Abstract
Patient: Female, 44
Final Diagnosis: Optic neuritis
Symptoms: Unilateral vision loss
Medication: —
Clinical Procedure: Fundoscopic examination
Specialty: Ophthalmology
Objective:
Rare disease
Background:
Systemic lupus erythematosus (SLE) causes sight-threatening, ophthalmologic problems that are frequently challenging to manage. Optic neuropathy is a rare ophthalmological complication of SLE that can progress to total bilateral vision loss if not identified and treated rapidly. We describe a patient with SLE who presented with an acute, painless unilateral optic neuropathy who subsequently experienced partial recovery of vision when treated with high-dose intravenous corticosteroids.
Case Report:
A 44-year-old female with known SLE presented with 4 days of painless, complete, and gradual vision loss in the right eye. Initial ophthalmologic examination revealed no light perception, afferent pupil defect, 4+ optic disc swelling, and 1+ venous tortuosity of the right eye. No hemorrhage or exudates were noted. Diagnostic workup revealed a lupus flare with elevated inflammatory markers including elevated anti-nuclear antibody, anti-ds-DNA antibody, anti-Sm antibody, and anti-phospholipid IgG antibody. The diagnosis of optic neuropathy was clinically established, and the patient was treated with high-dose intravenous corticosteroids. Her vision improved, and she was transitioned to oral corticosteroids with eventual significant improvement in her vision.
Conclusions:
Optic neuropathy is a rare and devastating ophthalmologic complication of SLE. The diagnosis can be made by linking key clinical findings on ophthalmologic examination with positive serological studies. If treated rapidly with immunosuppressive therapy, the vision loss can be reversed, and permanent blindness avoided. Although this rare complication is generally bilateral in nature, clinician must also be aware of unilateral disease and treat patients accordingly.
MeSH Keywords: Deaf-Blind Disorders; Lupus Erythematosus, Systemic; Optic Nerve Diseases; Optic Neuropathy, Ischemic
Background
Systemic lupus erythematosus (SLE) is a complex inflammatory disease with an average prevalence of about 50 case per 100 000 individuals [1]. Ocular manifestations of SLE were first described in 1929 by Semon and Wolff; incidences are not infrequent, occurring in up to one-third of patients [2,3]. The thrombotic and inflammatory nature of the disease can affect almost every anatomical structure of the eye. Symptoms range from dry eyes as seen in keratoconjunctivitis sicca post-transplantation, also known as secondary Sjogren’s Syndrome, to complete vision loss in diseases that affect the retina and optic nerve. Optic nerve disease, represented by optic neuritis and ischemic optic neuropathy (anterior and posterior) are rare, but more severe, vision-threatening manifestations that affect only 1% of SLE patients [4]. In this report, we describe a patient with SLE who presented with optic neuropathy, and we review the literature associated with clinical and serologic diagnosis as well as acute and chronic management.
Case Report
A 44-year-old African-American female with what was reported to be stable SLE, end stage renal disease secondary to lupus nephritis, and a failed renal transplant, developed photophobia and fatigue followed by 4 days of painless, acute vision loss in the right eye. She denied headache, skin rash, joint pains, chest pain, or any other constitutional symptoms.
Physical examination revealed no skin rash, normal cardiac and lung auscultation, and a normal abdominal examination. Neurological examination revealed normal strength and sensation in the upper and lower extremities and cranial nerves I and III–XI were grossly intact. Ophthalmologic examination revealed that she was unable to perceive light (NLP) with the right eye and the visual acuity of her left eye measured 20/25. Near vision without correction was nil on the right and a brisk Jaeger 1 on the left. Color vision was nil on the right and she was able to identify 10 out of 10 Hardy-Rand-Rittler plates on the left. Visual fields to confrontation on the right side revealed that the patient could see hand motion in her temporal field only. Visual fields were full to confrontation on the left side. Pupils were 3 mm being nonreactive on the right and 1+ reactive on the left and there was a 2+ right relative afferent pupillary defect evident. The patient was orthophoric at distance with full ductions, versions, pursuit, and saccadic eye movements. There was no significant ptosis, enhanced ptosis, lid lag, or lid retraction noted. Cranial nerves V and VII were intact including normal corneal reflexes. Ocular tensions were 12 and 17, respectively. Slit lamp examination was essentially normal each eye. Fundoscopic examination revealed marked optic disc swelling with a markedly diffusely pale optic disc and 1+ retinal venous tortuosity (Figure 1). There were no vitreous cells and no papillary or retinal hemorrhages. The examination of left eye, including the optic disc and retinal vasculature, was normal. Differential diagnosis included acute ischemic optic neuropathy, viral neuroretinitis, compressive neoplasm or abscess, and toxic drug effect.
Figure 1.
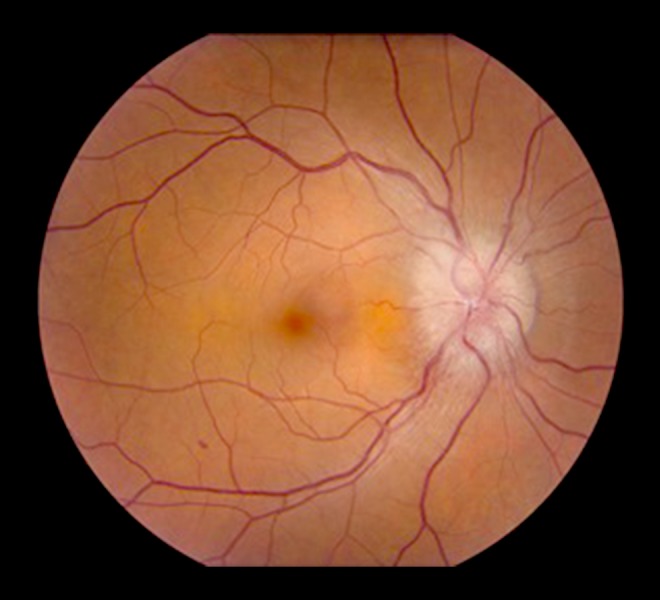
Funduscopic examination of a patient with optic neuropathy demonstrating an edematous, pale optic disc.
Computerized tomography (CT) scan of the head showed no neoplastic masses or signs of acute infection/brain abscess. CT scan of the orbits showed no compressive lesion of the optic nerve. There were no clinical or historical signs of systemic infection and infectious laboratory workup was overall negative. Drug screening and serum electrolytes were within normal limits. Inflammatory laboratory testing revealed elevated titers of several inflammatory markers consistent with a SLE flare: erythrocyte sedimentation rate (61 mm/hour; normal: 0–29 mm/hour); anti-nuclear antibody (>12 U; normal: <1 U); anti-ds-DNA antibody (294 IU/mL; normal: <30 IU/mL); anti-Sm antibody (>8 U; normal: <1 U); and anti-phospholipid IgG antibody (20.9 GPL; normal <10 GPL). Complement (C3 and C4) levels were within normal reference ranges. Acute optic neuropathy was diagnosed on the basis of the clinical examination and the unusual severity of the vision loss (NLP), coupled with the serologic evidence of a SLE flare. Treatment with high-dose intravenous dexamethasone (250 mg every 6 hours) was initiated and vision in the right eye began to return within the first few hours. Intravenous dexamethasone was continued for 3 days and her vision improved to the point that she could make out a hand moving 2 feet in front of her in all visual fields. She was transitioned to oral prednisone (80 mg/day) which was subsequently tapered over 3 weeks. Unfortunately, vision in her right eye failed to completely return, and at a subsequent neurology clinic visit, her right eye visual acuity was recorded at 20/200, far less than her pre-hospitalization baseline of 20/60-1.
Discussion
The pathogenesis of SLE is complex and can be comprised of multiple factors including gender and environment [5]. These factors can lead to the formation of both antibodies and immune complexes which can lead to a systemic, global inflammatory reaction. It is this global inflammation that leads to the multiple organ changes seen in SLE. Clinical history and examination involve confirming 4 out of 11 of the diagnostic criteria for SLE developed by the American College of Rheumatology [6,7]. These findings include malar rash, discoid rash, photosensitivity, oral ulcers, non-erosive arthritis of 2 or more peripheral joints, pleuritis or pericarditis, a renal disorder involving persistent proteinuria or cellular casts, a neurologic disorder involving seizures or psychosis, a hematologic disorder involving either hemolytic anemia, leukopenia, lymphopenia, or thrombocytopenia, an immunologic disorder involving anti-DNA antibody, Anti-Sm antibody or positive finding of antiphospholipid antibodies, and a positive antinuclear antibody. These findings may be noted on the present history and physical or documented at some time in the past.
Once SLE is confirmed, a thorough ophthalmologic examination must be conducted. Many different ocular findings may be present in SLE including eyelid abnormalities, ocular adnexa, keratoconjunctivitis sicca, iridocyclitis, retinal vasculitis, vasoocclusive disease, choroidopathy, and optic neuropathy [3]. Fundoscopic examination looking at blood vessels and nerves in detail is crucial in order to not overlook pathology (Table 1). SLE-associated optic neuritis characteristically presents as an acute, painful loss of vision secondary to infarction of the optic nerve secondary to arteriolar fibrinoid necrosis [8]. Conversely, optic neuropathy associated with SLE presents as bilateral, painless vision loss, with or without optic disc swelling; it is secondary to an ischemic process affecting the optic nerve head and retrobulbar nerve [3,8]. In a rare cohort of patients, unilateral vision loss associated with ischemic optic neuropathy is observed in patients with the presence of antiphospholipid antibodies; visual loss is secondary to a focal thrombotic event affecting the microcirculation rather than a global, vasculitic process [9]. Our patient presented with unilateral, painless vision loss, and swelling of the optic disc in the setting of elevated antiphospholipid antibody titers in a patient with an active SLE flare.
Table 1.
Clinical manifestations and diagnostic testing of systemic lupus erythematosus ocular diseases.
| Ocular finding | Clinical manifestation | Diagnostic testing |
|---|---|---|
| Eyelid disorder | Discoid lupus-type rash on lower eyelid | Eyelid biopsy with immunohistochemistry |
| Keratoconjunctivitis sicca | Dryness of the conjunctiva and cornea | Schirmer I test or Rose Bengal Score |
| Iridocyclitis | Inflammation of the iris and ciliary body | Slit lamp testing |
| Vaso-occlusive disease | Vision loss due to multiple branch retinal artery occlusions | Fluorescein retinal angiogram |
| Choroidopathy | Good visual acuity or patchy vision loss due to single or multiple areas of serous or exudative retinal detachment | Fundoscopic examination and fluorescein angiography |
| Optic neuropathy | Painless or painful vision loss due to ischemia of the optic nerve head and retrobulbar nerve | Fundus fluorescein angiography and MRI with gadolinium |
MRI – magnetic resonance imaging.
When SLE-associated optic neuritis is suspected, advance testing may include fundus fluorescein angiography (FFA), a complementary test that can detect retinal vasculature changes [4]. FFA in optic neuritis usually reveals vasodilation of the peripapillar capillaries and hyperfluorescence during the late phases of the examination [10]. Ischemic optic neuropathies are characterized by incomplete capillary and choroidal filling, followed by hyperfluoresceinic leakage (Figure 2). Optic neuropathies cause by retrobulbar lesions can have a normal funduscopic examination and FFA. In these cases, a magnetic resonance imaging (MRI) with gadolinium contrast may be needed in order to diagnose optic nerve enlargement and enhancement [4,11].
Figure 2.
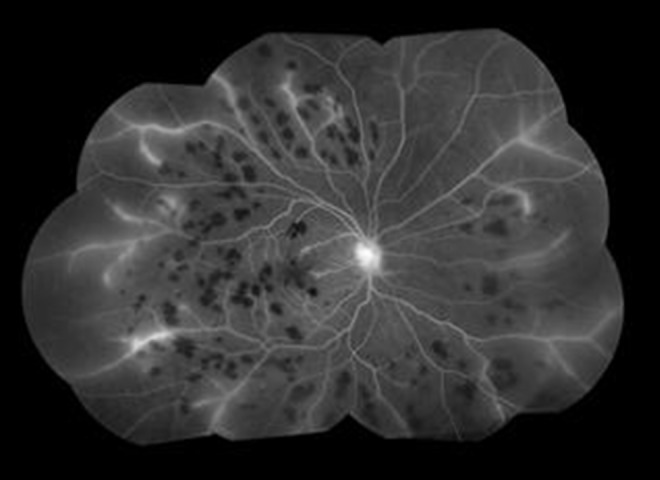
A fluorescein angiogram of lupus retinal vasculitis. Prominent features include scattered intraretinal hemorrhages, fluorescein leakage from the optic disc, vascular leakage from the large veins, and peripheral capillary non-perfusion
Immunosuppressive therapy is the mainstay treatment for both systemic and ocular SLE [12]. Treatment for ischemic optic neuropathy is controversial, especially in the presence of antiphospholipid antibodies. Because an acute thrombotic event rather than a global vasculitis appears to be the mechanism leading to visual loss, anticoagulation with warfarin or aspirin should be considered [12,13]. Although high-dose corticosteroids are usually given as empiric therapy, their role is to treat the accompanying systemic autoimmune illness rather than thrombotic sequelae from antiphospholipid syndrome [13]. Although methylprednisolone is the standard steroid given in cases of optic neuritis, we chose to use dexamethasone as it is known to have a better central nervous system (CNS) penetration. This higher CNS penetration is due to its ability to achieve higher free plasma levels related to its protein-binding capacity [14]. Hydroxychloroquine appears to be protective against thrombosis in patients with SLE and is considered as an approach to prevent thrombosis in the presence of antiphospholipid antibodies [15]. The standard treatment for SLE optic neuropathy includes high-dose intravenous methylprednisolone (1 g/day for 3 days) followed by oral prednisone (1 mg/kg/day) [16]. Unfortunately, up to 29% of patients may be refractory to corticosteroids [17]. Pulse-dosed intravenous cyclophosphamide for 6 months has been studied in open and controlled clinical trials and seems to be effective in corticosteroid refractory optic neuropathy [18].
Conclusions
Although rare, optic neuritis and ischemic optic neuropathy are ophthalmologic complications of SLE which can present suddenly and cause permanent vision loss. Obtaining a good patient history and performing a thorough funduscopic examination are crucial in making the proper diagnosis. Unilateral optic neuropathy with anti-phospholipid antibodies deserves early high-dose IV corticosteroids followed by a taper in order to treat the inflammatory component of SLE. Anticoagulation and hydroxychloroquine should strongly be considered as they may protect against additional thrombotic events. Physicians’ understanding of this workup and treatment may prevent vision loss in their SLE patients.
Footnotes
Conflicts of interest
None.
References:
- 1.Petri M. Epidemiology of systemic lupus erythematosus. Best Pract Res Clin Rheum. 2002;16(5):847–58. doi: 10.1053/berh.2002.0259. [DOI] [PubMed] [Google Scholar]
- 2.Semon HC, Wolff E. Acute lupus erythematosus, with fundus lesions. Proc R Soc Med. 1933;27:153–57. [PMC free article] [PubMed] [Google Scholar]
- 3.Palejwala NV, Walia HS, Yeh S. Ocular manifestations of systemic lupus erythematosus: A review of the literature. Autoimmune Dis. 2012;2012:290898. doi: 10.1155/2012/290898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Andrade FA, Guimaraes Moreira Balbi G, Bortoloti de Azevedo LG, et al. Neuro-ophthalmologic manifestations in systemic lupus erythematosus. Lupus. 2017;26(5):522–28. doi: 10.1177/0961203316683265. [DOI] [PubMed] [Google Scholar]
- 5.Silpa-archa S, Lee JJ, Foster CS. Ocular manifestations in systemic lupus erythematosus. Br J Ophthalmol. 2016;100(1):135–41. doi: 10.1136/bjophthalmol-2015-306629. [DOI] [PubMed] [Google Scholar]
- 6.Tan EM, Cohen AS, Fries JF, et al. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1982;25:1271–77. doi: 10.1002/art.1780251101. [DOI] [PubMed] [Google Scholar]
- 7.Yu C, Gershwin ME, Chang C. Diagnostic criteria for systemic lupus erythematosus: A critical review. J Autoimmun. 2014:48–49. 10–13. doi: 10.1016/j.jaut.2014.01.004. [DOI] [PubMed] [Google Scholar]
- 8.Sivaraj RR, Durrani OM, Denniston AK, et al. Ocular manifestations of systemic lupus erythematosus. Rheumatology (Oxford) 2007;46(12):1757–62. doi: 10.1093/rheumatology/kem173. [DOI] [PubMed] [Google Scholar]
- 9.Giorgi D, Balacco Gabrieli C. Optic neuropathy in systemic lupus erythematosus and antiphospholipid syndrome (APS): Clinical features, pathogenesis, review of the literature and proposed ophthalmological criteria for APS diagnosis. Clin Rheumatol. 1999;18(2):124–31. doi: 10.1007/s100670050069. [DOI] [PubMed] [Google Scholar]
- 10.Vine AK, Barr CC. Proliferative lupus retinopathy. Arch Ophthalmol. 1984;102:852–54. doi: 10.1001/archopht.1984.01040030672015. [DOI] [PubMed] [Google Scholar]
- 11.Uy HS, Chan PS. Systemic lupus erythematosus. In: Foster CS, Vitale A, editors. Diagnosis & Treatment of Uveitis. 2nd ed. New Delhi: Jaypee Brothers Medical Publishers; 2013. [Google Scholar]
- 12.Bajwa A, Foster SC. Ocular manifestations of systemic lupus erythematosus. J Clin Cell Immunol. 2014;5:191. [Google Scholar]
- 13.Tugcu B, Acar N, Coskun CT, et al. Nonarteritic anterior ischemic optic neuropathy as the presenting manifestation of primary antiphospholipid syndrome. Indian J Ophthalmol. 2014;62(5):642–44. doi: 10.4103/0301-4738.109535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Balis FM, Lester CM, Chrousos GP, et al. Differences in cerebrospinal fluid penetration of corticosteroids: Possible relationship to the prevention of meningeal leukemia. J Clin Oncol. 1987;5(2):202–7. doi: 10.1200/JCO.1987.5.2.202. [DOI] [PubMed] [Google Scholar]
- 15.Szymezak J, Ankri A, Fischer AM, Darnige L. [Hydroxychloroquine: A new therapeutic approach to the thrombotic manifestations of antiphospholipid syndrome] Rev Med Interne. 2010;31(12):854–57. doi: 10.1016/j.revmed.2010.08.018. [in French] [DOI] [PubMed] [Google Scholar]
- 16.Suri D, Abujam B, Gupta A, et al. Optic nerve involvement in childhood onset systemic lupus erythematosus: Three cases and a review of the literature. Lupus. 2015;25(1):93–96. doi: 10.1177/0961203315603142. [DOI] [PubMed] [Google Scholar]
- 17.Galindo-Rodriguez G, Avina-Zubieta JA, Pizarro S, et al. Cyclophosphamide pulse therapy in optic neuritis due to systemic lupus erythematosus: An open trial. Am J Med. 1999;106(1):65–69. doi: 10.1016/s0002-9343(98)00372-6. [DOI] [PubMed] [Google Scholar]
- 18.Frigui M, Frikha F, Sellemi D, et al. Optic neuropathy as a presenting feature of systemic lupus erythematosus: Two case reports and literature review. Lupus. 2011;20(11):1214–18. doi: 10.1177/0961203311403344. [DOI] [PubMed] [Google Scholar]


