Abstract
Purpose
Head and neck arteriovenous malformation (AVM) and fistulae treatment without reflux and with nidal penetration are challenging. We describe a case series including adult and pediatric patients utilizing a specific two-microcatheter technique using Onyx with strategic embolization of small feeding branches prior to dominant branch embolization. We aim to demonstrate the safety and efficacy of this technique.
Methods
Patient Selection
Head and neck vascular malformation cases were reviewed from 2010 to 2017. 11 patients between 2010 and 2017 were treated with serial embolization along with Onyx embolization utilizing a two-microcatheter technique. Five patients had cerebral AVMs, three had dural arteriovenous fistulae, two had mandibular AVMs, and one had a posterior neck AVM. Vascular anatomy, location, and procedural details were recorded.
Technique
During procedures 1–4, smaller arterial feeders were embolized first to maximally decrease the intranidal pressure at the time of the embolization of the major residual feeder. The dominant residual feeder was then embolized using two catheters. Coils followed by Onyx were initially deployed through the proximal catheter to form a dense plug. The plug was allowed to solidify for 30 min. Aggressive embolization of the nidus was then performed through the distal catheter.
Results
All 11 patients had excellent treatment results with complete (6) or near-complete (5) obliteration of the vascular malformation nidus. No procedural complications were noted, specifically no strokes, hemorrhages, or unintentionally retained catheter fragments occurred.
Conclusion
AVMs and fistulae are challenging to treat. A two-microcatheter technique for Onyx embolization with prior embolization of smaller arterial feeders is a safe and efficacious treatment option. This technique allows for maximal nidus penetration while minimizing the risk of nontarget embolization/reflux. In all cases, we achieved excellent results with complete or near-complete obliteration of the vascular malformation nidus.
INTRODUCTION
Treatment for head and neck vascular malformations is challenging and endovascular embolization is an increasingly utilized treatment option. The minimally invasive approach additionally allows for an evaluation of the angioarchitecture at the time of treatment. In addition, presurgical evaluation along with embolization is extremely helpful prior to definitive surgical management. Liquid embolic agents such as Onyx (Medtronic-Covidien, Irvine, CA, USA) along with coils are used frequently to provide plug formation of the dominant feeding branch along with penetration into the arteriovenous malformation (AVM) nidus or fistula point.
There are technical challenges associated with utilizing liquid embolic agents for the treatment of complex vascular malformations. Variable nidal and fistulae angioarchitecture along with multiple inflow and outflow channels can make this a challenging problem. Penetration into the nidus and fistula point without clinically significant reflux requires careful preembolization planning along with excellent embolization technique. The flow dynamics of a vascular malformation change once embolization has commenced on a feeding pedicle. Carefully selecting which inflow tracts to embolize first can help improve penetration into the fistula point or nidus once the dominant feeder is selected for embolization.
Recently, Abud et al. [1, 2] described techniques to prevent reflux during embolization utilizing a two-catheter technique. Each technique incorporates proximal plug formation with the more proximal microcatheter. This improves wedge-flow conditions for Onyx embolization through the distal microcatheter. We describe our technique including a different proximal plug formation followed by nidus and fistulae penetration using a two microcatheter system in the main feeding branch of the vascular malformation. In addition, we describe our technique of strategic embolization of smaller nidal or fistulae feeders to reduce intranidal pressure prior to embolization of the dominant feeding branch. We detail our application of this technique in both adult and pediatric patients with head and neck vascular malformations.
TECHNIQUE
The pressure cooker technique (PCT) previously described by Chapot et al. [3] positions a detachable microcatheter with the tip in the intranidal position. A second nondetchable microcatheter is positioned between the detachment zone and distal marker of the first microcatheter. Coils and NBCA Glue (Codman, West Chester, PA, USA) are used to form a plug through the nondetachable microcatheter. Onyx embolization is then performed through the distal microcatheter. In the modified PCT (mPCT) described by Abud et al. [2], microcatheters are positioned as described in the PCT. However, Onyx injection is performed through the detachable microcatheter first until reflux occurs. NBCA is then injected through the proximal microcatheter to form a plug. Onyx embolization is then performed through the distal microcatheter.
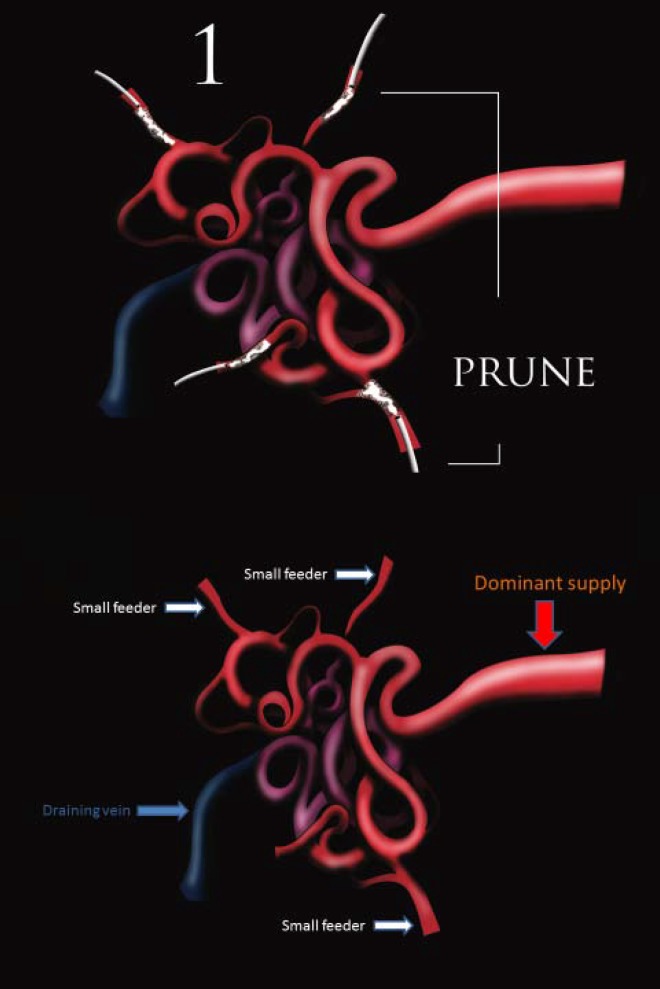
Our technique utilizes a “prune, plug, and penetrate” approach. First, serial arterial embolization is performed on smaller arterial feeders. This approach reduces the intranidal pressure at the time of the embolization of the major residual feeder. After the smaller branches have been embolized, the dominant feeding branch is selected. A DMSO compatible microcatheter is positioned near the nidus and a second DMSO compatible microcatheter is positioned proximally with the tip between the distal microcatheter tip and detachment zone. Plug formation is commenced through the proximal microcatheter with Onyx 34 (Medtronic, Minneapolis, MN, USA) and coils to optimize wedge-flow conditions. The onyx plug is allowed to form over a 30 min duration after which Onyx 18 is slowly injected through the distal microcatheter to penetrate the nidus of the vascular malformation.
RESULTS
11 cases were performed with this technique between 2010 and 2017. Of these cases, five were cerebral AVMs, three were dural AV fistulas, and three were head and neck AVMs. Six were pediatric cases. On follow-up evaluation, six patients had no residual vascular malformation. No deaths, strokes, or other neurological sequela occurred as a result of the procedure.
EXAMPLE CASE—MANDIBULAR AVM
A 10-year-old male with a right mandibular AVM was presented with bleeding from his upper teeth. The bleeding episodes became more frequent and an MRI face/neck was performed which was suggestive of a right mandibular AVM. After a lengthy discussion with the patient’s mother, elective embolization was performed. Pruning of smaller feeder branches was performed utilizing coils and NBCA glue. The dominant feeding branch (inferior alveolar artery) was then selected with two duo microcatheters (Microvention, Aliso Viejo, CA, USA). The proximal microcatheter was positioned in the proximal portion of the inferior alveolar artery and the distal microcatheter was positioned in the distal inferior alveolar artery just proximal to the AVM nidus. The microwire was left in place in the distal microcatheter to prevent occlusion of the lumen once the proximal embolization was commenced. The proximal inferior alveolar artery was embolized with two helix Concerto coils (Medtronic, Irvine, CA, USA). The proximal inferior alveolar artery was then embolized through the same catheter with Onyx 34. The Onyx cast was allowed to harden for 30 min. Embolization through the distal microcatheter was performed with Onyx 18 under roadmap technique. Five intraembolization arteriograms were performed during embolization demonstrating extension of the Onyx through the inferior alveolar artery into the large venous cavity and nidus within the mandible. Each arteriogram demonstrated progressively less shunting until the final angiogram demonstrated no evidence of shunting or residual AVM. In addition, there was no evidence of Onyx reflux proximal to the plug. Both catheters were removed uneventfully. A completion postembolization right external carotid arteriogram was performed demonstrating angiographic cure of the AVM.
DISCUSSION
Liquid embolic agents have been utilized with greater frequency for the treatment of head and neck AVMs [7]. Specifically, Onyx has become a preferred liquid embolic choice for AVMs and AV fistulas because it allows for greater control during embolization for longer periods of time when compared to NBCA. This can lead to better treatment results for AVMs and DAVFs [4]. Limitations and pitfalls occur without a defined treatment strategy prior to embolization. We believe that thoughtful optimization of flow dynamics for nidal and AV fistula penetration during dominant arterial branch embolization is therefore paramount to success. The “prune, plug, and penetrate” technique allows for this optimization.
Onyx embolization additionally requires repeated delicate injections over several minutes to create a proximal plug. During this time, delays in waiting for the plug formation prolong the procedure times and increase the risk of microcatheter occlusion. The risk of reflux increases as does the probability of loss of access to the nidal or fistula point. The dual microcatheter technique helps to improve penetration into the dominant feeding branch supply after proximal plug formation. Technical limitations to this technique include dominant arterial branch size which is too small for the placement of two microcatheters. Difficult and tortuous access is another limitation. These technical limitations are equally challenging when utilizing the PCT, mPCT, and attempting to use double-lumen balloons for embolization. Balloon use also poses the risk of pedicle rupture with balloon inflation.
In conclusion, our experience utilizing a multistep technique including pruning smaller arterial feeding branches prior to utilizing a two-microcatheter technique for the dominant feeding branch embolization can dramatically improve success rates. In addition, we demonstrated that this technique can be applied to both adult and pediatric vascular malformations.
Figure 1. (1) Prune, (2) plug, and (3) penetrate technique.
Figure 2. Preembolization right external carotid artery arteriogram.
Figure 3. Proxima (vertical arrow) and distal (horizontal arrow) microcatheter tips positioned in the inferior alveolar artery.
Figure 4. Proximal plug with coils and Onyx 34.
Figure 5. Postembolization right external carotid artery arteriogram with no evidence of residual AVM.
Table 1. Cerebral AVM cases.
| Age | Gender | Spetzler Martin | Location | Pedicles embolized with dual catheter | Result | Follow-up |
|---|---|---|---|---|---|---|
| 11 | F | 2 | Left occipital | Embolization 2- Left PCA | No residual-> surgery the next day | No residual at six months |
| 17 | M | 3 | Right frontal | Embolization 3- Right ACA | Minimal residual -> gamma knife | No residual at four months |
| 34 | M | 4 | Right frontal | Embolization 5- Right ACA | Minimal residual -> surgery the next day | No residual at 1 week |
| 53 | F | 4 | Left occipital | Embolization 3- Left PCA | Minimal residual-> surgery the next day | Pending |
| 16 | M | 3 | Right temporal | Embolization 1- Right PCA and MCA | Minimal residual -> surgery the next day | Pending |
Table 2. Dural AV fistula cases.
| Age | Gender | Cognard | Pedicles embolized with dual catheter | Result | Follow-up |
|---|---|---|---|---|---|
| 36 | M | 3 | Left occipital and middle meningeal | No residual | No residual at six months |
| 34 | F | 2b | Right occipital and middle meningeal | Minimal residual | No residual at 2 years |
| 88 | M | 2b | Right occipital and left posterior meningeal | Minimal residual | Minimal residual at one month |
Table 3. Head and neck AVMs cases.
| Age | Gender | Location | Pedicles embolized with dual catheter | Result | Follow-up |
|---|---|---|---|---|---|
| 10 | Male | Right mandibular | Embolization 1Right facial and internal maxillary | No residual | No residual at six months |
| 15 | Male | Left neck | Embolization 2, 4Deep cervical and transverse scapularDeep cervical and transverse scapular | Minimal residual | Pending |
| 10 | Female | Right mandibular | Embolization 1Right internal maxillary | No residual | Pending |
Acknowledgments
None.
REFERENCES
- Abud DG, et al. The modified pressure cooker technique: an easier way to control Onyx reflux. J Neuroradiol. 2016;43(3):218–222. doi: 10.1016/j.neurad.2016.01.146. [DOI] [PubMed] [Google Scholar]
- Abud DG, et al. Treatment of brain arteriovenous malformations by double arterial catheterization with simultaneous injection of Onyx: a retrospective series of 17 patients. Am J Neuroradiol. 2011;32(1):152–158. doi: 10.3174/ajnr.A2247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapot R, et al. The pressure cooker technique for treatment of brain AVMs. J Neuroradiol. 2014;41:87–89. doi: 10.1016/j.neurad.2013.10.001. [DOI] [PubMed] [Google Scholar]
- Mounayer C, et al. Nidal embolization of brain arteriovenous malformations using onyx in 94 patients. Am J Neuroradiol. 2007;28(3):518–523. [PMC free article] [PubMed] [Google Scholar]
- Michelozzi C, et al. Arterial embolization with onyx of head and neck paragangliomas. J Neurointerv Surg. 2016;8(6):626–635. doi: 10.1136/neurintsurg-2014-011582. [DOI] [PubMed] [Google Scholar]
- Weber W, et al. Endovascular treatment of intracranial arteriovenous malformations with onyx: technicalaspects. Am J Neuroradiol. 2007;28(2):371–377. [PMC free article] [PubMed] [Google Scholar]
- Saatci I, et al. Endovascular treatment of brain arteriovenous malformations with prolonged intranidal Onyx injection technique: long-term results in 350 consecutive patients with completed endovascular treatment course. J Neurosurg. 2011;115(1):78–88. doi: 10.3171/2011.2.JNS09830. [DOI] [PubMed] [Google Scholar]