Abstract
The BIRC5 gene encodes a survivin protein belonging to class III of inhibitors of apoptosis, IAP. This protein serves a dual role. First, it regulates cell death, and second, it is an important regulator of mitosis progression, although its physiological regulatory function has not been fully understood. Many studies have shown and confirmed that survivin is practically absent in mature tissues in nature, while its overexpression has been reported in many cancerous tissues. There is little information about the significance of BIRC5 expression in normal adult human stem cells. This paper presents the study and analysis of survivin expression at the transcription level using qPCR method, in hematopoietic stem cells from peripheral blood mobilized with a granulocyte growth factor, adherent cells derived from the umbilical cord, and normal bone marrow stem cells. The expression of this gene was also examined in the blood of normal healthy individuals. The results of the analysis have shown that the more mature the cells are, the lower the expression of the BIRC5 gene is. The lowest expression has been found in peripheral blood cells, while the highest in normal bone marrow cells. The more the CD34+ and CD105 cells in the tested material are, the higher the BIRC5 expression is. Stem cells from cell culture show higher BIRC5 expression. The study confirms the involvement of BIRC5 from the IAP family in many physiological processes apart from apoptosis inhibition. The possible effect of BIRC5 on cell proliferation; involvement in cell cycle, cell differentiation, survival, and maintenance of stem cells; and the possible effect of IAP on the antineoplastic properties of mesenchymal stem cells have been demonstrated. Our research suggests that BIRC5 may be responsible for the condition of stem cell pluripotency and its high expression may also be responsible for the dedifferentiation of tumor cells.
1. Introduction
Inhibitors of apoptosis (IAP) are a family of proteins and genes whose primary function is to block cell death in response to a variety of stimuli. Eight proteins from the IAP family (NAIP, cIAP1, cIAP2, XIAP, survivin, BRUCE, ML-IAP, and ILP2) have been identified in humans. They interact with many factors, including the ability to regulate and directly bind caspases, whose activation is inevitable in the correct process of apoptosis. Many human types of cancer have been reported to have increased expression of genes and proteins in the IAP family, in many cases having a negative correlation with the clinical condition of the patient, which in turn makes them an attractive target for antineoplastic therapy. The role of IAP proteins and their physiological functions are not fully understood. It is suggested that, apart from their involvement in pathways of apoptosis, they also play their role in cell differentiation, proliferation, signaling, and immune response [1–3].
Due to numerous studies confirming overexpression of IAP in neoplastic diseases and the frequent occurrence of correlated expression of these genes with unfavorable prognosis, they constitute a potential therapeutic target [4, 5]. An increased expression of inhibitors of apoptosis (IAP) has been reported, among others, in hematological malignancies [6–11], breast cancer [12], colon cancer [13–15], stomach cancer [15, 16], lymphoma, hepatocellular carcinoma [17], head and neck cancer [18], bladder cancer [19], and others. Much attention is also devoted to the possibility of using some IAP as diagnostic and prognostic markers in neoplastic diseases [20, 21]. It has been shown that in some types of cancer, cIAP1, cIAP2, Survivin, and XIAP expression levels are associated with unfavorable prognosis. IAP affect tumor cell activity, their invasion, and metastasis [22]; they are also often responsible for cancer cell resistance to chemotherapy and radiotherapy [1, 7]. In recent years, there have been reports of cancer cell apoptosis induced as a result of selective inhibition of IAP proteins by synthetic particles that act analogously to IAP which destabilize their activity and cause degradation through autoubiquitination [23–26].
Survivin encoded by the BIRC5 gene is located on 17q25. Survivin is the smallest protein of the IAP family and is 16.5 kDa large. It contains only one BIR domain which is important for its antiapoptotic function, while its CC domain interacts with the tubulin structure. The highest survivin expression was demonstrated in the G2/M phase of the cell cycle, whereas in the G1 phase, there is a rapid decline in its activity. The survivin gene BIRC5 encodes many genetic variants with unique functions and features, including survivin, survivin-ΔEx-3, survivin-2B, survivin-3B, and survivin 2 alpha. The BIRC5 protein plays a dual role. First, it regulates cell death through indirect or direct interaction with caspases [27], and second, it is an important regulator of mitosis progression and is a component of the CPC complex. It is suggested that survivin, apart from its involvement in cell proliferation [28], plays an important role in cell migration, angiogenesis, DNA damage repair, tissue response to injury, and immune response. In addition, survivin has been shown to regulate the synthesis of microRNA in human leukocytes by limiting the expression of microRNA biosynthesis-controlling proteins at a posttranscriptional level [29]. Most types of cancer are characterized by overexpression of BIRC5 [30]; they include the following types of cancer: breast, liver, ovarian, bladder, lung, stomach, and esophageal and hematological malignancies. In cancer cells, survivin has two main functions; first, it regulates mitosis by forming a CPC complex, and second, it inhibits the process of tumor cell apoptosis. Survivin is one of many important genes that affect tumor aggressiveness and its resistance to therapy, that is why there are numerous attempts to use it in cancer therapy [31–33].
Reactive oxygen species (ROS) leading to the occurrence of oxidative stress have the ability to regulate the expression of genes involved in many processes, among others, immune response or inflammation; it has been shown that oxidative stress can regulate the level of survivin in cancer cells [34, 35]. Survivin overexpression allows survival of cells exposed to oxidative stress [36]. In addition to cancer, increased expression of survivin has been demonstrated in autoimmune diseases and in patients with atherosclerosis in blood lymphocytes [37] which can be connected with increased ROS levels.
Aberrant expression of survivin and disruption of p53 are commonly associated with tumorigenesis [38]. Tumor suppressor gene TP53 regulates expression of genes involved in numerous biological processes, such as the control of the cell cycle, DNA repair, and apoptosis [39]. The tumor suppressor p53 can block cell cycle progression and induce apoptosis. There exists a high possibility that survivin is functionally linked with p53. Many studies have indicated that wildtype p53 can suppress survivin expression at the transcriptional level and that survivin loss of function partially mediates the p53-dependent apoptotic pathway. On the other hand, survivin can regulate p53 expression. One of the studies has shown that overexpression of survivin in human lung cancer cells blocked p53-dependent apoptosis [38].
Overexpression of survivin in carcinoma may overcome cell cycle checkpoints leading to aberrant progression of transformed cells through mitosis [31]. In recent years, efforts have been made to implement survivin as a preferential target and an important prognostic marker in cancer therapy. These approaches based on targeting survivin to enhance tumor cell response to apoptosis and inhibit tumor growth have been developed [38]. It is believed that in some types of cancer, survivin is a diagnostic marker in the early stages [40].
In recent years, numerous studies have been carried out to reduce the expression of the BIRC5 gene or reduce the protein concentration of survivin in cancer cells and their results are promising. Strategies are tested based on the use of antisense strategy, small interfering RNA, small-molecule survivin inhibitors such as YM 155, or immunotherapy [27, 40].
The greatest hope is placed on survivin-directed therapy due to the fact that it is practically absent in mature tissues in nature, while its overexpression has been reported in many cancerous tissues [41–43].
The aim of our study is to demonstrate the potential role of the BIRC5 gene in maintaining pluripotency and differentiation of human stem cells.
2. Material and Methods
The tested material consisted of stem cells and normal cells collected from a group of 131 patients; among them, 43 patients are from the Chair and Department of Haematooncology and Bone Marrow Transplantation, Independent Public Clinical Hospital No. 1 in Lublin, hospitalized between 2014 and 2016, in remission who had previously suffered from hematologic illnesses and provided samples of hematopoietic stem cells from peripheral blood which underwent mobilization through granulocyte growth factor sampled using leukapheresis method. 60 patients are from the Department of Obstetrics and Pathology of Pregnancy, Independent Public Clinical Hospital No. 1 in Lublin, hospitalized between 2014 and 2016, and provided samples of umbilical cords. Cells were isolated from Wharton's jelly by enzymatic extraction (21 patients) and explant method (39 patients). 8 patients are from the Department of Trauma Surgery and Emergency Medicine, Medical University of Lublin, hospitalized between 2014 and 2016, and provided samples of normal bone marrow during hip replacement procedure. 20 healthy volunteers provided samples of peripheral blood. The research was carried out according to the protocol and with the approval of the Bioethics Committee of the Medical University of Lublin, no. KE-0254/128/2014.
Normal cells from peripheral blood and bone marrow were isolated by density-gradient centrifugation using Histopaque-1077 reagent (Sigma, USA) and PBS (BioMed, Lublin, Poland).
Hematopoietic stem cells were isolated in the Department of Haematooncology and Bone Marrow Transplantation, Medical University of Lublin, from the blood of stem cell donors after remission (for autologous transplant). Cells were obtained from peripheral blood, using a cell separator after mobilization with a granulocyte growth factor [44].
Isolation of stem cells from Wharton's jelly from the umbilical cord (from 21 patients-WJC group) was performed by enzymatic digestion using the enzyme collagenase type I (Sigma, USA) [45]. Some of the stem cells from Wharton's jelly (from 39 patients) were isolated using the explant method. The cut pieces of the umbilical cord were placed directly in the culture vessel and incubated for 20 minutes so that the umbilical cord fragments stuck to the plastic surface. Subsequently, the fragments were gently immersed in the growth medium and cultured for 10 days (adherent culture: culture vessel—bottom surface area: 25cm2, TC Flask T25, Cell+, (Sarstedt Germany); volume of growth medium—10 ml, composition: DMEM (1x) + GlutaMAXTM-I [+] 1 g/l D-glucose [+] pyruvate (Gibco, UK); heat-inactivated FBS (Gibco, USA); and amphotericin B 250 μg/ml + penicillin/streptomycin (100x) (PAA, Austria)). Culture conditions are as follows: temperature—37°C, O2 concentration—4%, CO2—5%, and humidity—95%. After approximately 5 days, single cells that migrated from the umbilical cord were observed, sticking to the surface of the culture vessel.
Total RNA was isolated from cells by a modified method of Chomczyński and Sacchi using the following reagents: TRI Reagent (Sigma, USA), chloroform (Sigma, USA), isopropyl alcohol (Sigma, USA), and ethyl alcohol (POSCH).
After isolation, the RNA was dissolved in ultrapure water and the absorbance was measured using a NanoDrop 2000c Thermo Fisher Scientific spectrophotometer at 230 nm, 260 nm, 280 nm, and 320 nm wavelengths. Qualitative and quantitative evaluation of RNA extraction was performed.
Later, the reaction of reverse transcription (RT) was performed using a set of reagents—High-Capacity cDNA Transcription Kits (Applied Biosystems, USA) with RNAz inhibitor (RNase Inhibitor, Applied Biosystems, USA). 1 μg of isolated RNA was used in the RT reaction. The reaction was performed according to the manufacturer's protocol.
The study of BIRC5 expression was performed at the transcription level using PCR method in real time with StepOnePlus Applied Biosystems. Based on cDNA, qPCR reaction was performed using commercially available reagent kits from Applied Biosystems. TaqMan molecular probes were used for the tested genes: BIRC5 gene—Hs00153353_m1 (Applied Biosystems, USA), reference gene GAPDH—Hs99999905_m1 (Applied Biosystems, USA). The reactions were performed in 96-well plates (MicroAmp Fast Optical 96-Well Reaction Plate, Applied Biosystems, USA) in a volume of 25 μl/well, consisting of 1 μl cDNA synthesized in the reverse transcription reaction, 10.25 μl RNAz- and DNAz-free ultrapure water, 1.25 μl gene-specific probe, and 12.5 μl TaqMan Gene Expression Master Mix (Applied Biosystems, USA). The real-time PCR reaction, after the initial 10-minute denaturation at 95°C, was carried out according to the following scheme—40 cycles: 15 seconds at 95°C and 60 seconds at 60°C.
Gene expression analysis and statistical analysis were performed using ExpressionSuite Software v1.0.3., StepOne Software v2.2.2, and Statistica v13. Relative gene expression (RQ) was calculated by the formula: RQ = 2−∆∆Ct [46]. Statistical analysis was performed using one-way ANOVA and Unequal N HSD for post hoc tests. Significant results were recognized for p < 0.05.
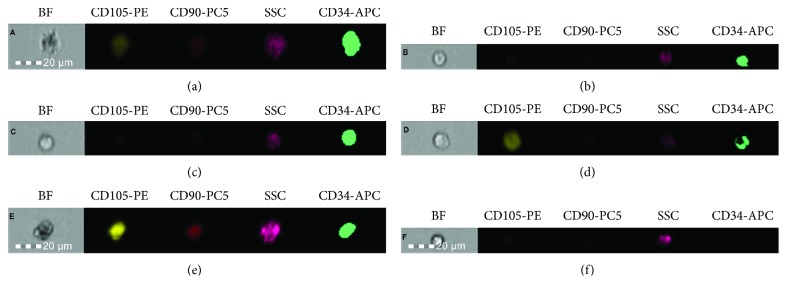
Some of the collected cells were used for cytometric analysis in order to mark expression of surface antigen characteristic of mesenchymal and hematopoietic stem cells. The research was performed on cells freshly collected from the tested material or after a period of freezing at the temperature of liquid nitrogen (in the case of hematopoietic stem cells isolated from peripheral blood). The percentage of cells demonstrating expression of surface antigens CD34, CD90, and CD105 was evaluated. The cytometric analysis was performed according to the protocol described in our paper [45]. Based on the cytometric analysis, the presence of CD34+, CD105+, and CD90+ cells in the tested material has been confirmed. It has been demonstrated that in the group of cells derived from Wharton's jelly, before and after subjecting to cell culture, more than half of the study population consisted of CD105+ cells. In turn, in the group of mobilized cells isolated from peripheral blood, before and after subjecting to cell culture, CD34+ cells represented the majority of the tested population. In these groups the percentage of CD90+ and CD105+ cells have not exceeded 5%.
3. Results
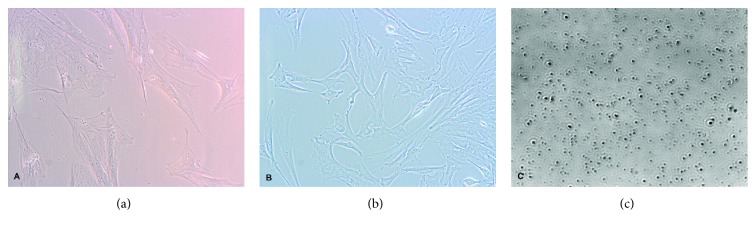
Photographic documentation of the tested cells was performed during cell culture (Figure 1) and during cytometric analysis (Figure 2).
Figure 1.
(a, b) Microscopic image of the sample from Wharton's jelly (WJC-CC) blood stem cells (PBSC-CC). The photographs were taken on day 10 during cell culture using an Olympus CKX 41 inverted microscope and Olympus XC50 camera (magnification 200x, eyepiece 10x, and lens 20x). (c) Microscopic image of the sample from peripheral. The photograph was taken on day 10 during cell culture using real-time live cell imaging system xCellence RT and Olympus IX81 inverted microscope (magnification 100x, eyepiece 10x, and lens 10x).
Figure 2.
Photographs of single samples of cells from the (a) BM group, (b) PBSC group, (c) PBSC-CC group, (d) WJC group, (e) WJC-CC group, and (f) PBMC group. Photographs presenting BF (microscope image) and fluorescence in channels, showing the expression of studied antigens (CD105, CD90, and CD34). SSC (side scatter—assessment of cell morphology). The analysis and photographs were taken using the FlowSight f. Amnis flow cytometer.
The research has shown that BIRC5 demonstrates expression at the transcription level in all trials, in the umbilical cord mesenchymal stem cells, hematopoietic stem cells derived from bone marrow and peripheral blood, and normal blood cells. Figure 3 shows average relative expression of BIRC5 (logRQ ± SE) in the tested groups.
Figure 3.
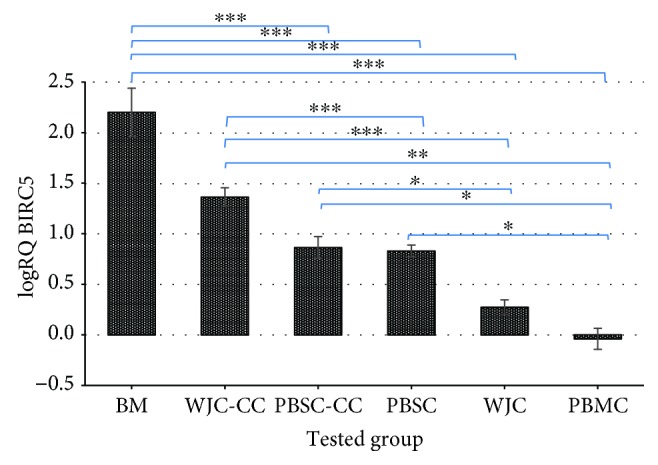
Average BIRC5 expression on the mRNA level in the group of normal bone marrow cells (BM), peripheral blood hematopoietic stem cells previously subjected to mobilization (PBSC), and Wharton's jelly cells from the umbilical cord isolated using enzymatic digestion with the enzyme collagenase type I (WJC), explant method (WJC-CC), as compared to the average BIRC5 expression in the group of normal peripheral blood cells from healthy individuals (PBMC) (blood—calibrator). The presented result is shown in the logarithm of average relative expression (logRQ) in the whole tested group ± SE. ∗∗∗p < 0.0001, ∗∗p < 0.001, and ∗p < 0.05.
Based on the analysis of BIRC5 expression in the group of tested cells, the lowest average expression has been found in the normal blood cells of healthy individuals, whereas the highest BIRC5 expression has been demonstrated in the normal bone marrow cells. This group shows nearly 350-fold increase in expression relative to the peripheral blood cells from healthy individuals. BIRC5 demonstrates expression 59 times significantly higher in cells isolated from the umbilical cord using the explant method, but in cells directly isolated from the umbilical cord using enzymatic digestion, BIRC5 expression was more than twice higher relative to blood cells. In peripheral blood hematopoietic stem cells subjected to mobilization, survivin gene expression is more than 10-fold higher than that of normal mature blood cells (Table 1).
Table 1.
The difference in BIRC5 expression levels in bone marrow cells (BM), peripheral blood cells subjected to mobilization (PBSC, PBSC-CC) and Wharton's jelly (WJC, WJC-CC), and in peripheral blood cells (PBMC). One-way ANOVA post hoc test (Unequal N HSD).
| The difference in BIRC5 expression levels | p value (one-way ANOVA; Unequal N HSD for post hoc tests) | |||||||
|---|---|---|---|---|---|---|---|---|
| Tested group | N | Mean BIRC5 expression (RQ ± SE) | BM | WJSC-CC | PBCS-CC | PBSC | WJSC | PBMC |
| BM | 8 | 350.2 ± 165.9 | 0.104711 | 0.000070∗ | 0.000067∗ | 0.000029∗ | 0.000029∗ | |
| WJC-CC | 39 | 59.0 ± 17.1 | 0.104711 | 0.152726 | 0.000734∗ | 0.000029∗ | 0.000030∗ | |
| PBSC-CC | 43 | 18.0 ± 10.6 | 0.000070∗ | 0.152726 | 1.000000 | 0.028835∗ | 0.009662∗ | |
| PBSC | 43 | 10.0 ± 1.9 | 0.000067∗ | 0.000734∗ | 1.000000 | 0.011196∗ | 0.010301∗ | |
| WJC | 21 | 2.5 ± 0.40 | 0.000029∗ | 0.000029∗ | 0.028835∗ | 0.011196∗ | 0.993846 | |
| PBMC | 20 | 1.2 ± 0.4 | 0.000029∗ | 0.000030∗ | 0.009662∗ | 0.010301∗ | 0.993846 | |
4. Discussion
In the research carried out by Fukuda et al. [47], it was noticed that stimulation with a growth factor causes the increase in survivin expression prior to the entry into the cell cycle, which suggests that the increase in survivin expression in hematopoietic stem cells may be related to a regulating influence of growth factor and not only to a cell cycle phase [47]. In our study, higher BIRC5 expression has been found in cells after 10 days of cell culture, which confirms the contribution of BIRC5 in a cell cycle and its involvement in cell proliferation. In the case of cultured Wharton's jelly cells, a significantly higher difference in BIRC5 expression has been observed compared to noncultured cells. It might be caused not only by the involvement of BIRC5 in cell proliferation but also by a higher content of mesenchymal stem cells in the tested material after adherent cell culture as compared to the noncultured heterogeneous population subjected to enzymatic isolation, which would explain high BIRC5 expression in stem cells.
The study by Zwerts et al. proved that the structures of the embryo show high survivin expression, whereas its absence in endothelial cells contributes to the death of the embryo. Studies carried out demonstrate that the presence of survivin is essential for normal development and organogenesis. The involvement of survivin in regulation of endothelial cell survival and its influence on maintaining vascular integrity play a vital role in neurogenesis, angiogenesis, and cardiogenesis [48].
Lee et al. in their research speculated that survival of undifferentiated human pluripotent stem cells (hPSC) is highly dependent on antiapoptotic factors like survivin; moreover, they found that exposure of human pluripotent stem cells to a survivin inhibitor like YM155 eliminates undifferentiated hPSC without affecting differentiated cells [49]. Zhou et al was noticed that survivin was one of the factors to participate in human embryonic stem cells or induced pluripotent stem cell pluripotency maintenance. They found that overexpression of survivin in human neural progenitor cells could enhance the efficiency of 1F-OCT4 reprogramming to induced pluripotent stem cells. Authors reported that the mechanism of survivin to maintain the pluripotent state of embryonic stem cells was that it could interact with β-catenin in the WNT signal pathway [50]. The research of Kapinas et al. also confirms the commitment of survivin to maintain the state of pluripotency; the authors suggest that survivin is regulated by miR203 and 0 and NANOG [51]. In our study, the correlation between higher BIRC5 expression and lower cell differentiation status has been proved. This phenomenon may be explained by the involvement of BIRC5 on the transcription level in maintaining stem cell pluripotency.
Alteri and Mull et al. reported very high levels of survivin expression in embryonic stem cells, pluripotent cells, and somatic stem cells. The authors suggest that survivin expression in these cells is related to regulation of cell proliferation and that it affects the signaling pathway characteristic for stem cells. It is also suggested that survivin in stem cells may be involved in pluripotency control at the level of gene expression, although this function has not been investigated yet [52, 53].
Leung et al. also report high survivin expression in hematopoietic stem cells. The authors suggest that BIRC5 is a key gene responsible for proliferation and sustaining hematopoietic stem cells and progenitor cells. It was also observed that a decrease in the level of survivin may result in the decrease of cell cycle efficiency, which in turn leads to defects in erythroid maturation. Another research shows that deletion of survivin in mice results in the loss of progenitor cells and hematopoietic stem cells and causes bone marrow ablation and sudden death [54]. In our research, the highest BIRC5 expression has been found in cells derived from normal bone marrow. Such high BIRC5 expression is probably due to the fact that bone marrow is a source of both hematopoietic stem cells and mesenchymal stem cells [55, 56].
Conducted own studies and analysis of available literature show that both hematopoietic and mesenchymal stem cells demonstrate survivin expression and that this gene is involved in stem cell survival. It is also essential for their differentiation and proper functioning.
Taking into consideration that many human types of cancer have been reported to have higher expression of genes and proteins from the IAP family which in numerous cases has a negative correlation with the clinical condition of the patient, IAP make an attractive target for antineoplastic therapy. Survivin expression has been reported in many types of cancer, and its level correlates with the more aggressive disease course and poor course of treatment. Normal mature tissues do not demonstrate survivin expression, or it is minimal as confirmed by the study. That is why survivin seems to be both a good diagnostic factor and a good prognostic factor as well as a target for antineoplastic therapy [31].
Fong et al. studied expression of numerous genes, including BIRC5 at the transcription level in human stem cell collected from Wharton's jelly (hWJSCs). Their analysis confirmed mRNA expression of BIRC5 in the tested cells. They showed that hWJSC is characterized by lower BIRC5 expression as compared to embryonic stem cells (ESCs). The authors suggest that lower BIRC5 expression in hWJSCs as compared to ECSs may be responsible for the antineoplastic properties of mesenchymal stem cells from Wharton's jelly [57]. In our own studies, survivin gene expression in mesenchymal cells from the umbilical cord subjected to cell culture (WJC-CC) demonstrates significantly higher levels than those in hematopoietic PBSC and in normal PBMC. On the other hand, cell population derived from the umbilical cord (WJC) directly after collagenase digestion in comparison with hematopoietic blood stem cells demonstrate lower expression, which might be due to the antineoplastic properties of mesenchymal stem cells freshly derived from the umbilical cord.
Lower BIRC5 expression in mesenchymal stem cells confirms their antineoplastic effect. Increased BIRC5 expression in hematopoietic stem cells relative to mesenchymal stem cells may be associated with a higher degree of differentiation of these cells which would confirm the involvement of BIRC5 in cell differentiation.
5. Conclusions
The study confirms the involvement of BIRC5 from the IAP family in many physiological processes apart from apoptosis inhibition. Our research suggests that BIRC5 may be responsible for the condition of stem cell pluripotency, and its high expression may also be responsible for the dedifferentiation of tumor cells.
Acknowledgments
This study was supported in part by founds from the project “the equipment of innovative laboratories doing research on new medicines used in the therapy of civilization and neoplastic diseases” within the Operational Program Development of Eastern Poland 2007-2013, Priority Axis I Modern Economy, Operations I.3 Innovation Promotion and the project “the evaluation of survivin expression in hematopoietic stem cells” within the Scholarship Fund of the Medical University of Lublin.
Abbreviations
- BM:
Bone marrow cells isolated using density-gradient centrifugation method (cells collected from a group of 8 patients)
- PBSC:
Peripheral blood hematopoietic stem cells previously subjected to mobilization (cells collected from a group of 43 patients)
- PBSC-CC:
Peripheral blood stem cells previously subjected to mobilization and cultured for the period of 10 days (cells collected from a group of 43 patients)
- WJC:
Wharton's jelly cells from the umbilical cord isolated using enzymatic digestion with the enzyme collagenase type I (cells collected from a group of 21 patients)
- WJC-CC:
Wharton's jelly cells from the umbilical cord cultured for the period of 10 days (cells collected from a group of 39 patients)
- PBMC:
Peripheral blood mononuclear cells isolated using density-gradient centrifugation method (cells collected from a group of 20 healthy volunteers).
Data Availability
The data used to support the findings of this study are included within the article and can be applicable from the corresponding author.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- 1.Silke J., Vucic D. IAP family of cell death and signaling regulators. Methods in Enzymology. 2014;545:35–65. doi: 10.1016/B978-0-12-801430-1.00002-0. [DOI] [PubMed] [Google Scholar]
- 2.Middleton A. J., Budhidarmo R., Day C. L. Use of E2~ubiquitin conjugates for the characterization of ubiquitin transfer by RING E3 ligases such as the inhibitor of apoptosis proteins. Methods in Enzymology. 2014;545:243–263. doi: 10.1016/B978-0-12-801430-1.00010-X. [DOI] [PubMed] [Google Scholar]
- 3.Almagro M. C., Vucic D. The inhibitor of apoptosis (IAP) proteins are critical regulators of signaling pathways and targets for anti-cancer therapy. Experimental Oncology. 2012;3:200–211. [PubMed] [Google Scholar]
- 4.Dubrez L., Rajalingam K. IAPs and cell migration. Seminars in Cell & Developmental Biology. 2015;39:124–131. doi: 10.1016/j.semcdb.2015.02.015. [DOI] [PubMed] [Google Scholar]
- 5.Wright C. W., Duckett C. S. Reawakening the cellular death program in neoplasia through the therapeutic blockade of IAP. Journal of Clinical Investigation. 2005;115(10):2673–2678. doi: 10.1172/JCI26251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smolewski P., Robak T. Inhibitors of apoptosis proteins (IAPs) as potential molecular targets for therapy of hematological malignancies. Current Molecular Medicine. 2011;11(8):633–649. doi: 10.2174/156652411797536723. [DOI] [PubMed] [Google Scholar]
- 7.Fulda S. Inhibitor of apoptosis (IAP) proteins in pediatric leukemia: molecular pathways and novel approaches to therapy. Frontiers in Oncology. 2014;4, article 3 doi: 10.3389/fonc.2014.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zaman S., Wang R., Gandhi V. Targeting the apoptosis pathway in hematologic malignancies. Leukemia & Lymphoma. 2014;55(9):1980–1992. doi: 10.3109/10428194.2013.855307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Finlay D., Teriete P., Vamos M., Cosford N. D. P., Vuorib K. Inducing death in tumor cells: roles of the inhibitor of apoptosis proteins. F1000Research. 2017;6:p. 587. doi: 10.12688/f1000research.10625.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chomik P., Gil-Kulik P., Filas M., et al. The expression BIRC6 gene in patients with chronic lymphocytic leukemia – a preliminary study. Current Issues in Pharmacy and Medical Sciences. 2014;27(3):179–182. doi: 10.1515/cipms-2015-0011. [DOI] [Google Scholar]
- 11.de Graaf A. O., de Witte T., Jansen J. H. Inhibitor of apoptosis proteins: new therapeutic targets in hematological cancer? Leukemia. 2004;18(11):1751–1759. doi: 10.1038/sj.leu.2403493. [DOI] [PubMed] [Google Scholar]
- 12.Pluta P., Jeziorski A., Cebula-Obrzut A. P., Wierzbowska A., Piekarski J., Smolewski P. Expression of IAP family proteins and Its clinical importance in breast cancer patients. Neoplasma. 2015;62(04):666–673. doi: 10.4149/neo_2015_080. [DOI] [PubMed] [Google Scholar]
- 13.Miura K., Karasawa H., Sasaki I. cIAP2 as a therapeutic target in colorectal cancer and other malignancies. Expert Opinion on Therapeutic Targets. 2009;13(11):1333–1345. doi: 10.1517/14728220903277256. [DOI] [PubMed] [Google Scholar]
- 14.Miura K., Fujibuchi W., Ishida K., et al. Inhibitor of apoptosis protein family as diagnostic markers and therapeutic targets of colorectal cancer. Surgery Today. 2011;41(2):175–182. doi: 10.1007/s00595-010-4390-1. [DOI] [PubMed] [Google Scholar]
- 15.Hu T., Weng S., Tang W., et al. Overexpression of BIRC6 is a predictor of prognosis for colorectal cancer. PLoS One. 2015;10(5, article e0125281) doi: 10.1371/journal.pone.0125281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jung S. A., Park Y. M., Hong S. W., et al. Cellular inhibitor of apoptosis protein 1 (cIAP1) stability contributes to YM155 resistance in human gastric cancer cells. Journal of Biological Chemistry. 2015;290(16):9974–9985. doi: 10.1074/jbc.m114.600874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Augello C., Caruso L., Maggioni M., et al. Inhibitors of apoptosis proteins (IAPs) expression and their prognostic significance in hepatocellular carcinoma. BMC Cancer. 2009;9(1):p. 125. doi: 10.1186/1471-2407-9-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen Y. K., Huse S. S., Lin L. M. Expression of inhibitor of apoptosis family proteins in human oral squamous cell carcinogenesis. Head & Neck. 2011;33(7):985–998. doi: 10.1002/hed.21582. [DOI] [PubMed] [Google Scholar]
- 19.Srivastava A. K., Singh P. K., Srivastava K., et al. Diagnostic role of survivin in urinary bladder cancer. Asian Pacific Journal of Cancer Prevention. 2013;14(1):81–85. doi: 10.7314/apjcp.2013.14.1.81. [DOI] [PubMed] [Google Scholar]
- 20.Hunter A. M., LaCasse E. C., Korneluk R. G. The inhibitors of apoptosis (IAPs) as cancer targets. Apoptosis. 2007;12(9):1543–1568. doi: 10.1007/s10495-007-0087-3. [DOI] [PubMed] [Google Scholar]
- 21.Glodkowska-Mrowka E., Solarska I., Mrowka P., et al. Differential expression of BIRC family genes in chronic myeloid leukaemia – BIRC3 and BIRC8 as potential new candidates to identify disease progression. British Journal of Haematology. 2014;5:740–742. doi: 10.1111/bjh.12663. [DOI] [PubMed] [Google Scholar]
- 22.Mehrotra S., Languino L. R., Raskett C. M., Mercurio A. M., Dohi T., Altieri D. C. IAP regulation of metastasis. Cancer Cell. 2010;17(1):53–64. doi: 10.1016/j.ccr.2009.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sekine K., Takubo K., Kikuchi R., et al. Small molecules destabilize cIAP1 by activating auto-ubiquitylation. Journal of Biological Chemistry. 2008;283(14):8961–8968. doi: 10.1074/jbc.m709525200. [DOI] [PubMed] [Google Scholar]
- 24.Feltham R., Bettjeman B., Budhidarmo R., et al. Smac mimetics activate the E3 ligase activity of cIAP1 protein by promoting RING domain dimerization. Journal of Biological Chemistry. 2011;286(19):17015–17028. doi: 10.1074/jbc.m111.222919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hassan M., Watari H., AbuAlmaaty A., Ohba Y., Sakuragi N. Apoptosis and molecular targeting therapy in cancer. BioMed Research International. 2014;2014:23. doi: 10.1155/2014/150845.150845 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 26.Galbán S., Hwang C., Rumble J. M., et al. Cytoprotective effects of IAPs revealed by a small molecule antagonist. Biochemical Journal. 2009;3:765–771. doi: 10.1042/bj20081677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khan Z., Khan A. A., Yadav H., Prasad G. B. K., Bisen P. S. Survivin, a molecular target for therapeutic interventions in squamous cell carcinoma. Cellular & Molecular Biology Letters. 2017;22(1):p. 8. doi: 10.1186/s11658-017-0038-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jarrin M., Mansergh F. C., Boulton M. E., Gunhaga L., Wride M. A. Survivin expression is associated with lens epithelial cell proliferation and fiber cell differentiation. Molecular Vision. 2012;18(27):58–69. [PMC free article] [PubMed] [Google Scholar]
- 29.Gravina G., Wasén C., Garcia-Bonete M. J., et al. Survivin in autoimmune diseases. Autoimmunity Reviews. 2017;16(8):845–855. doi: 10.1016/j.autrev.2017.05.016. [DOI] [PubMed] [Google Scholar]
- 30.Brodská B., Otevlelová P., Holoubek A. Decitabine and SAHA-induced apoptosis is accompanied by survivin downregulation and potentiated by ATRA in p53-deficient cells. Oxidative Medicine and Cellular Longevity. 2014;2014:13. doi: 10.1155/2014/165303.165303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jaiswal P. K., Goel A., Mittal R. D. Survivin: a molecular biomarker in cancer. Indian Journal of Medical Research. 2015;141(4):389–397. doi: 10.4103/0971-5916.159250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Owens T. W., Gilmore A. P., Streuli C. H., Foster F. M. Inhibitor of apoptosis proteins: promising targets for cancer therapy. Journal of Carcinogenesis & Mutagenesis. 2013;S14:p. 004. doi: 10.4172/2157-2518.s14-004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Di Stefano A. B., Iovino F., Lombardo Y., et al. Survivin is regulated by interleukin-4 in colon cancer stem cells. Journal of Cellular Physioogy. 2010;225(2):555–561. doi: 10.1002/jcp.22238. [DOI] [PubMed] [Google Scholar]
- 34.Dudzińska E., Gryzinska M., Ognik K., Gil-Kulik P., Kocki J. Oxidative stress and effect of treatment on the oxidation product decomposition processes in IBD. Oxidative Medicine and Cellular Longevity. 2018;2018:7. doi: 10.1155/2018/7918261.7918261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pervin S., Tran L., Urman R., et al. Oxidative stress specifically downregulates survivin to promote breast tumour formation. British Journal of Cancer. 2013;108(4):848–858. doi: 10.1038/bjc.2013.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kan C., Petti C., Bracken L., et al. Up-regulation of survivin during immortalization of human myofibroblasts is linked to repression of tumor suppressor p16INK4a protein and confers resistance to oxidative stress. The Journal of Biological Chemistry. 2013;288(17):12032–12041. doi: 10.1074/jbc.M112.447821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gil-Kulik P., Niedojadło A., Feldo M., et al. The gene expression of class III inhibitors of apoptosis in arteriosclerotic disease. Polish Journal of Public Health. 2014;124(1):38–41. doi: 10.2478/pjph-2014-0008. [DOI] [Google Scholar]
- 38.Chen X., Duan N., Zhang C., Zhang W. Survivin and tumorigenesis: molecular mechanisms and therapeutic strategies. Journal of Cancer. 2016;7(3):314–323. doi: 10.7150/jca.13332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dudzińska E., Gryzińska M., Ognik K., Krauze M., Listos P. Non-specific inflammatory bowel diseases and the risk of tumour growth. Medycyna Weterynaryjna. 2018;74(1):228–232. doi: 10.21521/mw.6048. [DOI] [Google Scholar]
- 40.Mobahat M., Narendran A., Riabowol K. Survivin as a preferential target for cancer therapy. International Journal of Molecular Sciences. 2014;15(2):2494–2516. doi: 10.3390/ijms15022494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schimmer A. D. Inhibitor of apoptosis proteins: translating basic knowledge into clinical practice. Cancer Research. 2004;64(20):7183–7190. doi: 10.1158/0008-5472.CAN-04-1918. [DOI] [PubMed] [Google Scholar]
- 42.Huang J., Lyu H., Wang J., Liu B. MicroRNA regulation and therapeutic targeting of survivin in cancer. American Journal of Cancer Research. 2014;1:20–31. [PMC free article] [PubMed] [Google Scholar]
- 43.Cheung C. H., Huang C. C., Tsai F. Y., et al. Survivin - biology and potential as a therapeutic target in oncology. Onco Targets Ther. 2013;6:1453–1462. doi: 10.2147/OTT.S33374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Borowska H., Klimek P., Cioch M. The obtaining of peripheral blood stem cells and evaluation of Its viability in the apheresis product before and after cryopreservation. Journal of Laboratory Diagnostics. 2014;50(3):249–254. [Google Scholar]
- 45.Walecka I., Gil-Kulik P., Krzyżanowski A., et al. Phenotypic characterization of adherent cells population CD34+ CD90+ CD105+ derived from Wharton's jelly. Medical Science Monitor. 2017;23:1886–1895. doi: 10.12659/MSM.902186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Livak K. J., Schmittgen T. D. Analysis of relative gene expression data using real-time quantitative PCR and the 2−ΔΔCT method. Methods. 2011;25(4):402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 47.Fukuda S., Foster R. G., Porter F. S., Pelus L. M. The antiapoptosis protein survivin is associated with cell cycle entry of normal cord blood CD34+ cells and modulates cell cycle and proliferation of mouse hematopoietic progenitor cells. Blood. 2002;100(7):2463–2471. doi: 10.1182/blood.v100.7.2463. [DOI] [PubMed] [Google Scholar]
- 48.Zwerts F., Lupu F., De Vriese A., et al. Lack of endothelial cell survivin causes embryonic defects in angiogenesis, cardiogenesis, and neural tube closure. Blood. 2007;109(11):4742–4752. doi: 10.1182/blood-2006-06-028068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee M. O., Moon S. H., Jeong H.-C., et al. Inhibition of pluripotent stem cell-derived teratoma formation by small molecules. Proceedings of the National Academy of Sciences of the United States of America. 2013;110(35):E3281–E3290. doi: 10.1073/pnas.1303669110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhou S., Liu Y., Feng R., et al. Survivin improves reprogramming efficiency of human neural progenitors by single molecule OCT4. Stem Cells International. 2016;2016:11. doi: 10.1155/2016/4729535.4729535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kapinas K., Kim H., Mandeville M., et al. microRNA-mediated survivin control of pluripotency. Journal of Cellular Physiology. 2015;230(1):63–70. doi: 10.1002/jcp.24681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Alteri D. C. Survivin – the inconvenient IAP. Seminars in Cell & Developmental Biology. 2015;39:91–96. doi: 10.1016/j.semcdb.2014.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mull A. N., Klar A., Navara C. Differential localization and high expression of survivin splice variants in human embryonic stem cells but not in differentiated cells implicate a role for survivin in pluripotency. Stem Cell Research. 2014;12(2):539–549. doi: 10.1016/j.scr.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 54.Leung C. G., Xu Y., Mularski B., Liu H., Gurbuxani S., Crispino J. D. Requirements for survivin in terminal differentiation of erythroid cells and maintenance of hematopoietic stem and progenitor cells. Journal of Experimental Medicine. 2007;204(7):1603–1611. doi: 10.1084/jem.20062395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Maijenburg M. W., Kleijer M., Vermeul K., et al. The composition of the mesenchymal stromal cell compartment in human bone marrow changes during development and aging. Haematologica. 2012;97(2):179–183. doi: 10.3324/haematol.2011.047753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Reagan M. R., Rosen C. J. Navigating the bone marrow niche: translational insights and cancer-driven dysfunction. Nature Reviews Rheumatology. 2016;12(3):154–168. doi: 10.1038/nrrheum.2015.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fong C. Y., Chak L. L., Biswas A., et al. Human Wharton’s jelly stem cells have unique transcriptome profiles compared to human embryonic stem cells and other mesenchymal stem cells. Stem Cell Reviews and Reports. 2010;7:1–16. doi: 10.1007/s12015-010-9166-x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used to support the findings of this study are included within the article and can be applicable from the corresponding author.