Abstract
Background
Type II superior labrum anterior and posterior (SLAP) lesions could induce chronic shoulder pain and impaired movement. Current management of Type II SLAP lesions consists of two well-established surgical procedures: arthroscopic biceps tenodesis and SLAP repair. However, which technique is preferred over the other is still a controversy.
Methods
We performed a systematic electronic database search on Cochrane Central Register of Controlled Trials, MEDLINE and Embase to identify articles equating superior labral repair with biceps tenodesis, which were reported before August 2017 which included the phrase “superior labral anterior posterior” or “SLAP.” The randomised controlled clinical trials that met our criteria were evaluated for quality of methodology. The results obtained were further analysed and correlated to present the benefits and drawbacks comparing the two SLAP repair surgical procedures.
Result
Based on our inclusion and exclusion criteria, we identified five articles (204 patients) that were included in this meta-analysis. The results indicate that prevalence of patients return to preinjury sports level and the patients satisfaction were found to be significantly better in tenodesis group than in the SLAP repair group (p < 0.05). As for the patient age, VAS score, American Shoulder and Elbow Surgeons score, University of California at Los Angeles score, postoperative stiffness and reoperation rates, no significant differences were evident among the two groups, thus supporting the results reported in the current literatures (p > 0.05).
Conclusions
Both the surgical treatments, SLAP repair and the biceps tenodesis, are efficacious in pain alleviation and recovery of shoulder function. But, compared with SLAP repair, biceps tenodesis showed higher rate of patient satisfaction and return to preinjury sports participation.
The translational potential of this article
Impart better understanding regarding discrepancies in the outcomes between biceps tenodesis and SLAP repair in treating patients with isolated Type II SLAP lesions.
Keywords: Labral repair, Superior labrum anterior and posterior, Tenodesis
Abbreviations: ASES, American Shoulder and Elbow Surgeons score; CMS, Coleman methodology score; SLAP, superior labrum anterior and posterior; UCLA, University of California at Los Angeles score; VAS, Visual Analogue Scale score; LOE, Level of evidence
Introduction
The superior labrum anterior and posterior (SLAP) lesions were primarily reported by Andrews et al [1] in 1985. Later, Snyder et al [2] classified these labral tears into four subtypes. Among the four types, Type II SLAP lesion is predominantly clinically most encountered, and it is elucidated from other types by detachment of the superior labrum and biceps anchor from the superior glenoid [3]. Type II SLAP lesion can cause chronic shoulder pain and dysfunction. Current conservative management for Type II SLAP lesion includes activity modification, non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroid injection, whereas patients with symptomatic Type II SLAP lesion in whom conservative treatment failed often undergo surgical treatment. Present surgical treatment generally consists of either arthroscopic superior labral repair or biceps tenodesis.
Several studies have reported that arthroscopic SLAP repair for Type II SLAP lesions could receive significant clinical or functional improvement. For example, Brockmeier et al [4] performed SLAP repair on Type II SLAP lesion patients with an average follow-up period of 2.7 years, and forty-one patients (87%) reported the outcome as good or excellent. Similarly, Boesmueller et al [5] found that arthroscopic SLAP repair resulted in acceptable functional outcomes, and half of the patients involved in competitive sports activity were able to return to their preinjury sports levels 6 months after surgery.
However, recently, some studies have found that SLAP repair was not as successful as originally reported and was associated with postoperative stiffness, continued pain, lower rates of return to activity and failure of the labrum to heal to the superior glenoid [6]. For example, Provencher et al [7] evaluated 179 Type II SLAP repairs and found that 66 patients (37%) met failure criteria, and 50 patients (28%) elected revision surgery. Waterman et al reported a failure in 13% (n = 31) of patients with SLAP repair, of whom six patients required revision SLAP repair and 25 patients underwent subpectoral biceps tenodesis. They demonstrated that majority of patients who underwent biceps tenodesis (76%) returned to active duty as compared with those who underwent revision SLAP repair (17%) [8].
In view of the findings in the aforementioned studies, as an alternative to SLAP repairs, biceps tenodesis has been the favoured surgical treatment for nonathletic patients. Some advantages of biceps tenodesis over SLAP repair may include less postoperative stiffness, higher rates of return to activity and better patient satisfaction. Boileau et al [9] compared the two surgical procedures and showed that 13 patients (87%) were able to recover to initial sports level participation after biceps tenodesis compared with only 20% (2 of 10) after SLAP repair (p = 0.01). Despite several reports, surgical management of Type II SLAP lesions is still disputed as there are several factors that could affect the surgical outcome, such as age, activity level, quality of the labral tissue and concomitant pathology [7], [10], [11], [12], [13]. Besides, there is no meta-analysis that compares the functional results among patients undergoing superior labral repair or biceps tenodesis of the isolated Type II SLAP lesions right now. Therefore, the scope of this meta-analysis is to determine whether there are discrepancies in the outcomes between biceps tenodesis and SLAP repair in treating patients with isolated Type II SLAP lesions.
Materials and methods
Search strategy
We carried out a meta-analysis of the literature with the search terms “superior labral anterior posterior” or “SLAP”. A complete search of the literature in the following databases was performed: MEDLINE (PubMed) (1950 to August 2017), Embase (Ovid) (1974 to August 2017) and Cochrane (1996 to August 2017). Our inclusion criteria included outcome-based studies of isolated Type II SLAP lesions which compared superior labral repair and biceps tenodesis by using clinical or functional scoring systems. Exclusion criteria included studies that involved cadaver or animal studies, biomechanical studies, literature reviews, letters to editors, expert opinion articles, case reports or technique notes which did not contain clinical outcome-based data.
Quality assessment
The Coleman methodology score (CMS) was applied to determine the quality of the involved studies. The CMS consists of 15 items in its checklist and is scaled from 0 to 100 points. A score from 85 to 100 is considered excellent, 70–84 as good, 55–69 as fair and below 55 as poor. An overall score of 100 suggests that the study avoids chance, bias and confounding variables. The quality assessment by CMS was carried out by two independent reviewers (one orthopaedic resident and one shoulder fellow). In addition, all the results were confirmed by the senior author.
Outcome measures
The identified studies were measured and analysed for the following outcomes: patient age, return to previous sport level, reoperation, patient satisfaction, University of California at Los Angeles (UCLA) score, American Shoulder and Elbow Surgeons (ASES) score, visual analogue scale (VAS) score and postoperative stiffness. Two reviewers evaluated the literature separately, and any discrepancies were reevaluated and resolved by consensus.
Statistical analysis
A formal meta-analysis was conducted only for clinical outcome data from comparative studies using Stata 12.0 (Stata Corp LP, College Station, TX, USA). Results for continuous or categorical outcomes were reported as a mean difference or an odds ratio, respectively, with 95% confidence intervals.
Results
Literature search
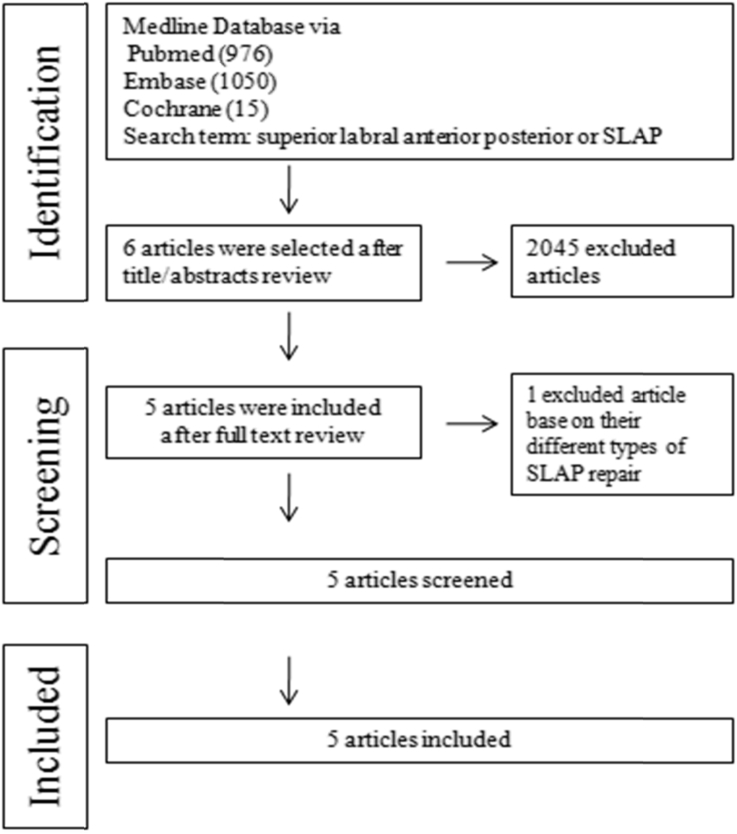
A total of 2051 studies were selected after an intensive database search on PubMed (n = 976), Embase (n = 1050) and Cochrane (n = 15). Of these 2051 articles, 2045 articles were excluded after title/abstracts review. Six articles that met our inclusion criteria were subsequently included after a full-text review. From these articles, one article was excluded as it reported different types of SLAP repair. Finally, five unique studies that met our study criteria were used for this meta-analysis (Figure 1). Three were retrospective cohort studies (LOE III), one was a case-control study and one was a double-blind, sham-controlled trial (LOE II) and reported from 2009 to 2017 (Table 1).
Figure 1.
Flow chart summarising study profile and selection procedure.
Table 1.
Characteristics of the included studies.
| Author | Study, LoE | Participants | Intervention | Follow-up time | Outcomes |
|---|---|---|---|---|---|
| Boileau P et al [9] | Cohort study, III | 25 consecutive patients operated for an isolated Type II SLAP lesion between 2000 and 2004 | 10 SLAP repair 15 tenodesis |
Minimum 2 years SLAP repair: 35 (24–69) months Tenodesis: 34 (24–68) months |
Constant score, patient satisfaction, sports level and reoperation rate |
| Denard PJ et al [26] | Retrospective cohort study, III | 37 patients surgically managed isolated Type II SLAP lesions between November 2003 and February 2009 | 22 SLAP repair 15 tenodesis |
Minimum 2 years SLAP repair: 63.2 ± 14.5 months Tenodesis group: 41.1 ± 19.8 months |
Patient satisfaction, sports level, UCLA score, ASES score, VAS score and ROM |
| Ek et al [25] | Retrospective cohort study, III | 25 patients who had undergone surgery for an isolated Type II SLAP lesion between 2008 and 2011 | 10 SLAP repair 15 tenodesis |
Minimum 24 months SLAP repair: mean 35 months (range, 25–52) Tenodesis group: mean 31 months (range, 26–43) |
Patient satisfaction, sports level, ASES score, VAS score and SSV score |
| Zhao et al [19] | Case-control study, IV | 38 patients with Type II SLAP injury were treated with SLAP repair and biceps tenodesis from March 2009 to March 2012 | 22 SLAP repair 16 tenodesis |
2 years | UCLA score and SST score |
| Schrøder et al [27] | Double-blind three-armed randomised, sham-controlled study, I | 118 patients with Type II SLAP injury were treated with SLAP repair and biceps tenodesis from January 2008 to January 2014 | 40 labral repair 39 tenodesis 39 sham surgery |
2 years | WOSI and Rowe score, OISS score, the EuroQol (EQ-5D, EQ-VAS) and patient satisfaction |
ASES = American Shoulder and Elbow Surgeons; LoE = level of evidence; SLAP = superior labrum anterior and posterior; UCLA = University of California at Los Angeles; VAS, visual analogue scale; SST score = simple shoulder test; SSV = subjective shoulder value; WOSI score = western ontario shoulder instability index; OISS score = Oxford Instability Shoulder Score; EQ-5D = EuroQol 5-Dimensional questionnaire; EQ-VAS = EuroQol-visual analogue scale.
Demographics
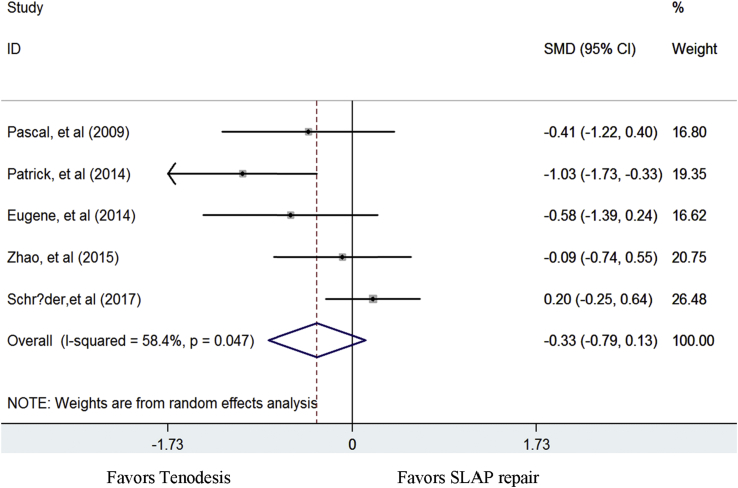
In our study, a total of 204 patients were analysed from the selected five studies, which included 104 SLAP repairs and 100 biceps tenodesis. Generally, no significant difference was observed in the baseline age of the patients between the cohorts (p = 0.157, Fig. 2).
Figure 2.
Standard differences in means for patient ages between biceps tenodesis and SLAP repair groups.
SLAP = superior labrum anterior and posterior.
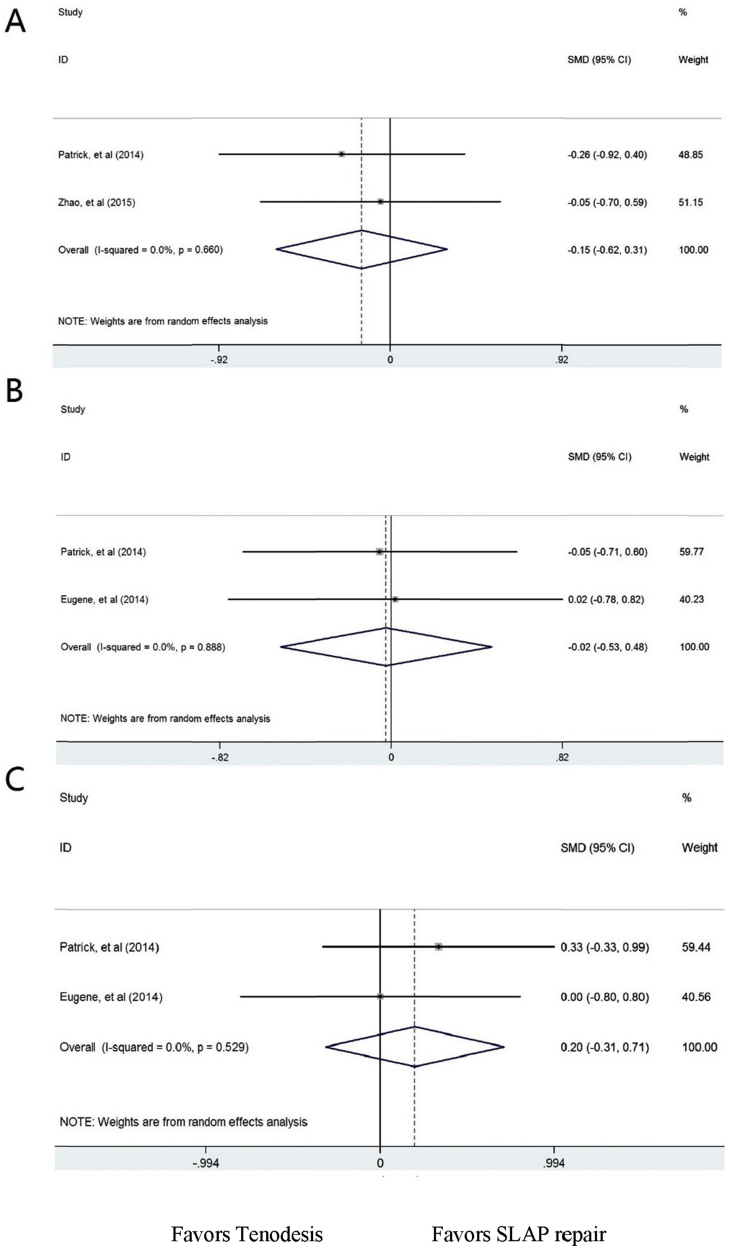
Surgical outcome score
Patients were clinically assessed both preoperatively and postoperatively on a number of outcome-based scores that included the UCLA score, ASES score and VAS score in the studies. The UCLA score was evaluated in 2 of the 5 studies with statistically significant improvement from preoperatively to postoperatively at the final follow-up. A standard mean difference of −0.155 (−0.615 to 0.306) was determined (p = 0.510), implying that no significant difference was found in the UCLA score among the two cohorts (Fig. 3A). Two studies among the five selected studies were evaluated for the ASES score. A standard mean difference of −0.024 (−0.532 to 0.483) was found (p = 0.925). No significant difference was observed between the two cohorts for the ASES score (Fig. 3B). The VAS score was evaluated in two studies. A standard mean difference of −0.198 (−0.311 to 0.708) was found (p = 0.446). No significant difference was observed regarding the VAS score between the two cohorts (Fig. 3C).
Figure 3.
Standard differences in means for functional scores (UCLA increased score, ASES score and VAS score) between biceps tenodesis and SLAP repair groups.
ASES = American Shoulder and Elbow Surgeons; SLAP = superior labrum anterior and posterior; UCLA = University of California at Los Angeles; VAS, visual analogue scale.
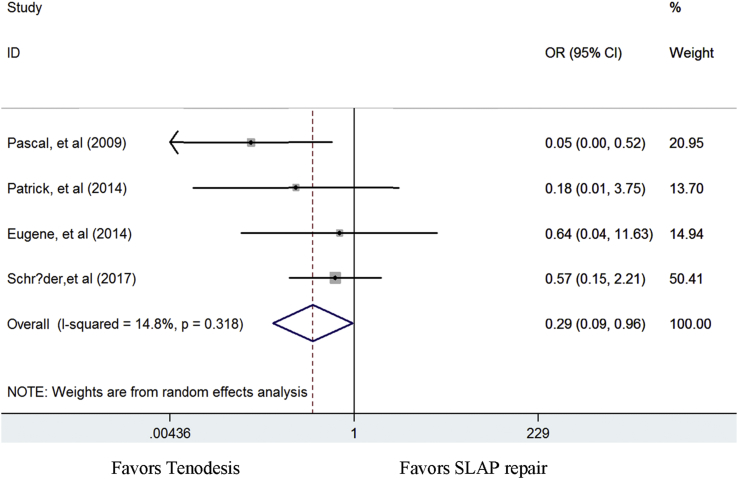
Patient satisfaction
Four studies evaluated the patients' satisfaction outcome. An odds ratio of 0.294 (0.091–0.955) was found in favour of tenodesis (p = 0.042), thereby indicating that the patient satisfaction was significantly better in the biceps tenodesis group than in the SLAP repair group (Fig. 4).
Figure 4.
Odds ratios for patient satisfaction between biceps tenodesis and SLAP repair groups.
SLAP = superior labrum anterior and posterior.
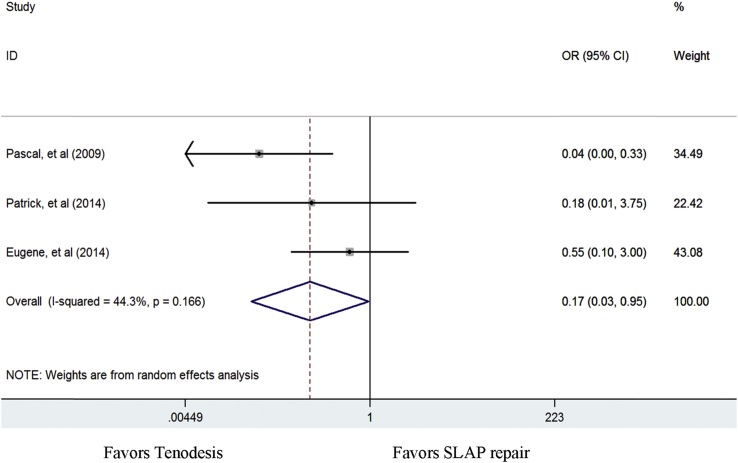
Return to sporting activity
Three of five studies selected had evaluated return to sporting activity between the two groups. An odds ratio of 0.170 (0.031–0.950) was measured in favour of the tenodesis group (p = 0.044), thus indicating that the incidence of patients who postoperatively return to reinjury sports activity was significantly better in the tenodesis group than in the SLAP repair group (Fig. 5).
Figure 5.
Odds ratios for patient return to sporting activity between biceps tenodesis and SLAP repair groups.
SLAP = superior labrum anterior and posterior.
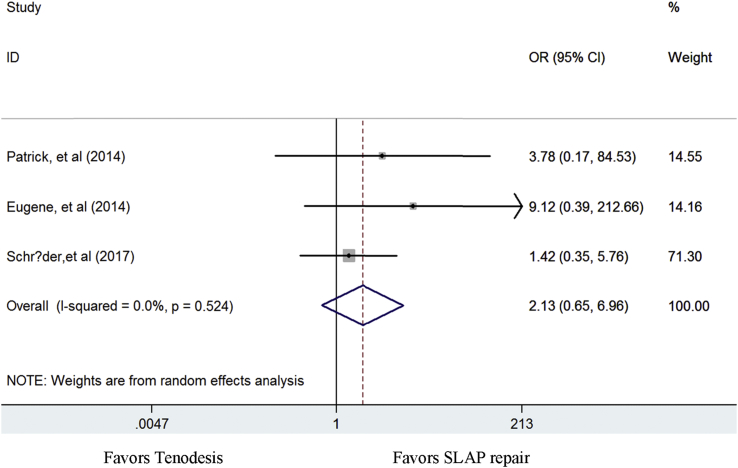
Postoperative stiffness
Postoperative stiffness was examined in three studies. An odds ratio of 2.127 (0.650–6.957) was measured (p = 0.212). No significant difference was found in the postoperative stiffness outcome among the two cohorts (Fig. 6).
Figure 6.
Odds ratios for postoperative stiffness between biceps tenodesis and SLAP repair groups.
SLAP = superior labrum anterior and posterior.
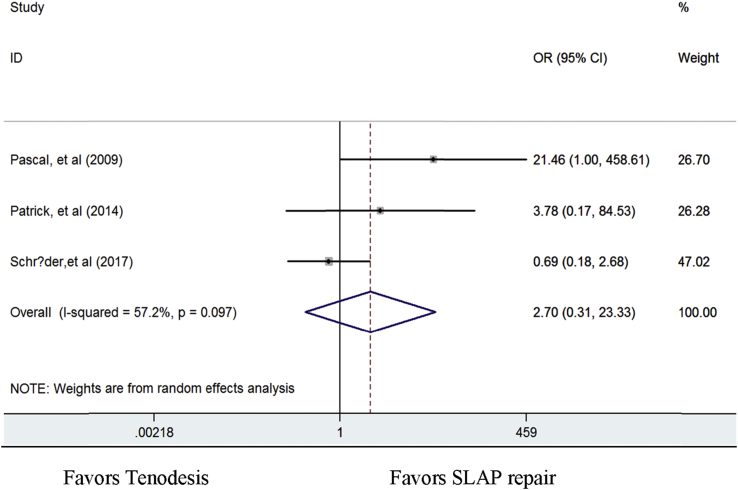
Reoperation
Reoperation was reported in three studies. An odds ratio of 2.698 (0.312–23.326) was measured (p = 0.097). No significant difference was found in the reoperation rate among the two cohorts (Fig. 7).
Figure 7.
Odds ratios for reoperation between biceps tenodesis and SLAP repair groups.
SLAP = superior labrum anterior and posterior.
Discussion
Type II SLAP lesions could cause severe pain during shoulder movement, especially overhead, or when lifting objects and significantly reduce ease of shoulder range of motion (ROM) and strength. The current surgical treatments generally comprise one of two, superior labral repair or biceps tenodesis. However, which of the two procedures is preferred treatment of Type II SLAP lesion is still an active debate in clinical field. In this study, we performed a meta-analysis to determine whether there is discrepancy in the outcomes between the two procedures postoperatively. Based on study design criteria, five articles (204 patients) were selected and assessed in this meta-analysis. The results obtained imply that the prevalence of the patient satisfaction and patients who return to preinjury sports level was significantly greater in the tenodesis group than in the SLAP repair group (p < 0.05) postoperatively. As for the measures such as patient age, VAS score, ASES score UCLA score, postoperative stiffness and reoperation rates, no significant differences was found among the two cohorts, thus conforming to the results reported in the currently available literature (p > 0.05).
Friel et al reported that arthroscopic SLAP repair of Type II lesions with bio-absorbable suture anchors could significantly ameliorate shoulder functional capacity and pain relief postoperatively [14]. However, other studies have reported poor results with patient satisfaction and return of activity after SLAP repair [15], [16], [17], [18], [19]. In a retrospective case study, Yung et al reported that postoperative UCLA scores in patients who underwent Type II SLAP repair ranged from excellent to moderate scores in 75% of patients, whereas the remaining 25% had poor UCLA scores [20]. Also, Boileau et al reported a constant improvement in scores from 65 to 83 points in patients after SLAP repair; however, 60% (6 of 10) of the patients reported to be disappointed due to chronic pain or failure to return to initial sports activity participation level [9]. Similarly, Cohen et al also found that although SLAP repair patients had high outcome scores, patient satisfaction could not be improved past 71%. In addition, around 41% of the patients reported experiencing some extent of shoulder pain during the night [21]. These results agreed with our findings that the prevalence of the patient satisfaction and the number of patients who return to preinjury sports activity level were significantly lower in SLAP repair group than in the tenodesis group (p < 0.05).
Age is an important factor that is considered an postoperative functional outcome for isolated SLAP repairs. Neri et al first evaluated age as one of the vital factors [22] and reported good-to-excellent outcomes with higher incidences of return to initial activity level for many suitably determined patients who underwent isolated Type II SLAP repair, regardless of the patients' age. On the other hand, numerous reports have indicated that the postoperative outcomes of SLAP repairs are unpredictable, notably in aged patients [23], [24]. Provencher et al evaluated 179 SLAP repair patients [7] at an average follow-up period of 40.4 months and documented that 66 patients reported failure of SLAP repair and 55 patients underwent revision surgery. Advanced age (>36 years) was a single measure, among the groups, that was associated with increased failure rate. However, in this study, we could only analyse difference in ages and reoperation rates in two groups separately, and we found that there were no significant difference in the age and reoperation rate between the two groups, which may have been due to the small number of studies and patient anticipations, were relatively small. Further prospective randomised controlled clinical studies with more patient anticipations are needed to clarify it.
Moreover, SLAP repair patients are at risk of developing postoperative stiffness, and the patients must also undergo extensive postoperative rehabilitations. Brockmeier et al reported that after SLAP repair surgery, four patients (8.5%) had observed severe shoulder stiffness. Among them, three patients achieved about 15° of the preinjury range of motion by conservative management, whereas the fourth patient had developed severe adhesive capsulitis and attained full motion after arthroscopic lysis of adhesion [4]. In our research, we found that three studies in SLAP repair and one study in tenodesis reported stiffness as the most common postoperative complication, which was resolved by conservative management such as physical therapy [25] or surgical management including capsular release [26] and tenodesis [27]. However, over long-term follow-up, there was no significant difference in incidences of postoperative stiffness between the two treatments.
In the United States, there is a decreasing trend in SLAP repair from 69.3% to 44.8%, whereas an increasing trend of incidences of biceps tenodesis from 1.9% to 18.8% was observed from 2003 to 2011 [28]. Erickson et al also studied the recent trends in SLAP repair surgeries between 2004 and 2014. They found that the total number of biceps tenodesis had significantly increased, whereas the number and relative percentage of SLAP repairs had significantly decreased over the past 10 years [29]. Furthermore, biceps tenodesis can also be used as revision treatment of failed SLAP repair. Boileau et al [9] reported that four patients with failed SLAP repairs underwent subsequent biceps tenodesis, with favourable outcomes and a full return to their previous level of sports activity. In view of this, we suggest that biceps tenodesis could be efficiently performed and achieve better outcomes in case of failed SLAP repair.
Limitations
In this study, there are a few limitations. First, the small number of studies was inducted for meta-analysis, and three of the included studies involved the use of a retrospective database. Second, comparatively small sample number of patients was available for analysis. Third, there was a lack of sufficient number of studies that focused on the outcome of biceps tenodesis in younger patients with Type II SLAP injury. These limitations could be overcome through a multicenter randomised controlled clinical study involving both older and younger patients.
Conclusions
Both the procedures, SLAP repair and biceps tenodesis, are effective in pain relief and recovery of functional activity in patients suffering from isolated Type II SLAP lesions. Compared with SLAP repair, biceps tenodesis could attain higher rate of patient satisfaction and greater number of patients could return to preinjury sports participation. In view of this, biceps tenodesis could be a preferable choice to SLAP repair, especially for failed SLAP repair patients.
Conflict of interest
All the authors declare no conflict of interest.
Acknowledgements
This research was supported by the National Natural Science Foundation of China (No. 81301578).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jot.2018.09.002.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Andrews J.R., Carson W.G., Jr., McLeod W.D. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13(5):337–341. doi: 10.1177/036354658501300508. [eng] [DOI] [PubMed] [Google Scholar]
- 2.Snyder S.J., Karzel R.P., Del Pizzo W., Ferkel R.D., Friedman M.J. SLAP lesions of the shoulder. Arthrosc: J Arthrosc Relat Surg: Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 1990;6(4):274–279. doi: 10.1016/0749-8063(90)90056-j. [eng] [DOI] [PubMed] [Google Scholar]
- 3.Snyder S.J., Banas M.P., Karzel R.P. An analysis of 140 injuries to the superior glenoid labrum. J Shoulder Elbow Surg. 1995;4(4):243–248. doi: 10.1016/s1058-2746(05)80015-1. [eng] [DOI] [PubMed] [Google Scholar]
- 4.Brockmeier S.F., Voos J.E., Williams R.J., 3rd, Altchek D.W., Cordasco F.A., Allen A.A. Outcomes after arthroscopic repair of type-II SLAP lesions. J Bone Jt Sur Am Vol. 2009;91(7):1595–1603. doi: 10.2106/JBJS.H.00205. [eng] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boesmueller S., Tiefenboeck T.M., Hofbauer M., Bukaty A., Oberleitner G., Huf W. Progression of function and pain relief as indicators for returning to sports after arthroscopic isolated type II SLAP repair—a prospective study. BMC Muscoskel Disord. 2017;18(☆) doi: 10.1186/s12891-017-1620-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huri G., Hyun Y.S., Garbis N.G., McFarland E.G. Treatment of superior labrum anterior posterior lesions: a literature review. Acta Orthop Traumatol Turcica. 2014;48(3):290–297. doi: 10.3944/AOTT.2014.3169. [eng] [DOI] [PubMed] [Google Scholar]
- 7.Provencher M.T., McCormick F., Dewing C., McIntire S., Solomon D. A prospective analysis of 179 type 2 superior labrum anterior and posterior repairs: outcomes and factors associated with success and failure. Am J Sports Med. 2013;41(4):880–886. doi: 10.1177/0363546513477363. [eng] [DOI] [PubMed] [Google Scholar]
- 8.Waterman M.B.R., Arroyo C.W., Heida C.K., Burks C.R., Pallis C.M. SLAP repairs with combined procedures have lower failure rate than isolated repairs in a military population: surgical outcomes with minimum 2-year follow-up. Orthop J Sports Med. 2015;3(8):861–873. doi: 10.1177/2325967115599154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Boileau P., Parratte S., Chuinard C., Roussanne Y., Shia D., Bicknell R. Arthroscopic treatment of isolated type II SLAP lesions: biceps tenodesis as an alternative to reinsertion. Am J Sports Med. 2009;37(5):929–936. doi: 10.1177/0363546508330127. [DOI] [PubMed] [Google Scholar]
- 10.Alpert J.M., Wuerz T.H., O'Donnell T.F., Carroll K.M., Brucker N.N., Gill T.J. The effect of age on the outcomes of arthroscopic repair of type II superior labral anterior and posterior lesions. Am J Sports Med. 2010;38(11):2299–2303. doi: 10.1177/0363546510377741. [eng] [DOI] [PubMed] [Google Scholar]
- 11.Denard P.J., Ladermann A., Burkhart S.S. Long-term outcome after arthroscopic repair of type II SLAP lesions: results according to age and workers' compensation status. Arthrosc: J Arthrosc Relat Surg: Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2012;28(4):451–457. doi: 10.1016/j.arthro.2011.09.005. [eng] [DOI] [PubMed] [Google Scholar]
- 12.Kanatli U., Ozturk B.Y., Bolukbasi S. Arthroscopic repair of type II superior labrum anterior posterior (SLAP) lesions in patients over the age of 45 years: a prospective study. Arch Orthop Trauma Surg. 2011;131(8):1107–1113. doi: 10.1007/s00402-011-1348-8. [eng] [DOI] [PubMed] [Google Scholar]
- 13.Schroder C.P., Skare O., Gjengedal E., Uppheim G., Reikeras O., Brox J.I. Long-term results after SLAP repair: a 5-year follow-up study of 107 patients with comparison of patients aged over and under 40 years. Arthrosc: J Arthrosc Relat Surg: Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2012;28(11):1601–1607. doi: 10.1016/j.arthro.2012.02.025. [eng] [DOI] [PubMed] [Google Scholar]
- 14.Friel N.A., Karas V., Slabaugh M.A., Cole B.J. Outcomes of type II superior labrum, anterior to posterior (SLAP) repair: prospective evaluation at a minimum two-year follow-up. J Shoulder Elbow Surg. 2010;19(6):859–867. doi: 10.1016/j.jse.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim S.H., Ha K.I., Choi H.J. Results of arthroscopic treatment of superior labral lesions. J Bone Jt Surg Am Vol. 2002;84-A(6):981. doi: 10.2106/00004623-200206000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Ide J., Maeda S., Takagi K. Sports activity after arthroscopic superior labral repair using suture anchors in overhead-throwing athletes. Am J Sports Med. 2005;33(4):507–514. doi: 10.1177/0363546504269255. [DOI] [PubMed] [Google Scholar]
- 17.Gorantla K., Gill C., Wright R.W. The outcome of type II SLAP repair: a systematic review. Arthrosc J Arthrosc Relat Surg. 2010;26(4):537–545. doi: 10.1016/j.arthro.2009.08.017. [DOI] [PubMed] [Google Scholar]
- 18.Katz L.M., Hsu S., Miller S.L., Richmond J.C., Khetia E., Kohli N. Poor outcomes after SLAP repair: descriptive analysis and prognosis. Arthrosc: J Arthrosc Relat Surg: Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2009;25(8):849–855. doi: 10.1016/j.arthro.2009.02.022. [eng] [DOI] [PubMed] [Google Scholar]
- 19.Zhao C., Hu J.T., Kong M.X., Qiu B.S., Gu H.F., Zhang S.J. Case-control study on superior labrum from anterior to posterior repair and biceps tenodesis for the treatment of type II SLAP injury. Zhongguo Gu Shang. 2015;28(6):531–535. [PubMed] [Google Scholar]
- 20.Yung P.S., Fong D.T., Kong M.F., Lo C.K., Fung K.Y., Ho E.P. Arthroscopic repair of isolated type II superior labrum anterior-posterior lesion. Knee Surg Sports Traumatol Arthrosc: Off J ESSKA. 2008;16(12):1151–1157. doi: 10.1007/s00167-008-0629-4. [eng] [DOI] [PubMed] [Google Scholar]
- 21.Cohen D.B., Coleman S., Drakos M.C., Allen A.A., O'Brien S.J., Altchek D.W. Outcomes of isolated type II SLAP lesions treated with arthroscopic fixation using a bioabsorbable tack. Arthrosc J Arthrosc Relat Surg. 2006;22(2):136–142. doi: 10.1016/j.arthro.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 22.Neri B.R., Vollmer E.A., Kvitne R.S. Isolated type II superior labral anterior posterior lesions: age-related outcome of arthroscopic fixation. Am J Sports Med. 2009;37(5):937–942. doi: 10.1177/0363546508328417. [eng] [DOI] [PubMed] [Google Scholar]
- 23.Erickson J., Lavery K., Monica J., Gatt C., Dhawan A. Surgical treatment of symptomatic superior labrum anterior-posterior tears in patients older than 40 years: a systematic review. Am J Sports Med. 2015;43(5):1274–1282. doi: 10.1177/0363546514536874. [DOI] [PubMed] [Google Scholar]
- 24.Weber S.C., Martin D.F., Rd S.J., Harrast J.J. Superior labrum anterior and posterior lesions of the shoulder: incidence rates, complications, and outcomes as reported by American Board of Orthopedic Surgery. Part II candidates. Am J Sports Med. 2012;40(7):1538–1543. doi: 10.1177/0363546512447785. [DOI] [PubMed] [Google Scholar]
- 25.Ek E.T., Shi L.L., Tompson J.D., Freehill M.T., Warner J.J. Surgical treatment of isolated type II superior labrum anterior-posterior (SLAP) lesions: repair versus biceps tenodesis. J Shoulder Elbow Surg. 2014;23(7):1059–1065. doi: 10.1016/j.jse.2013.09.030. [DOI] [PubMed] [Google Scholar]
- 26.Denard P.J., Parsley B.K., Burkhart S.S. Arthroscopic biceps tenodesis compared with repair of isolated type II SLAP lesions in patients older than 35 years. Orthopedics. 2014;37(3):e292–e297. doi: 10.3928/01477447-20140225-63. [DOI] [PubMed] [Google Scholar]
- 27.Schrøder C.P., Skare Ø., Reikerås O., Mowinckel P., Brox J.I. Sham surgery versus labral repair or biceps tenodesis for type II SLAP lesions of the shoulder: a three-armed randomised clinical trial. Br J Sports Med. 2017;51(24):1759–1766. doi: 10.1136/bjsports-2016-097098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mackinnonpatterson B., Creighton R.A., Spang J.T., Kamath G.V. Surgical trends in the treatment of superior labrum anterior and posterior (SLAP) lesions of the shoulder. Analysis of data from the American Board of Orthopaedic Surgery Certification Examination Database. Am J Sports Med. 2014;2(2 Suppl):1904–1910. doi: 10.1177/0363546514534939. [DOI] [PubMed] [Google Scholar]
- 29.Erickson B.J., Jain A., Abrams G.D., Nicholson G.P., Cole B.J., Romeo A.A. SLAP lesions: trends in treatment. Arthrosc: J Arthrosc Relat Surg: Off Publ Arthrosc Assoc N Am Int Arthrosc Assoc. 2016;32(6):976–981. doi: 10.1016/j.arthro.2015.11.044. [eng] [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.