Abstract
Background
Preoperative planning of total knee arthroplasty is usually performed using knee-centred computed tomography (CT) data sets. The disadvantage of these data sets is having no account of the biomechanical axis of the lower extremity, known as Mikulicz line. It aligns the femoral head to the middle of the talocrural joint. For optimal prosthesis arrangement, the knee CT data set must therefore be brought in congruency with this line of loading to achieve the best results and eliminate rotational malalignments.
This study aims to establish a relation between the knee-centred clinical coordinate system (CCS) and a biomechanical coordinate system (BCS) based on the Mikulicz line.
Methods
CT data sets of 45 lower extremities were evaluated. Using VG Studio Max, a visualisation and measurement software program; each CT data set was aligned according to the CCS and BCS. After superimposing both the aligned data sets, the deviations of both coordinate systems in all three planes were measured with the centre of the knee defined as the origin.
Results
For the coronal plane, the CCS was demonstrated to be 2.54° in adduction compared to the BCS [standard deviation (SD) = 1.8°]. In sagittal view, the CCS was demonstrated to be 0.3° retroversed (SD = 3.27°). Finally, the deviation in the axial plane showed an outward rotation of 3.39° (SD = 1.99°). The alignment as well as the measurements demonstrated high intraobserver and interobserver reproducibility.
Conclusion
Both coordinate systems can be established in knee-centred CT data sets in a reproducible manner. Clearly, the CCS differs significantly from the BCS describing the biomechanical axis, but mathematical-based adaptations and corrections can be performed.
The translational potential of this article
The findings of this study allow a mathematical conversion of a knee CT to the biomechanical axis of the leg.
Keywords: Alignment, Computed tomography, Coordinate system, Mikulicz line, Total knee arthroplasty
Introduction
Despite the steadily growing numbers of primary and secondary total knee arthroplasties (TKAs) [1], the optimal approach for preoperational planning is still debatable. In the present literature, it is stated that two of 10 patients who underwent TKA are unsatisfied with the outcome [2], [3], [4], [5]. To address this issue, various patient-specific factors are investigated, including the gender [6], [7], reasonable expectations [4], mental health of the patient [8], [9] as well as the influence of age [10] and socioeconomic status [11], [12]. Apart from these considerations, certain procedure-specific factors apparently significantly influence the outcome. Next to the implant design [13] or preoperational knee extension deformities [14], the postoperative alignment of the prosthesis [15], [16], [17] is proven to be of utmost importance. Lotke and Ecker [15] were one of the first to describe a significant correlation between a well-positioned prosthesis and a good clinical outcome. Jeffery et al [16] went one step further in the definition of “well-positioned” and stated that to prevent loosening of the prosthesis, it should be aligned to the biomechanical axis of the leg in the coronal plane. This biomechanical axis, called the Mikulicz line, combines originally the vertex of the femoral head to the midpoint of the talocrural joint and was first defined by Mikulicz [16], [18]. Today, the middle of the femoral head is widely used as the proximal orientation point.
In implant planning till date, numerous studies have recommended seeking a neutral alignment of ± 3° varus/valgus to the mechanical axis of the limb in the coronal plane [16], [19], [20]. In the sagittal plane, a mechanically neutral orientation is likewise stated, although less investigated [21]. To complete the alignment, a slight external rotation between 2° and 5° is advised [21], [22]. Even if this targeted alignment and the needed accuracy are known, preoperative imaging for the planning of TKA is not yet standardised. In general, anteroposterior radiographs of the knee joint are used for the planning procedure. Unfortunately, this method appears to be highly affected by the patients' leg rotation [23] and varus/valgus status [24]. Newly derived three-dimensional imaging techniques in combination with computed tomography (CT) imaging software are capable of producing more accurate and reproducible results by identifying and marking anatomical landmarks [25], [26]. These techniques can improve the alignment of the CT data set. Unfortunately, owing to economical as well as radiation reasons, the CT data set is usually limited to the knee joint itself and excludes the proximal femur as well as the upper ankle joint, which are required to identify the Mikulicz line.
Owing to the importance of proper alignment of the prosthesis during the operational process, a preoperative planning of the prosthesis alignment today is necessary and mandatory in clinical routine. Since the use of patient-specific instruments is rising in first world countries, preoperative knee joint CTs are more commonly performed and can be used for the process of preoperational planning. Therefore, we aim to evaluate the orientation of a knee joint–centred CT data set in a clinical coordinate system (CCS) versus a biomechanical coordinate system (BCS) which represents the biomechanical axis. This way the CCS could easily be converted to an alignment, representing the optimal arrangement according to the Mikulicz line.
To analyse the two defined coordinate systems and to describe the correlation to each other, we postulate the following hypotheses:
-
(1)
The CCS differs in its orientation in space from the BCS.
-
(2)
There is a reproducible relation between the two systems such that a mathematical conversion into each other is achievable.
Materials and methods
This study adhered to the principles of the Declaration of Helsinki.
All CT data sets were derived from corpses assigned to medical research and education and were selected from the data bank of the Institute of Anatomy, University of Basel, Switzerland.
All of them were acquired using a Siemens SOMATOM 16 (Siemens, Erlangen, Germany) CT scanner using a steady protocol (130 kV, 240 mAs, slice collimation 1.5 mm, supine position and right lower limb only).
The alignment of the CT data sets as well as all measurements were carried out using the visualisation and measurement software VGStudio Max 2.2 (Volume Graphics GmbH, Heidelberg, Germany). The accuracy and precision of this program were demonstrated in the work of Nowakowski et al [26].
As a first step, the CT data sets for this study were selected by prealigning them using a “simple registration” function of the program following the proposal of MacWilliams et al [27]. In the coronal view, the posterior condylar line was arranged horizontally. The distal-anterior femoral cortex was allocated vertically in the sagittal view, and as a result, the articular joint space projected itself horizontally in the coronal view. After these alignment procedures, the anatomical axes of the femur and tibia were marked, and the resulting angle in between was measured in the coronal and sagittal planes to determine the flexion/extension angle as well as varus/valgus angle of the lower extremity.
By visual examination and analysis of the measured angles, the following exclusion criteria were defined: knee or hip prosthesis, clinically relevant genu varum and valgum and major degenerative pathologies of the musculoskeletal system, including major degenerative changes to the articular surfaces and flexion of the leg >15°. The remaining 45 specimens were included in the study (25 ♀, mean age: 84.0; 20 ♂, mean age: 84.5).
As a second step, the predefined coordinate systems were implemented into the CT data sets.
For the alignment in accordance to the CCS, a protocol in accordance to Nowakowski et al [28] based on the studies of McPherson et al [29] and Grood and Suntay [30], which defines the following axis, was used:
-
•
X-axis: Cylindrical axis of the femur.
-
•
Y-axis: Flexion facet of the medial tibial plateau.
-
•
Z-axis: Perpendicular to X- and Y-axes (Figure 1A).
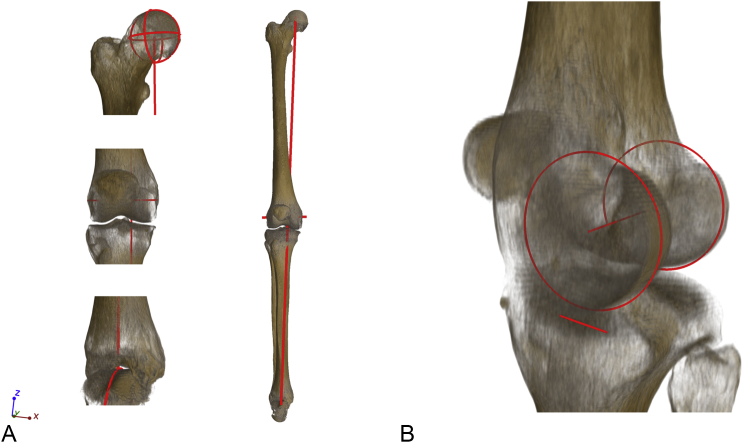
Figure 1.
Three-dimensional reconstruction of the lines defining the compared coordinate systems generated by using VGStudio Max. (A) Implementation of the biomechanical coordinate system by a semiautomatic combination of the middle of the femoral head (top left) and the middle of the talocrural joint (bottom left) to define the Mikulicz line (Z-axis). The X-axis was defined by the surgical transepicondylar line (middle left); (B) Application of the knee-centred coordinate system. The line combining the two centres of the lateral and medial condylar circle described the X-axis. The Y-axis was defined by the flexion facet of the medial tibial condyle. The Z-axis was constructed to be perpendicular.
The BCS is based on the biomechanical axis defined by the Mikulicz line [18]. It combines the middle of the femoral head with the middle of the talocrural joint, and this way described the Z-axis. The surgical transepicondylar axis was used to determine the direction of the Y-axis. The X-axis was positioned perpendicular to the other two axes (Figure 1B).
Finally, both the coordinate systems were superimposed using VGStudio Max. The origin of both the systems was defined to be the intersection point of the Mikulicz line and the tibial plateau. In all planes, the absolute deviation of both systems was measured and documented. Therefore, the angles were semiautomatically determined using the BCS as an anatomical reference system and measuring the deviations of the CCS. The deviations of the CCS were defined as a positive angle value in the three different planes when it made a retroversion and adduction in an inward rotation. The angle deviation in the coronal plane was defined as Ω in the sagittal plane Ψ and in the axial plane ϒ.
To evaluate the interobserver and intraobserver variability, the measurements were carried out by multiple observers (Examiner 1: T.S.; Examiner 2: S.H.; Table 1).
Table 1.
Intraobserver and interobserver variability.
| Series of examination | Coronal plane (Ω) | p | Sagittal plane (Ψ) | p | Axial plane (ϒ) | p |
|---|---|---|---|---|---|---|
| 1a | 2.54 | 0.00 | 0.30 | 0.54 | −3.39 | 0.00 |
| 1b | 2.55 | 0.00 | 0.14 | 0.78 | −3.22 | 0.00 |
| 2 | 2.55 | 0.00 | 0.37 | 0.46 | −3.08 | 0.00 |
Absolute values in °; Significance level p.
1a) Examiner 1, first analysis; 1b) Examiner 1, second analysis.
2) Examiner 2.
The statistical analysis was performed using Stata 14.2 (StataCorp, USA) [31]. For each set of measurements, the mean and reference standard deviation (SD) with the corresponding confidence intervals were calculated for each plane. To evaluate the first null hypothesis, one sample t test was conducted. To assess the possible correlation between age, varus/valgus axes and flexion/extension of the specimen with the results, a Pearson correlation was carried out as well as a t test to evaluate the influence of sex.
Results
All 45 specimens could be analysed with the application of these defined coordinate systems. The absolute as well as derived results are as follows:
Coronal plane
Positive angle values represent adduction, and negative values, abduction.
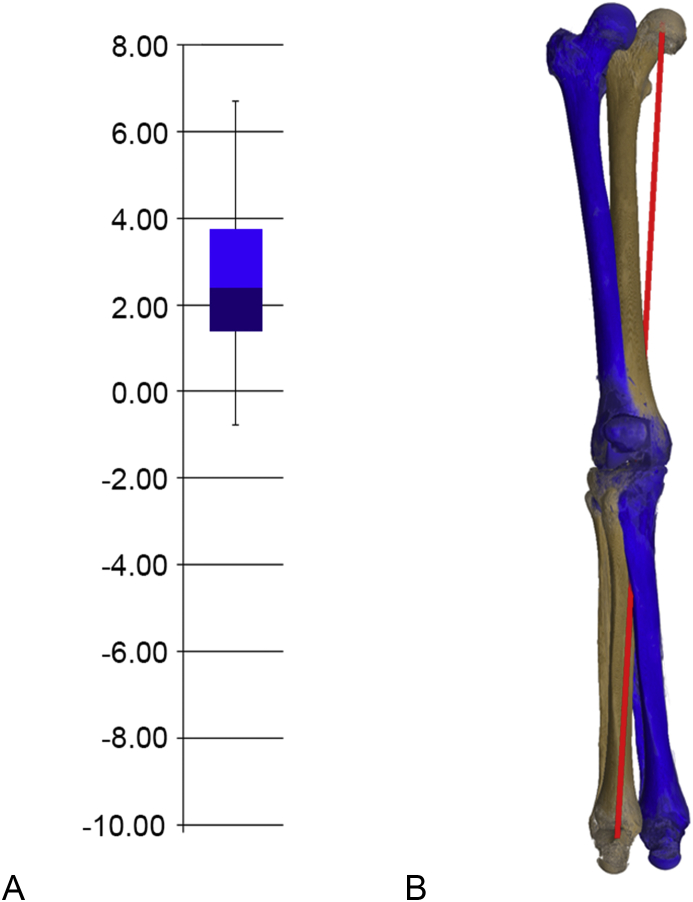
Overall, we found a mean Ω of 2.54° (SD = 1.80°), accounting for an adduction of the CCS in comparison to the BCS (Figure 2). The deviation of the two systems was shown to be highly significant (p < 0.001).
Figure 2.
Deviation in the coronal plane between the CCS and BCS. (A) Absolute values of adduction. (B) Visualisation of adduction of CCS (blue) in comparison to BCS (bone colour). BCS = biomechanical coordinate system; CCS = clinical coordinate system.
Sagittal plane
Positive angle values represent retroversion, and negative values, anteversion.
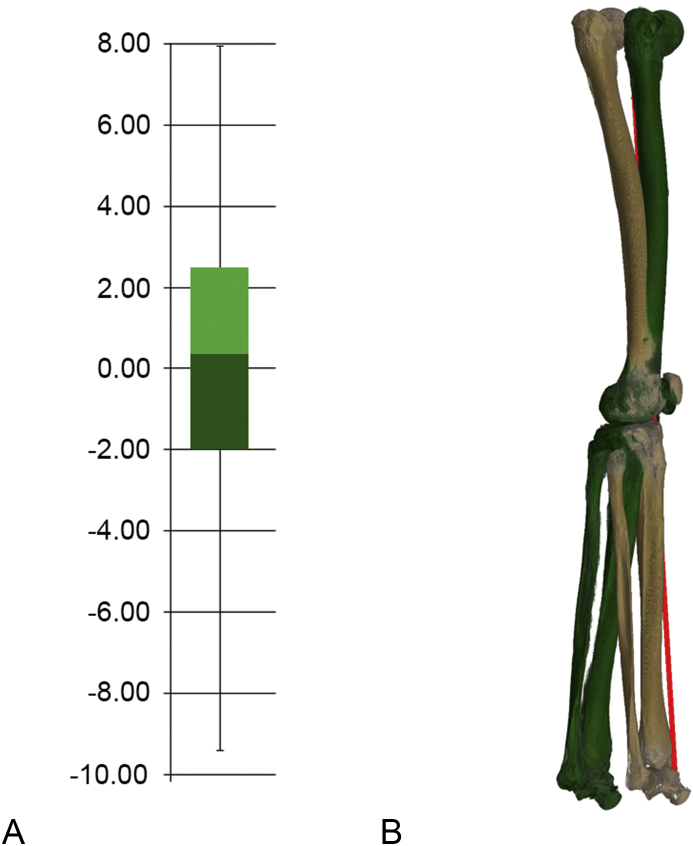
A mean Ψ of 0.30° (SD = 3.27°) was derived. Compared to the BCS, the CCS showed a slight retroversion (Figure 3). The deviation of the two systems was not significant (p = 0.54).
Figure 3.
Deviation in the sagittal plane between the CCS and BCS. (A) Absolute values of retroversion. (B) Visualisation of the retroversion of CCS (green) in comparison to BCS (bone colour). BCS = biomechanical coordinate system; CCS = clinical coordinate system.
Axial plane
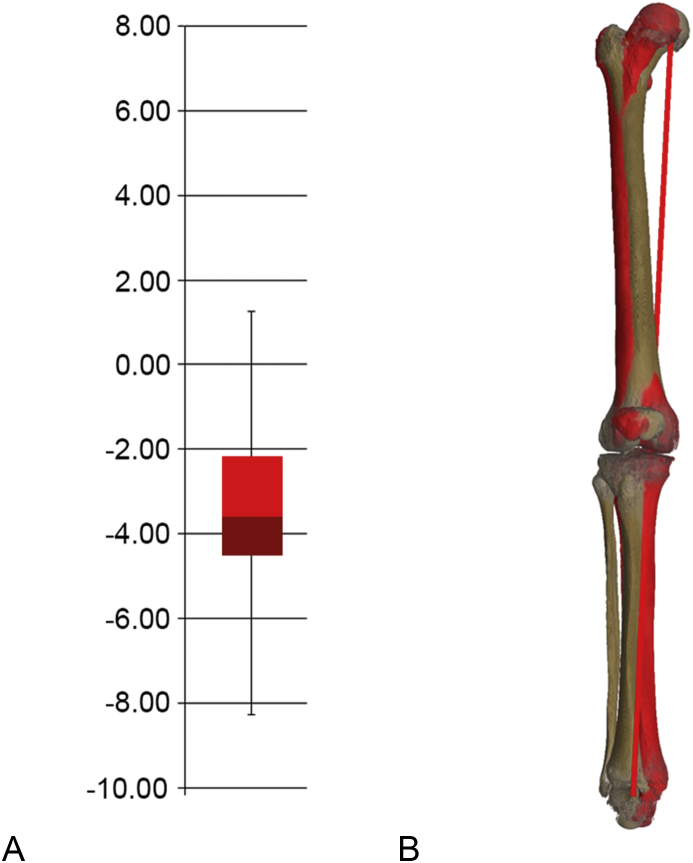
Positive angle values represent inward rotation, and negative values, outward rotation.
The study population showed a mean ϒ of −3.39° (SD = 1.99°). This highly significant (p < 0.001) deviation between the two systems presented an outward rotation of the CCS in comparison to the BCS (Figure 4).
Figure 4.
Deviation in the axial plane between the CCS and BCS. (A) Absolute values of outward rotation. (B) Visualisation of the outward rotation of CCS (red) in comparison to BCS (bone color). BCS = biomechanical coordinate system; CCS = clinical coordinate system.
Mathematical-based adaptation formulas
Coronal plane: CCS + 2.54° abduction = BCS.
Sagittal plane: CCS + 0.30° anteversion = BCS.
Axial plane: CCS + 3.39° inward rotation = BCS.
Statistics
The absolute results as well as the intraobserver and interobserver variability are presented in Table 1.
We found highly significant results in the coronal and axial planes, whereas the sagittal plane showed no significant results.
By dividing the results into groups of male and female, we found Ω to be slightly higher in males, Ψ slightly higher in females and ϒ 1° higher in males. The differences nevertheless showed no significant correlation as established using the t test and were within the range of SD (Table 2).
Table 2.
Results of all measurements in (°) divided into gender groups.
| Group | Coronal plane (Ω) | 95% Confidence interval | Sagittal plane (Ψ) | 95% Confidence interval | Axial plane (ϒ) | 95% Confidence interval |
|---|---|---|---|---|---|---|
| Female | 2.03 | 1.26 to 2.79 | 0.48 | −0.99 to 1.95 | −2.77 | −3.39 to −2.15 |
| Male | 3.20 | 2.44 to 3.94 | 0.01 | −1.39 to 1.41 | −3.81 | −4.86 to −2.75 |
| Combined | 2.55 | 2.00 to 3.09 | 0.27 | −0.72 to 1.26 | −3.23 | −3.81 to −2.65 |
| t | −2.23 | 0.47 | 1.84 |
t = impact factor of significant differentiation.
A significant correlation of the absolute value of angle shift in the three defined planes and an initial varus/valgus angle of the lower extremity could not be established (p = −0.05 to 0.75). The same is also true for the significance of correlation of the initial flexion (p = −0.08 to 0.83) and any specific age of the analysed sample (p = −0.23 to 0.60) with regards to the angle shift of the two coordinate systems. The data in any analysis are found to be homogeneously distributed.
Discussion
The alignment of a total knee prosthesis is a well-discussed topic in the field of arthroplasty. Approximately 40 years ago, the first authors observed a significant correlation between a postoperatively well-aligned prosthesis and a good clinical outcome and recommended to place the prosthesis in 3°–7° valgus [15]. Various authors confirmed a better clinical outcome with similar alignment targets [16], [17], [21], [32]. However, recent studies began to question these goals [33], [34], [35]. Morgan et al [34] observed no statistical significance when comparing the revision rate between the three postoperative alignment groups: varus, neutral and valgus. After obtaining similar results, Parratte et al [33] proposed that alignment may not be considered as a dichotomous variable (well aligned vs. not well aligned); however, alignment goals should rather be defined for each patient individually.
To assess these alignment goals, there are two different main approaches for defining the biomechanical axis of the lower limb during preoperational planning.
The first approach is the use of long-leg radiographs to identify and mark the Mikulicz line [16], [36], [37]. Bäthis et al [19] added optical tracking devices during the operational procedure, achieving significantly better results than obtaining by the conventional technique. The problems they faced were defined by the use of two-dimensional radiographs and the increased complexity during the operation. Next to different flexion angles and rotation changes of the leg during the X-ray examination, the operation time increased and got more complex. These fundamental challenges can only be overcome by the use of the more accurate three-dimensional imaging methods such as CT [23].
The second approach is using three-dimensional data sets of the entire leg to identify the femoral head and the talocrural joint and construct the Mikulicz line [38]. Although the use of newer three-dimensional imaging techniques was found to be accurate [25], [26], those large data sets are obviously more expensive to acquire. Furthermore, if those data sets are acquired with CT, the patients will be exposed to a greater amount of ionising radiation.
To quantify the exposure of a patient to ionising radiation, the concept of effective dose is often used [39]. For calculating the effective dose, the weighted organ doses must be added up. The more sensitive the organs are to the field of radiation, the higher is the effective dose required for a specific procedure. Studies showed that for this reason, a patient undergoing a CT scan of the hip is almost 20 times more exposed to radiation as one patient who receives a CT scan of the knee [40]. Henckel et al [41] demonstrated that it is possible to reduce the effective dose of a mechanical axis–defining whole-limb CT examination to the level of a conventional anteroposterior radiograph of the leg. This is possible by scanning only the relevant fields of interest for the mechanical axis: the femoral head, knee and talocrural joint, as it was described by Bäthis et al [42]. In their study, the achieved alignment in TKA showed a significantly better restoration of the mechanical leg alignment than the use of preoperative long-leg radiographs. Nevertheless, following the as low as reasonably achievable principle, it would be preferable to just use knee CT data sets as we have done in this study. Because these data sets are often available owing to the wide distribution and application of patient-specific instruments, we inhere provide a method of CT-based preoperative planning that can be seen as further stage of the idea of Bäthis et al [42]. This way, additional examinations could be avoided which would lead to reduced cost and could prevent harm to the patient.
In our study, we could align all data sets according to the two defined coordinate systems. It was easily and rapidly implemented into all specimens using only three anatomical landmarks. The flexion surfaces of the two femoral condyles and the flexion surface of the medial tibial condyle were observed to be well identifiable throughout the population. In the coronal and axial plane, we observed distinct and significant deviations of the mean difference from 0°. More importantly, we observed SDs for deviations lower than 2° for the coronal and axial plane and above 3° for the sagittal plane.
Nearly identical mean values and SDs were observed in both repetitions of the first observer as well as for the second one, suggesting that these numbers are indeed characteristics of the two coordinate systems and not of the individual ability of the observer.
The deviation measurements showed, for both observers, no indications of a systematic difference and SD of a substantially lower magnitude, particularly for the BCS; therefore, one can conclude that the results reflect a genuine difference between the two approaches and not just the mistakes in the measurement procedure of each system.
An additional argument for a genuine difference between the systems is given by the differences of the deviation measurements within and between the observers. We observed only a slight difference in the mean deviation measurements (although significant for the difference between the first and second observer), but very moderate SDs, indicating a high reproducibility of the single-deviation measurements.
Our study proved that it is possible to reconstruct the direction of the Mikulicz line accurately in the coronal plane, suggesting that the intercondylar axis is closely related to the Mikulicz line, as those two axes were responsible for the correlation in the coronal plane. In the sagittal plane, the two coordinate systems did not overlap constantly; thus, a strong correlation between the medial flexion facet of the tibia and the Mikulicz line could not be demonstrated. Given the sagittal plane to be reconstructed and the measurements performed semiautomatically by surface definition, slight differences in the identification of anatomical landmarks by the two examiners could explain these slight distinctions. Furthermore, the high age and following the ongoing osteoarthritis make it very difficult to clearly determine the flexion facet of the medial tibial condyle. The results of the axial plane showed also a strong correlation between the two coordinate systems, which resembles the relation between the intercondylar axis and the transepicondylar axis. In the further statistical analysis, all measurements were shown to be normally distributed and not affected by interobserver and intraobserver variability.
We therefore propose to align CT data sets of the knee according to the knee-centred coordinate system to obtain a standardised approach. Simultaneously, it is easily possible to conclude the direction of the mechanical axis of the leg by using the mathematical-based adaptation formulas. This approach should be evaluated further in the preoperational planning of a total knee prosthesis. We therefore conclude to obtain the same results owing to this newly gained method with the reconstructed Mikulicz line.
Conclusions
The insertion of the CCS was shown to be highly reproducible. The orientation in the space of the data sets differed between the CCS and the BCS in the coronal and axial planes. A relation could additionally be demonstrated between the two systems, thereby allowing for a mathematical conversion.
It should be considered to align clinical CT data sets according to the CCS, which would allow conclusions to the biomechanical axis in an economical and patient-friendly manner which would establish a standardised approach.
Conflicts of interest
The authors have no conflicts of interest relevant to this article.
Acknowledgements
The authors wish to thank Werner Vach, University Hospital Basel, Switzerland, for revising our methods and statistical analysis. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jot.2018.07.005.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Kurtz S.M., Ong K.L., Lau E., Widmer M., Maravic M., Gómez-Barrena E. International survey of primary and revision total knee replacement. Int Orthop. 2011;35(12):1783–1789. doi: 10.1007/s00264-011-1235-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bourne R.B., Chesworth B.M., Davis A.M., Mahomed N.N., Charron K.D. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57–63. doi: 10.1007/s11999-009-1119-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hawker G., Wright J., Coyte P., Paul J., Dittus R., Croxford R. Health-related quality of life after knee replacement. Results of the knee replacement patient outcomes research team study. J Bone Jt Surg Am. 1998;80(2):163–173. doi: 10.2106/00004623-199802000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Noble P.C., Conditt M.A., Cook K.F., Mathis K.B. The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35–43. doi: 10.1097/01.blo.0000238825.63648.1e. [DOI] [PubMed] [Google Scholar]
- 5.Wylde V., Learmonth I., Potter A., Bettinson K., Lingard E. Patient-reported outcomes after fixed-versus mobile-bearing total knee replacement. Bone Jt J. 2008;90(9):1172–1179. doi: 10.1302/0301-620X.90B9.21031. [DOI] [PubMed] [Google Scholar]
- 6.Kamath A.F., Horneff J.G., Gaffney V., Israelite C.L., Nelson C.L. Ethnic and gender differences in the functional disparities after primary total knee arthroplasty. Clin Orthop Relat. 2010;468(12):3355–3361. doi: 10.1007/s11999-010-1461-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh J.A., Gabriel S., Lewallen D. The impact of gender, age, and preoperative pain severity on pain after TKA. Clin Orthop Relat Res. 2008;466(11):2717–2723. doi: 10.1007/s11999-008-0399-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hirschmann M.T., Testa E., Amsler F., Friederich N.F. The unhappy total knee arthroplasty (TKA) patient: higher WOMAC and lower KSS in depressed patients prior and after TKA. Knee Surg Sports Traumatol Arthrosc. 2013;21(10):2405–2411. doi: 10.1007/s00167-013-2409-z. [DOI] [PubMed] [Google Scholar]
- 9.Lingard E.A., Katz J.N., Wright E.A., Sledge C.B. Predicting the outcome of total knee arthroplasty. J Bone Jt Surg Am. 2004;86(10):2179–2186. doi: 10.2106/00004623-200410000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Meehan J.P., Danielsen B., Kim S.H., Jamali A.A., White R.H. Younger age is associated with a higher risk of early periprosthetic joint infection and aseptic mechanical failure after total knee arthroplasty. J Bone Jt Surg Am. 2014;96(7):529–535. doi: 10.2106/JBJS.M.00545. [DOI] [PubMed] [Google Scholar]
- 11.Feldman C.H., Dong Y., Katz J.N., Donnell-Fink L.A., Losina E. Association between socioeconomic status and pain, function and pain catastrophizing at presentation for total knee arthroplasty. BMC Muscoskel Disord. 2015;16(1):18. doi: 10.1186/s12891-015-0475-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis E.T., Lingard E.A., Schemitsch E.H., Waddell J.P. Effects of socioeconomic status on patients' outcome after total knee arthroplasty. Int J Qual Health Care. 2008;20(1):40–46. doi: 10.1093/intqhc/mzm059. [DOI] [PubMed] [Google Scholar]
- 13.Victor J., Ghijselings S., Tajdar F., Van Damme G., Deprez P., Arnout N. Total knee arthroplasty at 15–17 years: does implant design affect outcome? Int Orthop. 2014;38(2):235–241. doi: 10.1007/s00264-013-2231-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ritter M.A., Lutgring J.D., Davis K.E., Berend M.E., Pierson J.L., Meneghini R.M. The role of flexion contracture on outcomes in primary total knee arthroplasty. J Arthroplasty. 2007;22(8):1092–1096. doi: 10.1016/j.arth.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 15.Lotke P.A., Ecker M.L. Influence of positioning of prosthesis in total knee replacement. J Bone Jt Surg Am. 1977;59(1):77–79. [PubMed] [Google Scholar]
- 16.Jeffery R.S., Morris R.W., Denham R.A. Coronal alignment after total knee replacement. Bone Jt J. 1991;73(5):709–714. doi: 10.1302/0301-620X.73B5.1894655. [DOI] [PubMed] [Google Scholar]
- 17.Fang D.M., Ritter M.A., Davis K.E. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty. 2009;24(6):39–43. doi: 10.1016/j.arth.2009.04.034. [DOI] [PubMed] [Google Scholar]
- 18.Mikulicz J. Die seitlichen Verkrümmungen am Knie und deren Heilungsmethoden. Arch f klin Chir. 1879;23:560–630. [Google Scholar]
- 19.Bäthis H., Perlick L., Tingart M., Lüring C., Zurakowski D., Grifka J. Alignment in total knee arthroplasty. Bone Jt J. 2004;86(5):682–687. doi: 10.1302/0301-620x.86b5.14927. [DOI] [PubMed] [Google Scholar]
- 20.Werner F.W., Ayers D.C., Maletsky L.P., Rullkoetter P.J. The effect of valgus/varus malalignment on load distribution in total knee replacements. J Biomech. 2005;38(2):349–355. doi: 10.1016/j.jbiomech.2004.02.024. [DOI] [PubMed] [Google Scholar]
- 21.Kim Y.-H., Park J.-W., Kim J.-S., Park S.-D. The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop. 2014;38(2):379–385. doi: 10.1007/s00264-013-2097-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anouchi Y., Whiteside L., Kaiser A., Milliano M. The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res. 1993;(287):170–177. [PubMed] [Google Scholar]
- 23.Lonner J.H., Laird M.T., Stuchin S.A. Effect of rotation and knee flexion on radiographic alignment in total knee arthroplasties. Clin Orthop Relat Res. 1996;331:102–106. doi: 10.1097/00003086-199610000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Swanson K.E., Stocks G.W., Warren P.D., Hazel M.R., Janssen H.F. Does axial limb rotation affect the alignment measurements in deformed limbs? Clin Orthop Relat Res. 2000;371:246–252. doi: 10.1097/00003086-200002000-00029. [DOI] [PubMed] [Google Scholar]
- 25.Victor J., Van Doninck D., Labey L., Innocenti B., Parizel P., Bellemans J. How precise can bony landmarks be determined on a CT scan of the knee? Knee. 2009;16(5):358–365. doi: 10.1016/j.knee.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 26.Nowakowski A.M., Müller-Gerbl M., Valderrabano V. Assessment of knee implant alignment using coordinate measurement on three-dimensional computed tomography reconstructions. Surg Innovat. 2012;19(4):375–384. doi: 10.1177/1553350611429689. [DOI] [PubMed] [Google Scholar]
- 27.MacWilliams B., DesJardins J., Wilson D., Romero J., Chao E. A repeatable alignment method and local coordinate description for knee joint testing and kinematic measurement. J Biomech. 1998;31(10):947–950. doi: 10.1016/s0021-9290(98)00106-7. [DOI] [PubMed] [Google Scholar]
- 28.Nowakowski A.M., Kamphausen M., Pagenstert G., Valderrabano V., Müller-Gerbl M. Influence of tibial slope on extension and flexion gaps in total knee arthroplasty: increasing the tibial slope affects both gaps. Int Orthop. 2014;38(10):2071–2077. doi: 10.1007/s00264-014-2373-3. [DOI] [PubMed] [Google Scholar]
- 29.McPherson A., Kärrholm J., Pinskerova V., Sosna A., Martelli S. Imaging knee position using MRI, RSA/CT and 3D digitisation. J Biomech. 2005;38(2):263–268. doi: 10.1016/j.jbiomech.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 30.Grood E.S., Suntay W.J. A joint coordinate system for the clinical description of three-dimensional motions: application to the knee. J Biomech Eng. 1983;105(2):136–144. doi: 10.1115/1.3138397. [DOI] [PubMed] [Google Scholar]
- 31.StataCorp . vol. 14. StataCorp LP; College Station, TX: 2015. (Stata statistical software: release). [computer program] [Google Scholar]
- 32.Bargren J.H., Blaha J., Freeman M. Alignment in total knee arthroplasty: correlated biomechanical and clinical observations. Clin Orthop Relat Res. 1983;173:178–183. [PubMed] [Google Scholar]
- 33.Parratte S., Pagnano M.W., Trousdale R.T., Berry D.J. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Jt Surg. 2010;92(12):2143–2149. doi: 10.2106/JBJS.I.01398. [DOI] [PubMed] [Google Scholar]
- 34.Morgan S.S., Bonshahi A., Pradhan N., Gregory A., Gambhir A., Porter M. The influence of postoperative coronal alignment on revision surgery in total knee arthroplasty. Int Orthop. 2008;32(5):639–642. doi: 10.1007/s00264-007-0391-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bonner T., Eardley W., Patterson P., Gregg P. The effect of post-operative mechanical axis alignment on the survival of primary total knee replacements after a follow-up of 15 years. J Bone Jt Surg Br. 2011;93(9):1217–1222. doi: 10.1302/0301-620X.93B9.26573. [DOI] [PubMed] [Google Scholar]
- 36.Pfitzner T., Abdel M.P., von Roth P., Perka C., Hommel H. Small improvements in mechanical axis alignment achieved with MRI versus CT-based patient-specific instruments in TKA: a randomized clinical trial. Clin Orthop Relat Res. 2014;472(10):2913–2922. doi: 10.1007/s11999-014-3784-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kim Y.-H., Kim J.-S., Yoon S.-H. Alignment and orientation of the components in total knee replacement with and without navigation support: a prospective, randomised study. Bone Jt J. 2007;89(4):471–476. doi: 10.1302/0301-620X.89B4.18878. [DOI] [PubMed] [Google Scholar]
- 38.Ensini A., Timoncini A., Cenni F., Belvedere C., Fusai F., Leardini A. Intra-and post-operative accuracy assessments of two different patient-specific instrumentation systems for total knee replacement. Knee Surg Sports Traumatol Arthrosc. 2014;22(3):621–629. doi: 10.1007/s00167-013-2667-9. [DOI] [PubMed] [Google Scholar]
- 39.Jacobi W. The concept of the effective dose a proposal for the combination of organ doses. Radiat Environ Biophys. 1975;12(2):101–109. doi: 10.1007/BF01328971. [DOI] [PubMed] [Google Scholar]
- 40.Biswas D., Bible J.E., Bohan M., Simpson A.K., Whang P.G., Grauer J.N. Radiation exposure from musculoskeletal computerized tomographic scans. JBJS. 2009;91(8):1882–1889. doi: 10.2106/JBJS.H.01199. [DOI] [PubMed] [Google Scholar]
- 41.Henckel J., Richards R., Lozhkin K., Harris S., y Baena F.R., Barrett A. Very low-dose computed tomography for planning and outcome measurement in knee replacement. Bone Jt J. 2006;88(11):1513–1518. doi: 10.1302/0301-620X.88B11.17986. [DOI] [PubMed] [Google Scholar]
- 42.Bäthis H., Perlick L., Tingart M., Lüring C., Perlick C., Grifka J. Radiological results of image-based and non-image-based computer-assisted total knee arthroplasty. Int Orthop. 2004;28(2):87–90. doi: 10.1007/s00264-003-0533-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.