Abstract
Introduction:
Despite awareness of overall poor survival rates following cardiopulmonary resuscitation (CPR), some orthopedic patients with significant comorbidities continue to have inappropriate resuscitation plans. Furthermore, in certain injury groups such as patients with hip fractures, survival outcome data are very limited; current discussions regarding resuscitation plans may be inaccurate. This study assesses survival in orthopedic patients following CPR, to inform decision-making between physicians, surgeons, and patients.
Methods:
A dual center, retrospective cohort study was performed analyzing all orthopedic admissions that received CPR over a 25-month period, with a minimum of 1 year follow-up. National Cardiac Arrest Audit data, “mortality and morbidity” meeting records, National Hip Fracture Databases, and electronic notes were analyzed. Survival duration was measured, alongside reason for admission, location CPR occurred, and initial rhythm encountered.
Results:
Thirty-two patients received CPR over the 25-month period (median age: 83; range: 30-96). Three (9%) of 32 patients survived to discharge. Only 1 of the 26 patients older than 65 years survived to discharge. Fifteen (47%) of 32 had hip fractures, where 4 (27%) of 15 of this group survived 24 hours; none survived to discharge. When recorded, 22 (92%) of 24 initially had a nonshockable rhythm.
Discussion:
Cardiopulmonary resuscitation was conceptualized as a treatment for reversible cardiopulmonary causes. When used in trauma and orthopedic patients, especially older and/or hip fracture patients, it seldom led to hospital discharge. Different admission practices such as “front door” orthogeriatric reviews may explain the contrast in usage of CPR between the hospitals.
Conclusion:
Survival rates following CPR were very low, with it proving specifically ineffective in hip fracture patients. Although every decision about resuscitation should be patient centered and individualized, this study will allow clinicians to be more realistic about outcomes from CPR, particularly in the hip fracture group.
Keywords: geriatric medicine, geriatric trauma, trauma surgery, hospitalist, cardiopulmonary resuscitation, hip fracture, survival
Introduction
Poor understanding of the role of cardiopulmonary resuscitation (CPR) has been associated with its inappropriate use and undignified deaths. CPR was conceived as a treatment for reversible situations that led to a cardiopulmonary arrest.1 However, survival following CPR remains around 15% to 20% for in-hospital arrests with poorer outcomes in patients with frailty and comorbidities.2,3 With age, survival rates worsen further with 11% to 15% of patients aged 80 years and older surviving to discharge (with only 20% of these patients living independently).4,5 This implies that a significant proportion of patients receive CPR inappropriately which may be an inefficient use of resuscitation resources. As there is minimal evidence assessing outcomes in orthopedic patients, informed decision-making regarding resuscitation status is difficult. This problem is magnified in the 65 000 patients who sustain hip fractures each year in the United Kingdom,6 as there is no research on the survival rates following CPR in these patients.
In this study, we aim to establish the survival rates for trauma and orthopedic patients following in-hospital CPR, with specific analysis of patients with hip fractures, to inform and enhance discussions between clinicians, patients, and their relatives.
Methods
A dual center, retrospective cohort study was performed analyzing all orthopedic admissions (trauma and elective) that received CPR between May 1, 2014, and May 31, 2016, at North Bristol NHS Trust, United Kingdom (NBT) and the Royal United Hospitals Bath NHS Foundation Trust, Bath, United Kingdom (RUH). The NBT is a major trauma center, where hip fracture patients are initially managed by orthopedic surgeons with input from orthogeriatricians, whereas the RUH is a district general hospital, where these patients are admitted under the care of orthogeriatricians with orthopedic input. Patient data, including who received CPR during their hospital admission, were identified from the National Cardiac Arrest Audit database, morbidity and mortality meeting data, patient notes, freedom of information requests, and discharge summaries. Patient demographics and reasons for admission were recorded. The primary outcome measure was survival to discharge. Secondary outcome measures recorded were rhythm initially encountered, return of spontaneous circulation (ROSC), survival to 24 hours, to 48 hours, and to 1 year. Separate analysis of patients admitted with hip fractures was performed, which utilized the National Hip Fracture Database 2015 and 2016 reports7,8 to estimate the number of hip fracture patients in each hospital over the 25-month period.
Statistical analyses were performed using IBM SPSS Statistics for Windows, version 20 (IBM Corp, Armonk, New York), with significance accepted at an α level of P < .05. Wilcoxon-Mann-Whitney tests were used to examine differences between groups (hip fracture presence or absence, age younger or older than 65 years).
Results
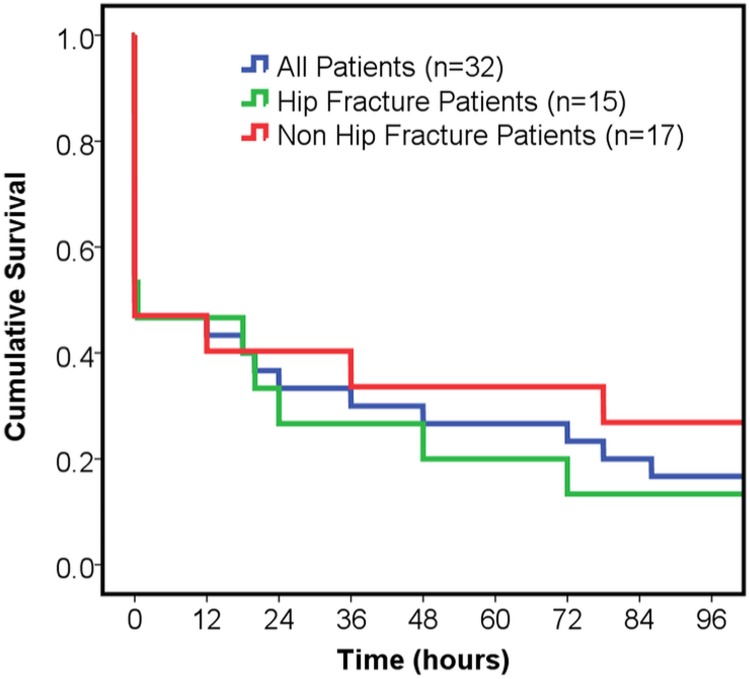
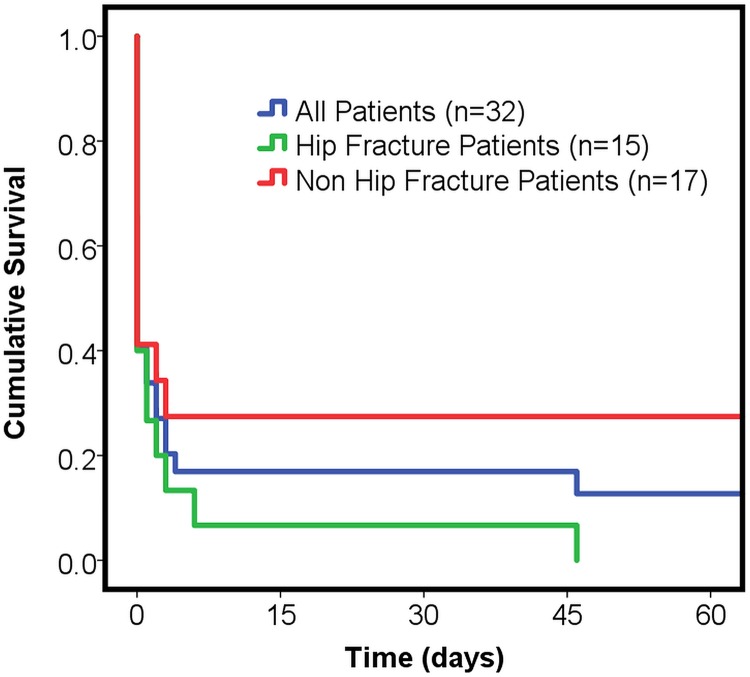
Thirty-two trauma and orthopedic patients were identified as having received CPR over the 25-month period, median age 83 (range: 30-96); 25 at NBT and 7 at RUH (Table 1). This represents 0.1% of all elective and trauma orthopedic patients in each hospital; 17 430 and 8283 patients were admitted to each hospital, respectively, during this period (Freedom of Information requests, August 2018). Fifteen (47%) patients achieved ROSC with only 10 (31%) patients surviving 24 hours or more, and 3 (9%) patients surviving to discharge (Figures 1 and 2). Twenty-six patients were admitted with lower limb conditions (3 of these electively and 15 were patients with hip fractures), 3 were polytrauma patients, 2 had upper limb fractures, and 1 patient had a spinal fragility fracture.
Table 1.
Survival and Initial Encountered Rhythm Data for All Patients and Patients With and Without Hip Fractures for Both Hospitals.
| Variable | All Patients | Hip Fracture Patients | Non-Hip Fracture Patients | Patients Above 65 Years | Patients Below 65 Years |
|---|---|---|---|---|---|
| Median age when receiving CPR (range) | 83 (30-96) | 85 (67-96) | 73 (30-93) | 82 (67-96) | 50 (30-61) |
| Number of patients receiving CPR | 32 | 15 | 17 | 26 | 6 |
| Number of patients surviving to: | |||||
| ROSC | 15 (47%) | 8 (53%) | 7 (41%) | 12 (46%) | 3 (50%) |
| 24 hours | 10 (31%) | 4 (27%) | 6 (35%) | 7 (27%) | 3 (50%) |
| 48 hours | 8 (25%) | 3 (20%) | 5 (29%) | 5 (19%) | 3 (50%) |
| Discharge | 3 (9%) | 0 (0%) | 3 (18%) | 1 (4%) | 2 (33%) |
| One year | 3 (9%) | 0 (0%) | 3 (18%) | 1 (4%) | 2 (33%) |
| Initial rhythm recorded: | |||||
| PEA | 17 (53%) | 7 (47%) | 10 (59%) | 13 (50%) | 4 (66%) |
| Asystole | 5 (16%) | 0 (0%) | 5 (29%) | 4 (15%) | 1 (17%) |
| Pulseless VT | 2 (6%) | 1 (7%) | 1 (6%) | 1 (4%) | 1 (17%) |
| Not recorded | 8 (25%) | 7 (47%) | 1 (6%) | 8 (31%) | 0 (0%) |
| Location CPR performed: | |||||
| Theaters | 9 (28%) | 6 (40%) | 3 (18%) | 6 (23%) | 3 (50%) |
Abbreviations: CPR, cardiopulmonary resuscitation; ROSC, return of spontaneous circulation; PEA, Pulseless Electrical Activity; VT, Ventricular Tachycardia.
Figure 1.
Kaplan-Meier survival curve for first 96 hours, showing all patients (n = 32) in blue, hip fracture patients (n = 15) in green, and non-hip fracture patients (n = 17) in red.
Figure 2.
Kaplan-Meier survival curve for first 60 days, showing all patients (n = 32) in blue, hip fracture patients (n = 15) in green, and non-hip fracture patients (n = 17) in red.
No patients with hip fractures who received CPR survived to discharge. The patients living to discharge were a 55-year-old male admitted as a polytrauma, an 88-year-old male with a humeral shaft fracture (the only patient older than 65 to survive to discharge) and a 30-year-old male admitted for elective removal of ankle metalwork.
In the hospital where the orthogeriatric services admit patients with hip fractures, rather than the orthopedic doctors, none received CPR. This contrasts with 15 such patients in the other hospital receiving this treatment. The proportion of all hip fracture patients admitted to both hospitals receiving CPR were 15 (1.5%) of 1001 at NBT and 0 (0%) of 1153 at RUH. Using 30-day mortality data from the National Hip Fracture Database reports, within this period approximately 75 and 82 patients died at NBT and RUH, respectively. As 15 hip fracture patients received CPR at NBT in this same period, at least 20% of all hip fracture patients who died in the NBT hospital received CPR that did not result in discharge from hospital.
Assessing all cases, the initial rhythm was recorded in 24 (75%) of 32 cases, with 22 (92%) of 24 of those recorded showing a nonshockable rhythm (Pulseless Electical Activity (PEA) or asystole); the 3 patients surviving to discharge had PEA arrests. Overall, 9 (28%) of 32 patients received CPR intraoperatively or in recovery; this figure was 6 (40%) of 15 for patients admitted with hip fractures (P > .05). Of these 9 intra- or perioperative cases, 2 patients survived to discharge (a polytrauma patient and a patient admitted for elective metalwork removal).
Discussion
Cardiopulmonary resuscitation attempts were generally unsuccessful, with only 9% of patients, over a 25-month period, surviving to discharge. With 1.5% of patients with hip fractures in one hospital receiving CPR during their admission, yet none surviving to discharge, this highlights the poor outcomes that can be anticipated and are experienced. However, this also demonstrates that do not attempt CPR (DNACPR) orders are potentially being used more appropriately for patients with hip fractures in the other hospital as no CPR was administered to this group, with no significant difference in the 30-day mortality rate during the assessed period (7.1% at RUH, 7.5% at NBT; P = .19).7,8
Hip fractures most frequently occur in frail and elderly patients. In many situations, their injury is a surrogate marker for their overall health status, and thus, such patients are vulnerable to acute deteriorations in their chronic clinical or subclinical conditions. They frequently have multiple comorbidities, life-limiting conditions, poor mobility, and the need for significant help with activities of daily living. Cardiopulmonary arrests are often a result of acute-on-chronic end-organ failure rather than a reversible acute event.9 Hence, as CPR is associated with low survival to discharge rates even when used to treat reversible conditions in otherwise well patients, it is unsurprising that none of the patients with hip fractures in this study survived to be discharged.
A DNACPR order is created to prevent inappropriate resuscitation. The legality behind this process and where the decision-making lies differs worldwide.10 In the United Kingdom, the decision to perform CPR is ultimately the choice of medical professionals, with patient involvement throughout the decision-making process.11 In the United States, however, DNACPR orders remain exclusively a patient decision, and in other countries, they may not be recognized at all.12 When making the decision to complete a DNACPR order, it is vital to communicate clearly with both the patient and their relatives; the only exception to this would be if the medical team felt such a discussion would cause extreme stress and/or harm to the patient.13 Historically, clinicians have been found to struggle with DNACPR requests,14 with several reasons for this suggested, including fear of litigation,15 poor communication with patients,16-18 and concerns about creating fear by focusing on the patient’s chance of survival.19,20 Discussing CPR early and having the appropriately trained staff available for these discussions can have a significant impact on the overall use of CPR, whereas delays can result in it being administered inappropriately. When actual survival rates are discussed with patients, their decision to potentially receive CPR often changes.21-24 The outcome rates from this study can help in these discussions with patients and their families by providing quantitative outcomes to enable informed, shared decision-making.
In addition to the survival rates recorded, other predictors of a poor outcome were frequently found during CPR in hip fracture patients. Nonshockable rhythms reflect nonarrhythmogenic causes for cardiac arrest and are associated with poorer rates of survival.4 This study found that, when documented, PEA/asystole was the most common initial rhythm encountered, seen in 92% of cases. This compares with the national figure of 72% when considering patients with any condition.4 This may explain the differences in overall survival rates in this study compared to other patient populations.
This study also noted that in 28% of cases, CPR was administered intraoperatively or in recovery. This may have been as a result of appropriate decision-making, that is, a positive decision to perform CPR in theater but not in the ward environment, given the anticipated greater chance of a reversible cause being involved in any arrest in theater.25 Regardless, this highlights the importance of deciding on resuscitation status prior to any surgery, with clear documentation in the patient’s notes regarding what conditions would and would not warrant CPR. One study showed that 30% of physicians and 18% of anesthetists felt that DNACPR orders should be suspended intraoperatively.26 However, complete suspension is thought by others to not be justified,27 as adequate preoperative discussion should be had instead.28 Events occurring during operations emphasize that this is a very high-risk patient group; and thus, the presence of senior anesthetists and surgeons intraoperatively is vital.
There are some limitations with this study. Firstly, in patients who survived following CPR, there was no assessment of cerebral status, nor place of discharge. This information would provide a better insight into each patient’s outcome and whether they returned to their previous functional level. Secondly, the timing, location, and content of the DNACPR discussions were not recorded, in part because there are no standardized processes for when, or with whom, these decisions should occur. Thirdly, a small number of cardiac arrests may have been unrecorded in the sources used and therefore not included in the study. For example, an intraoperative cardiac arrest may have been successfully managed by anesthetists in theater, with no cardiac arrest call made. Fourthly, as the calculations for hip fracture patients who received unsuccessful in-hospital CPR used 30-day mortality data, it will also include patients who died postdischarge. Thus, as the total number of in-hospital deaths is likely to be less than the 30-day figure, it potentially means that the 20% calculated is an underestimation. Fifthly, the case mix of patients presenting to each hospital is different; NBT is a major trauma center whereas the RUH is a district general hospital with an older demographic. Further to this, there is a policy at the RUH to admit hip fracture patients under orthogeriatric care with orthopedic input, rather than initially under the care of orthopedic surgeons. This “front door” approach to managing such patients facilitates early opportunities for patients and their families to discuss the role of CPR with a trained physician. Such discussions with an experienced physician can be invaluable for both the patient and their family and may explain why no patients with hip fractures received CPR at the RUH. Finally, all orthopedic admissions were included, totaling 25 713 trauma and elective orthopedic, of which approximately 2154 were hip fracture patients. However, as the percentage of all patients (0.1%) receiving CPR was small, the total number eligible for inclusion in this study potentially limits its validity. This means that few further associations can be deduced from the data, with any potential differences between groups being undetected due to an increased chance of a type 2 error. Nevertheless, the overall trends in outcomes consistently suggest that hip fracture patients have very poor outcomes from CPR, and its use should be considered carefully when they are admitted to hospital.
Conclusions
Cardiopulmonary resuscitation in trauma and orthopedic patients is associated with poor outcomes with only 9% surviving to 1 year. Patients with hip fractures have been shown to have worse outcomes, with none such patients in this study even surviving to discharge. This is the first time the specific ineffectiveness of CPR in hip fracture patients has been reported and supports the existing data on the overall low survival rates following CPR. Although every decision about resuscitation should be patient centered and individualized, this information can be used to better inform DNACPR discussions with patients and their relatives.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: James W. A. Fletcher  https://orcid.org/0000-0003-4147-5013
https://orcid.org/0000-0003-4147-5013
References
- 1. Jude JR, Kouwenhoven WB, Knickerbocker GG. Cardiac arrest: report of application of external cardiac massage on 118 patients. JAMA. 1961;178(11):1063–1070. [DOI] [PubMed] [Google Scholar]
- 2. Sulzgruber P, Sterz F, Poppe M, et al. Age-specific prognostication after out-of-hospital cardiac arrest—The ethical dilemma between ‘life-sustaining treatment’ and ‘the right to die’ in the elderly. Eur Heart J Acute Cardiovasc Care. 2017;6(2):112–120. [DOI] [PubMed] [Google Scholar]
- 3. Andrew E, Nehme Z, Bernard S, Smith K. The influence of comorbidity on survival and long-term outcomes after out-of-hospital cardiac arrest. Resuscitation. 2017;110:42–47. [DOI] [PubMed] [Google Scholar]
- 4. Nolan JP, Soar J, Smith GB, et al. Incidence and outcome of in-hospital cardiac arrest in the United Kingdom National Cardiac Arrest Audit. Resuscitation. 2014;85(8):987–992. [DOI] [PubMed] [Google Scholar]
- 5. van Gijn MS, Frijns D, van de Glind EM, C van Munster B, Hamaker ME. The chance of survival and the functional outcome after in-hospital cardiopulmonary resuscitation in older people: a systematic review. Age Ageing. 2014;43(4):456–463. [DOI] [PubMed] [Google Scholar]
- 6. Royal College of Physicians. National Hip Fracture Database Annual Report 2017. London, United Kingdom: RCP, 2017. [Google Scholar]
- 7. Royal College of Physicians. National Hip Fracture Database Annual Report 2015. London, United Kingdom: RCP, 2015. [Google Scholar]
- 8. Royal College of Physicians. National Hip Fracture Database Annual Report 2016. London, United Kingdom: RCP, 2016. [Google Scholar]
- 9. Resuscitation Council (UK). Advanced Life Support. 7th ed London, United Kingdom: Resuscitation Council (UK); 2016. [Google Scholar]
- 10. Gibbs AJO, Malyon AC, Fritz ZBM. Themes and variations: an exploratory international investigation into resuscitation decision-making. Resuscitation. 2016;103:75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. British Medical Association, Resuscitation Council (UK), Royal College of Nursing. Decisions Relating to Cardiopulmonary Resuscitation. London, United Kingdom: 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Meñaca A, Evans N, Andrew EVW, et al. End-of-life care across Southern Europe: a critical review of cultural similarities and differences between Italy, Spain and Portugal. Crit Rev Oncol Hematol. 2012;82(3):387–401. [DOI] [PubMed] [Google Scholar]
- 13. R (On behalf of David Tracey personally and on behalf of the Estate of Janet Tracey (Deceased)) v (1) Cambridge University Hospitals NHS Foundation Trust (2) Secretary of State for Health, (EWCA Civ 822.54 2014).
- 14. Ebell MH, Afonso AM. Pre-arrest predictors of failure to survive after in-hospital cardiopulmonary resuscitation: a meta-analysis. Fam Pract. 2011;28(5):505–515. [DOI] [PubMed] [Google Scholar]
- 15. Fried T, Miller M, Stein M, et al. The slow code. N Engl J Med. 1998;1998(338):1921–1923. [Google Scholar]
- 16. Kernerman P, Cook DJ, Griffith LE. Documenting life-support preferences in hospitalized patients. J Crit Care. 1997;12(4):155–160. [DOI] [PubMed] [Google Scholar]
- 17. Mirza A, Kad R, Ellison NM. Cardiopulmonary resuscitation is not addressed in the admitting medical records for the majority of patients who undergo CPR in the hospital. Am J Hosp Palliat Med. 2005;22(1):20–25. [DOI] [PubMed] [Google Scholar]
- 18. Hofmann JC, Wenger NS, Davis RB, et al. Patient preferences for communication with physicians about end-of-life decisions. Ann Intern Med. 1997;127(1):1–12. [DOI] [PubMed] [Google Scholar]
- 19. Lynn J, Harrell FE, Jr, Cohn F, Hamel MB. Defining the terminally ill: insights from support. Duquesne Law Rev. 1996;35(1):311–336. [PubMed] [Google Scholar]
- 20. de Pentheny O’Kelly C, Urch C, Brown EA. The impact of culture and religion on truth telling at the end of life. Nephrol Dial Transplant. 2011;26(12):3838–3842. [DOI] [PubMed] [Google Scholar]
- 21. Murphy DJ, Burrows D, Santilli S, et al. The influence of the probability of survival on patients’ preferences regarding cardiopulmonary resuscitation. N Engl J Med. 1994;330(8):545–549. [DOI] [PubMed] [Google Scholar]
- 22. Jones GK, Brewer KL, Garrison HG. Public expectations of survival following cardiopulmonary resuscitation. Acad Emerg Med. 2000;7(1):48–53. [DOI] [PubMed] [Google Scholar]
- 23. Callahan EH, Thomas DC, Goldhirsch SL, Leipzig RM. Geriatric hospital medicine. Med Clin North Am. 2002;86(4):707–729. [DOI] [PubMed] [Google Scholar]
- 24. Cherniack EP. Increasing use of DNR orders in the elderly worldwide: whose choice is it? J Med Ethics. 2002;28(5):303–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Clemency MV, Thompson NJ. Do not resuscitate orders in the perioperative period: patient perspectives. Anesth Analg. 1997;84(4):859–864. [DOI] [PubMed] [Google Scholar]
- 26. Burkle CM, Swetz KM, Armstrong MH, Keegan MT. Patient and doctor attitudes and beliefs concerning perioperative do not resuscitate orders: anesthesiologists’ growing compliance with patient autonomy and self-determination guidelines. BMC Anesthesiol. 2013;13:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Truog Robert D, Waisel David B, Burns Jeffrey P. DNR in the OR: a goal-directed approach. Anesthesiology. 1999;90(1):289–295. [DOI] [PubMed] [Google Scholar]
- 28. Sumrall WD, Mahanna E, Sabharwal V, Marshall T. Do not resuscitate, anesthesia, and perioperative care: a not so clear order. Ochsner J. 2016;16(2):176–179. [PMC free article] [PubMed] [Google Scholar]