Abstract
Purpose:
To present a case of a complicated intracorneal ring segment (ICRS) implantation procedure in a patient with keratoconus, who experienced significant visual improvement, although the ICRS implantation had to be aborted.
Methods:
A 25-year-old female patient with keratoconus underwent femtosecond laser-assisted ICRS implantation in her right eye (OD) for improving visual acuity.
Results:
The procedure had to be aborted, because ICRS implantation was not possible. Anterior segment imaging 1 month after the procedure showed full-thickness corneal incision with corneal microperforation. However, patient’s visual acuity improved significantly due to amelioration of the keratometric findings. Keratometric and visual improvement was preserved at 6 months postoperatively.
Conclusion:
Our case report shows that femtosecond laser-assisted full-thickness corneal incision on the astigmatic axis combined with the intracorneal tunnel creation resulted unexpectedly in keratometric and visual improvement in this keratoconus patient, even without the implantation of the ICRS.
Keywords: full-thickness corneal incision, induced fibrogenesis, intracorneal ring segment, keratoconus, visual improvement
Introduction
Intracorneal ring segments (ICRS) are polymethyl methacrylate (PMMA) implants, which are inserted into the cornea aiming to alter its geometry in a manner that it will enhance its refractive properties and thereby will improve visual acuity. The use of ICRS implantation for the management of keratoconus was first introduced in 2000.1 Implantation was initially managed mechanically, but over the last years femtosecond laser-assisted implantation has been gaining increasing interest and gradually replaced the conventional mechanical technique.2
It has been documented that the implantation of ICRS decreases keratometric readings, spherical equivalent, and cylinder, reduce high-order aberrations, and improve uncorrected distance visual acuity (UDVA) and corrected distance visual acuity (CDVA) in patients with keratoconus.3,4 Complication rate is relatively low and mostly includes infections, ICRS displacement, migration or extrusion, corneal scarring, and corneal vascularization.5,6
Hereby, we report the unexpected visual and keratometric improvement in a period of 6 months of a female keratoconus patient who underwent an aborted femtosecond laser-assisted ICRS implantation that resulted in unexpected keratometric and visual improvement. The patient provided a written informed consent for publication of clinical data and images.
Case report
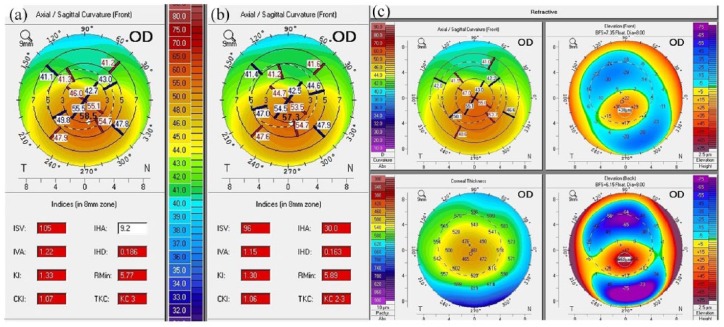
A 25-year-old female patient with keratoconus attended our clinic in February 2017. UDVA was 3/10 on the right eye (OD) and 2/10 on the left (OS). CDVA was 7/10 (8/10 with pinhole) and 6/10 (10/10 with pinhole). Refraction OD was −0.75/−4.00/87° and OS −4.25/−3.50/122°. Corneal topography showed Kmax 58.5 D OD and 58.9 D OS, while the thinnest point of corneal pachymetry was measured at 465 and 468 µm, respectively (Figure 1(a)). The patient had undergone bilateral corneal collagen crosslinking (CXL) for progressive keratoconus in 2014, resulting in a stable cornea. For visual improvement purposes and due to contact lens intolerance, we decided to proceed with a femtosecond laser-assisted ICRS implantation on the right eye. In regard to our nomogram, we recommended an implantation of one Keraring with 210° length and 300 µm thickness. The patient agreed and provided her written consent for the scheduled procedure in March 2017.
Figure 1.
Corneal topography of right eye (OD) with keratoconus showing Kmax of 58.9 D before intracorneal ring segment (ICRS) implantation (a), Kmax of 57.3 D 1 month after (b) and corneal topography of right eye with keratoconus showing Kmax of 57.7 D and the thinnest pachymetric point at 459 µm 6 months after complicated femtosecond laser-assisted ICRS implantation (c).
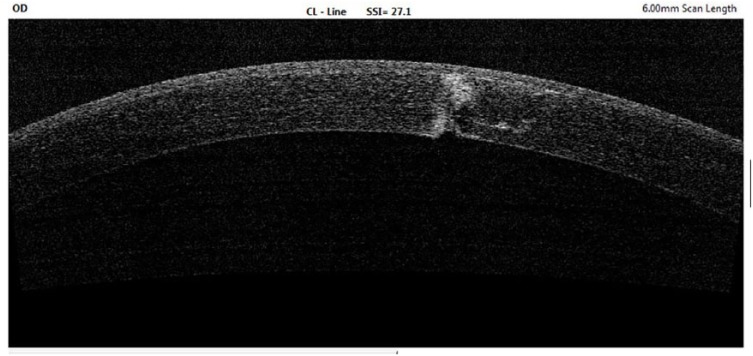
Briefly, after topical anesthesia with proparacaine hydrochloride 0.5%, the corneal apex was marked with ink under a surgical microscope Zeiss OPMI LUMERA 700 (Carl Zeiss Jena GmbH, Jena, Germany). A suction ring of 9.5 mm was applied, and after applanation a corneal tunnel of 1.3 mm width was created with the Leonardo da Vinci Femtosecond Laser (LDV Z6; Ziemer Ophthalmic Systems AG, Allmendstrasse, Switzerland) in the 5-mm zone with 80% corneal depth, as well as a single, radial, 2.7-mm corneal incision at the tunnel starting point. The corneal tunnel length was equal to the ring segment arc length plus 10°. However, the intracorneal ring was never introduced, due to corneal perforation at the incision site resulting in air bubbles in the anterior chamber and termination of the procedure.
Postoperatively, regimen for the next 2 weeks four times per day included chloramphenicol 0.5% and ofloxacin 0.3% eye drops. Fluorometholone 0.1% eye drops were administered four times per day for 4 weeks. A bandage contact lens was also applied (PureVision; Bausch & Lomb Inc., Rochester, NY, USA).
On postoperative follow-up 1 month after the procedure, UDVA was 8/10 and CDVA was 10/10. Refraction was measured at −1.00/–3.00/80°. Corneal topography showed Kmax of 57.3 D with the thinnest pachymetric point at 469 µm (Figure 1(b)). Anterior segment ocular coherence tomography revealed a full-thickness corneal incision, resulting in corneal microperforation (Figure 2). On slit lamp, anterior chamber was deep and quiet with negative Seidel sign. The patient maintained stable refraction (–1.0/–3.25/88°) and stable CDVA (9/10) at 6 months of follow-up postoperatively. Corneal topography showed Kmax of 57.7 D with the thinnest pachymetric point at 459 µm at 6 months postoperatively (Figure 1(c)).
Figure 2.
Anterior segment ocular coherence tomography showing full-thickness corneal incision with corneal microperforation after femtosecond laser-assisted ICRS implantation.
ICRS: intracorneal ring segment.
Discussion
ICRS are widely used in the management of stable keratoconus, in order to achieve visual improvement.3,4 In our case, the insertion of the ICRS was aborted due to corneal perforation. Interestingly, the patient’s UDVA and CDVA significantly improved 1 month after procedure, while keratometric and visual improvement was preserved at 6 months postoperatively. Although the refraction did not change significantly, Kmax decreased by 1.6 D at the first month, as a result of the full-thickness corneal incision and the corneal tunnel creation. It appears that the observed keratometric amelioration accounts for the patient’s visual improvement, although improvement of the keratometric readings is usually observed 6 months after ICRS implantation. Similarly, spherical equivalent normally improves no more than 1.5 D in the first semester after ICRS implantation.
To our knowledge, there has been no other report suggesting that full-thickness corneal incision on the astigmatic axis together with intracorneal tunnel could result in keratometric improvement in keratoconus. A recent promising technique, where a deep stromal puncturing was performed in order to reintegrate the entire flap into the residual stroma, highlighted the potential benefit of induced fibrogenesis as a treatment to stabilize the progression of post-LASIK keratectasia as an alternative to CXL.7
This highlighted phenomenon of surgically induced fibrogenesis may explain our favorable findings after abortion of the ICRS implantation. We believe that our unexpected result should be further investigated in the frame of an experimental study in order to validate its potential clinical implication in the management of corneal tunnel–induced fibrogenesis during femtosecond laser-assisted ICRS implantation in the management of keratoconus.
Footnotes
Conflict of interest statement: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Contributor Information
Iraklis Vastardis, St.-Johannes-Hospital, Dortmund, Germany.
Ahmed Thabit, Queen Victoria Hospital NHS Foundation Trust, East Grinstead, UK.
Mohamed Elalfy, Queen Victoria Hospital NHS Foundation Trust, East Grinstead, UK.
Samer Hamada, Queen Victoria Hospital NHS Foundation Trust, East Grinstead, UK.
Zisis Gatzioufas, Queen Victoria Hospital NHS Foundation Trust, East Grinstead, UK.
References
- 1. Colin J, Cochener B, Savary G, et al. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg 2000; 26: 1117–1122. [DOI] [PubMed] [Google Scholar]
- 2. Shabayek MH, Alió JL. Intrastromal corneal ring segment implantation by femtosecond laser for keratoconus correction. Ophthalmology 2007; 114: 1643–1652. [DOI] [PubMed] [Google Scholar]
- 3. Piñero DP, Alio JL. Intracorneal ring segments in ectatic corneal disease - a review. Clin Experiment Ophthalmol 2010; 38(2): 154–167. [DOI] [PubMed] [Google Scholar]
- 4. Vega-Estrada A, Alio JL, Brenner LF, et al. Outcome analysis of intracorneal ring segments for the treatment of keratoconus based on visual, refractive, and aberrometric impairment. Am J Ophthalmol 2013; 155(3): 575–584. [DOI] [PubMed] [Google Scholar]
- 5. Giacomin NT, Mello GR, Medeiros CS, et al. Intracorneal Ring Segments Implantation for Corneal Ectasia. J Refract Surg 2016; 32(12): 829–839. [DOI] [PubMed] [Google Scholar]
- 6. Coskunseven E, Kymionis GD, Tsiklis NS, et al. Complications of intrastromal corneal ring segment implantation using a femtosecond laser for channel creation: a survey of 850 eyes with keratoconus. Acta Ophthalmol 2011; 89(1): 54–57. [DOI] [PubMed] [Google Scholar]
- 7. Jarade E, Chelala E, Arej N, et al. Inducing fibrogenesis and new interfibrillary bonds in post-laser in situ keratomileusis keratectasia. J Cataract Refract Surg 2018; 44(9): 1062–1065. [DOI] [PubMed] [Google Scholar]