido et al.1 | ACI | – | 7.7 |
ACI: autologous chondrocyte implantation; M-ACI: matrix-assisted autologous chondrocyte implantation; OAT: osteochondral allograft transplantation.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Publication funding was provided by BioTissue SA.
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
References
- 1. Pascual-Garrido C, Slabaugh MA, L’Heureux DR, et al. Recommendations and treatment outcomes for patellofemoral articular cartilage defects with autologous chondrocyte implantation: prospective evaluation at average 4-year follow-up. Am J Sports Med 2009; 37(Suppl. 1): 33S–41S. [DOI] [PubMed] [Google Scholar]
- 2. Gracitelli GC, Meric G, Pulido PA, et al. Fresh osteochondral allograft transplantation for isolated patellar cartilage injury. Am J Sports Med 2015; 43(4): 879–884. [DOI] [PubMed] [Google Scholar]
- 3. Freymann U, Petersen W, Kaps C. Cartilage regeneration revisited: entering of new one-step procedures for chondral cartilage repair. OA Orthop 2013; 1(1): 6. [Google Scholar]
- 4. Steadman JR, Rodkey WG, Briggs KK, et al. The microfracture technic in the management of complete cartilage defects in the knee joint. Orthopade 1999; 28(1): 26–32. [DOI] [PubMed] [Google Scholar]
- 5. Vanlauwe JJ, Claes T, Van Assche D, et al. Characterized chondrocyte implantation in the patellofemoral joint: an up to 4-year follow-up of a prospective cohort of 38 patients. Am J Sports Med 2012; 40(8): 1799–1807. [DOI] [PubMed] [Google Scholar]
- 6. Kon E, Filardo G, Gobbi A, et al. Long-term results after hyaluronan-based MACT for the treatment of cartilage lesions of the patellofemoral joint. Am J Sports Med 2016; 44(3): 602–608. [DOI] [PubMed] [Google Scholar]
- 7. Gomoll AH, Gillogly SD, Cole BJ, et al. Autologous chondrocyte implantation in the patella: a multicenter experience. Am J Sports Med 2014; 42(5): 1074–1081. [DOI] [PubMed] [Google Scholar]
- 8. Becher C, Ettinger M, Ezechieli M, et al. Repair of retropatellar cartilage defects in the knee with microfracture and a cell-free polymer-based implant. Arch Orthop Trauma Surg 2015; 135(7): 1003–1010. [DOI] [PubMed] [Google Scholar]