Abstract
Background
The goal of therapeutic exercise is to facilitate a neuromuscular response by increasing or decreasing muscular activity in order to reduce pain and improve function. It is not clear what dosage of exercise will create a neuromuscular response.
Purpose
The purpose of this study was to assess the effects following a three-week home program of a daily single exercise, the prone horizontal abduction exercise (PHA), on neuromuscular impairments of motor control as measured by scapular muscle EMG amplitudes, strength, and secondarily outcomes of self-reported pain and function between individuals with and without subacromial pain syndrome.
Study Design
Prospective Case-Control, Pilot Study
Methods
Twenty-five individuals participated; eleven with shoulder pain during active and resistive motions (Penn Shoulder Score: 77 ± 11) and 14 matched healthy controls (Penn Shoulder Score: 99 ± 27) (p < 0.001). Participants underwent baseline and follow up testing at three weeks including surface electromyography (EMG) of the serratus anterior, upper, and lower trapezius of the involved (painful group) or matched shoulder (control group) during an elevation task and maximal isometric shoulder strength testing. All participants were instructed in a PHA exercise to be performed daily (3 sets; 10 reps). Subjects logged daily exercise adherence. Neuromuscular adaptations were defined by changes in EMG amplitudes (normalized to MVIC) of serratus anterior, upper trapezius, and lower trapezius and strength. Secondary outcomes of self-reported pain and function were also compared between groups following the three-week intervention.
Results
After three weeks of a daily PHA exercise, the painful group demonstrated a greater decrease in baseline-elevated EMG amplitudes in the lower trapezius by 7% (95%CI 2.6-11%) during the concentric phase of the overhead lifting task (p 0.006). EMG amplitudes of the healthy control group did not change at three-week follow-up. Additionally, the change in serratus anterior mean EMG amplitude in the painful group -1.6% (IQR -22.9 to 0.8%) was significantly greater (p 0.033) than the healthy group change score, 2.5% (IQR -2.3 to 5.7%) during the eccentric phase (p 0.034). While the painful group was weaker in abduction and flexion at baseline and at follow up, both groups had a significant increase in all strength measures (p≤0.014). Concurrent with increased strength and normalizing EMG amplitudes, the painful group significantly improved on the Penn Shoulder Score with a mean change 9.8 points (95%CI 7.0, 12.6) (p < 0.001).
Conclusion
In this pilot case-control study, a single home exercise performed daily for three weeks demonstrated neuromuscular adaptations with improvements in muscle activity and strength. These were concurrent with modest, yet significant improvements pain and function in individuals with mild rotator cuff related shoulder pain.
Level of Evidence
3
Keywords: Electromyography, impingement, muscle strength, rehabilitation, subacromial pain
INTRODUCTION
Abnormal scapular kinematics and altered scapular muscle electromyographic activation levels during humeral elevation are associated with rotator cuff related shoulder pain.1-4 Decreased or excessive scapular upward rotation are commonly reported scapular motion alterations.4,5 However, there are challenges to clinicians’ ability to reliably identify specific alterations leading to refined scapular dyskinesis tests that indicate presence or absence of alterations in scapular motion.6-8 Corresponding to these altered scapular biomechanics during shoulder elevation are alterations in motor control, as evidenced by abnormal electromyographic (EMG) activity of scapular musculature in individuals with rotator cuff related shoulder pain relative to normal controls.1 Motor control impairments likely contribute to abnormal scapular motion and rotator cuff related shoulder pain. These motor control impairments appear to include the relative balance of scapular muscles, such as increased activation of the upper trapezius and altered activation and onset timing in the lower trapezius and serratus anterior muscles.9-14
Exercise programs that not only focus on scapular muscle strengthening, but emphasize motor control, including quality of movement and timing, have been advocated for the treatment of individuals with subacromial pain syndrome and included in shoulder sports injury prevention programs.5,9,12,15 Prior work from De May, et al.16 found that an intervention consisting of four scapular focused exercises over a six-week period in overhead athletes with subacromial pain resulted in a clinically and statistically significant improvement in self-reported pain and function measured by the shoulder pain and disability index.16,17 Furthermore, changes in motor control were also found with reduced EMG amplitudes in the upper trapezius during elevation and onset timing of lower trapezius and serratus compared to upper trapezius.16 Thus, improvements in pain and function appear to be related to changes in scapular muscle motor control following a six-week exercise program. However, it is not known if strength improvements occurred simultaneously as this was not a variable reported in the DeMay et al.16 study. The prone humeral horizontal abduction (PHA) exercise was one of the four exercises included in their study.
The PHA exercise has been consistently included in many shoulder rehabilitation and shoulder sports injury prevention programs.9,18-21 The PHA has demonstrated greater scapular kinematic changes in upward rotation, posterior tilt, and external rotation compared to the resting position18 and high activation levels of both posterior scapular and rotator cuff musculature.16,22-24 While DeMay et al.16 showed changes following six weeks of training, neuromuscular adaptations can occur in as few as two to three weeks prior to physiological muscle change including hypertrophy.25
Ultimately, common goals of rehabilitation for patients including athletes with shoulder pain are to improve function and reduce pain. Exercise has been proposed as an effective intervention to achieve these goals. However, patients often struggle with adhering to home exercise regimens due to multiple barriers such as low physical activity, time, lack of understanding, or poor self-efficacy.26 27 Clinicians are frequently faced with the dilemma of which exercises to prescribe to achieve the rehabilitation goals without over-burdening the patient. Perhaps only one exercise targeting scapular and rotator cuff strength may be effective as a home program to improve impairments in neuromuscular control, pain, and function in individuals with subacromial pain. Early perceived positive changes in pain, function and/or impairments have been shown to facilitate better outcomes over the course of physical therapy treatment.28,29 Furthermore, if a simple intervention results in perceivable improvements in just a few weeks, then patients may be willing to accept a more comprehensive intervention. Therefore, the purpose of this study was to conduct a pilot study to assess the effects following a three-week home program of a daily single exercise, the PHA, on neuromuscular impairments of motor control as measured by scapular muscle EMG amplitudes, strength, and secondarily outcomes of self-reported pain and function between individuals with and without subacromial pain syndrome. The authors hypothesize that greater changes in neuromuscular impairments as measured by scapular muscle EMG amplitudes and force generated with strength tests, as well as a improvement in secondary measures of pain and function, will be greater in the painful shoulder group following a three-week program of a daily bout of a single exercise, the PHA.
METHODS
Participants
Twenty-five adults volunteered to participate in this prospective case-control study. Participants were recruited as a sample of convenience from the university community. Eleven individuals with rotator cuff related shoulder pain (painful group) and 14 healthy participant case-controls (healthy group) were recruited (Table 1). All participants signed a University Institutional Review Board approved written informed consent prior to initiating test procedures.
Table 1.
Mean ( ± standard deviation) participant demographics and PENN Shoulder Score.
| All Participants (n = 25) | Healthy Group | Painful Group | Group Comparison (p-value) | |
|---|---|---|---|---|
| Gender | 0.231 | |||
| Men | 10 | 7 | 3 | |
| Women | 15 | 7 | 8 | |
| Age (yrs) | 30 ± 9 | 28 ± 6 | 33 ± 12 | 0.16 |
| Height (cm) | 171 ± 8 | 173 ± 6 | 170 ± 10 | 0.39 |
| Weight (kg) | 72 ± 13 | 74 ± 16 | 71 ± 8 | 0.68 |
| PENN Shoulder Score | 90 ± 13 | 99 ± 2 | 77 ± 11 | <0.001* |
Statistically significant difference between groups
Participants from either group were excluded if they were for any reason unable to perform the PHA shoulder exercise, had allergies to adhesive, neurological disorders or positive findings on an upper quarter myotomal or dermatomal screen other than reduced shoulder strength, limitations in shoulder passive range of motion (other than limitations in internal rotation or horizontal adduction characteristic of posterior shoulder tightness), or a history of neck or shoulder fracture or surgery. Participants in the painful group were included if shoulder pain was reproduced during active, passive or resistive shoulder motion with a clinical exam. Specifically participants were included if one of passive tests, the Hawkins and/or Neer impingement signs, were positive and pain was reproduced with resisted abduction or external rotation or a painful arc was present during active abduction. Painful participants were excluded if the shoulder pain was greater than a 7/10 on the numeric pain rating scale so that strengthening would be tolerated30 or passive range of motion was limited. Healthy participants were recruited if they had no complaints of shoulder or neck pain within the last six months and included if they had no reproduction of pain during active, passive shoulder range of motion in all planes (sagittal, coronal, transverse) or resisted shoulder motion in abduction, flexion or internal/external rotation at 90 degrees of abduction. Also participants had to demonstrate normal cervical spine range of active motion in all planes without pain. Participants in the painful group were not currently seeking treatment. Healthy participants were matched by sex and hand dominance of the shoulder tested to those in the painful group.
As part of the inclusion/exclusion process, all patients’ cervical and shoulder mobility were evaluated using standard clinical measures of active, passive, and resistive range of motion. Scapular dyskinesis testing was performed as described previously, with five repetitions of abduction and flexion while holding a three- or five-pound weight.7 The test was considered positive if obvious dyskinesis, noted by winging, excessive elevation or protraction, or dysrhythmia during arm elevation or lowering.7 The clinical screening examination included a neurological upper quarter myotomal and dermatomal screen, rotator cuff testing to rule out large/massive rotator cuff tears with drop arm, external rotation lag and horn blowers signs,31 Neer and Hawkins impingement tests, presence or absence of the sulcus sign, anterior-posterior drawer, and apprehension testing.32-34 All testing was completed by a licensed physical therapist.
All participants completed a physical activity readiness questionnaire, a medical history questionnaire, and the Penn Shoulder Score during baseline evaluation. The Penn Shoulder Score is a validated, self-reported, regional disability scale from zero to 100 points. One hundred points is a perfect score indicating no pain, high satisfaction, and normal function. The Penn Shoulder Score has strong reliability and a minimal detectable change score of 12 points.35 The Penn Shoulder Score was administered at baseline testing and after the three-week intervention.
Procedures
Participants attended two sessions three weeks apart and underwent the same procedures on both sessions. Scapular neuromuscular activity of the upper trapezius, lower trapezius, and serratus anterior was measured via surface EMG during the arm elevation task. The participants’ skin was prepared for surface electrode placement, shaved if needed, lightly debrided with fine sandpaper, and cleaned with alcohol. Bipolar surface electrodes (Blue Sensor; Glen Burnie, MD) were placed parallel to the muscle fibers with a two-centimeter inter-electrode distance on the serratus anterior,36 upper portion of the trapezius37 and lower portion of the trapezius38 (Table 2). A surface ground electrode was placed on the contralateral acromion process. An electrogoniometer (SG110, Biometrics, Ladysmith, VA, USA) was placed on the shoulder, across the scapular spine and distal to the deltoid, to capture arm elevation motions. The EMG channel and electrogoniometer leads were connected to a portable amplifier (Run Technologies, Mission Viejo, CA). Electrode placement was visually confirmed with resisted contractions of the instrumented muscles while verifying the EMG activity with an oscilloscope. The EMG amplitudes of each muscle were recorded while standing with the arms at the side.
Table 2.
Electrode Placement and MVIC/strength test positions.
| EMG collected | Electrode Location | MVIC/Strength test position |
|---|---|---|
| Upper Trapezius | A mark was made on the skin at the midpoint on a line joining the C7 spinous process and tip of the posterior lateral angle of the acromion. The electrodes were placed over a point 1/2 distance between this point and the posterior lateral angle of the acromion37 |
Abduction: The participant abducted his/her arm to 90 ° with thumb pointing up. The hand held dynamometer was applied just proximal to the elbow with the participant sitting upright. The participant abducted his/her arm up against resistance applied through the humerus |
| Lower Trapezius | The arm was elevated in abduction to 125 ° and the electrodes were placed at the midpoint from the T7 spinous process to the inferior angle of the scapula in line with muscle fibers obliquely superior and laterally38 |
Prone Elevation: In a prone position, the participant abducted his/her arm to 125 ° with thumb up. Subject was asked to push up against the hand held dynamometer that was placed on distal arm just proximal to the radial styloid. |
| Serratus Anterior | With the arm elevated to 125 ° the electrodes were places over the 7th intercostal space, just anterior to the fibers of the latissimus dorsi in line with the serratus anterior muscle fibers36 |
Flexion: With subject seated, resistance was applied with the hand held dynamometer to distal arm proximal to the wrist in a perpendicular direction with the humerus elevated to 125 ° in the sagittal plane |
The EMG amplitude data were collected during maximum voluntary isometric contractions (MVIC) in order to compare amplitude data for the task of interest between participants. In order to obtain strength measures, a hand-held dynamometer (JTech Commander, Midvale UT) was used during all MVIC testing. Participants performed two five-second MVICs for each scapular muscle, using standardized test positions in randomized order (Table 2).21,39-41 Participants were familiarized with the MVIC procedure by first performing a submaximal practice trial for each isometric make test performed. Strength, defined as peak force generated, was simultaneously recorded with hand held dynamometer during the MVICs. Participants were given one-minute of rest between trials. To assist with determining maximal effort, the output of the two maximal effort trials had to be within 10% of each other. Additional trials were captured until two highest values were within 10%. The average maximal force (kg) produced during the two maximal trials (MVIC) was calculated and then normalized to each subject's body weight (kg) to yield strength as a % body weight. Three strength tests/MVIC positions were performed: shoulder abduction with the arm at 90 °, prone elevation with the arm at 125 ° of abduction, and seated shoulder flexion at 125 ° (Table 2). MVIC EMG value used for normalization was determined based on highest recorded EMG amplitude regardless of test position, due to the synergy between these muscles.42
Arm elevation task
Each participant was asked to perform ten repetitions of weighted bilateral elevation in the scapular plane as previously described.7,16 The amount of weight used was based on the participant's body weight. Participants with a body weight less than 150 pounds (68 kg) used three-pound weights, (1.4kg) and those with a body weight equal or greater than 150 pounds (68kg) used five-pound (2.3kg) weights. The weights were held in each hand, and EMG data was collected during arm elevation. A metronome was used to control the rate of elevation; a full elevation cycle was achieved in a four second count with two second count for maximal concentric elevation and two second count for eccentric lowering. Practice trials were provided to achieve the desired rate and range of motion of arm elevation.7 EMG activity was recorded during the entire duration of the elevation trials.
Prone Horizontal Abduction Exercise Intervention
The PHA is a commonly used exercise in both preventive and rehabilitation interventions.15,29,43 Participants were instructed to perform a prone horizontal abduction (PHA) exercise with verbal and tactile feedback to ensure correct performance. The therapist positioned and supported the participant's arm in the PHA position (abduction to 100 ° with external rotation) while manually guiding the scapula into depression and retraction as a cue for the desired scapular movement with the exercise. Verbal cues to fully externally rotate the humerus, to tip scapula back and downwards, and to avoid a shrugging motion were also provided. Tactile feedback with tapping was provided to the lower trapezius to facilitate activation.44 The participant was then asked to demonstrate the full exercise while additional verbal and tactile feedback was provided. The efficacy of this exercise instruction on scapular muscle activity has been previously demonstrated.44 Once proper technique was achieved, the participant was asked to perform three sets of ten repetitions daily at home. Participants were provided with a weight to use at home that was equal to two percent of his or her bodyweight, as adapted from De Mey, et al.16 Additionally, participants were given written instructions that described how to perform the PHA exercise and an exercise log to record daily exercise adherence.41
EMG Data Processing
A 16-channel EMG system (Run Technologies, Mission Viejo, CA) was used to record muscle activity. All raw EMG data were transmitted at 2000 Hz via a fiber optic cable through a Myopac transmitter unit (Run Technologies, Mission Viejo, CA) to the receiver unit. Unit specifications for the Myopac included a common mode rejection ratio (CMRR) of 90 dB, an amplifier gain of 2000 for the surface EMG electrode, and an amplifier gain of 1000 for the electrogoniometer. Using Datapac 5 software (Run Technologies, Mission Viejo, CA), all raw EMG data were processed digitally with a passive demeaning filter to correct for a DC offset. All raw EMG data had a high pass fourth order finite impulse response filter set at 10.0 Hz, then were full-wave rectified. Finally, a low pass cut-off of 6.0 Hz with a fourth order Butterworth filter was used to smooth the data.41
The MVIC was determined by identifying the highest 500ms window of EMG activity during the two five-second maximal isometric trial for each muscle tested. The highest 500ms of EMG activity recorded during resting was subtracted out of all MVIC and exercise recorded EMG activity as background noise.45 The mean EMG amplitudes were normalized to the MVIC EMG amplitudes to represent mean muscle activity. The electrogoniometer was used to identify two, concentric and eccentric, phases of the elevation task. The reproducibility of the experimental procedure and EMG data processing was good to excellent as previously established.46 Trials four through eight were averaged for each phase separately to represent each participant's mean EMG amplitude during the elevation task. This processing was performed to derive mean EMG concentric and eccentric EMG amplitudes for each muscle at baseline and discharge to be used for statistical analyses.
Statistical Analysis
As data were obtained to generate preliminary estimates of changes in neuromuscular adaptations in this pilot case-control study, no a priori sample size analysis was performed to determine statistical power to detect between group differences in treatment effects. All data were evaluated for normality using the Shapiro-Wilk test of normality and Q-Q plot. Chi-square and independent t-tests were used to compare baseline group participant demographics and three-week follow up self-reported adherence to the daily PHA exercise as a proportion of days completed. To determine the effects of a three-week single PHA exercise home program on changes in neuromuscular adaptations during the active elevation task and shoulder strength between groups, separate 2x2 repeated-measures ANOVAs were used to evaluate change between groups over time in mean EMG amplitudes (concentric; eccentric phases of elevation task) in the lower trapezius, upper trapezius and normalized maximal strength (% body weight) in abduction, flexion, and prone elevation. The within participant factor was time (baseline, three-week follow up) and the between-participants factor was group (painful, healthy). In the event of statistical significance, post-hoc testing was performed using pairwise comparisons and a Bonferroni corrected alpha. To evaluate differences over time between groups in the Penn Shoulder Score and serratus anterior mean concentric and eccentric EMG amplitudes during the elevation task, separate non-parametric Mann-Whitney U tests were performed to compare change scores from baseline to discharge between the two groups (healthy and painful) due to the non-normal distribution of these data. Alpha was set at 0.05 for all analyses.
RESULTS
Eleven individuals with shoulder pain (painful group) and 14 healthy participant case-controls (healthy group) completed the study. Baseline characteristics of the two groups were not significantly different for age, height or weight (Table 1). However, as expected the painful group had lower Penn Shoulder Scores than the healthy group at baseline (p < 0.001). There were no significant differences (p 0.581) in the proportion of self-reported adherence to the daily PHA exercise between the painful group (83.1%) and the healthy group (79.1%). However, only 8/11 (72%) subjects in the painful group and 9/14 (64%) subjects the healthy control group returned the compliance log.
There was a significant group by time interaction (p = 0.045) with the lower trapezius muscle during the concentric phase of arm elevation. The painful group demonstrated greater lower trapezius EMG amplitudes at baseline, and a significant (p 0.006) 7% (95%CI 2.6-11%) mean reduction in EMG amplitudes at three-week follow-up compared to no change (p>0.05) in the healthy group. Similar results were found in lower trapezius EMG amplitudes during the eccentric phase. During eccentric phase arm elevation task, the painful group had greater EMG amplitude in the lower trapezius muscle at baseline. The reduction in EMG amplitude at follow up did not reach statistical significance for the time x group interaction (p 0.081). However, there was a statistically significant main effect of group given the higher baseline and follow up eccentric lower trapezius EMG amplitudes in the painful group (5.8%; 95%CI 2.1-9.5%) across both time points (p 0.004) (Table 3).
Table 3.
Results of change in EMG amplitudes as percentage of MVIC.
| Healthy Group (n 14); Painful Group (n 11) | Baseline EMG Amplitude | 3-week Follow up EMG Amplitude | Interaction for group x time | Post-hoc testing (p-value) |
|---|---|---|---|---|
| Concentric UT | ||||
| Healthy Group | 43 ± 12 | 41 ± 13 | 0.335 | |
| Painful Group | 55 ± 19 | 49 ± 16 | ||
| Eccentric UT | ||||
| Healthy Group | 21 ± 7 | 20 ± 10 | 0.086 | |
| Painful Group | 30 ± 17 | 23 ± 8 | ||
| Concentric LT* | ||||
| Healthy Group | 17 ± 8 | 15 ± 5 | 0.045* | 0.930 |
| Painful Group | 28 ± 12 | 21 ± 7 | 0.006† | |
| Eccentric LT‡ | ||||
| Healthy Group | 9 ± 4 | 9 ± 4 | 0.081 | |
| Painful Group | 18 ± 9‡ | 13 ± 4‡ |
= Indicates a significant group by time interaction
= indicates a significant change between baseline and 3-week follow up
= indicates a significant main effect of group (p = 0.004). The painful group had significantly greater EMG amplitude at both time points compared to the healthy group.
UT = Upper Trapezius
LT = Lower Trapezius
The upper trapezius EMG amplitudes did not demonstrate a group by time interaction in either the concentric or eccentric phases of arm elevation (p 0.33, p 0.086), respectively (Table 3). While there were trends of main effect of group (p 0.09) with the painful group demonstrating greater upper trapezius mean EMG amplitudes in both phases of elevation at baseline and follow up, this did not quite reach statistical significance in either phase (p 0.06; p 0.097). Additionally there were trends towards a main effect of time with both groups showing a mean of 3-4% decrease in upper trapezius EMG amplitudes from baseline to three week follow up, yet this did not reach significance during the concentric (p 0.067) or eccentric (p 0.092) phases, respectively.
The serratus anterior EMG amplitude change scores were calculated with a negative number indicating a reduction in EMG amplitude from baseline to three-week follow-up. Results of non-parametric Mann-Whitney U tests analyses show that during the concentric phase of arm elevation, there were similar changes in the painful group -9.4% (IQR -36.5 to 9.7%) compared to the healthy group change 3.2% (IQR -8.2 to19.8%) which were not statistically significant (p = 0.075). However, during arm lowering (the eccentric phase of the task), the change in serratus anterior mean EMG amplitude in the painful group -1.6% (IQR -22.9 to 0.8%) was significantly greater (p 0.033) than the healthy group change score, 2.5% (IQR -2.3 to 5.7%).
Results of individual 2-way repeated-measures ANOVA used to evaluate change in strength, revealed no difference in the change in maximal normalized force generated between the groups over time with a group by time interaction of p>0.59 (Table 4). However, there was a significant increase in all three strength measures in both groups demonstrating a main effect of time (p≤0.014). (Table 4) Additionally, the healthy group generated more force with strength tests in abduction (p 0.02, 3.4%; 95%CI 0.6, 6.2) and flexion (p 0.03, mean 2.6%; 95%CI 0.3, 4.9) than the painful group, across both time points. While this was true for abduction and flexion, there were no significant differences (p = 0.08); between the groups in force generated with the prone elevation at either time point (mean difference 1.8%, 95%CI -0.2, 3.7). (Table 4) Lastly, there was a significant difference in the change in the Penn Shoulder Score between groups (p < 0.001) with an improvement in the Penn Shoulder Score in the painful group by a mean of 9.8 points (95%CI 7.0, 12.6) compared to no change in the healthy group (mean change = -0.43 points; 95%CI = -2.9, 2.1).
Table 4.
The normalized strength, force generated as percent of bodyweight, at baseline and discharge.
| Healthy group (n 14) Painful group (n 11) | Baseline | 3-week Follow up | Interaction group x time (p-value) | Main effect of Time (mean difference; 95%CI; p-value) | Main effect of group (mean difference; 95%CI; p-value) |
|---|---|---|---|---|---|
| Abduction | |||||
| Healthy | 13.2 ± 3.6 | 14.5 ± 3.8 | 0.59 | 3.4% (0.6-6.2%) | |
| Painful | 9.6 ± 2.8 | 11.2 ± 3.1 | p 0.02† | ||
| Total (n 25) | 11.6 ± 3.6 | 13.1 ± 3.8 | 1.5% (0.9-2.0%) p<0.001* |
||
| Prone Elevation | |||||
| Healthy | 7.7 ± 2.7 | 9.8 ± 3.1 | 0.85 | 1.8% (-0.2 – 3.7%) | |
| Painful | 6 ± 2.2 | 8 ± 1.3 | p 0.08 | ||
| Total (n 25) | 6.9 ± 2.5 | 8.9 ± 2.6 | 2.0% (1.3-2.6%) p<0.001* |
||
| Flexion | |||||
| Healthy | 11.5 ± 3.2 | 12.5 ± 3.3 | 0.97 | 2.6% (0.3-4.9%) | |
| Painful | 8.9 ± 2.5 | 9.8 ± 2.3 | p 0.03† | ||
| Total (n 25) | 10.3 ± 3.2 | 11.3 ± 3.2 | 1.0% (0.2-1.7%) p 0.014* |
indicates significant main effect of time. Results represent change regardless of group
indicates significant main effect of group. Results represent group differences regardless of timepoint
DISCUSSION
The results of the current study suggest neuromuscular adaptations occur following a three-week program of a single exercise, PHA, performed daily in individuals with and without rotator cuff related shoulder pain. Interestingly, there appeared to be carry-over effects with changes in muscle activity (EMG amplitudes) during a functional elevation task that occurred following a daily three-week PHA exercise program, but primarily in the painful group. In the painful group, baseline mean EMG amplitudes of the lower trapezius and serratus anterior were elevated and significantly reduced following the three-week PHA exercise program in both the concentric and eccentric phases of the elevation task, respectively. Greater EMG activity in the lower trapezius and serratus at baseline in the painful group suggests greater muscle activity is required to perform the submaximal arm elevation task at baseline compared to three-week follow up testing. This decrease in muscle activity needed to perform the elevation task occurred concurrent with a modest but significant increase in shoulder strength increase following a three-week daily single exercise that targeted the posterior shoulder musculature. This supports the hypothesis that neuromuscular adaptations occurred following a three-week PHA. Furthermore, the mean lower trapezius and serratus anterior EMG amplitudes were lower at baseline and did not significantly change in the healthy control group following the three-week intervention. Concurrent with neuromuscular changes, the painful group also had a significant improvement in the Penn Shoulder Score from baseline to three-week follow up, although not beyond the minimal detectable change. Results of this pilot study are encouraging, since recent research has shown that early changes to physical therapy interventions can occur29 and are predictive of future results.28,47 The current study results indicate that individuals with rotator cuff related shoulder pain demonstrate neuromuscular adaptions following a three-week single PHA exercise program approximating mean muscle activity and strength found in healthy individuals as self-reported pain and function improves.
Neuromuscular Adaptations: EMG amplitudes
In the current study, the painful group had a significant decrease in lower trapezius and serratus anterior EMG amplitude during the arm elevation task from baseline to three-week follow up compared to the healthy control group. These changes are consistent with prior research showing neuromuscular change occurs with exercise in short-term follow up.25 The significant change found in the lower trapezius is likely due to the specificity of the exercise prescribed. Prior work has shown that the PHA exercise elicits high levels of lower trapezius activity, 59% of MVIC during the concentric phase of the exercise, compared to the serratus anterior and upper trapezius with 12.5% and 24% MVIC, respectively.22 Furthermore, the verbal and tactile exercise instruction provided at baseline was intended to facilitate greater lower trapezius muscle activity and reduce excessive upper trapezius activity during the PHA exercise. The effects of the specific verbal and tactile instruction to facilitate targeted lower trapezius muscle performance with the PHA have been previously demonstrated.44
Interestingly, there do appear to be carry-over of the effects of a PHA exercise to the elevation task, specifically with reduced lower trapezius EMG amplitudes by 7% (p 0.006) in the concentric phase at three-week follow up (Table 3). This is consistent with findings of prior research by DeMay, et al. who found a 15% reduction in lower trapezius muscle activity following a six-week scapular muscle strengthening program in individuals with subacromial pain syndrome. The current results are consistent with these prior study results with approximately half the reduction in excessive mean lower trapezius EMG activity, in only three weeks of a single PHA exercise. Furthermore, only the current pilot study included a healthy control group that had lower mean EMG activity during the elevation task at baseline that did not significantly change at follow up. Inclusion of the healthy control group also allowed the authors to evaluate change scores in the non-normally distributed serratus anterior EMG amplitudes between groups from baseline to follow up in the current study. There was a statistically significant change from baseline to discharge (p 0.033) in mean serratus anterior amplitudes during the eccentric phase of the elevation task in the painful group −1.6% (IQR -22.9 to 0.8%), compared to the healthy group. In previous research by DeMey et al,16 similar mean changes (2%) were not significant following a six-week exercise program in individuals with subacromial pain syndrome.
The relative decreases in EMG amplitudes found in the lower trapezius and serratus anterior during a functional task following a three-week strengthening program are expected can be an indication that muscular demands are diminished.16 Repeating the same arm elevation task prior to and following a training intervention, one would expect that the task would be less demanding after the intervention. Data supports this observation in the current case- control pilot study, even though statistical significant differences were not always achieved. Patients with shoulder pain were prescribed exercises that are intended to strengthen and improve motor control of the target muscles to reduce the heightened EMG activity during a submaximal functional task. In this study, the authors’ observed that a single PHA exercise altered neuromuscular activity used to perform a common task with activities of daily living that is often painful in the population with rotator cuff related pain.
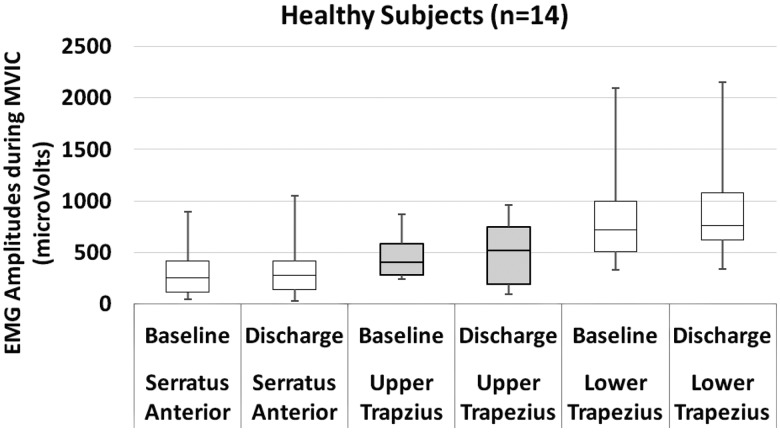
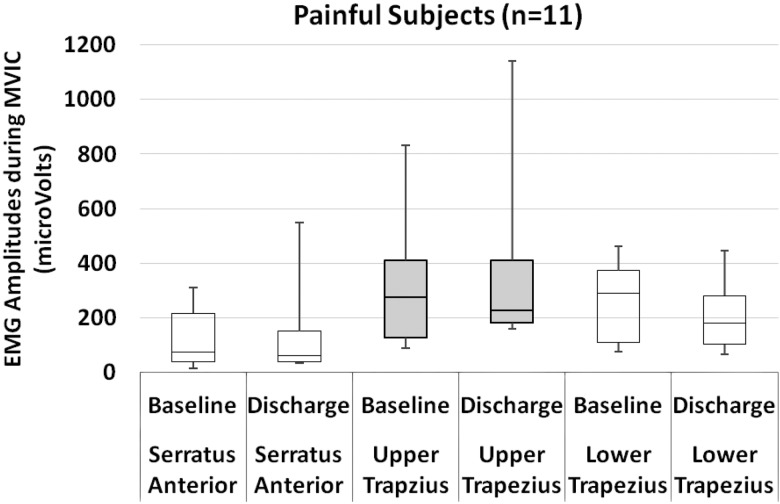
While neural adaptations may be one rationale for the reduced EMG amplitude results in the painful group, consideration must also be given to methodology used in this study that required both the painful and healthy groups to perform a maximal voluntary isometric contraction. The maximal EMG amplitude during the MVIC was used to normalize the EMG data during the functional task in both painful and healthy groups. This introduces a concern that neuromuscular changes found in the current study may not be attributed to neuromuscular adaptations in the painful group, but may be simply due to a reduction in pain with the MVIC with the follow up testing. In the current study the authors did not capture pain ratings during the MVIC in the painful group. However, to address this potential confounder, the raw EMG microvolts recorded during the MVIC that were used to normalize the EMG amplitudes for both groups at both time points were analyzed using a non-parametric Wilcoxon Signed Rank test to determine if meaningful changes occurred between testing days. As shown in Figures 1 and Figure 2, there were no significant differences between EMG amplitudes used to normalize the task EMG mean amplitude data for either group between baseline and three-week follow up (p > 0.11). Given little to no change in the MVIC EMG amplitude data between baseline and follow up in the painful group, authors suggest that changes found in the mean MVIC normalized EMG amplitudes with the elevation task can be attributed to true neuromuscular adaptations.
Figure 1.
Box plot of healthy subjects’ microvolts during maximal voluntary isometric contraction testing for elevation, abduction, and prone elevation.
Figure 2.
Box plot of painful subjects’ microvolts during maximal voluntary isometric contraction testing for elevation, abduction, and prone elevation.
Neuromuscular Adaptations: Strength
Over the three weeks of the current study revealed small but consistent and statistically significant strength gains of one to two percent bodyweight in both groups. It is known that progressive resistance exercise increases strength, but few studies relate these gains specifically to shoulder rehabilitation.48 In the current study, both healthy and painful groups demonstrated and increase in isometric maximal force production measured by a handheld dynamometer in abduction, flexion and prone elevation by 1-2% body weight. Given the mean body weight of participants in the current study (72kg; 158lbs), maximal isometric force generated in shoulder flexion gains would equate to and increase from 7.4kg to 8.1kg (16.3 to 17.8 lbs) in both groups. These results are comparable to the previously reported mean strength in shoulder flexion values in healthy adults and those with rotator cuff related shoulder pain 6.8kg to 7.7kg (15.0 to 16.9lbs).49,50 With shoulder abduction strength testing, current study results equate to an increase in maximal force generated from 8.4kg to 9.4kg (18.5 to 20.7lbs) following a three-week PHA daily exercise in both groups. The current study results provide evidence that over a short period of training, neuromuscular adaptations with both changes in muscle EMG activity and strength occur from a single shoulder exercise over a three-week period of daily training in individuals with rotator cuff related shoulder pain. This is an important finding with value-based healthcare, as clinicians search for ways to overcome the poor adherence to rehabilitation exercise.26,27,51
Self-reported Pain and Function
Pain and function were measured using the Penn Shoulder Score. The painful group showed statistically significant improvement in the Penn Shoulder Score by a mean of 9.8 points over a three-week period. A minimal detectable change of 10.7 points in patients who start with a Penn Shoulder Score above 76, has been reported to be clinically meaningful35 which is less than one point short of change in the current cohort. Similarly, with a different metric measuring shoulder function, De Mey et al 16 demonstrated an 18-point improvement on the SPADI which resulted from four exercises over a six-week period. In three weeks of a single exercise, an approximate ten percent improvement in self-reported pain and function was observed. The De Mey et al16 study examined the effects of four exercises over six weeks, which showed almost 20% improvement in self-reported function. The results of this current study demonstrate similar trends of improvement as the previous study16 and strengthen the value of the neuromuscular changes found in the painful group with a three-week PHA exercise. It appears that neuromuscular changes are also associated with early patient-centered changes in pain and function obtained with a streamlined home exercise program consisting of one exercise. This is important, because early improvement is a positive predictor of final outcomes in patients with shoulder pain.28
Rehabilitation faces the constant challenge of ensuring patient exercise adherence. 26,27 Perceived simplicity and short duration of treatment, immediacy of benefit, and absence of side effects are known factors that increase patient adherence.52 Performing only one effective exercise confronts these perceived obstacles to adherence and would benefit those patients with limited motivation and time. During the course of the current study, 17/25 participants returned their exercise logs. From the 17 logs received, it was determined that the adherence rate to the daily exercise was 68%. This is certainly on the higher end of reported compliance with home exercise programs as previous studies have found compliance to any or all of the HEP to be 60-75%.26 This assumes that individuals who did not return the exercise logs had a similar adherence rate, which is not likely. However, there were no differences between groups in the proportion who did not return logs in our study. Daily PHA exercise offers clinicians the opportunity to prescribe an intervention that may be performed without specialized equipment while also promoting functional and strength gains that match patient concerns.
A statistically significant difference was not obtained for the painful group in all outcomes measured in this study. Strong trends of improvement were observed in those that were not statistically significant in the painful cohort. This provides further evidence that a streamlined, efficient, home exercise program may improve neuromuscular impairments, self-reported function and reduce pain in individuals with mild rotator cuff related shoulder pain that were not actively seeking treatment. Prior studies have demonstrated higher adherence with a home exercise program when the program consists of fewer exercises in a military population53 (three versus six exercises) and with an elderly population54 (two compared to eight exercises). Currently, there is no evidence on the dosing necessary to achieve patient outcomes in patients with rotator cuff related shoulder pain. While the current pilot study results suggest a single exercise may result in neuromuscular changes with a home program in patients with mild pain and functional loss in three weeks, an adequately powered larger study of patients seeking rehabilitation is warranted.
There are limitations due to the nature of this pilot study case-control design. The study had a small sample of convenience, limiting the generalizability of the conclusions. The small sample also limited the authors’ ability to perform any planned subgroup analysis of adherent versus non-adherent participants. With a small sample size, the study results may also be influenced by a type II error. While statistically significant changes were not demonstrated in all of the outcome measures, trends were found in most of the other non-significant outcomes. Results certainly provide evidence of feasibility that neuromuscular adaptations may occur with a single exercise in three weeks in individuals with rotator cuff related shoulder pain and justification for future study with larger sample size. The authors did not assess whether participants were participating in a strengthening program prior to enrollment; however, individuals were asked to refrain from other upper body strength training during the three-week period. Participants in the current study with painful shoulders were mildly impaired as determined with the Penn Shoulder Score (77/100) and were not actually seeking treatment. Thus this daily three-week single exercise intervention was not tested on patients with painful shoulders seeking care. Result of the current study are however, generalizable to a younger, physically active population that are experiencing mild symptoms, which further supports the use of the PHA exercise in both rehabilitation and injury prevention programs for young adult athletes.43
CONCLUSIONS
To the authors’ knowledge, there is no evidence demonstrating the short-term effects of a single shoulder exercise on neuromuscular adaptations, specifically muscle activity and strength, as these may relate to changes in pain and function in individuals with rotator cuff related shoulder pain. Pilot studies are necessary to justify larger more costly and potentially burdensome studies in patients, particularly when feasibility, or concern for equipoise due to treatments prescribed by the clinicians may be a challenge. The modest improvements in strength and associated decreases in baseline elevated EMG amplitudes in individuals with rotator cuff related pain in this pilot study substantiates the notion that early neural adaptations can occur during the early phases (three weeks) of a rehabilitation program with a single strengthening exercise performed at home.25 Furthermore, these neuromuscular adaptations are associated with significant improvements in patient-rated outcomes measured by the Penn Shoulder Score. In the time of emerging value-based healthcare, clinicians may want consider the potential for improvements gained by one effective exercise that the patient is likely to perform, rather than many exercises that may overwhelm the patient and lead to diminished self-efficacy, adherence, and outcomes. This study provides evidence that a single exercise of PHA may be a viable treatment option in the short-term in individuals with mild pain and functional loss due to rotator cuff related shoulder pain, precipitating neuromuscular adaptations that carry over into a functional overhead lifting task. Future trials should consider comparison of neuromuscular control and patient related outcomes as it relates to exercise dosage at several time points during a course of rehabilitation to identify a typical recovery trajectory. Additionally, other factors including genetic or psychosocial phenotypes that may or may not respond to a streamlined home program may impact study results warranting further study.
REFERENCES
- 1.Phadke V Camargo P Ludewig P. Scapular and rotator cuff muscle activity during arm elevation: A review of normal function and alterations with shoulder impingement. Rev Bras Fisioter. 2009;13(1):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lawrence RL Braman JP Laprade RF Ludewig PM. Comparison of 3-dimensional shoulder complex kinematics in individuals with and without shoulder pain, part 1: sternoclavicular, acromioclavicular, and scapulothoracic joints. J Orthop Sports Phys Ther. 2014;44(9):636-645, A631-638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lin JJ Hsieh SC Cheng WC Chen WC Lai Y. Adaptive patterns of movement during arm elevation test in patients with shoulder impingement syndrome. J Orthop Res. 2011;29(5):653-657. [DOI] [PubMed] [Google Scholar]
- 4.Timmons MK Thigpen CA Seitz AL Karduna AR Arnold BL Michener LA. Scapular kinematics and subacromial-impingement syndrome: a meta-analysis. J Sport Rehabil. 2012;21(4):354-370. [DOI] [PubMed] [Google Scholar]
- 5.Ludewig PM Reynolds JF. The association of scapular kinematics and glenohumeral joint pathologies. J Orthop Sports Phys Ther. 2009;39(2):90-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uhl TL Kibler WB Gecewich B Tripp BL. Evaluation of clinical assessment methods for scapular dyskinesis. Arthroscopy. 2009;25(11):1240-1248. [DOI] [PubMed] [Google Scholar]
- 7.McClure P Tate AR Kareha S Irwin D Zlupko E. A clinical method for identifying scapular dyskinesis, part 1: reliability. J Athl Train. 2009;44(2):160-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tate AR McClure P Kareha S Irwin D Barbe MF. A clinical method for identifying scapular dyskinesis, part 2: validity. J Athl Train. 2009;44(2):165-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cools AM Declercq GA Cambier DC Mahieu NN Witvrouw EE. Trapezius activity and intramuscular balance during isokinetic exercise in overhead athletes with impingement symptoms. Scand J Med Sci Sports. 2007;17(1):25-33. [DOI] [PubMed] [Google Scholar]
- 10.Cools AM Witvrouw EE Declercq GA Danneels LA Cambier DC. Scapular muscle recruitment patterns: trapezius muscle latency with and without impingement symptoms. Am J Sports Med. 2003;31(4):542-549. [DOI] [PubMed] [Google Scholar]
- 11.Cools AM Witvrouw EE Declercq GA Vanderstraeten GG Cambier DC. Evaluation of isokinetic force production and associated muscle activity in the scapular rotators during a protraction-retraction movement in overhead athletes with impingement symptoms. Br J Sports Med. 2004;38(1):64-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roy JS Moffet H Hebert LJ Lirette R. Effect of motor control and strengthening exercises on shoulder function in persons with impingement syndrome: a single-subject study design. Man Ther. 2009;14(2):180-188. [DOI] [PubMed] [Google Scholar]
- 13.Worsley P Warner M Mottram S, et al. Motor control retraining exercises for shoulder impingement: effects on function, muscle activation, and biomechanics in young adults. J Shoulder Elbow Surg. 2013;22(4):e11-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wadsworth DJ Bullock-Saxton JE. Recruitment patterns of the scapular rotator muscles in freestyle swimmers with subacromial impingement. Int J Sports Med. 1997;18(8):618-624. [DOI] [PubMed] [Google Scholar]
- 15.Kuhn JE. Exercise in the treatment of rotator cuff impingement: a systematic review and a synthesized evidence-based rehabilitation protocol. J Shoulder Elbow Surg. 2009;18(1):138-160. [DOI] [PubMed] [Google Scholar]
- 16.De Mey K Danneels L Cagnie B Cools AM. Scapular muscle rehabilitation exercises in overhead athletes with impingement symptoms: effect of a 6-week training program on muscle recruitment and functional outcome. Am J Sports Med. 2012;40(8):1906-1915. [DOI] [PubMed] [Google Scholar]
- 17.Roy JS MacDermid JC Woodhouse LJ. Measuring shoulder function: a systematic review of four questionnaires. Arthritis Rheum. 2009;61(5):623-632. [DOI] [PubMed] [Google Scholar]
- 18.Oyama S Myers JB Wassinger CA Lephart SM. Three-dimensional scapular and clavicular kinematics and scapular muscle activity during retraction exercises. J Orthop Sports Phys Ther. 2010;40(3):169-179. [DOI] [PubMed] [Google Scholar]
- 19.Reinold MM Escamilla RF Wilk KE. Current concepts in the scientific and clinical rationale behind exercises for glenohumeral and scapulothoracic musculature. J Orthop Sports Phys Ther. 2009;39(2):105-117. [DOI] [PubMed] [Google Scholar]
- 20.Townsend H Jobe FW Pink M Perry J. Electromyographic analysis of the glenohumeral muscles during a baseball rehabilitation program. Am J Sports Med. 1991;19(3):264-272. [DOI] [PubMed] [Google Scholar]
- 21.Moseley JB Jr. Jobe FW Pink M Perry J Tibone J. EMG analysis of the scapular muscles during a shoulder rehabilitation program. Am J Sports Med. 1992;20(2):128-134. [DOI] [PubMed] [Google Scholar]
- 22.Cools AM Dewitte V Lanszweert F, et al. Rehabilitation of scapular muscle balance: which exercises to prescribe? Am J Sports Med. 2007;35(10):1744-1751. [DOI] [PubMed] [Google Scholar]
- 23.Reinold MM Wilk KE Fleisig GS, et al. Electromyographic analysis of the rotator cuff and deltoid musculature during common shoulder external rotation exercises. J Orthop Sports Phys Ther. 2004;34(7):385-394. [DOI] [PubMed] [Google Scholar]
- 24.L. BTAMWDWBW. EMG analysis of posterior rotator cuff exercises Athletic Training. 1990;25(1):40,42-45. [Google Scholar]
- 25.Sale DG. Neural adaptation to resistance training. Med Sci Sports Exerc. 1988;20(5 Suppl):S135-145. [DOI] [PubMed] [Google Scholar]
- 26.Sluijs EM Kok GJ van der Zee J. Correlates of exercise compliance in physical therapy. Phys Ther. 1993;73(11):771-782; discussion 783-776. [DOI] [PubMed] [Google Scholar]
- 27.Jack K McLean SM Moffett JK Gardiner E. Barriers to treatment adherence in physiotherapy outpatient clinics: a systematic review. Man Ther. 2010;15(3):220-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Uhl TL Smith-Forbes EV Nitz AJ. Factors influencing final outcomes in patients with shoulder pain: A retrospective review. J Hand Ther. 2017;30(2):200-207. [DOI] [PubMed] [Google Scholar]
- 29.Tate AR McClure PW Young IA Salvatori R Michener LA. Comprehensive impairment-based exercise and manual therapy intervention for patients with subacromial impingement syndrome: a case series. J Orthop Sports Phys Ther. 2010;40(8):474-493. [DOI] [PubMed] [Google Scholar]
- 30.McClure PW Michener LA. Staged Approach for Rehabilitation Classification: Shoulder Disorders (STAR-Shoulder). Phys Ther. 2015;95(5):791-800. [DOI] [PubMed] [Google Scholar]
- 31.Walch G Boulahia A Calderone S Robinson AH. The ‘dropping’ and ‘hornblower's’ signs in evaluation of rotator-cuff tears. J Bone Joint Surg Br. 1998;80(4):624-628. [DOI] [PubMed] [Google Scholar]
- 32.Hegedus EJ Goode A Campbell S, et al. Physical examination tests of the shoulder: a systematic review with meta-analysis of individual tests. Br J Sports Med. 2008;42(2):80-92; discussion 92. [DOI] [PubMed] [Google Scholar]
- 33.Hegedus EJ Goode AP Cook CE, et al. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br J Sports Med. 2012;46(14):964-978. [DOI] [PubMed] [Google Scholar]
- 34.Michener LA Walsworth MK Doukas WC Murphy KP. Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Arch Phys Med Rehabil. 2009;90(11):1898-1903. [DOI] [PubMed] [Google Scholar]
- 35.Leggin BG Michener LA Shaffer MA Brenneman SK Iannotti JP Williams GR, Jr. The Penn shoulder score: reliability and validity. J Orthop Sports Phys Ther. 2006;36(3):138-151. [DOI] [PubMed] [Google Scholar]
- 36.Ekstrom RA Bifulco KM Lopau CJ Andersen CF Gough JR. Comparing the function of the upper and lower parts of the serratus anterior muscle using surface electromyography. J Orthop Sports Phys Ther. 2004;34(5):235-243. [DOI] [PubMed] [Google Scholar]
- 37.McLean L Chislett M Keith M Murphy M Walton P. The effect of head position, electrode site, movement and smoothing window in the determination of a reliable maximum voluntary activation of the upper trapezius muscle. J Electromyogr Kinesiol. 2003;13(2):169-180. [DOI] [PubMed] [Google Scholar]
- 38.Nieminen H Takala EP Viikari-Juntura E. Normalization of electromyogram in the neck-shoulder region. Eur J Appl Physiol Occup Physiol. 1993;67(3):199-207. [DOI] [PubMed] [Google Scholar]
- 39.Ekstrom RA Donatelli RA Soderberg GL. Surface electromyographic analysis of exercises for the trapezius and serratus anterior muscles. J Orthop Sports Phys Ther. 2003;33(5):247-258. [DOI] [PubMed] [Google Scholar]
- 40.Kelly BT Kadrmas WR Kirkendall DT Speer KP. Optimal normalization tests for shoulder muscle activation: an electromyographic study. J Orthop Res. 1996;14(4):647-653. [DOI] [PubMed] [Google Scholar]
- 41.De Mey K Cagnie B Danneels LA Cools AM Van de Velde A. Trapezius muscle timing during selected shoulder rehabilitation exercises. J Orthop Sports Phys Ther. 2009;39(10):743-752. [DOI] [PubMed] [Google Scholar]
- 42.Dal Maso F Marion P Begon M. Optimal Combinations of Isometric Normalization Tests for the Production of Maximum Voluntary Activation of the Shoulder Muscles. Arch Phys Med Rehabil. 2016;97(9):1542-1551 e1542. [DOI] [PubMed] [Google Scholar]
- 43.Wilk KE Meister K Andrews JR. Current concepts in the rehabilitation of the overhead throwing athlete. Am J Sports Med. 2002;30(1):136-151. [DOI] [PubMed] [Google Scholar]
- 44.Seitz AL Kocher JH Uhl TL. Immediate effects and short-term retention of multi-modal instruction compared to written only on muscle activity during the prone horizontal abduction exercise in individuals with shoulder pain. J Electromyogr Kinesiol. 2014;24(5):666-674. [DOI] [PubMed] [Google Scholar]
- 45.Burden A. How should we normalize electromyograms obtained from healthy participants? What we have learned from over 25 years of research. J Electromyogr Kinesiol. 2010;20(6):1023-1035. [DOI] [PubMed] [Google Scholar]
- 46.Seitz AL Uhl TL. Reliability and minimal detectable change in scapulothoracic neuromuscular activity. J Electromyogr Kinesiol. 2012;22(6):968-974. [DOI] [PubMed] [Google Scholar]
- 47.Bolton JE Hurst HC. Prognostic factors for short-term improvement in acute and persistent musculoskeletal pain consulters in primary care. Chiropr Man Therap. 2011;19(1):27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McClure PW Bialker J Neff N Williams G Karduna A. Shoulder function and 3-dimensional kinematics in people with shoulder impingement syndrome before and after a 6-week exercise program. Phys Ther. 2004;84(9):832-848. [PubMed] [Google Scholar]
- 49.Katolik LI Romeo AA Cole BJ Verma NN Hayden JK Bach BR. Normalization of the Constant score. J Shoulder Elbow Surg. 2005;14(3):279-285. [DOI] [PubMed] [Google Scholar]
- 50.Burrus C Deriaz O Luthi F Konzelmann M. Role of pain in measuring shoulder strength abduction and flexion with the Constant-Murley score. Ann Phys Rehabil Med. 2017;60(4):258-262. [DOI] [PubMed] [Google Scholar]
- 51.Ice R. Long-term compliance. Phys Ther. 1985;65(12):1832-1839. [DOI] [PubMed] [Google Scholar]
- 52.Smith-Forbes EV Howell DM Willoughby J Armstrong H Pitts DG Uhl TL. Exploration of factors associated with patient adherence in upper extremity rehabilitation: a mixed methods embedded design. Arch Phys Med Rehabil. 2016; 97(8):1262-1268.e1. [DOI] [PubMed] [Google Scholar]
- 53.Eckard T Lopez J Kaus A Aden J. Home exercise program compliance of service members in the deployed environment: an observational cohort study. Mil Med. 2015;180(2):186-191. [DOI] [PubMed] [Google Scholar]
- 54.Henry KD Rosemond C Eckert LB. Effect of number of home exercises on compliance and performance in adults over 65 years of age. Phys Ther. 1999;79(3):270-277. [PubMed] [Google Scholar]