Abstract
Objective:
To assess the role of single photon emission computed tomography (SPECT/CT) in the evaluation of knee pain as well as comparing bone scintigraphy (BS), SPECT and SPECT/CT, and assessing the incremental value of SPECT/CT.
Methods:
BS, SPECT and SPECT/CT of patients with knee pain (39 patients, 65 knees, 105 lesions) were directly compared for lesion detection, localisation and characterisation using lesion-based, knee-based and patient-based analyses in this retrospective study.
Results:
Lesion detection: BS (91.4%), SPECT (100%) and SPECT/CT (100%). SPECT and SPECT/CT detected significantly more lesions than BS (p < 0.05). Lesion localisation: BS (38.5–41.7%), SPECT (74.4–83.3%) and SPECT/CT (100%). SPECT localised significantly more lesions than BS; SPECT/CT localised significantly more lesions than BS and SPECT (p < 0.01). Lesion characterisation: BS (23.0–52.1%), SPECT (30.8–56.2%) and SPECT/CT (92.3–96.9%). SPECT/CT characterised significantly more lesions than BS and SPECT (p < 0.01). Characterisation of non-arthropathy lesions: BS (6.25%), SPECT (12.5%) and SPECT/CT (93.75%). SPECT/CT characterised significantly more non-arthropathy lesions than BS and SPECT (p < 0.01). BS and SPECT detected none, while SPECT/CT detected 100% of the causative/contributing/associated conditions that co-existed with osteoarthritis. Therefore SPECT/CT detected not only just osteoarthritis but also the causative/contributing/associated conditions.
Conclusion:
SPECT/CT added significant incremental value to BS and SPECT irrespective of whether evaluation was lesion-based, knee-based or patient-based. SPECT/CT represents a viable alternative to MRI, and addition of SPECT/CT to BS and SPECT should be considered in the evaluation of knee pain.
Advances in knowledge:
Incremental value of bone SPECT/CT in knee pain.
Introduction
Knee pain is a common symptom and may cause significant morbidity and reduction in quality of life. A wide spectrum of pathology affecting bones, joints and soft tissues may cause knee pain. Imaging is a valuable adjunct to clinical assessment in evaluating the cause of knee pain—options include radiography, ultrasound, CT, MRI, 99mTc methylene diphosphonate (Tc-99m MDP) two-phase bone scintigraphy (BS), single photon emission computed tomography(SPECT) and SPECT/CT.
Plain X-ray is often the first line of line of investigation used in the assessment of knee pain as is the easiest and a cost-effective modality. However, detailed assessment of bone; ligaments, cartilage, and soft-tissue are limited on plain X-ray. CT scan is useful in the assessment of cortical bone abnormalities and fractures eloquently and provides excellent anatomical detail but may be optimal to assess soft tissue abnormalities. MRI offers excellent soft tissue contrast and is useful to assess the integrity of the cartilage, subarticular bone changes/abrasions, subchondral cystic changes, meniscal/ ligament abnormalities, and synovial inflammation/bursitis, without radiation burden. However, contrast agents used in CT and MRI has small risk of hypersensitivity reactions.
Selecting the most appropriate imaging modality is essential and should be directed by clinical assessment and knowledge of the mechanism of injury. Imaging findings, together with clinical findings, will in turn direct subsequent management. Timely and appropriate imaging strategies are therefore vital in evaluation of the knee.
BS has a high sensitivity, good contrast resolution and ability to demonstrate bone abnormalities early before morphological changes are evident.1–4 BS is also affordable and widely available. However, BS has limited specificity largely due to the non-specific mechanism of tracer uptake, which essentially reflects bone turnover of any aetiology. SPECT allows tomographic imaging and multiplanar reconstruction5–7 resulting in better contrast resolution, anatomical localisation and characterisation of lesions.2,8–12 This in turn translates to improvement in sensitivity, specificity and accuracy.3, 13 Addition of companion CT to SPECT in hybrid SPECT/CT imaging harnesses the excellent anatomical detail and spatial resolution provided by CT, which further improves the precision of lesion localisation and accuracy of lesion characterisation and hence improves specificity.2,14–17 Furthermore CT allows scatter and attenuation correction that improves spatial resolution.1,5–7 The marriage of functional and anatomical imaging techniques in SPECT/CT is complementary and synergistic, combining the contrast resolution of SPECT with the spatial resolution of CT, maximising the strengths and mitigating the limitations of each individual modality, resulting in improved sensitivity and specificity. This in turn translates to increased diagnostic confidence, improved diagnostic accuracy, more definitive diagnoses, and fewer equivocal and indeterminate findings. Ultimately, this speeds diagnosis and expedites treatment.
SPECT/CT had been reported to improve localisation and characterisation of bone metastases2,8–10 and bone infection18–22 resulting in increased diagnostic accuracy. SPECT was reported to be accurate in evaluating the knee23–26 and useful in directing arthroscopy.23, 27,28 However there are currently limited data on SPECT/CT in the evaluation of the knee. Data from small series showed SPECT/CT to be useful in characterising and diagnosing post-surgical knee pain.29, 30 Although SPECT/CT is generally recognised to be more accurate than BS and SPECT,9,10,31–33 there are as yet no available data quantifying the improvement of SPECT/CT over BS and SPECT, and whether the incremental value of SPECT/CT is significant in evaluation of the knee. Such data are important to justify the higher cost, greater radiation burden and longer scan time of using SPECT/CT. This study aims to address this issue of how much incremental value SPECT/CT adds by directly comparing BS, SPECT and SPECT/CT in the detection, localisation and characterisation of knee lesions.
methods and Materials
Patients
This retrospective study was part of SPECT/CT service evaluation audit and analysed 39 patients (14 males and 25 females; median age, 43 years; range, 22 to 84 years) who presented with knee pain and had undergone X-ray of knee joints followed by BS and SPECT/CT of the knee. All lesions around the knees detected on BS, SPECT and SPECT/CT were included in the analysis and 35/39 patients were followed up for at least 1 year. Four patients were lost to follow up.
Two-phase bone scintigraphy
BS of the knees was performed before SPECT/CT. After intravenous administration of 600 MBq of Tc-99m MDP, early phase blood pool imaging was performed within 5 min and delayed phase bone imaging was performed 3 to 4 h post injection. Planar images of the knees were acquired using a dual-head gamma camera with low energy high resolution collimators. Anterior, posterior and lateral projections of the knees were acquired for early and delayed phase imaging. Delayed whole body images were acquired as well.
SPECT and SPECT/CT
SPECT/CT of the knees was performed after completion of BS. SPECT/CT images were acquired using a dual-head gamma camera with 16-slice CT system (Precedence 16, Philips, Milpitas, CA) as described previously.34 Low-dose CT was acquired first (120 kV, 100 mA per slice, pitch of 1.188 with rotation time of 0.75 s, 16 × 0.75 mm collimation, images reconstructed to 0.683 mm transverse pixel size and 1.5 mm slice thickness). After CT acquisition, SPECT was performed without changing the patient’s position using a dual-head gamma camera with low energy high resolution collimators in 128 projections of 20 s each over 360°. Reconstruction of SPECT data were performed with Orderly Subsets Expectation Maximum (5 iterations over 8 subsets), incorporating depth-dependent resolution compensation (Astonish, Philips Medical Systems) using the manufacturer’s software (AutoSPECT +v3.5 and Syntegra v2.2).34
Image and statistical analysis
Two nuclear medicine physicians and a musculoskeletal radiologist reviewed the scans. The nuclear medicine physicians reported the Tc-99m MDP bone scans (planar and SPECT) independently. The musculoskeletal radiologist reviewed the CT study. The final diagnosis was made based on corroborating BS, SPECT and CT findings. The number of knee lesions that were detected, precisely localised and accurately characterised was determined. A lesion was considered detected if it could be visualised on the imaging modality. A lesion was considered precisely localised if the exact site of lesion could be determined. A lesion was considered accurately characterised if a single diagnosis could be made without other differentials. Bone tumours or tumour-like lesions were considered accurately characterised if they could be determined as benign or malignant.
Imaging findings of BS, SPECT and SPECT/CT were analyzed and direct comparison of BS, SPECT and SPECT/CT was made based on detection, localisation and characterisation of lesions. Lesion-based, knee-based and patient-based analyses were undertaken and incremental values were calculated. Statistical significance of the incremental values was determined using McNemar test with p value of less than 0.05 (p < 0.05) considered as statistically significant.
Results
There were 105 lesions detected by BS, SPECT and SPECT/CT in 65 knees from 39 patients (Table 1). The majority of knee lesions involved bones and joints (n = 101) while the remainder involved soft tissues (n = 4). The single most common knee lesion by far was osteoarthritis (45/105 lesions, 42.9%).
Table 1.
Spectrum of knee lesions detected on BS, SPECT and SPECT/CT
| Type of lesion | Number |
| Bones and joints | |
| Osteoarthritis | 45 |
| Psoriatic arthropathy | 4 |
| Synovial inflammation | 1 |
| Osteonecrosis | 8 |
| Osteochondral abnormality | 8 |
| Loose body | 1 |
| Meniscus injury | 1 |
| Osteoid osteoma | 2 |
| Benign bone lesion | 4 |
| Malignant bone tumour | 4 |
| Patella maltracking/malalignment | 9 |
| Bipartite patella with pseudoarthrosis | 1 |
| Loosening of knee prosthesis | 2 |
| Bony remodelling post surgery/trauma | 4 |
| Fracture | 2 |
| Shin splint | 2 |
| Bone infection | 3 |
| Soft tissues | |
| Soft tissue infection with sinus | 1 |
| Prepatellar bursitis | 2 |
| Quadriceps tendinosis | 1 |
| Total | 105 |
Diagnosis of knee lesions
The knee lesions in this study encompassed a wide spectrum of aetiologies including degenerative, traumatic, infective, neoplastic, congenital and iatrogenic causes. Diagnoses of knee lesions were confirmed by imaging (BS, SPECT, SPECT/CT or MRI), surgery, biopsy, follow-up (clinical or imaging) or any combination of these.
Osteoid osteoma, osteonecrosis, osteochondral abnormality, loose bodies, patella maltracking/malalignment, bipartite patella with pseudoarthrosis, and fractures were diagnostic on the CT component of SPECT/CT with corresponding increase in osteoblastic activity. The fractures involved the proximal fibula in one patient and lateral tibial condyle in another. Osteoarthritis, synovial inflammation, shin splint, meniscus injury and quadriceps tendinosis were diagnostic on BS and SPECT showing typical patterns of tracer uptake. Lesions due to bone remodelling were secondary to prior surgical procedures and trauma namely anterior cruciate ligament reconstruction, lateral collateral ligament reconstruction and healing fracture, and these were diagnosed on SPECT/CT with increased osteoblastic activity at the site of surgery or trauma. Soft tissue lesions namely prepatellar bursitis and soft tissue infection in the anterior knee were diagnosed on SPECT/CT with abnormal extra osseous tracer uptake in the affected soft tissues. CT showed a draining sinus in a case of soft tissue infection. Benign bone lesions were diagnosed on CT and follow-up. On CT, benign bone lesions were well-defined with narrow zone of transition and were stable on follow-up. Malignant bone lesions were osteosarcoma of the proximal tibia and lymphomatous marrow involvement, both of which were diagnosed on histology. Osteosarcoma showed increased vascularity and intense osteoblastic activity on BS, and ill-defined appearance with a wide zone of transition and cortical breach on CT. Lymphomatous marrow lesions were ill-defined with a wide zone of transition on CT and showed increased metabolic activity on staging 18F-FDG PET/CT with complete metabolic resolution post-chemotherapy. All the lesions due to bone infection had a background of prior surgical intervention namely total knee replacement and below knee amputation. One lesion was diagnosed with Indium-111 white blood cell scan while the others were diagnosed based on clinical, biochemical, microbiological and imaging findings and follow-up. Clinical information that corroborated with imaging findings were helpful in confirming diagnosis namely history of psoriasis, renal transplantation, surgical intervention or trauma. A patient with prior renal transplantation had osteonecrosis likely secondary to long-term treatment with steroids. In addition osteoid osteoma, patella maltracking/malalignment and infection had typical signs or symptoms.
Lesion-based analysis (SPECT vs SPECT/CT for 105 lesions)
Of the 105 knee lesions, BS detected 96/105 (91.4%), SPECT 105/105 (100%) and SPECT/CT 105/105 lesions (100%). SPECT and SPECT/CT detected 9 more lesions than BS (8.6%, p < 0.05). The results are summarised in Table 2.
Table 2.
Comparing BS, SPECT and SPECT/CT in the detection of 105 knee lesions
| BS vs SPECT vs SPECT/CT (n = 105) | ||
| Modality | Number of lesions (%) | Difference (BS vs SPECT or SPECT/CT) |
| Detection | ||
| BS | 96 (91.4%) | 9 (8.6%) p < 0.05 |
| SPECT | 105 (100%) | |
| SPECT/CT | 105 (100%) | |
SPECT and SPECT/CT detected all 105 lesions. For lesion localisation, SPECT accurately localised 89/105 lesions (84.8%) and SPECT/CT 105/105 lesions (100%). For lesion characterisation, SPECT characterised 56/105 lesions (53.3%) and SPECT/CT 102/105 lesions (97.1%). On comparing, SPECT/CT localised 16 more lesions (15.2%, p < 0.001) and characterised 46 more lesions (43.8%, p < 0.001) than SPECT. The results are summarised in Table 3 and Figure 1.
Table 3.
Comparing SPECT and SPECT/CT in lesion-based analysis of 105 knee lesions
| SPECT vs SPECT/CT (n = 105) | ||
| Modality | Number of lesions (%) | Difference (SPECT vs SPECT/CT) |
| Localisation | ||
| SPECT | 89 (84.8%) | 16 (15.2%) p < 0.001 |
| SPECT/CT | 105 (100%) | |
| Characterization | ||
| SPECT | 56 (53.3%) | 46 (43.8%) p < 0.001 |
| SPECT/CT | 102 (97.1%) | |
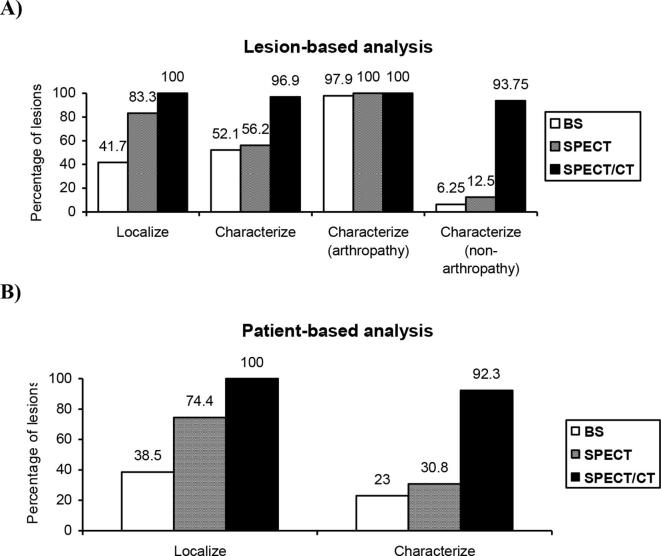
Figure 1.
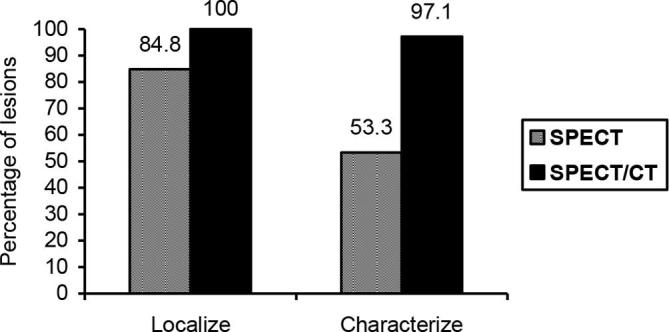
Graph illustrating the incremental value (SPECT vs SPECT/CT) in lesion-based analysis of 105 knee lesions.
Lesion-based analysis (BS vs SPECT vs SPECT/CT for 96 lesions)
All 96 knee lesions detected by BS were also detected by SPECT and SPECT/CT, and were therefore used for comparison of these three imaging modalities. For lesion localisation, BS accurately localised 40/96 (41.7%), SPECT 80/96 (83.3%) and SPECT/CT 96/96 (100%) lesions. On comparing, SPECT localised 40 more lesions (41.7%, p < 0.001) than BS, SPECT/CT 56 more lesions (58.3%, p < 0.001) than BS and 16 more lesions (16.7%, p < 0.001) than SPECT. For lesion characterisation, BS characterised 50/96 (52.1%), SPECT 54/96 (56.2%) and SPECT/CT 93/96 (96.9%) lesions. On comparing, SPECT characterised 4 more lesions (4.2%, p > 0.1) than BS, SPECT/CT 43 more lesions (44.8%, p < 0.001) than BS and 39 more lesions (40.6%, p < 0.001) than SPECT. The results are summarised in Table 4 and Figure 2a.
Table 4.
Comparing BS, SPECT and SPECT/CT in lesion-based analysis of 96 knee lesions
| BS vs SPECT vs SPECT/CT (n = 96) | ||||
| Modality | Number of lesions (%) | Difference (BS vs SPECT) | Difference (BS vs SPECT/CT) | Difference (SPECT vs SPECT/CT) |
| Localisation | ||||
| BS | 40 (41.7%) | } 40 (41.7%) } P < 0.001 | } 56 (58.3%) P < 0.001 } | |
| SPECT | 80 (83.3%) | } 16 (16.7%) } P < 0.001 | ||
| SPECT/CT | 96 (100%) | |||
| Characterisation | ||||
| BS | 50 (52.1%) | } 4 (4.2%) } P > 0.1 | } 43 (44.8%) P < 0.001 } | |
| SPECT | 54 (56.2%) | } 39 (40.6%) } P < 0.001 | ||
| SPECT/CT | 93 (96.9%) | |||
| BS vs SPECT vs SPECT/CT (excluding arthropathy lesions n = 48) | ||||
| Modality | Number of lesions detected (%) | Difference (BS vs SPECT) | Difference (BS vs SPECT/CT) | Difference (SPECT vs SPECT/CT) |
| Characterisation | ||||
| BS | 3 (6.25%) | } 3 (6.25%) } P > 0.2 | } 42 (87.5%) P < 0.001 } | |
| SPECT | 6 (12.5%) | } 39 (81.25%) } P < 0.001 | ||
| SPECT/CT | 45 (93.75%) | |||
Figure 2.
Graphs illustrating the incremental values (BS vs SPECT vs SPECT/CT) in lesion-based analysis of 96 knee lesions (A), patient-based analysis of knee lesions in 39 patients (B).
Among the 96 lesions, 48 lesions were due to arthropathy namely osteoarthritis (n = 44) and psoriatic arthropathy (n = 4). BS characterised 47/48 (97.9%), SPECT 48/48 (100%) and SPECT/CT 48/48 (100%) arthropathy lesions. In a subset analysis of the remaining 48 non-arthropathy lesions, BS characterised 3/48 (6.25%), SPECT 6/48 (12.5%) and SPECT/CT 45/48 (93.75%) lesions. On comparing, SPECT characterised 3 more lesions (6.25%, p > 0.2) than BS, SPECT/CT 42 more lesions (87.5%, p < 0.001) than BS and 39 more lesions (81.25%, p < 0.001) than SPECT for non-arthropathy lesions. The findings showed that BS and SPECT could characterise arthropathy lesions very well but were poor at characterising non-arthropathy lesions. In contrast SPECT/CT could characterise both arthropathy and non-arthropathy lesions very well. The results are summarised in Table 4 and Figure 2a.
Subset analysis was performed for 9 knees with osteoarthritis that had co-existing conditions causing, contributing to or associated with osteoarthritis namely patellar maltracking/malalignment (n = 6), osteochondral lesion (n = 2) and loose bodies (n = 1). Both BS and SPECT detected none of the 9 causative/contributing/associated lesions although they could detect all 9 osteoarthritis lesions. In contrast SPECT/CT detected all 9 causative/contributing/associated lesions in addition to all 9 osteoarthritis lesions. Therefore SPECT/CT detected not just osteoarthritis but also the cause of it, and the lesions contributing to or associated with it.
Patient-based analysis (BS vs SPECT vs SPECT/CT for 39 patients)
There were 39 patients with knee pain. Bilateral knee lesions were detected in 26 patients (66.7%) and unilateral knee lesions in 13 patients (33.3%). For lesion localisation, BS accurately localised all knee lesions for 15/39 patients (38.5%), SPECT for 29/39 patients (74.4%) and SPECT/CT for 39/39 patients (100%). On comparing, SPECT localised all knee lesions in 14 more patients (35.9%, p < 0.001) than BS, SPECT/CT in 24 more patients (61.5%, p < 0.001) than BS, and SPECT/CT in 10 more patients (25.6%, p < 0.002) than SPECT. The results are summarised in Table 5 and Figure 2b.
Table 5.
Comparing BS, SPECT and SPECT/CT in patient-based analysis of knee lesions in 39 patients
| BS vs SPECT vs SPECT/CT (n = 39) | ||||
| Modality | Number of lesions (%) | Difference (BS vs SPECT) | Difference (BS vs SPECT/CT) | Difference (SPECT vs SPECT/CT) |
| Localisation | ||||
| BS | 15 (38.5%) | } 14 (35.9%) } p < 0.001 |
} 24 (61.5%) p < 0.001 } |
|
| SPECT | 29 (74.4%) | } 10 (25.6%), } p < 0.002 |
||
| SPECT/CT | 39 (100%) | |||
| Characterisation | ||||
| BS | 9 (23%) | } 3 (7.7%) } p > 0.2 |
} 27 (69.2%) p < 0.001 } |
|
| SPECT | 12 (30.8%) | } 24 (61.5%) } p < 0.001 |
||
| SPECT/CT | 36 (92.3%) | |||
For lesion characterisation, BS characterised all knee lesions for 9/39 patients (23.0%), SPECT for 12/39 patients (30.8%) and SPECT/CT for 36/39 patients (92.3%). On comparing, SPECT characterised all knee lesions in 3 more patients (7.7%, p > 0.2) than BS, SPECT/CT in 27 more patients (69.2%, p < 0.001) than BS, and SPECT/CT in 24 more patients (61.5%, p < 0.001) than SPECT. The results are summarised in Table 5 and Figure 2b.
Discussion
Two-phase bone scintigraphy has high sensitivity but limited specificity.1 When evaluating the knee, specificity is important as there are many causes of knee pain with different pathology having different prognosis and management strategy. Furthermore, multiple pathologies can co-exist in a single knee and each may contribute to symptoms to varying degrees. Therefore management of knee pain requires a more individualised approach catering to the knee pathology and patient’s lifestyle. To achieve this, accurate diagnosis of the cause of knee pain is vital.
Although BS was sensitive and could detect 91.4% of knee lesions in this study, addition of SPECT or SPECT/CT further improved the already good sensitivity with a significant incremental value of 8.6%. However the greatest benefit of SPECT/CT was seen in the significant incremental value that it added to BS for both localisation and characterisation of lesions (44.8 to 69.2%) regardless of whether analysis was lesion-based, knee-based or patient-based. SPECT/CT also added significant incremental value to SPECT for localisation and characterisation of lesions (15.2 to 61.5%). SPECT added significant incremental value to BS for localisation of lesions (35.4 to 41.7%) but not for characterisation of lesions (3.1 to 7.7%). BS and SPECT characterised arthropathy lesions very well (97.9 and 100% respectively) but were dismal at characterising non-arthropathy lesions (6.25 and 12.5% respectively) whereas SPECT/CT was excellent at characterising both arthropathy and non-arthropathy lesions (100 and 93.75% respectively).
There was a progressive stepwise improvement from BS to SPECT to SPECT/CT for localisation and characterisation of lesions. Every stepwise improvement and incremental value was significant except for improvement of lesion characterisation from BS to SPECT which was small and not significant since both modalities were similarly poor. This pattern of progressive stepwise improvement and incremental value was similar for lesion-based, knee-based and patient-based analyses and was therefore reproducible irrespective of whether evaluation was made from the perspective of the lesion, knee or patient.
The significant incremental value that SPECT/CT adds for characterising lesions is largely due to the companion CT (Figures 3–5). CT provides excellent anatomical information and can accurately diagnose morphological abnormalities namely patellar malalignment, bipartite patella with pseudoarthrosis, osteochondral lesions and loose bodies, which could not be confidently characterised on BS or SPECT. Osteoid osteoma, osteonecrosis and fracture have typical and diagnostic CT appearances. Arguably BS and SPECT can possibly characterise osteoid osteoma, osteonecrosis and fracture as well especially with corroborating clinical history but the level of confidence is lower and definitive diagnosis is limited on BS. CT is able to more accurately distinguish between benign and malignant bone lesions using features such a lesion margin and the definition of zone of transition between normal and abnormal trabecular patterns. Without CT information, BS and SPECT will be less efficient in characterising and differentiating benign from malignant bone lesions. When evaluating soft tissue lesions, SPECT/CT precisely localises tracer uptake to soft tissues resulting in accurate characterisation. Without CT, BS and SPECT are less able to determine whether the tracer uptake is from soft tissues or bones due to close proximity and hence are unable to characterise accurately. Finally, CT can demonstrate anatomical abnormalities that cause or contributes to osteoarthritis including patellar maltracking/malalignment, osteochondral lesion and loose bodies which BS and SPECT cannot. Thus SPECT/CT not only detects osteoarthritis but also demonstrates the cause of it, which is valuable in directing treatment to the cause rather than simply managing osteoarthritis.-
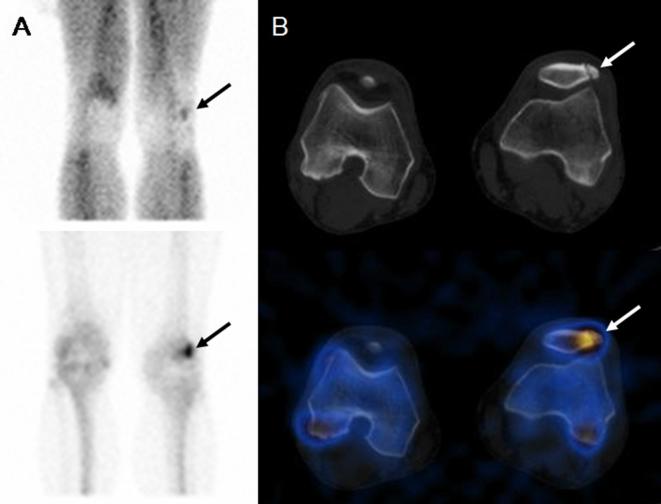
Figure 3.
Bipartite patella. A 38-year-old male with left knee pain. (A) Two-phase bone scintigraphy shows a non-specific hypervascular osteoblastic focus in the left patella (arrows). (B) SPECT/CT localises the osteoblastic focus to the synchondrosis of a left bipartite patella (arrows). [Reproduced with kind permission from Lu SJ et al, Value of SPECT/CT in the evaluation of knee pain. Clin Nucl Med 2013; 38(6): e258–60.35]
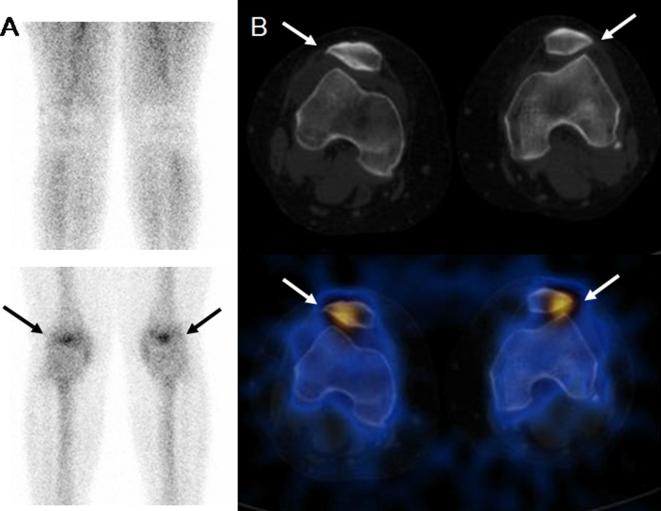
Figure 4.
Patellar maltracking. A 33-year-old female with bilateral knee pain. (A) Two-phase bone scintigraphy shows non-specific focal increased osteoblastic activity in both patellae arrows). (B) SPECT/CT shows lateral deviation of both patellae and shallow trochlear grooves with increased osteoblastic activity at the lateral patellofemoral articulations (arrows). [Reproduced with kind permission from Lu SJ et al, Value of SPECT/CT in the evaluation of knee pain. Clin Nucl Med 2013; 38(6): e258–60.35]
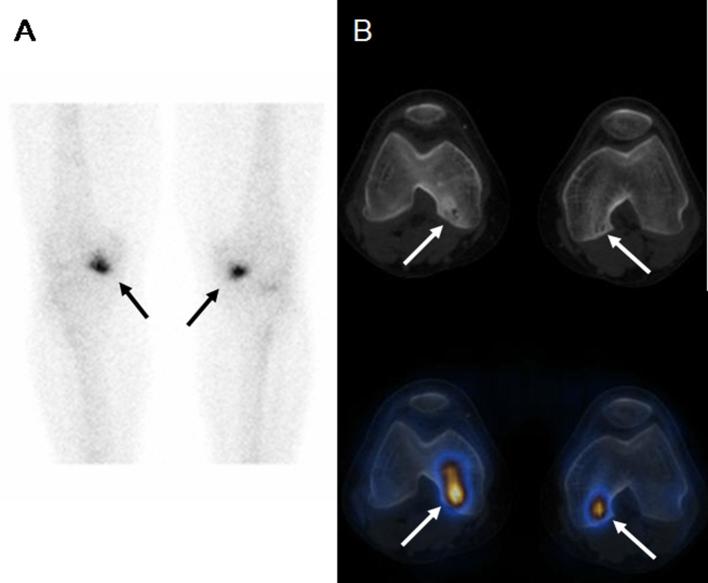
Figure 5.
Avascular necrosis. A 65-year-old male with a history of renal transplantation and long-term steroids treatment presented with bilateral knee pain. (A) Planar bone scintigraphy shows non-specific focal increased osteoblastic activity at the medial aspects of both knee joints (arrows). (B) SPECT/CT localises the osteoblastic foci to the sclerotic marrow lesions at the posterior aspects of both medial femoral condyles, which are more prominent on the right side (arrows).[ Reproduced with kind permission from Lu SJ et al; Value of SPECT/CT in evaluation of knee pain. Clin Nucl Med 2013; 38 (6): e258–6.035]
Initial clinical evaluation of the knee and knowledge of the mechanism of injury are important for determining the likely causes of knee pain and directing the most appropriate imaging test to perform. MRI is often the favoured imaging modality to evaluate the knee because it is excellent at assessing soft tissues and bone marrow, providing superior anatomical details and soft tissue characterisation. MRI also does not have ionising radiation. However MRI is limited in assessing bone cortical abnormalities and post-surgical knees with indwelling orthopedic hardware causing significant artefacts. There are also known contraindications to MRI namely claustrophobia, severe obesity, presence of embedded metallic foreign bodies, pacemakers and indwelling non-MRI compatible clips/implants. In instances where MRI is limited, contraindicated or not available, SPECT/CT represents a viable alternative option to evaluate the knee. SPECT/CT also represents a useful problem-solving tool when MRI findings are equivocal or indeterminate.
SPECT had been reported to be accurate in evaluating the knee23–26 and useful in directing arthroscopy.23, 27,28 With the significant incremental value that SPECT/CT adds to SPECT as demonstrated in this study, SPECT/CT can perform better than SPECT and possibly as well as MRI for evaluation of the knee. Thus far limited data from small series on SPECT/CT evaluation of the knee found it useful for assessing post-surgical knee pain with resultant change of management.29, 30 Prospective studies comparing SPECT/CT with MRI in assessing the knee and defining the roles that each imaging modality plays will be welcomed. Nevertheless it is important to view different imaging modalities like SPECT/CT and MRI as complementary rather than competitive. The importance of careful clinical evaluation of each patient before deciding on the most appropriate imaging test to perform cannot be overemphasised.
If BS is the most appropriate imaging modality to investigate the knee, addition of SPECT/CT may be considered regardless of whether BS detects any abnormality. This is because SPECT/CT detects, localises and characterises significantly more knee lesions than BS with significant incremental value, thereby improving both sensitivity and specificity. This adds diagnostic confidence and improves diagnostic accuracy. Ultimately the positive impact of SPECT/CT reduces delay in diagnosis and expedites treatment thereby benefiting patients. The significant incremental value SPECT/CT adds to both BS and SPECT can play an important part in justifying the higher cost, greater radiation burden and longer scan time of using SPECT/CT for evaluation of the knee. Specific studies assessing the cost-effectiveness of SPECT/CT may be needed. However purely from an imaging perspective, there is justification in adding SPECT/CT to BS for evaluation of the knee based on the significant incremental value SPECT/CT adds.
This study was not without limitations. Since the primary aim of this study was to determine the incremental value that SPECT/CT could add to BS in evaluating the knee, the abnormalities studied and analysed were those detected by BS, SPECT and SPECT/CT. Another limitation was the presence of more than one lesion per knee in a majority of the knees (58.5%) and the difficulty in determining which lesions were causing symptoms. Ideally only lesions causing symptoms were significant and evaluated while incidental asymptomatic lesions that did not require treatment were ignored. However arbitrarily deciding which lesions were likely to cause symptoms would be ambiguous and subjective. To overcome this, all lesions around the knees detected on BS, SPECT and SPECT/CT were included for analysis since the objective was to determine detection, localisation and characterisation of knee lesions in general. Lesion-based, knee-based and patient-based analyses were undertaken to paint a more holistic and representative picture overall.
Conclusion
SPECT/CT adds significant incremental value to BS and SPECT for evaluation of the knee. In essence, SPECT improves detection and localisation of lesions while SPECT/CT further improves dramatically localisation and characterisation of lesions. Addition of SPECT/CT to BS or SPECT results in greater diagnostic confidence, improved diagnostic accuracy, more definitive diagnoses and less inconclusive interpretations. Purely from an imaging perspective, there is justification in adding SPECT/CT to BS for evaluation of the knee. SPECT/CT represents a viable alternative when MRI is not feasible and a useful problem-solving tool when MRI findings are inconclusive, and may yet play an increasing role in evaluation of the knee.
Contributor Information
Suat-Jin Lu, Email: suat_jin_lu@yahoo.com.
Fahim Ul Hassan, Email: drfahim.hassan@gmail.com.
Sanjay Vijayanathan, Email: sanjay.vijayanathan@gstt.nhs.uk.
Gopinath Gnanasegaran, Email: gopinath.gnanasegaran@nhs.net.
REFERENCES
- 1.Van der Wall H, Lee A, Magee M, Frater C, Wijesinghe H, Kannangara S, et al. Radionuclide bone scintigraphy in sports injuries. Semin Nucl Med 2010; 40: 16–30. doi: 10.1053/j.semnuclmed.2009.08.006 [DOI] [PubMed] [Google Scholar]
- 2.Utsunomiya D, Shiraishi S, Imuta M, Tomiguchi S, Kawanaka K, Morishita S, et al. Added value of SPECT/CT fusion in assessing suspected bone metastasis: comparison with scintigraphy alone and nonfused scintigraphy and CT. Radiology 2006; 238: 264–71. doi: 10.1148/radiol.2373041358 [DOI] [PubMed] [Google Scholar]
- 3.Schillaci O, Danieli R, Manni C, Simonetti G. Is SPECT/CT with a hybrid camera useful to improve scintigraphic imaging interpretation? Nucl Med Commun 2004; 25: 705–10. doi: 10.1097/01.mnm.0000130240.83949.54 [DOI] [PubMed] [Google Scholar]
- 4.Hasegawa BH, Wong KH, Iwata K, Barber WC, Hwang AB, Sakdinawat AE, et al. Dual-modality imaging of cancer with SPECT/CT. Technol Cancer Res Treat 2002; 1: 449–58. doi: 10.1177/153303460200100605 [DOI] [PubMed] [Google Scholar]
- 5.Zaidi H, Hasegawa B. Determination of the attenuation map in emission tomography. J Nucl Med 2003; 44: 291–315. [PubMed] [Google Scholar]
- 6.Townsend DW, Beyer T, Blodgett TM. PET/CT scanners: a hardware approach to image fusion. Semin Nucl Med 2003; 33: 193–204. doi: 10.1053/snuc.2003.127314 [DOI] [PubMed] [Google Scholar]
- 7.Seo Y, Wong KH, Sun M, Franc BL, Hawkins RA, Hasegawa BH, et al. Correction of photon attenuation and collimator response for a body-contouring SPECT/CT imaging system. J Nucl Med 2005; 46: 868–77. [PubMed] [Google Scholar]
- 8.Even-Sapir E, Keidar Z, Bar-Shalom R. Hybrid imaging (SPECT/CT and PET/CT)-improving the diagnostic accuracy of functional/metabolic and anatomic imaging. Semin Nucl Med 2009; 39: 264–75. doi: 10.1053/j.semnuclmed.2009.03.004 [DOI] [PubMed] [Google Scholar]
- 9.Horger M, Eschmann SM, Pfannenberg C, Vonthein R, Besenfelder H, Claussen CD, et al. Evaluation of combined transmission and emission tomography for classification of skeletal lesions. AJR Am J Roentgenol 2004; 183: 655–61. doi: 10.2214/ajr.183.3.1830655 [DOI] [PubMed] [Google Scholar]
- 10.Römer W, Nömayr A, Uder M, Bautz W, Kuwert T. SPECT-guided CT for evaluating foci of increased bone metabolism classified as indeterminate on SPECT in cancer patients. J Nucl Med 2006; 47: 1102–6. [PubMed] [Google Scholar]
- 11.Kobayashi K, Okuyama C, Kubota T, Nakai T, Ushijima Y, Nishimura T, et al. Do short-time SPECT images of bone scintigraphy improve the diagnostic value in the evaluation of solitary lesions in the thoracic spine in patients with extraskeletal malignancies? Ann Nucl Med 2005; 19: 557–66. doi: 10.1007/BF02985048 [DOI] [PubMed] [Google Scholar]
- 12.Savelli G, Maffioli L, Maccauro M, De Deckere E, Bombardieri E. Bone scintigraphy and the added value of SPECT (single photon emission tomography) in detecting skeletal lesions. Q J Nucl Med 2001; 45: 27–37. [PubMed] [Google Scholar]
- 13.Even-Sapir E. Imaging of malignant bone involvement by morphologic, scintigraphic, and hybrid modalities. J Nucl Med 2005; 46: 1356–67. [PubMed] [Google Scholar]
- 14.Horger M, Bares R. The role of single-photon emission computed tomography/computed tomography in benign and malignant bone disease. Semin Nucl Med 2006; 36: 286–94. doi: 10.1053/j.semnuclmed.2006.05.001 [DOI] [PubMed] [Google Scholar]
- 15.Han LJ, Au-Yong TK, Tong WC, Chu KS, Szeto LT, Wong CP, et al. Comparison of bone single-photon emission tomography and planar imaging in the detection of vertebral metastases in patients with back pain. Eur J Nucl Med 1998; 25: 635–8. doi: 10.1007/s002590050266 [DOI] [PubMed] [Google Scholar]
- 16.Kosuda S, Kaji T, Yokoyama H, Yokokawa T, Katayama M, Iriye T, et al. Does bone SPECT actually have lower sensitivity for detecting vertebral metastasis than MRI? J Nucl Med 1996; 37: 975–8. [PubMed] [Google Scholar]
- 17.Even-Sapir E, Martin RH, Barnes DC, Pringle CR, Iles SE, Mitchell MJ, et al. Role of SPECT in differentiating malignant from benign lesions in the lower thoracic and lumbar vertebrae. Radiology 1993; 187: 193–8. doi: 10.1148/radiology.187.1.8451412 [DOI] [PubMed] [Google Scholar]
- 18.Horger M, Eschmann SM, Pfannenberg C, Storek D, Dammann F, Vonthein R, et al. The value of SPET/CT in chronic osteomyelitis. Eur J Nucl Med Mol Imaging 2003; 30: 1665–73. doi: 10.1007/s00259-003-1321-z [DOI] [PubMed] [Google Scholar]
- 19.Van Acker F, Nuyts J, Maes A, Vanquickenborne B, Stuyck J, Bellemans J, et al. FDG-PET, 99mtc-HMPAO white blood cell SPET and bone scintigraphy in the evaluation of painful total knee arthroplasties. Eur J Nucl Med 2001; 28: 1496–504. doi: 10.1007/s002590100603 [DOI] [PubMed] [Google Scholar]
- 20.Rini JN, Bhargava KK, Tronco GG, Singer C, Caprioli R, Marwin SE, et al. PET with FDG-labeled leukocytes versus scintigraphy with 111In-oxine-labeled leukocytes for detection of infection. Radiology 2006; 238: 978–87. doi: 10.1148/radiol.2382041993 [DOI] [PubMed] [Google Scholar]
- 21.Palestro CJ, Love C, Tronco GG, Tomas MB, Rini JN. Combined labeled leukocyte and technetium 99m sulfur colloid bone marrow imaging for diagnosing musculoskeletal infection. Radiographics 2006; 26: 859–70. doi: 10.1148/rg.263055139 [DOI] [PubMed] [Google Scholar]
- 22.Horger M, Eschmann SM, Pfannenberg C, Storek D, Vonthein R, Claussen CD, et al. Added value of SPECT/CT in patients suspected of having bone infection: preliminary results. Arch Orthop Trauma Surg 2007; 127: 211–21. doi: 10.1007/s00402-006-0259-6 [DOI] [PubMed] [Google Scholar]
- 23.Ryan PJ, Chauduri R, Bingham J, Fogelman I. A comparison of MRI and bone SPET in the diagnosis of knee pathology. Nucl Med Commun 1996; 17: 125–31. doi: 10.1097/00006231-199602000-00006 [DOI] [PubMed] [Google Scholar]
- 24.Cook GJ, Ryan PJ, Clarke SE, Fogelman I. SPECT bone scintigraphy of anterior cruciate ligament injury. J Nucl Med 1996; 37: 1353–6. [PubMed] [Google Scholar]
- 25.Ryan PJ, Reddy K, Fleetcroft J. A prospective comparison of clinical examination, MRI, bone SPECT, and arthroscopy to detect meniscal tears. Clin Nucl Med 1998; 23: 803–6. doi: 10.1097/00003072-199812000-00002 [DOI] [PubMed] [Google Scholar]
- 26.Collier BD, Johnson RP, Carrera GF, Isitman AT, Veluvolu P, Knobel J, et al. Chronic knee pain assessed by SPECT: comparison with other modalities. Radiology 1985; 157: 795–802. doi: 10.1148/radiology.157.3.3877315 [DOI] [PubMed] [Google Scholar]
- 27.So Y, Chung JK, Seong SC, Sohn YJ, Kang HS, Lee DS, et al. Usefulness of 99Tcm-MDP knee SPET for pre-arthroscopic evaluation of patients with internal derangements of the knee. Nucl Med Commun 2000; 21: 103–9. doi: 10.1097/00006231-200001000-00017 [DOI] [PubMed] [Google Scholar]
- 28.Murray IP, Dixon J, Kohan L. SPECT for acute knee pain. Clin Nucl Med 1990; 15: 828–40. doi: 10.1097/00003072-199011000-00015 [DOI] [PubMed] [Google Scholar]
- 29.Hirschmann MT, Konala P, Iranpour F, Kerner A, Rasch H, Friederich NF, et al. Clinical value of SPECT/CT for evaluation of patients with painful knees after total knee arthroplasty--a new dimension of diagnostics? BMC Musculoskelet Disord 2011; 12: 36. doi: 10.1186/1471-2474-12-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hirschmann MT, Adler T, Rasch H, Hügli RW, Friederich NF, Arnold MP, et al. Painful knee joint after ACL reconstruction using biodegradable interference screws- SPECT/CT a valuable diagnostic tool? A case report. Sports Med Arthrosc Rehabil Ther Technol 2010; 2: 24. doi: 10.1186/1758-2555-2-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gnanasegaran G, Barwick T, Adamson K, Mohan H, Sharp D, Fogelman I, et al. Multislice SPECT/CT in benign and malignant bone disease: when the ordinary turns into the extraordinary. Semin Nucl Med 2009; 39: 431–42. doi: 10.1053/j.semnuclmed.2009.07.005 [DOI] [PubMed] [Google Scholar]
- 32.Strobel K, Burger C, Seifert B, Husarik DB, Soyka JD, Hany TF, et al. Characterization of focal bone lesions in the axial skeleton: performance of planar bone scintigraphy compared with SPECT and SPECT fused with CT. AJR Am J Roentgenol 2007; 188: W467–W474. doi: 10.2214/AJR.06.1215 [DOI] [PubMed] [Google Scholar]
- 33.Even-Sapir E, Flusser G, Lerman H, Lievshitz G, Metser U. SPECT/multislice low-dose CT: a clinically relevant constituent in the imaging algorithm of nononcologic patients referred for bone scintigraphy. J Nucl Med 2007; 48: 319–24. [PubMed] [Google Scholar]
- 34.Mohan HK, Gnanasegaran G, Vijayanathan S, Fogelman I. SPECT/CT in imaging foot and ankle pathology-the demise of other coregistration techniques. Semin Nucl Med 2010; 40: 41–51. doi: 10.1053/j.semnuclmed.2009.08.004 [DOI] [PubMed] [Google Scholar]
- 35.Lu SJ, Ul Hassan F, Vijayanathan S, Fogelman I, Gnanasegaran G. Value of SPECT/CT in the evaluation of knee pain. Clin Nucl Med 2013; 38: e258–60. [DOI] [PubMed] [Google Scholar]