Abstract
Background and Purpose
Researchers have used an injury risk algorithm utilizing demographic data, injury history, the Functional Movement Screen™ (FMS™) and Lower Quarter Y Balance Test™ (YBT™) scores to categorize individual injury risk. The purpose of this study was to identify if a group-based hybrid injury prevention program utilizing key factors from previous research with the addition of an individualized approach can modify the injury risk category of athletes.
Study Design
Cohort Study
Methods
Forty-four female subjects (ages 14-17) were recruited from a local high school soccer team. Pre-participation testing included demographic data, injury history, FMS™ and YBT™ to determine if each athletes’ injury risk category using the Move2Perform algorithm. Post-testing took place after an eight-week exercise-based intervention program was completed. McNemar analysis was utilized to assess changes in the injury risk categories.
Results
A significant number of athletes (21 of 44) moved to lower risk categories at posttest (p=0.000; Z=-3.869). Of the 32 athletes in the High Risk category at pretest, 16 were Low Risk after the intervention (p=0.002).
Conclusions
A preseason, group injury prevention training program with individually prescribed corrective exercises, resulted in a significant number of subjects decreasing their injury risk category. The primary statistically significant decrease of injury risk category was seen in the Moderate Risk individuals moving down to Slight. There were three athletes that moved from the Substantial Risk category to Slight, however, this change was not statistically significant.
Level of Evidence
2
Keywords: Movement system, injury prevention training program, risk category
INTRODUCTION
With over seven million students participating in high school athletics alone, the yearly occurrences of sports related injury are very high. Injuries range from one day of lost time to career limiting injuries. Potential career limiting injuries like anterior cruciate ligament tears, ulnar collateral ligament tears, and compound fractures are on the rise across the spectrum of little leaguers to professional athletes.1,2 Despite the presence of injury prevention programs, sports injuries are a continued problem with an estimated two million injuries occurring annually.1 While injury prevention programs like FIFA 11+, the PEP program, and SportsMetrics have been shown to decrease injury rate, they do not work for all populations or even all individuals in the population.3 One reason that these programs might not work in all cases is that injury risk is multifactorial and the aforementioned programs are not individualized nor comprehensive with their interventions. For example, FIFA 11 + includes a variety of running, strength, plyometric and balance exercises, but no exercises to address commonly present mobility restrictions. SportsMetrics focuses on jumping and landing mechanics, but lacks other evidence-based injury prevention interventions to address balance, core, strength and/or mobility. Since injury risk is multifactorial and each individual has unique deficits, it seems logical to individualize the interventions as much as is practical. This individualization would address additional domains, potentially resulting in a greater injury risk reduction.
Researchers have identified multiple risk factors that increase risk of injury, with previous injury being the most consistently reported risk factor.4 Other variables such as low or high body mass index, faulty biomechanics, core motor control deficits, and muscle flexibility deficits have also been identified as risk factors.4 Knee valgus with drop jump landing has been identified as another risk factor for anterior cruciate ligament tears in female athletes.5 To complicate matters further, each individual may possess different combinations of risk factors. Thus, group programs may spend too much time on a particular risk factor for an individual that does not possess that problem, and too little time on risk factors that are more profound for the individual thereby under or overdosing specific prevention efforts.
Identifying risk factors is beneficial in order to begin the process of prevention, however, screening for every risk factor is not practical. The Functional Movement Screen™ (FMS™) and Y-Balance Test Lower Quarter (YBT-LQ™) are two tools that have emerged in the literature as field-expedient options to capture multiple risk factors efficiently.6-21 The FMS™ is a series of tests that can screen a person's ability to perform seven fundamental bodyweight tasks, scored on an ordinal scale from 0-3. Initial research of the FMS™ identified a cut score of ≤14 on FMS™ to be predictive of injury risk in American football players.12,19 This cut point was supported by a recent meta-analysis, which concluded that individuals scoring ≤14 had an OR of 2.74 (95% CI 1.70-4.43).22 Additionally, at least one asymmetry in hurdle stepping, lunging, active straight leg raising, or quadruped diagonal reaching patterns was associated with increased risk for a time-loss musculoskeletal injury in American football players22 and later confirmed by Mokha et al23 as a risk factor for potential musculoskeletal injury in Division II athletes. The Y Balance Test Lower Quarter™ (YBT-LQ™) is a test that measures a person's dynamic motor control at his or her limits of stability. Three studies have explored the relationship between scores on the YBT-LQ™ and future injury.15,16,24 Researchers have found that cutoff composite scores vary based on variables such as sport, gender, and age, but can be highly sensitive in detecting increased injury risk, making the YBT-LQ™ a useful screening tool. Asymmetries in the anterior and posteromedial reach on the YBT-LQ™ have been shown to increase risk for injury in active populations.16,25
Researchers have developed a computer algorithm (Move2Perform, Functional Movement Systems, Chatham, VA) that can synthesize multiple risk factors including demographic factors, injury history, and results of field-expedient tests (including the FMS™ and YBT-LQ™) to place an athlete into one of four categories according to risk level. The software algorithm further uses population specific cut points to place the athlete in the risk category. Lehr et al3 established a significant association between the risk category of an athlete identified by the computer algorithm and noncontact lower extremity injury in collegiate athletes. Athletes who were in the Substantial and Moderate Risk were 3.4 times more like to sustain an injury compared to those in Slight or Optimal groups.3
While athletes at high risk for injury may be able to be identified by the Move2Perform algorithm, the question remains if risk category can be modified. Both the FMS™ and YBT-LQ™ have been identified as modifiable with exercise. Kiesel et al27 found that utilizing a seven-week off-season intervention program, 52% of professional football players in the program were able to score above the injury cut score of 14. Individualized corrective exercises were prescribed based on each player's specific deficit on the FMS™ and the athletes had a supervised progression of these corrections over the course of seven weeks.27 A randomized controlled trial performed by Bodden et al28 also identified the FMS™ is modifiable with the prescription of corrective exercises over a course of four and eight weeks in mixed martial arts athletes.28 The YBT-LQ™ and SEBT have also been shown to be modifiable with an exercised based program. Steffen et al29 identified a significant improvement of functional balance as tested by the SEBT in athletes who highly adhered to the FIFA 11 + program which included a 20 min warm-up consisting of 15 single exercises that focused on strength, plyometrics, agility and field balance techniques. Those athletes also were identified as having a 72% reduction of injury risk based on their improvements on the SEBT.29 Thus, FIFA 11 + appears to be effective at reducing injury risk, but may benefit from the addition of an individualized approach to further decrease injury risk.
A systematic approach to injury prevention should take the best available evidence and apply it in a logical manner. Since group injury prevention programs have been shown to decrease injury rate,30-32 it would be prudent to include the components of these programs that demonstrate effectiveness. There are also several other variations of injury prevention training protocols within the literature which include strength training, coordination, speed and agility, flexibility, balance training, and jumping. Rossler et al32 found a 46% reduction in injuries in organized youth sports with the implementation of an exercise-based injury prevention program and further identified the need for jumping/plyometric exercises being particularly relevant for the reduction. Among the 21 studies reviewed by Rossler et al,32 each study included either a progressive difficulty level that increased weekly or a continuous difficulty level which increased at each session. There are lots of variability in session time frames as some injury prevention programs included only a five-minute warm-up, while others lasted for 30 minutes. Overall, Rossler et al32 found that all injury prevention programs were significantly effective in children and adolescents with the greatest risk reduction in the sub-elite athlete.
While it appears exercise-based injury prevention programs decrease risk of injury and improve scores on functional movement and balance testing, no current research has identified if the Move2Perform injury risk category can be modified. Therefore, the purpose of this study was to identify if a group-based hybrid injury prevention program utilizing key factors from previous research with the addition of an individualized approach can modify the injury risk category of athletes.
METHODS
This study was approved by the University of Evansville's Institutional Review Board. Fifty-four high school female soccer players were enrolled in the program over the course of three years, with forty-four athletes included in participation of the program. All players were educated on the program and testing involved. Inclusion criteria included: 14-17 years old, female, current athlete in preseason of their sport. Subjects were excluded from the program if they had a current injury or were not medically cleared to participate. Previous injury was defined as ‘any injury occurring during athletic activity resulting in medical attention and/or the removal of the player from the current session and/or subsequent time loss of at least one athletic session (match or practice) as a direct result of that injury.’26 All of the subjects were under legal age, therefore parental informed consent and release of testing information for research use was obtained in order to house athlete's data within the Move2Perform database. Each athlete's data was pulled from the Move2Perfom database and deidentified for statistical analysis. Program design included individually prescribed corrective exercises and 14 supervised group sessions that included jump, agility, and core training over the course of eight weeks.
Testing
Testing was performed on all 44 subjects at the beginning of the eight-week training session. Testing included demographic data, injury history, FMS™ and YBT™ testing which identified each athlete's injury risk category per Move2Perform algorithm. Each athlete was categorized in one of the following categories: Substantial deficit, Moderate deficit, Slight deficit, or Optimal. Each athlete was re-tested with the aforementioned protocol after they completed the eight-week training program.
Training Sessions
After their initial Move2Perform category was identified, each athlete received corrective exercise strategies based upon their FMS™ and YBT™ scores regardless of their category. Corrective exercise prescription was based upon the hierarchy of the Functional Movement Systems model in which deficits in symmetry, mobility, and stability were identified and ranked. Once those areas of deficit were identified each athlete received their three individualized corrective exercise strategies to perform as part of their warm-up and cool-down during the training program.
Athletes participated in an eight-week group program which included supervised sessions, two days per week. Each session consisted of each athlete's corrective exercises, a functional warm-up based on the FIFA 11+, three 20-minute circuits that included jump training, core strengthening, and agility training, and a cool-down consisting of each athlete's corrective exercises. The program followed a structured progression with each circuit increasing in difficulty and complexity of movement pattern over the course of eight weeks. See Appendix 1 for more detailed description of the program.
Statistical Methods
The primary outcome for this study was change in risk category. Significant changes in the four risk categories (Substantial, Moderate, Slight, and Optimal) were determined using a Wilcoxon Signed Ranks Test with significance set at 0.05. An additional analysis was performed using a modified risk cutoff based on the results from Lehr's study, which condensed Moderate and Substantial categories to a single to “High Risk” category, and Slight and Optimal to a single “Low Risk” category. Change across this risk threshold was determined using a McNemar's test, with significance set at 0.05.
RESULTS
Fifty-four athletes participated in pretest. Ten athletes did not complete the program due to financial constraints (four participants) of participation or other schedule conflicts (six participants). No injuries were sustained during participation in the program, therefore forty-four athletes were included in the final analysis.
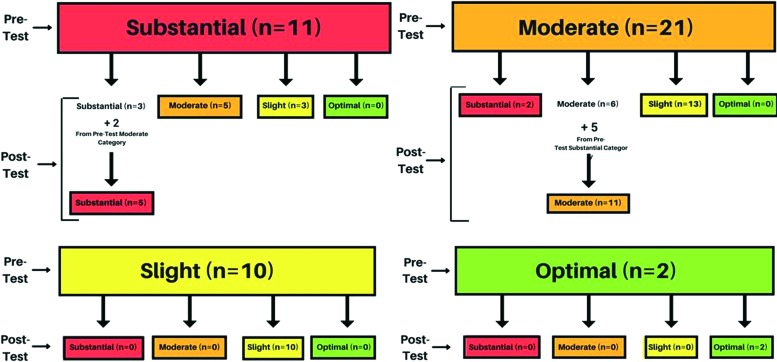
A Wilcoxon Signed Ranks test was used to determine change in risk category from pretest to posttest. Twenty-one athletes had an improved risk category (i.e. movement to a lower risk category), two athletes had decline in risk category (i.e. movement to a higher risk category), and twenty-one athletes were ties (i.e. no change in risk category). Figure 1 illustrates the movements of athletes by category at pre-test and post-test. The improvement in risk category from pretest to posttest was significant (p=0.000, Z=−3.869).
Figure 1.
Participant injury risk category movement from pre-test to post-test.
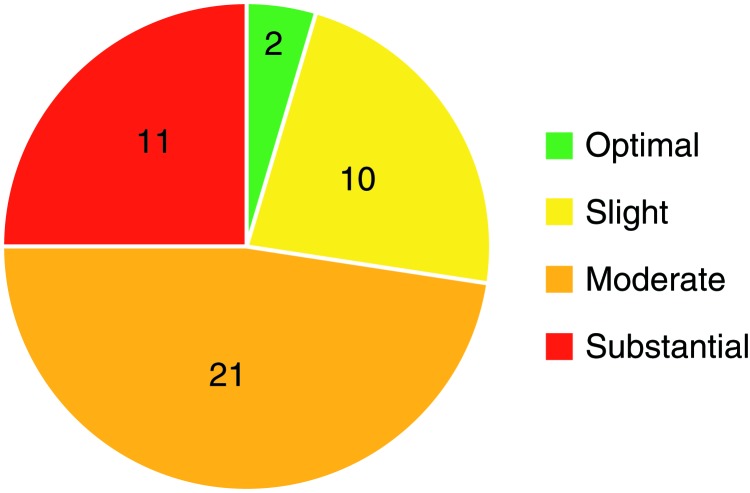
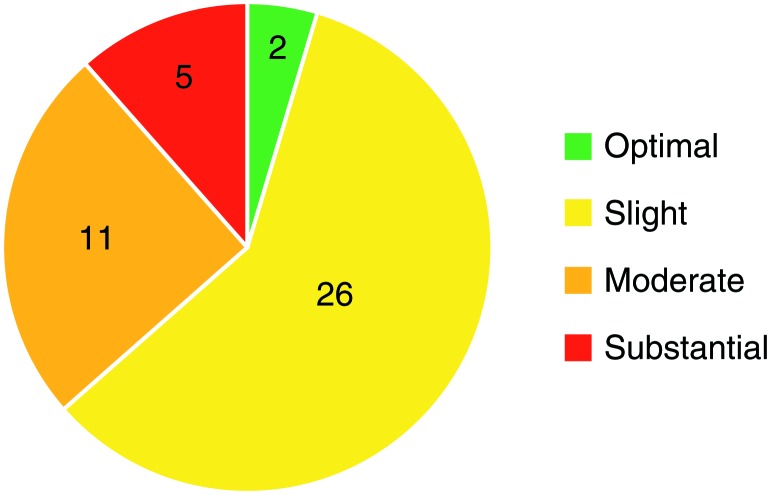
Of the forty-four athletes, thirty-two were in the High Risk (Substantial and Moderate Risk combined) category at pretest. At posttest, sixteen of the athletes in the High Risk category had moved to the Low Risk (Slight and Optimal Risk combined) category. More specifically, at pre-test there were 11 athletes in the Substantial Risk category and five remained at post-test, 21 athletes in Moderate category at pre-test and 11 remained at post-test, and there were 10 athletes in Slight category and two in Optimal category at pre-test which remained in their measured category at post-test. The results of the McNemar's analysis revealed that the number of High Risk athletes moving to the Low Risk category was significant (p<0.000; see Table 1). Figures 2 and 3 indicate the total number of participants in each risk category at pretest and at posttest.
Table 1.
2×2 table calculated with McNemar's analysis demonstrating significant movement of participants in the High Risk group pretest to the Low Risk group at posttest.
| Posttest | ||||
|---|---|---|---|---|
| High Risk | Low Risk | Total | ||
| Pretest | High Risk | 16 | 16* | 32 |
| Low Risk | 0 | 12 | 12 | |
| Total | 16 | 28 | 44 | |
= statistically significant difference at p = 0.0002
Figure 2.
Participant total per category at pre-test.
Figure 3.
Participant total per category at post-test.
DISCUSSION
The purpose of this retrospective study was to determine if injury risk category as defined by Move2Perform is modifiable. It has been suggested in previous research that categorizing athletes with efficient screening tools allows for prioritization of prevention strategies.4 To the authors’ knowledge, this is the first study to look at the ability to change Move2Perform injury risk category based on an injury prevention training program and/or individualized treatment. The program in this study utilized an individualized group intervention strategy, which included individualized corrective exercises based on FMS™ and YBT™ scores, jump training, agility drills and core strengthening. The results of this study showed that nearly 48% of athletes moved to a lower risk category following intervention. This finding is consistent with previous intervention studies looking at interventions to improve either the FMS™ or the YBT-LQ™.6-14 Therefore, an individualized group injury prevention program can be beneficial in not only improving performance on the FMS™ and YBT-LQ™, but may alter risk category as well.
Using Lehr's modified categories, 50% of athletes in the High Risk category moved to Low Risk at posttest. While this change is statistically significant, its clinical relevance is likely more important. Athletes in the High Risk category have been reported to be 3.4 times more likely to sustain an injury compared to their Low Risk peers per Lehr et al,4 therefore crossing the threshold from the High Risk to Low Risk category may decrease injury risk but this needs to be studied further. Movement within groups was primarily seen in the athletes who were in the Moderate risk category at pre-test. Sixty-two percent (13 athletes) of the Moderate Risk pre-test athletes moved into the Slight Risk category at post-test which was a statistically significant change (p<0.0001). The researchers believe this holds clinical significance as well, by demonstrating the ability for a clinician to triage the Moderate risk athletes into a group training program in order to potentially decrease their injury risk level. The clinical application would include utilizing the pre-testing protocol and injury risk categorization, then enrolling athletes that are in either the Moderate, Slight, or Optimal injury risk categorization into an individualized group training program like the one this study describes. By following that protocol at pre-season, the remaining athletes in the Substantial Risk category would be able to have more individualized assessment and treatment which would in turn lessen the burden on the clinicians triaging care.
Athletes that are categorized in Substantial Risk are in that category due to current injury, current pain, and/or substantially poor movement competency. Basic movement competency means an athlete is able to exhibit a full array of range of motion, body control and movement awareness in various postures. All three of these characteristics are major risk factors for subsequent time-loss injury. The authors hypothesized the Substantial Risk category athletes would not see enough injury risk factor reductions from implementation of a group injury prevention training program (albeit a partially individualized program) because the program was too high level for the demonstrated movement competency, and/or athletes were experiencing pain at pre-test, and/or athletes were currently injured at pre-test. There were three outliers that did move from Substantial Risk to Slight Risk category. Looking at each of those athlete's pre-test information compared to their post-test, there was not a clear pattern of why those individuals improved and others in Substantial category did not. Two of the athletes had pain at pre-test in the upper extremity that they did not report at post-test which allowed for a decrease in a significant risk factor. The other athlete was able to demonstrate improved YBT-LQ™ composite scores and cleared asymmetries within the FMS™ which allowed for movement to a lower risk category. The movement between categories of those three athletes was not statistically significant. Future research with a larger sample size may shed more light on if an individualized group training program does in fact modify the Substantial Risk athlete's category similarly to the decrease seen in the Moderate Risk group. At this time the authors’ recommendation for the Substantial Risk athlete's care would be to have more formalized assessment of the risk factors causing the athlete to be rated as substantial and then for each athlete to receive individualized treatment.
There were a few limitations identified by the authors. One limitation of this study is the lack of control group, which precludes a clear cause/effect relationship as no randomization occurred. Thus, it also cannot be determined the relative contribution of each of the parts of the intervention to changing risk category. A second limitation was a lack of control of co-interventions which may have influenced the outcomes of the study. Although the authors have no reason to believe this impacted the results of the study, the participants may have received additional interventions such as personal training, weight lifting, massage and/or chiropractic care. There also was no short-term or long-term follow-up to identify if the change in injury risk category was maintained over time. And finally, due to the retrospective nature of this study, full demographic data (height and weight) on the participants was not obtained. Additional research should focus on the maintenance of injury risk categories and the actual injury risk reduction occurred once an individual's category has been modified.
Although the specific results of this study cannot be generalized beyond the population tested, matching Moderate, Slight and Optimal Risk category athletes with a standard individualized group injury prevention program appears to do no harm and significantly benefit those in the Moderate Risk category. Matching the Substantial Risk category athletes with an individualized treatment program may also allow ideal allocation of available resources in the high school athletic training room to the individuals that need it the most. Therefore, it will be beneficial to perform additional studies with a larger sample size to increase the external validity as well as confirm the broad use of this injury prevention method.
CONCLUSIONS
The results of the current study indicate that an athlete's injury risk category can be altered; however, the strategy to implement is dependent on the athlete's initial risk category. Group injury prevention training programs can be utilized to change the injury risk category in athletes who are categorized as either Optimal, Slight or Moderate, but a more individualized approach may be needed for athletes that fall in the Substantial risk category. Utilizing the Move2Perform algorithm can be beneficial during pre-participation physicals to identify an athlete's injury risk category and also provide a good filtering system for utilization of injury prevention resources.
References
- 1.Darrow CJ Collins CL Yard EE Comstock RD. Epidemiology of severe injuries among United States high school athletes: 2005-2007. Am J Sports Med. 2009;37(9):1798-1805. [DOI] [PubMed] [Google Scholar]
- 2.Aman M Forssblad M Henriksson-Larsén K. Insurance claims data: a possible solution for a national sports injury surveillance systemϿ. An evaluation of data information against ASIDD and consensus statements on sports injury surveillance. BMJ Open. 2014;4(6):e005056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Noyes FR Barber Westin SD. Anterior cruciate ligament injury prevention training in female athletes: a systematic review of injury reduction and results of athletic performance tests. Sports Health. 2012;4(1):36-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lehr ME Plisky PJ Butler RJ Fink ML Kiesel KB Underwood FB. Field-expedient screening and injury risk algorithm categories as predictors of noncontact lower extremity injury. Scand J Med Sci Sports. 2013;23(4):e225-e232. [DOI] [PubMed] [Google Scholar]
- 5.Hewett TE Myer GD Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492-501. [DOI] [PubMed] [Google Scholar]
- 6.Chorba RS, Chorba DJ, Bouillon LE, Overmyer CA, Landis JA. Use of a functional movement screening tool to determine injury risk in female collegiate athletes. N Am J Sports Phys Ther. 2010;5(2):47-54. [PMC free article] [PubMed] [Google Scholar]
- 7.O'Connor FG Deuster PA Davis J Pappas CG Knapik JJ. Functional movement screening: predicting injuries in officer candidates. Med Sci Sports Exerc. 2011;43(12):2224-2230. [DOI] [PubMed] [Google Scholar]
- 8.Cook G Burton L Hoogenboom B. Pre-participation screening: the use of fundamental movements as an assessment of function - part 2. N Am J Sports Phys Ther. 2006;1(3):132-139. [PMC free article] [PubMed] [Google Scholar]
- 9.Teyhen DS Shaffer SW Lorenson CL, et al. The Functional Movement Screen™: a reliability study. J Orthop Sports Phys Ther. 2012;42(6):530-540. [DOI] [PubMed] [Google Scholar]
- 10.Schneiders AG Davidsson Å Hörman E. Functional movement screen™ normative values in a young, active population. Int J Sports Phys Ther. 2011;6(2). [PMC free article] [PubMed] [Google Scholar]
- 11.Minick KI Kiesel KB Burton L Taylor A Plisky P Butler RJ. Interrater reliability of the Functional Movement Screen™. J Strength Cond Res. 2010;24(2):479-486. [DOI] [PubMed] [Google Scholar]
- 12.Plisky PJ Rauh MJ Kaminski TW Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36(12):911-919. [DOI] [PubMed] [Google Scholar]
- 13.Gribble PA Terada M Beard MQ, et al. Prediction of lateral ankle sprains in football players based on clinical tests and body mass index. Am J Sports Med. 2016;44(2):460-467. [DOI] [PubMed] [Google Scholar]
- 14.Gribble PA Hertel J Plisky P. Using the Star Excursion Balance Test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train. 2012;47(3):339-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Butler RJ Lehr ME Fink ML Kiesel KB Plisky PJ. Dynamic balance performance and noncontact lower extremity injury in college football players: an initial study. Sports Health. 2013;5(5):417-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith CA Chimera NJ Warren M. Association of y balance test reach asymmetry and injury in division I athletes. Med Sci Sports Exerc. 2015;47(1):136-141. [DOI] [PubMed] [Google Scholar]
- 17.Herrington L Hatcher J Hatcher A McNicholas M. A comparison of Star Excursion Balance Test reach distances between ACL deficient patients and asymptomatic controls. Knee. 2009;16(2):149-152. [DOI] [PubMed] [Google Scholar]
- 18.Hertel J Braham RA Hale SA Olmsted-Kramer LC. Simplifying the star excursion balance test: analyses of subjects with and without chronic ankle instability. J Orthop Sports Phys Ther. 2006;36(3):131-137. [DOI] [PubMed] [Google Scholar]
- 19.Plisky PJ Gorman PP Butler RJ Kiesel KB Underwood FB Elkins B. The reliability of an instrumented device for measuring components of the star excursion balance test. N Am J Sports Phys Ther. 2009;4(2):92-99. [PMC free article] [PubMed] [Google Scholar]
- 20.Delahunt E Chawke M Kelleher J, et al. Lower limb kinematics and dynamic postural stability in anterior cruciate ligament-reconstructed female athletes. J Athl Train. 2013;48(2):172-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Frohm A Heijne A Kowalski J Svensson P Myklebust G. A nine-test screening battery for athletes: a reliability study. Scand J Med Sci Sports. 2012;22(3):306-315. [DOI] [PubMed] [Google Scholar]
- 22.Bonazza NA Smuin D Onks CA Silvis ML Dhawan A. Reliability, validity, and injury predictive value of the Functional Movement Screen™: A systematic review and meta-analysis. Am J Sports Med. 2017;45(3):725-732. [DOI] [PubMed] [Google Scholar]
- 23.Mokha M Sprague PA Gatens DR. Predicting musculoskeletal injury in national collegiate athletic association division II athletes from asymmetries and individual-test versus composite Functional Movement Screen™ scores. J Athl Train. 2016;51(4):276-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cosio-Lima L Knapik JJ Shumway R, et al. Associations between Functional Movement Screening™, the Y Balance Test™, and injuries in Coast Guard training. Mil Med. 2016;181(7):643-648. [DOI] [PubMed] [Google Scholar]
- 25.Gonell AC Romero JAP Soler LM. Relationship between the Y Balance Test scores and soft tissue injury incidence in a soccer team. Int J Sports Phys Ther. 2015;10(7):955-966. [PMC free article] [PubMed] [Google Scholar]
- 26.Moran RW Schneiders AG Mason J Sullivan SJ. Do Functional Movement Screen™ (FMS™) composite scores predict subsequent injury? A systematic review with meta-analysis. Br J Sports Med. 2017;51(23):1661-1669. [DOI] [PubMed] [Google Scholar]
- 27.Kiesel K Plisky P Voight M. Can serious injury in professional football players be predicted by the Functional Movement Screen™? North American Journal of Sports Physical Therapy. 2(August 2007):147-158. [PMC free article] [PubMed] [Google Scholar]
- 28.Bodden JG Needham RA Chockalingam N. The effect of an intervention program on Functional Movement Screen™ test scores in mixed martial arts athletes. Journal of Strength and Conditioning. 2015;29(1):219-225. [DOI] [PubMed] [Google Scholar]
- 29.Steffen K Emery CA Romiti M, et al. High adherence to a neuromuscular injury prevention programme (FIFA 11+) improves functional balance and reduces injury risk in Canadian youth female football players: a cluster randomised trial. Br J Sports Med. 2013;47(12):794-802. [DOI] [PubMed] [Google Scholar]
- 30.Padua DA Frank B Donaldson A, et al. Seven steps for developing and implementing a preventive training program: lessons learned from JUMP-ACL and beyond. Clin Sports Med. 2014;33(4):615-632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lindblom H Waldén M Carlfjord S Hägglund M. Implementation of a neuromuscular training programme in female adolescent football: 3-year follow-up study after a randomised controlled trial. Br J Sports Med. 2014;48(19):1425-1430. [DOI] [PubMed] [Google Scholar]
- 32.Rössler R Donath L Verhagen E Junge A Schweizer T Faude O. Exercise-based injury prevention in child and adolescent sport: a systematic review and meta-analysis. Sports Med. 2014;44(12):1733-1748. [DOI] [PubMed] [Google Scholar]
- 33.Sekulic D Uljevic O Peric M Spasic M Kondric M. Reliability and factorial validity of non-specific and tennis-specific pre-planned agility tests; preliminary analysis. J Hum Kinet. 2017;55:107-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bizzini M Junge A Dvorak J. The “11+” Manual: A complete warm-up programme to prevent injuries. http://www.yrsa.ca/pdf/Fifa11/11plus_workbook_e.pdf.
- 35.Haff GG Triplett NT. Essentials of Strength Training and Conditioning 4th Edition. Human Kinetics; 2015. [Google Scholar]