Abstract
This article describes several barriers to widespread dissemination of manualized family-based treatments for adolescent substance use (ASU). We then offer a highly promising solution for adopting and sustaining family therapy in usual care: distilling the core practice elements of empirically validated family therapy models for ASU. We present a conceptual distillation of family therapy for ASU grounded in existing observational fidelity measures for three manualized models, a process that yielded four core elements: Family Engagement, Relational Reframing, Family Behavior Change, and Family Restructuring. We then introduce an innovative empirical method for distilling core elements that can serve as a template for rigorous distillation of other treatment approaches. Finally, we discuss how core elements can enhance family therapy services within the diverse workforce of usual care for ASU.
Keywords: Adolescent substance use, family therapy, core elements, usual care
1. Introduction
Although family therapy has by far the largest base of empirical support for treating adolescent substance use (ASU), there are several intransigent barriers to widespread adoption of manualized family therapy models. This article describes an alternative path to promoting family therapy adoption, the core elements strategy, which offers important advantages overpurveyor-driven dissemination with regard to sustaining quality implementation in routine service settings. The initial step along this path is successfully distilling the core treatment techniques of empirically validated family therapy models for ASU. We first present a conceptual distillation of family therapy for ASU that is grounded in existing observational fidelity measures for three manualized models. We then describe an innovative empirical method for distilling core elements that can serve as a template for rigorous distillation of other treatment approaches. We conclude by discussing how coreelements can enhance family therapy services within the diverse workforce of usual care for ASU.
2. Dissemination Challenge: Unmet Clinical Need for Family Therapy for ASU
2.1 Family Therapy for ASU is Ripe for Widespread Dissemination
Currently family therapy (FT) enjoys the strongest evidence base for treating ASU (Hogue, Henderson, Ozechowski, & Robbins, 2014). FT for ASU follows an ecological orientation that targets multiple interacting systems (e.g., family, school, peer, juvenile justice) within which adolescents develop. There are a handful of manualized, empirically supported FT models designed to treat ASU, the most prominent being brief strategic family therapy (BSFT), functional family therapy (FFT), multidimensional family therapy (MDFT), and multi systemic therapy (MST) (Baldwin, Christian, Berkeljon, & Shadish, 2012). Although these “brand-name” models differ from one another along several dimensions of intervention focus and sequencing (see Section 4.1), they are common members of the broader FT approach, whose signature features include embracing developmentally calibrated parenting strategies, intervening directly with family members to repair intrafamilial relationships, and addressing challenges encountered by adolescents and caregivers in key extrafamilial systems (Rowe, 2012).
Manualized FT models have reached the highest levels of empirical validation for ASU, posting an exemplary record of success in comparison to bona fide alternative treatments (Hogue et al., 2014). Meta-analyses of randomized trials demonstrate that FT consistently prevails against other manualized ASU treatments as well as usual care, and it produces the largest average effect sizes by a wide margin (Baldwin et al., 2012; Tanner-Smith et al., 2013). The FT approach also has the strongest empirical support for treating adolescent disruptive behaviors that commonly co-occur with ASU, such as aggression, conduct disorder and delinquency (Baldwin et al., 2012; Chorpita et al., 2011; McCart & Sheidow, 2016). Studies of manualized FT for ASU also frequently report significant reductions in internalizing symptoms and gains in prosocial functioning (described in Hogue & Liddle, 2009).
Due in large part to its extensive evidence base, the FT approach has long been strongly endorsed by federal agencies (e.g., Center for Substance Abuse Treatment, 1999), national associations (e.g., American Academy of Child and Adolescent Psychiatry, 1997), and policy-making groups (e.g., Drug Strategies, 2003). More recently there is also incentive from ASU clinical providers and payers to deliver FT services: FT is now approved for treating ASU and co-occurring disorders by federal and private insurance plans (Blue Cross, 2013; Cigna, 2012; Oxford, 2013) and regulatory agencies that govern licensed treatment providers (e.g., State of New York, 2010; State of Pennsylvania, 2010). Thus there is impetus from all corners to expand FT adoption and implementation in usual care for ASU (Kaslow, Broth, Smith, & Collins, 2012).
2.2 Barriers to Widespread Adoption of Manualized FT Models in Usual Care for ASU
Despite their unrivaled empirical portfolio and policy support for treating ASU, manualized FT models have not yet been widely adopted within ASU treatment systems nationwide. Moreover, large-scale federal initiatives to install evidence-based practices for ASU in community settings have passed over manualized FTs in favor of individual and group models (e.g., Godley, Garner, Smith, Meyers, & Godley, 2011; Ramchand, Griffin, Suttorp, Harris, & Morral, 2011). The overarching barrier to adoption of brand-name FTs appears to be the mismatch between dissemination methods used by these models versus the needs of the provider community. Developers of manualized FTs disseminate their respective models by establishing corporate entities (i.e., model purveyors) that contract directly with host agencies to govern adoption activities (Henggeler & Sheidow, 2012). To support high-fidelity implementation, each brand-name model contains an extensive set of quality assurance (QA) procedures anchored by a treatment manual, standardized training toolkit, guidelines for ongoing training and observational consultation from model experts, and quality improvement methods that feed implementation data back to therapists and facilitate site recertification (see Hogue, Ozechowski, Robbins, & Waldron, 2013). These purveyor-driven QA procedures are considered essential for effective model implementation and are required for proper credentialing in each of the respective manualized FTs.
Proprietary licensing and QA procedures present three sizeable barriers to the feasibility of importing manualized FTs into usual care: (a) Cost: Purveyor contracts cost tens of thousands of dollars annually for initial training plus certification maintenance (Substance Abuse and Mental Health Services Administration, 2012). This is routinely affordable only for well-funded practice networks, principally government-operated sectors of care (e.g., juvenile justice, child welfare) in which clients are high risk, services are high cost, and stakes for success are high profile (Chambers, Ringeisen, & Hickman, 2005). (b) Flexibility: Manualized FTs feature highly structured intervention sequencing and require wholesale implementation of all treatment components. These model characteristics prohibit piecemeal implementation and selective treatment planning favored by many practitioners, and they discourage flexible use of discrete model components as auxiliary interventions for cases where substance use is not the primary referral problem (Chorpita, Daleiden, & Weisz, 2005a). (c) Sustainability: Beyond cost, QA procedures for multicomponent FTs are difficult to sustain over time in usual care due to vicissitudes in local regulatory practices, reduction in purveyor commitment or availability, decrease in provider stamina to honor QA procedures for an extended period, and demoralization among staff when external agents are responsible for ongoing judgments about clinical performance and intervention priorities (Gallo & Barlow, 2012). For all these reasons, importing and sustaining purveyor-driven FT models is beyond the reach of most ASU providers (Hogue et al., 2013).
3. Dissemination Solution: Distill the Core Elements of FT for ASU
Adoption barriers such as those listed above are common to manualized treatments of every kind, not just FT. As a result, experts in child and adolescent mental health (e.g., Chorpita, Becker, &Daleiden, 2007; Garland, Hawley, Brookman-Frazee, & Hurlburt, 2008; Weisz, Ugueto, Herren, Afienko, &Rutt, 2011), substance use (Carroll & Rounsaville, 2006; Hogue, 2010; Magill et al., 2016), and behavioral health policy (Institute of Medicine, 2015) all advocate an alternative strategy to complement manual-driven methods: Focus on core elements of empirically supported treatments that are common across models for similar populations. As defined by Chorpita and colleagues (Chorpita et al., 2005a; Chorpita, Daleiden, & Weisz, 2005b; Daleiden, Chorpita, Donkervoet, Arensdorf, &Brogan, 2006), the core elements approach seeks to define a reduced set of intervention techniques that are common ingredients in multiple evidence-based treatments for a given disorder. This is achieved by (a) specifying the discrete techniques prescribed by similar manuals (see Chorpita & Weisz, 2009) and (b) distilling these techniques into a smaller number of overlapping elements that are core features (and presumptive active ingredients) of each manual (Chorpita & Daleiden, 2009). As a result, the distilled core practice elements are approach-specific (i.e., identified with a particular treatment orientation and/or modality) but model-free (i.e., not inextricably bound to a single manual or intervention sequence). This section (1) articulates the primary strengths of the core elements strategy for advancing the dissemination of evidence-based interventions (EBIs) for every variety of behavioral disorder and (2) describes recent studies demonstrating that core elements of FT for ASU can be delivered in a community setting with fidelity and effectiveness comparable to that achieved by manualized FTs.
3.1 (Potentially) Transformative Advantages of Disseminating Core Elements
The core elements strategy has been deemed a “disruptive innovation” (Rotheram-Borus, Swendeman, & Chorpita, 2012): a simpler and more accessible alternative service (e.g., ATM machines, drug-store eyeglasses) that does not replace a specialty option (bank tellers, opticians) but instead meets essential needs of the customer majority in a more scalable, replicable, and sustainable manner. The overall goal of the core elements strategy is to shift the emphasis of dissemination and implementation away from exclusive focus on manual-driven treatment models and toward focus on shared elements of research-supported treatments that are more easily translated into practice. The potentially transformative advantages of core elements are presented in Figure 1, utilizing McHugh and Barlow’s (2010) framework for conceptualizing phases of disseminating EBIs: organizational planning, training, continuous quality control, and sustainability. Whereas treatment manuals are predominantly complex, uniform, and disorder-specific, distilled core elements are granular, flexible, and transdiagnostic—three user-centered features (Lyon & Koerner, 2016) that help solve vexing barriers associated with implementing manuals in everyday practice.
Figure 1.


Functional Comparison ofTwo Strategies for Disseminating Evidence-Based Interventions: Treatment Manuals versus Core Elements
*Based on McHugh & Barlow (2010).
1. Glisson (2002); 2. Chorpita, Becker, & Daleiden (2007); 3. Schoenwald et al. (2008); 4. Carroll & Rounsaville (2006); 5. Borntrager, Chorpita, Higa-McMillan, & Weisz (2009); 6. Carroll, Kadden, Donovan, Zweben, & Rounsaville (1994); 7. Aarons, Sommerfeld, Hecht, Silovsky, & Chaffin (2009); 8. Knudsen, Ducharme, & Roman (2008); 9. Weisz et al. (2012); 10. Ward et al. (2013); 11. Addis, Wade, & Hatgis (1999); 12. Addis & Krasnow (2000); 13. Hayes (2002); 14. Westen, Novotny, & Thompson-Brenner (2005); 15. Weisz et al. (2011); 16. Rotheram-Borus, Swendeman, & Chorpita (2012); 17. Garland, Hawley, Brookman-Frazee, & Hurlburt (2008); 18. Liberman & Corrigan (1994); 19. Chorpita & Daleiden (2009); 20. Gallo & Barlow (2012); 21. Chorpita, Daleiden, & Weisz (2005b).
As depicted in Figure 1, the core elements strategycan potentially improve the feasibility of procedures for training community providers and monitoring fidelity by introducing discrete interventions that can be more readily learned by clinical staff and more flexibly applied to a larger set of clinical problems. Core elements represent a comfortable middle ground between molar versus molecular formulation of treatment processes that is well-suited for describing the eclectic clinical practices favored in usual care (Barth et al., 2014; Garland et al., 2010). At the same time, this strategypreservesmany indispensable benefits of treatment specification found in manuals (e.g., well-delineated treatment techniques and fidelity procedures) without consigning therapists to the herculean task of implementing and/or adapting a different manual for each kind of client (Chorpita et al., 2005b). The dissemination advantages presented in Figure 1 are particularly germane to the cost, flexibility, and sustainability barriers described above for manualized FTs. If ultimately proven effective, the benefits of the core elements strategy for disseminating EBIs may be profound: unify and simplify the task of implementing EBIs in routine care with fidelity; retain the importance of provider judgment about duration, intensity, and other parameters of EBI delivery; and provide evidence-based options for client groups for whom no manuals currently exist (Chorpita et al., 2005a; Daleiden & Chorpita, 2005; Rotheram-Borus et al., 2012; Ward et al., 2013).
Core elements can also complement, and perhaps even boost, dissemination of treatment manuals by enhancing the basic clinical competencies of community practitioners (Garland et al., 2008) as well as co-exist with manualized models to provide a range of treatment planning options for clinicians operating in busy treatment marketplaces (Southam-Gerow et al., 2014). Indeed, treatment marketplaces appear to be already infused with EBIs in both manualized and non-manualized form, as evidenced by the strong endorsement of EBIs voiced in surveys of practice habits by front-line clinicians in substance use (Gifford et al., 2012) and mental health (Cook, Biyanora, Elhai, Schnurr, & Coyne, 2010). The apparent infusion of EBIs into everyday care is undoubtedly related to efforts by clinical training programs to encourage evidence-based practice among their trainees (e.g., Barth et al., 2014). Of course, absent objective (e.g., observational) data on the actual implementation of EBIs in usual care (see Hogue, Dauber, Lichvar, Bobek, & Henderson, 2015; Hurlburt, Garland, Nguyen, & Brookman-Frazee, 2010), it is impossible to state with certainty how extensively, and with what degree of fidelity, this infusion has occurred (Garland et al., 2010).
It is critical to underscore that distilled core elements are not equivalent to manualized treatments. Broadly speaking, manualized treatments contain two interdependent dimensions: model content and model coordination (Chorpita et al., 2005a, 2005b). Content refers to model-endorsed treatment techniques and therapeutic procedures, from which core elements can be distilled. In contrast, coordination refers to model-specific principles for clinical decision-making about when and how to use various techniques and procedures. The coordination dimension defines idiosyncratic aspects of model delivery—rules for timing, sequencing, and client- and context-specific targeting of interventions—that constitute the unique parameters and implementation nuances of a given model (see Garland, Hurlburt, & Hawley, 2006; Kazdin, 1999). These coordination principles determine, for example, how rigidly versus flexibly a therapist should implement model content, as well as the prescribed balance between fidelity versus adaptation for individual cases or clinical groups (McHugh, Murray, & Barlow, 2009).
Because the distillation process involves content only, it does not capture coordination parameters that guide effective treatment. Core elements thus cannot supplant full treatment models or be utilized effectively as brief versions. Rather, core elements can (a) supplement manualized training and implementation procedures for corresponding treatment models; (b) be organized themselves according to a standardized coordination system (a de facto “manual”) that facilitates decision-making about when and with whom to implement which combination of elements (e.g., MATCH-ADTC [Chorpita & Weisz, 2009], described in the following paragraph); or (c) be used independently by practicing clinicians who bring their own conceptualizations about timing, sequence, and relative emphasis to each case (see Lyon & Koerner, 2016), with the caveat that treatment planning remain guided by evidence-based assessment and treatment selection principles (Jensen-Doss, 2015). As core elements distillation progresses, we will also discover the limits of its utility in certain treatment contexts and/or with certain presenting problems. For example, some behavioral disorders may be so complex or otherwise treatment-resistant (e.g., Borderline Personality Disorder) that high-fidelity implementation of a disorder-specific manualized treatment (e.g., Dialectical Behavior Therapy; Linehan, 2014) is virtually required for clinical success.
3.2 Empirical Justification for Distilling Core Elements of FT for ASU
For youth behavioral treatment in general, the field is beginning to investigate whether core practice elements can be clinically effective in usual care, and initial findings are quite promising. A recent randomized trial (Weisz et al., 2012) tested a core elements protocol, MATCH-ADTC (Chorpita & Weisz, 2009), containing cognitive-behavioral and parent training interventions for childhood anxiety, depression, and disruptive disorders. To counter the hazard of core elements lending themselves to countless novel combinations (Lyon & Koerner, 2016), this protocol is standardized with regard to technique specification, formulaic intervention selection, and client customization, including a flowchart with decision rules for when to delivernon-standard techniques based on evolving case circumstances. Results showed that MATCH-ADTC outperformed disorder-specific treatment manuals and usual care in promoting improvements in child outcomes (Weisz et al., 2012) and maintained its advantage over usual care at two-year follow-up (Chorpita et al., 2013). These findings were replicated in a controlled trial in Los Angeles County, where MATCH-ADTC outperformed manualized treatments for anxiety, depression, disruptive behavior, and trauma-related disorders (Chorpita et al., 2017). Moreover, ithas been associated with greater perceived benefits and satisfaction by participating therapists (Chorpita et al., 2015). Additional effectiveness evidence is provided by statewide system-of-care reforms for youth services in Hawaii (Daleiden et al., 2006; Nakamura et al., 2011), where introducing core element protocols over a 4-year period resulted in tripling the rate of improvement in child functioning, reducing average length of services episode 40-60%, and reducing average expenditures per point of outcome improvement 40%. Recent statewide dissemination initiatives for approaches like MATCH-ADTC (e.g., Southam-Gerow et al., 2014;Starin et al., 2014) have similarly demonstrated that the core elements strategy can be implemented at scalewithin public healthcare systems.
For the FT approach for ASU in particular, the dissemination shortfall of manualized FTs, combined with the dissemination advantages of core elements, beg the question: Is non-manualized FT—governed by core FT intervention principles and supported by routinely available agency resources—a viable alternative to manualized models for treating ASU in usual care? Although family-based services are commonly endorsed in youth behavioral care (Hoagwood, 2005), the potency of the FT approach in naturalistic form is virtually untested (Kaslow, Broth, Smith, & Collins, 2012). If the success of FT techniques depends fundamentally upon the implementation boost provided by manualized procedures and purveyor-driven QA, then core element FT delivered without substantial extramural support may be ineffective.
This issue was recently addressed by a randomized trial (Hogue, Dauber, Henderson, et al., 2015) that evaluated non-manualized FT delivered as routine care for ASU and comorbid disorders. Participants were 205 inner-city adolescents (mean age 15.7 years; 52% male; 59% Hispanic, 21% African American) drawn from a school- and community-based referral network; at baseline 63% reported primary mental health problems and 37% primary SU problems. Adolescents were randomly assigned to one of two study conditions: (1) Usual Care—Family Therapy (UC-FT): a single community mental health clinic that practiced non-manualized, structural-strategic family therapy as the routine standard of care for youth behavior problems; (2) Usual Care—Other (UC-Other): a group of five treatment sites that collectively represent the most common venues for treating adolescent behavior problems: two community mental health clinics, two outpatient psychiatry clinics, and one drug counseling center; no UC-Other site featured FT as a routine intervention approach.
Trial results support the effectiveness of naturalistic FT along several dimensions. The UC-FT condition showed adherence to signature techniques of the FT approach (e.g., addressing family communication and attachment, coaching multiparticipant interactions in session, targeting multiple family members for change), as well as differentiation from numerous techniques associated with alternative approaches (cognitive-behavioral therapy, motivational interviewing, drug counseling) favored inthe UC-Other condition; FT fidelity was verified via therapist self-report (Hogue, Dauber, & Henderson, 2014) and non-participant observational ratings (Hogue, Dauber, Lichvar, Bobek, & Henderson, 2015). Clinical outcomes at one-year follow-up (Hogue, Dauber, Henderson, et al., 2015) found that across the entire sample, adolescents showed significant declines in youth-reported externalizing and internalizing symptoms, caregiver-reported externalizing and internalizing symptoms, and delinquent acts. Additionally, UC-FT produced greater reductions than UC-Other in youth-reported externalizing and internalizing symptoms among the whole sample, in delinquency acts among substance-using youth, and in alcohol and drug use among substance-using youth. The trajectories of youth-reported externalizing and internalizing symptoms indicated that UC-FT youth maintained continuous declines over the course of one year, whereas declines among UC-Other youth leveled off or slightly reversed over time.
To elaborate these positive results, a follow-upstudy (Hogue et al., 2016) examined whether the UC-FT therapists achieved performance benchmarks for treatment fidelity (see Hogue, Dauber, Samuolis, & Liddle, 2006) and adolescent outcomes (see Baldwin et al., 2012) established by brand-name FTs in controlled trials for ASU and conduct problems. Perhaps surprisingly, UC-FT therapists statistically exceeded the observation-based fidelity benchmark for adherence to core FT techniques. Regarding change in client functioning at 6-month follow-up, the effect sizes achieved by UC-FT therapists for externalizing symptoms and delinquent acts were each statistically superior to the outcomes benchmark, and the effect size for internalizing symptoms was statistically equivalent (SU outcomes could not be examined due to limited sample size). And contrary to expectations about robust individual therapist differences, the twelve sampled UC-FT clinicians demonstrated a high degree of performance uniformity: Each one approximated the fidelity benchmark, and only two produced outcomes that appeared relatively weak on any change variable. Albeit from one trial only, these data attest that naturalistic FT in usual care can achieve performance standards that are squarely in line with those of manualized FTs reported in controlled trials.
These results do not certify the contention that core element FT delivered in everyday practice is clinically equivalent to brand-name FT implemented with extramural support from purveyors; such a comparison requires a randomized controlled investigation. Even so, it remains noteworthy that mainstream FT practitioners working in routine conditions can yield measurable successes in fidelity to core FT techniques and in long-term client outcomes. These results might well influence cost-benefit decisions made by government agencies that set regulatory policies and system-wide priorities for treating ASU youth: The resounding success of manualized FT is a powerful recommendation for initiating contracted services with an available purveyor. Yet, for providers and systems experiencing resource limitations, it appears legitimate to weigh the feasibility of cultivating core element FT services—perhaps factoring in upgrades to local FT supervision and quality monitoring procedures (Hogue et al., 2013)—against the barriers of importing a manualized model. With this possibility in mind, the following section details efforts to distill the core elements of FT for ASU using both conceptual and empirical methods.
4. Conceptual and Empirical Methods for Distilling the Core Elements of FT for ASU
The primary goal of distilling core practice elements of empirically supported treatments is to accumulate a roster of interventions that (1) are linked to favorable outcome data and (2) are more specific than treatment orientation and also more flexible and transdiagnostic than treatment manuals/models (Chorpita & Daleiden, 2009); see Figure 1. As discussed prior, the process of distilling core elements involves identifying discrete clinical practices contained in multiple manuals or protocols for a given clinical disorder or population. This fundamentally conceptual approach relies on expert review of the content of treatment manuals and/or published descriptions of protocols, usually fortified by team-based coding and consensus procedures among multiple reviewers (e.g., Becker et al., 2015; Chorpita et al., 2005b), and sometimes further confirmed by surveyingnational experts (e.g., Garland et al., 2008).
In the most ambitious distillation project yet undertaken, Chorpita and Daleiden (2009) reviewed 322 randomized clinical trials of behavioral interventions for children and adolescents across the psychiatric spectrum. From companion manuals and protocol descriptions they isolated 41 reliably coded practice elements variously used to treat anxiety and depression, conduct problems, attention and impulsivity, sleep and eating problems, autism-spectrum problems, substance use, and so forth. Each of these 41 distilled practices was considered “elemental”, in that the available literature offered no indication that these practices could be further parsed into lower-order or constituent components. Notably, from among the numerous trials containing a FT condition, the authors identified only one undifferentiated code that they broadly termed “family therapy”. This underscores the absence of progress to date in distilling core elements for the FT approach.
There have been several other distillation projects in the youth behavioral health arena. Becker and colleagues (2015) reviewed 40 randomized trials involving strategies for engaging youth and families in mental health services, finalizing a list of 22 core elements of treatment engagement that included service practices (e.g., promoting treatment accessibility) as well as clinical practices. Garland and colleagues (2008) reviewed the extant literature on eight treatment models with strong efficacy for treating childhood disruptive behavior and confirmed 21 core elements spanning four categories: therapeutic content, treatment technique, working alliance, and treatment parameters. Similar projects yielded a portfolio of 52 “kernel” interventions deemed principal units of behavioral influence underlying evidence-based prevention and treatment models (Embry & Biglan, 2008; see also Weisz et al., 2011), a brief protocol of common interventions in school mental health settings (Lyon et al., 2014), and a list of 24 practice elements for at risk children in early childhood settings (McLeod et al., 2016). An interesting and fundamentally different approach is the “unified” protocol, an inverse strategy in which core features are identified not for clinical interventions but instead for the targeted behavior problems; the prime example is conceptualizing negative emotionality as a singular latent syndrome underlying most anxiety and depressive disorders than can be addressed by a single protocol for adults (Barlow et al., 2010) or adolescents (Ehrenreich, Goldstein, Wright, & Barlow, 2009).
4.1 Conceptual Distillation: Examining Existing Fidelity Tools from Manualized FT Models
The FT approach for ASU is well positioned to support a conceptual distillation process with far more differentiated results than the solitary “family therapy” element isolated for the Chorpita and Daleiden (2009) taxonomy. There is ample evidence from existing research that three brand-name FT models for ASU—FFT, MDFT, BSFT—share a set of common techniques that are operationalized in their respective observational fidelity measures, are empirically linked to client outcomes, and can be readily synthesized into core practices. The FFT observational fidelity tool (Therapist Adherence Rating Scale; Ozechowki & Waldon, 2016) defineskey family interventions such as minimizing blame (Alexander, Waldron, Barton, &Mas, 1989), reframing negative behaviors (Robbins, Alexander, Newell, &Turner, 1996), and interrupting defensive interactions among family members (Robbins, Alexander, &Turner, 2000), that have been correlated with both in-session and post-treatment outcomes. The MDFT tool (Therapist Behavior Rating Scale1; Hogue et al., 1998) assesses techniques that are ubiquitous within the FT approach (e.g., coach family interactions; improve communication and attachment) and that predict long-term gains in family functioning as well as adolescent symptoms (Hogue et al., 2006; Hogue et al., 2008; Hogue, Liddle, Dauber, & Samuolis, 2004). The BSFT tool (Videotape Rating Checklist; Hervis & Robbins, 2015) also captures classic foci of the FT approach—joining, diagnostic enactment, reframing, and restructuring interventions—associated with sequence-specific effects on treatment engagement, family functioning, and adolescent symptoms (Robbins et al., 2011)2. In sum, across fidelity-outcome studies of manualized FT for ASU, common treatment techniques have emerged as “active ingredients”(Kazdin & Nock, 2003) in their respective models that reliably predict clinical gains. Moreover, these discrete techniques are fully operationalized in observational fidelity tools featured in purveyor-driven QA procedures, making these tools ideal foundations for the distillation process.
Thus, our conceptual distillation process for three brand-name FT models for ASU was grounded in examination of observational fidelity scales for each respective model. This distillation method diverges somewhat from the typical method of reviewing manuals and protocol descriptions, with the following advantage: It capitalizes on available work by model developers to operationalize manual procedures into distinct treatment techniques that are putatively essential to model adherence. That is, FT model experts have already laid bare their blueprints, creating opportunity to ascertain common structures and materials. The three fidelity scales were independently reviewed by all authors, each of whom has expertise in either FT for ASU (AH, MB, SD, CEH) or in distillation of practice elements from manualized treatments for youth behavioral disorders (BDM, MASG). The goal of the review was to inspect all three scales in order to identify thematic clinical strategies that appeared to be (1) common across the models, (2) theoretically salient to the FT approach, and (3) embodied by multiple items from all three scales. The independent reviews were then tabulated by the first two authors and re-circulated among reviewers, after which final consensus was reached.
Figure 2 depicts the results of this conceptual distillation process, which produced four core FT elements: Family Engagement, Relational Reframing, Family Behavior Change, and Family Restructuring. Figure 2 also lists the constituent treatment techniques from the three fidelity scales, ranging from 6 to 16 techniques for each core element. The first element, Family Engagement, is characterized by therapist behaviors aiming simultaneously to (1) enhance family members’ involvement and investment in treatment and (2) build the relationship between the therapist and all family members. The focus on building family member alliance with the therapist and the therapeutic process is meant to increase family engagement in every aspect of treatment. Whereas the core FT elements are intrinsically flexible, Family Engagement interventions are invariably specified by manualized FT models as taking place during the initial phase of treatment. It is worth noting that engaging family members in youth services can be extremely challenging, particularly among high-risk families (Becker et al, 2015; McKay & Bannon, 2004). For this reason manualized FTs have a longstanding commitment to promoting clinical techniques thatencourage family members to attend treatment (e.g., Santisteban et al., 1996) and to invest deeply in the treatment process (e.g., Liddle, 1995).
Figure 2.


Conceptual Distillation of Family Therapy Core Elements based on Observational Fidelity Scales for Three Empirically Supported Models for Adolescent Substance Use
*Listed numerals indicate the numbering of individual items from the respective fidelity scales.
**This scale contains 2 items that do not contribute conceptually to any of the 4 core elements.
FFT-TARS = Functional Family Therapy—Therapist Adherence Rating Scale
MDFT-TBRS = Multidimensional Family Therapy—Therapist Behavior Rating Scale
BSFT-VRC = Brief Strategic Family Therapy—Videotape Rating Checklist
The second element, Relational Reframing, consists of interventions designed to move away from individual and intrapsychic ways of defining problems and generating solutions, and towards a systemic conceptualization focused on relational processes. These interventions also aim to remove pathological descriptions and attributions for adolescents’ and other family members’ behaviors. Relational Reframe interventions seek to motivate and prepare family members to make systemic changes, that is, changes in their relationships.
In defining the third and fourth FT elements, reviewers were guided by mechanisms of change originally defined by the earliest strategic family therapy models:first- versus second-order change (Nichols & Schwartz, 1991). In first-order change, family patterns of interactions or sequences are altered at the behavioral level only, such that therapists endeavor to bring about observable shifts in actions. In second-order change, therapists instead target underlying beliefs, premises, or family rules; it is hoped that changes in these latent processes will then prompt behavior change (Watzlawick & Weakland, 1977). To take a clinical example: An adolescent and his parent may beinstructed on usingmore effective communication strategies to decrease arguing (first-order); or, they may explore and then repair relationship ruptures that have created interpersonal distance and conflict, which would in turn decrease their arguing (second-order). The clinical outcome is the same, but the processes for change are fundamentally different (Davey et al., 2011).
The third core FT element, Family Behavior Change, constitutes first-order change. These interventions aim to shift behaviors, teach concrete new skills, and encourage individual behavior changes that will allow for improved family relationships. New skills and behaviors are positively reinforced and coached, for both individuals and the entire family. The fourth element, Family Restructuring, constitutes second-order change, that is, change in the way the family system is governed. These interventions endeavor to prompt shifts in attachment and emotional processes between family members. Members are also encouraged to develop insight into predominant cycles of relational interactions, and how these cycles are linked to observable behaviors.
Though hardly exhaustive of the FT approach, these four elements specified in Figure 2 are a representative foundation of common FT strategies, as evidenced by the shared content of the fidelity tools. Just as certainly, the constituent techniqueslisted for each element do not represent the full complement of interventions prescribed by the three models; nevertheless, they are conceptually-shared interventions that have been linked to outcomes for each model and therefore hold great potential for dissemination as clinically efficacious practices. Not coincidentally, these distilled practices map closely onto the framework of the Structural Family Therapy model defined principally by Minuchin (Minuchin, 1974; Minuchin & Fishman, 1981), a common progenitor of manualized FTs for ASU and for the FT approach in general.
This focus on core elements is not intended to negate highly meaningful differences among FFT, MDFT, and BSFT in the intervention procedures delineated by each. However, it can be argued that signature differences among these models reside largely in the coordination dimension—distinctions pertaining to the timing, sequence, and relative emphasis of interventions, as well as session composition. To illustrate this point, Figure 3 maps a few examples of underlying clinical theory, model-specific coordination principles, model-specific content, and model-shared content that characterize FFT, MDFT, and BSFT as described in their respective manuals. Because all three models are examples of the “ecological” FT approach for treating ASU (Hogue et al., 2014; for “behavioral” FT models see Azrin et al., 2001; Donohue& Azrin, 2011), they share a set of cross-model theoretical foundations that governtheir dual intervention focus on family interactions and key extrafamilial systems (Becker & Curry, 2008); see the top level of Figure 3. Each model also features signature coordination principles that distinguish it from the other two, along with numerous treatment strategies and techniques (i.e., Content) that are points of unique emphasis; see the middle level. But again, many other strategies and techniques can be classified as content that is shared across the three models (common) as well as essential for treatment success (core)—that is, core practice elements; see the bottom level.
Figure 3.


Manualized FT for ASU: Sampling of Theoretical Foundations, Model Coordination, & Model Content
4.2 Empirical Distillation: Triangulating Observational Ratings from Manualized FT Sessions
Conceptual methods for distilling core elements, which center on expert review of treatment manuals and protocol content, enjoy the considerable virtues of strong face validity, modest technical demands, and flexibility in review procedures. By the same token, conceptual methods are subject to legitimate questions regarding the reliability and generalizability of distillation results: How credibly do the distilled elements represent the original EBI content? Would different groups of experts reach meaningfully different results, and if so, what are the implications for the clinical validity of the elements themselves? These questions loom largest for highly complex EBIs that resist easy disaggregation and/or reduction to simpler constructs, such as FT (Chorpita & Daleiden, 2009). As detailed above, in the case of FT for ASU our solution to these difficulties was to leverage model developers’ efforts to disaggregate their own complex treatments: In creating observational fidelity scales for their respective brand-name models, developers have already specified the key constituent elements of each.
There is also a viable, albeit more time-intensive and technically demanding, complement to conceptual distillation methods: empirical distillation via nonparticipant ratings by trained observers. Nonparticipant ratings of treatment implementation remain the gold standard for assessing treatment fidelity in both research (Hogue, Liddle, & Rowe, 1996) and front-line practice settings (Garland, Bickman, & Chorpita, 2010). In the ensuing paragraphs we detail our current study, funded by the National Institute on Drug Abuse (R01DA037496), aimed at empirically distilling core elements of FT for ASU via observational ratings of recorded sessions using the same three fidelity scales employed in our conceptual work. We believe these empirical methods could be fruitfully implemented to distill core elements from other EBIs that are similarly complex, and perhaps, to increase confidence in the validity of core practices that are, or have been, defined for virtually any treatment approach.
Phase 1 of our study involves collecting observational fidelity data on a pool of 300 recorded sessions sampled from controlled trials and purveyor training materials of FFT, MDFT, and BSFT; this is termed the gold-standard pool because all sessions are verified to be high-fidelity examples of the given model. We will conduct a fully-crossed observational analysis of gold-standard treatment sessions: All three model-specific observational fidelity measures (FFT-TARS, MDFT-TBRS, BSFT-VRC; see Figure 2) will each be used to code 100 sessions apiece from each model—that is, all 300 tapes will be coded with all three measures. We will then triangulate these fidelity ratings to derive and validate clusters of commonly implemented treatment techniques, as follows: (1) exploratory followed by confirmatory factor analyses to derive latent clusters of techniques, expecting that each derived factor will contain techniques from multiple fidelity measures; (2) analysis of the internal consistency of derived factors, expecting strong item-total correlations among techniques loading on the same factor; (3) convergent and discriminant validity analysis, expecting strong inter-item correlations among techniques representing the same factor versus weak correlations among techniques from different factors; and (4) item response quality (see Embretson & Reise, 2000) in the form of strong item discrimination properties and item parsimony on the final set of techniques identified for each factor.
Phase 2 involves confirming the derived factors of model-shared treatment techniques on a pool of 300 front-line sessions sampled from dissemination studies of community therapists delivering FT for clients with ASU and related behavioral problems. This step is critical for verifying that the factors retain conceptual and empirical coherence in the hands of end users (Lyon & Koerner, 2016). We will conduct additional observational analyses in which the treatment techniques populating the newly derived Phase 1 factors are then used to code front-line sessions, of which there will be three complementary varieties: 100 sessions from an implementation study aimed at delivering a wholesale manualized FT; 100 sessions from a treatment development studyaimed at adapting a manualized FT to address a co-occurring disorder; and 100 sessions from a naturalistic study of non-manualized FT delivered in usual care. We will analyze this second set of observational ratings using methods identical to those in Phase 1: confirmatory factor analysis to determine whether the gold-standard factors are retained in the front-line pool, followed by internal consistency, convergent and discriminant validity, and item response quality analyses of confirmed factors—thereby establishing the construct validity of the derived factors in community-based settings.
Finally, Phase 3 will establish the predictive validity of the derived factors using benchmark fidelity and outcome criteria collected on the front-line pool. First, we will use the observational fidelity data collected during Phase 2 to predict original treatment adherence scores archived for each front-line session; these adherence scores were independently collected during the original fidelity evaluation activities for each of the three samples. Second, we will use the Phase 2 ratings to predict changes in adolescent clinical functioning at one-year follow-up, focusing on substance use, externalizing and internalizing symptoms, and delinquent behaviors.
During this rigorous three-phase study process, the derived latent factors containing model-shared treatment techniques will methodically graduate as validated core elements of FT for ASU. Of course it remains to be seen whether the empirically distilled elements match—or indeed, how closely they resemble—the conceptually distilled elements proposed above. This comparison will prove instructive for assessing the added value of our empirical distillation methods, and perhaps, for prompting additional consideration of the strengths and limits of conceptual distillation methods overall.
5. Clinical Implications and Utilities of Distilling Core Elements of FT for ASU
5.1. Adopting Core Practice Elements in the Emerging Healthcare Market
For core elements to be a legitimate alternative to manualized treatment, they need to be supported by suitable companion QA procedures that promote fidelity in community settings, akinto the extensive QA systems used by manual purveyors (Hogue et al., 2013). The time is opportune for developing such procedures. The emerging healthcare market, spurred by the Affordable Care Act, is focused on establishing reliable standards for quality healthcare (Institute of Medicine, 2011). These priorities have generated nationwide mandates for increasing quality and accountability in behavioral care (Institute of Medicine, 2015), creating unprecedented opportunities to increase adoption of EBIs via training and certification requirements built into state and local contracts. As a result, effective QA procedures featuring reliable quality measures are in enormous demand (Zima et al., 2013). Despite this need, behavioral health remains woefully deficient in EBI implementation supports and metrics (Hoagwood, 2013). Arguably the biggest advance to date has been the establishment of quality indicators designed to assess broad principles of care such as appropriate treatment assignment, retention and follow-up rates, referrals for medication and ancillary care, and client safety (see Pincus, Spaeth-Rublee, &Watkins, 2011). While useful for delineating basic contours of adequate service delivery (for the latest ASU example see Bekkering et al., 2014; Cacciola et al., 2015; NIDA, 2014), such broad principles of care do not inform the selection and delivery of specific treatment techniques to meet the unique needs of individual clients (Garland et al., 2010; Garland & Schoenwald, 2013). Likewise, the quality indicators used to asses such principles can only verify if a given procedure occurred or a service quota was met; they cannot specify how procedures should be implemented or measure whether services were delivered with acceptable fidelity.
To place QA procedures and measures squarely at the center of the new behavioral healthcare market, two of the authors (McLeod et al., 2013) have proposed a theoretical model according to which research-established fidelity metrics serve as quality indicators for behavioral treatment. Figure 4 illustrates this model. The left section lists structural characteristics of care that influence both treatment implementation and outcomes, while the right section lists the multifaceted set of outcomes considered relevant within the quality of care framework. The middle section depicts the multiple elements of treatment implementation that are salient for effective delivery of EBIs, articulating both technical factors (specific interventions, therapist skill) and relational factors, given that both are related to outcomes. According to this model (see also Garland et al., 2010; Proctor et al., 2009), QA procedures for EBI implementation should be anchored by multidimensional fidelity metrics that reliably define and assess the nature and quality of services delivered. The existing vacuum in EBI quality metrics designed for front-line behavioral care can be efficiently filled in part by core practice elements that have companion QA tools, such as the electronic dashboards for case tracking and decision-making associated with MATCH-ADTC (Chorpita et al., 2008; Chorpita & Daleiden, 2014), as well as the observational fidelity scale of individual treatment techniques we plan to develop for FT for ASU (described above).
Figure 4.
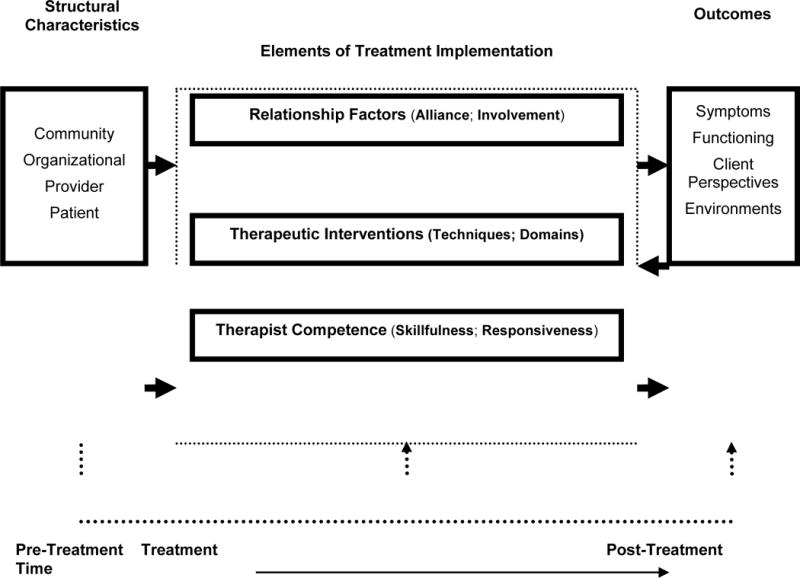
Model of Treatment Implementation within a Quality of Care Framework*
*Reprinted with permission: McLeod, B. D., Southam‐Gerow, M. A., Tully, C. B., Rodríguez, A., & Smith, M. M. (2013). Making a case for treatment integrity as a psychosocial treatment quality indicator for youth mental health care. Clinical Psychology: Science and Practice, 20, 14-32
5.2. Virtues of FT Core Elements for Treating Multi problem Youth in Multiple Settings
As argued above, the core elements strategy appears uniquely suited for facilitating delivery of FT interventions in youth behavioral health settings. Core elements offer great utility for guiding “off-map” interventions that are commonplace in usual care, such as local adaptation of EBIs for clients with unusual or boundary-condition diagnoses, and flexible combinations of techniques for clients with co-occurring disorders (Gallo & Barlow, 2012). Similarly, the relevance mapping strategy outlined by Chorpita, Bernstein, and Daleiden (2011) represents another potential application. Relevance mapping is an approach that matches the socio demographic and presenting problem characteristics in a given population of clients within an agency or system to the evidence base, thereby identifying the maximum number of those clients covered by existing EBIs, a proportion that is often in the 65-75% range. The approach also provides the smallest set of practice elements that therapists would need to deliver in order to provide appropriate services to the covered clients.
In addition, FT core elements could be implemented discretely or collectively to address the full spectrum of disruptive behavior problems in high-risk adolescents—SU, delinquency, aggression, conduct disorder—for which manualized FTs have proven effective (Baldwin et al., 2012; Henggeler & Sheidow, 2012; McCart & Sheidow, 2016). In this way FT core elements would be a new resource for community clinicians to supplement treatment planning and family involvement efforts for high-risk, hard-to-engage adolescents across the board. FT core elements can therefore be a credible (though only partial) solution to the urgent demand for adaptable, transdiagnostic interventions capable of treating multiproblem youth involved in multiple systems of care (Hawkins, 2009; Kazak et al., 2010).
Looking forward, widespread adoption of FT core elements could also lay a sturdy foundation for the next generation of FT dissemination and training initiatives (e.g., web-based; virtual reality; distance learning; see Weingardt, 2004) intended to grow new competencies in novice family therapists and boost expertise in trained therapists within core areas of family-based work (Celano, Smith, & Kaslow, 2010). Widespread adoption of FT core elements, or for that matter the core elements of any empirically supported approach, could also produce recursive benefits for disseminating manualized treatments. Clinicians who are inexperienced or otherwise unfamiliar with manual-based EBIs are often under-motivated or unprepared to adopt treatment manuals (Gallo & Barlow, 2012). Learning first to deliver core elements with fidelity and confidence may well pave the way for these clinicians to eventually take up wholesale manuals in their routine practices, thereby upgrading the overall quality of available services.
Acknowledgments
Aaron Hogue, Ph.D., Molly Bobek, LCSW, and Sarah Dauber, Ph.D., National Center on Addiction and Substance Abuse; Craig E. Henderson, Department of Psychology, Sam Houston State University; Bryce D. McLeod, Ph.D. and Michael A. Southam-Gerow, Ph.D., Department of Psychology, Virginia Commonwealth University.
Preparation of this article was supported by the National Institute on Drug Abuse (R01DA037496; PI: Hogue). The authors would like to thank Bruce Chorpita, Olga Hervis, Silvia Kaminsky, Michael Robbins, Ashli Sheidow, and Holly Waldron for their invaluable contributions to the ideas presented.
Footnotes
In recent years the MDFT purveyor organization developed a revised observational fidelity tool to promote MDFT dissemination and implementation, the MDFT Intervention Inventory (Rowe et al., 2013), that is more model-specific than the Therapist Behavior Rating Scale.
The self-report fidelity measures utilized in MST studies (see Henggeler, Pickrel, & Brondino, 1999; Schoenwald, Sheidow, & Letourneau, 2004) assess global intervention principles rather than discrete treatment techniques and thus do not lend themselves to core element distillation.
Contributor Information
Aaron Hogue, National Center on Addiction and Substance Abuse.
Molly Bobek, National Center on Addiction and Substance Abuse.
Sarah Dauber, National Center on Addiction and Substance Abuse.
Craig E. Henderson, Sam Houston State University
Bryce D. McLeod, Virginia Commonwealth University
Michael A. Southam-Gerow, Virginia Commonwealth University
References
- Aarons GA, Sommerfeld D, Hecht D, Silovsky J, Chaffin M. The impact of evidence-based practice implementation and fidelity monitoring on staff turnover: Evidence for a protective effect. Journal of Consulting & Clinical Psychology. 2009;77:270–280. doi: 10.1037/a0013223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addis ME, Krasnow AD. A national survey of practicing psychologists’ attitudes towards psychotherapy treatment manuals. Journal of Consulting & Clinical Psychology. 2000;68:331–339. doi: 10.1037//0022-006x.68.2.331. [DOI] [PubMed] [Google Scholar]
- Addis ME, Wade WA, Hatgis C. Barriers to dissemination of evidence-based practices: Addressing practitioners’ concerns about manual-based psychotherapies. Clinical Psychology: Science and Practice. 1999;6:430–441. [Google Scholar]
- Alexander JF, Waldron HB, Barton C, Mas CH. Minimizing blaming attributions and behaviors in deliquent families. Journal of Consulting and Clinical Psychology. 1989;57:19–24. doi: 10.1037//0022-006x.57.1.19. [DOI] [PubMed] [Google Scholar]
- American Academy of Child and Adolescent Psychiatry. Practice parameters for the assessment and treatment of children and adolescents with substance use disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:140–156. doi: 10.1097/00004583-199710001-00009. [DOI] [PubMed] [Google Scholar]
- Azrin NH, Donohue B, Teichner G, Crum T, Howell J, DeCato L. A controlled evaluation and description of individual-cognitive problem solving and family-behavioral therapies in conduct-disordered and substance dependent youth. Journal of Child and Adolescent Substance Abuse. 2001;11:1–43. [Google Scholar]
- Baldwin SA, Christian S, Berkeljon A, Shadish WR. The effects of family therapies for adolescent delinquency and substance abuse: A meta-analysis. Journal of Marital and Family Therapy. 2012;38:281–304. doi: 10.1111/j.1752-0606.2011.00248.x. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Farchione TJ, Fairholme CP, Ellard KK, Boisseau CL, Allen LB, Ehrenreich-May JT. Unified protocol for transdiagnostic treatment of emotional disorders: Therapist guide. Oxford University Press; 2010. [Google Scholar]
- Barth RP, Kolivoski KM, Lindsey MA, Lee BR, Collins KS. Translating the common elements approach: Social work’s experiences in education, practice, and research. Journal of Clinical Child & Adolescent Psychology. 2014;43:301–311. doi: 10.1080/15374416.2013.848771. [DOI] [PubMed] [Google Scholar]
- Becker SJ, Curry J. Outpatient interventions for adolescent substance abuse: A quality of evidence review. Journal of Consulting & Clinical Psychology. 2008;76:531–543. doi: 10.1037/0022-006X.76.4.531. [DOI] [PubMed] [Google Scholar]
- Becker KD, Lee BR, Daleiden EL, Lindsey M, Brandt NE, Chorpita BF. The common elements of engagement in children’s mental health services: Which elements for which outcomes? Journal of Clinical Child & Adolescent Psychology. 2015;44:30–43. doi: 10.1080/15374416.2013.814543. [DOI] [PubMed] [Google Scholar]
- Bekkering GE, Aertgeerts B, Asueta‐Lorente JF, Autrique M, Goossens M, Smets K, Hannes K. Practitioner Review: Evidence‐based practice guidelines on alcohol and drug misuse among adolescents: a systematic review. Journal of Child Psychology and Psychiatry. 2014;55:3–21. doi: 10.1111/jcpp.12145. [DOI] [PubMed] [Google Scholar]
- Blue Cross. Behavioral Health Medical Necessity Critreia, Office of Medical Policy and Technological Assessment (OMPTA), Anthem Blue Cross. Woodland Hills, CA: 2013. Retrieved from. [Google Scholar]
- Borntrager C, Chorpita BF, Higa-McMillan C, Weisz JR. Provider attitudes toward evidence-based practice: Are the concerns with the evidence or with the manuals? Psychiatric Services. 2009;60:677–81. doi: 10.1176/ps.2009.60.5.677. [DOI] [PubMed] [Google Scholar]
- Cacciola JS, Meyers K, Ward S, Rosenwasser B, Arria A, McLellan AT. Assessing adolescent substance abuse programs with updated quality indicators: The development of a consumer guide for adolescent treatment. Journal of Child & Adolescent Substance Abuse. 2015;24:142–154. doi: 10.1080/1067828X.2013.777378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Kadden RM, Donovan DM, Zweben A, Rounsaville BJ. Implementing treatment and protecting the validity of the independent variable in treatment matching studies. Journal of Studies in Alcohol. 1994;12:149–55. doi: 10.15288/jsas.1994.s12.149. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ. Behavioral therapies: The glass would be half full if only we had a glass. In: Miller WR, Carroll KM, editors. Rethinking Substance Abuse: What the Science Shows and What We Should Do About It. New York: Guilford; 2006. [Google Scholar]
- Celano MP, Smith CO, Kaslow NJ. A competency-based approach to couple and family therapy supervision. Psychotherapy: Theory, Research, Practice, Training. 2010;47:35–44. doi: 10.1037/a0018845. [DOI] [PubMed] [Google Scholar]
- Center for Substance Abuse Treatment. Treatment of Adolescents with Substance Use Disorders. Rockville, MD: 1999. (Treatment Improvement Protocol (TIP) Series, no 32. DHHS publication no. (SMA) 99-3283). [Google Scholar]
- Chambers D, Ringeisen H, Hickman E. Federal, state, and foundation initiatives around evidence-based practices for child and adolescent mental health. Child and Adolescent Mental Health. 2005;14:307–327. doi: 10.1016/j.chc.2004.04.006. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Becker KD, Daleiden EL. Understanding the common elements of evidence-based practice: Misconceptions and clinical examples. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46:647–652. doi: 10.1097/chi.0b013e318033ff71. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Bernstein A, Daleiden EL, Research Network on Youth Mental Health Driving with roadmaps and dashboards: Using information resources to structure the decision models in service organizations. Administration and Policy in Mental Health and Mental Health Services Research. 2008;35:114–123. doi: 10.1007/s10488-007-0151-x. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Bernstein A, Daleiden EL. Empirically guided coordination of multiple evidence-based treatments: An illustration of relevance mapping in children’s mental health services. Journal of Consulting and Clinical Psychology. 2011;79:470–80. doi: 10.1037/a0023982. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL. Mapping evidence-based treatments for children and adolescents: Application of the distillation and matching model to 615 treatments from 322 randomized trials. Journal of Consulting & Clinical Psychology. 2009;77:566–579. doi: 10.1037/a0014565. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL. Structuring the collaboration of science and service in pursuit of a shared vision. Journal of Clinical Child & Adolescent Psychology. 2014;43:323–338. doi: 10.1080/15374416.2013.828297. [DOI] [PubMed] [Google Scholar]
- Chorpita B, Daleiden E, Ebesutani C, Young J, Becker K, Starace N. Evidence-based treatments for children and adolescents: An updated review of indicators of efficacy and effectiveness. Clinical Psychology: Science and Practice. 2011;18:154–172. [Google Scholar]
- Chorpita BF, Daleiden EL, Park AL, Ward AM, Levy MC, Cromley T, Krull JL. Child STEPs in California: A cluster randomized effectiveness trial comparing modular treatment with community implemented treatment for youth with anxiety, depression, conduct problems, or traumatic stress. Journal of consulting and clinical psychology. 2017;85(1):13. doi: 10.1037/ccp0000133. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Daleiden EL, Weisz JR. Modularity in the design and application of therapeutic interventions. Applied & Preventive Psychology. 2005a;11:141–156. [Google Scholar]
- Chorpita BF, Daleiden EL, Weisz JR. Identifying and selecting the common elements of evidence based interventions: A distillation and matching model. Mental Health Services Research. 2005b;7:5–20. doi: 10.1007/s11020-005-1962-6. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Park A, Tsai K, Korathu-Larson P, Higa-McMillan CK, Nakamura BJ, Krull J. Balancing effectiveness with responsiveness: Therapist satisfaction across different treatment designs in the Child STEPs randomized effectiveness trial. Journal of Consulting and Clinical Psychology. 2015;83:709–718. doi: 10.1037/a0039301. [DOI] [PubMed] [Google Scholar]
- Chorpita BF, Weisz JR. Modular approach to therapy for children with anxiety, depression, trauma, or conduct problems (MATCH-ADTC) 2009 Proprietary material: http://www.practicewise.com/portals/0/MATCH_public/index.html.
- Chorpita BF, Weisz JR, Daleiden EL, Schoenwald SK, Palinkas LA, Miranda J, Research Network on Youth Mental Health Long-term outcomes for the Child STEPs randomized effectiveness trial: A comparison of modular and standard treatment designs with usual care. Journal of Consulting and Clinical Psychology. 2013;81:999–1009. doi: 10.1037/a0034200. [DOI] [PubMed] [Google Scholar]
- Cigna. Level of Care Guidelines, Cigna Medical Necessity Criteria for Treatment of Behavioral Health and Substance Use Disorders 2012 [Google Scholar]
- Cook JM, Biyanova T, Elhai J, Schnurr PP, Coyne JC. What do psychotherapists really do in practice? An internet study of over 2,000 practitioners. Psychotherapy: Theory, Research, Practice, Training. 2010;47:260–267. doi: 10.1037/a0019788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daleiden EL, Chorpita BF. From data to wisdom: Quality improvement strategies supporting large-scale implementation of evidence-based services. Child and Adolescent Psychiatric Clinics of North America. 2005;14:329–349. doi: 10.1016/j.chc.2004.11.002. [DOI] [PubMed] [Google Scholar]
- Daleiden EL, Chorpita BF, Donkervoet C, Arensdorf AM, Brogan M. Getting better at getting them better: Health outcomes and evidence-based practice within a system of care. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45:749–756. doi: 10.1097/01.chi.0000215154.07142.63. [DOI] [PubMed] [Google Scholar]
- Davey M, Duncan T, Kissil K, Davey A, Fish LS. Second-order change in marriage and family therapy: A web-based modified Delphi study. American Journal of Family Therapy. 2011;39:100–111. [Google Scholar]
- Donohue B, Azrin NH. Family behavior therapy: A step-by-step approach to adolescent substance abuse. Hoboken, NJ: John Wiley & Sons; 2011. [Google Scholar]
- Drug Strategies. Treating teens: A guide to adolescent drug programs. Washington, DC: 2003. [Google Scholar]
- Ehrenreich JT, Goldstein CR, Wright LR, Barlow DH. Development of a unified protocol for the treatment of emotional disorders in youth. Child & Family Behavior Therapy. 2009;31:20–37. doi: 10.1080/07317100802701228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Embretson S, Reise S. Item response theory for psychologists. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. [Google Scholar]
- Embry DD, Biglan A. Evidence-based kernels: Fundamental units of behavioral influence. Clinical Child and Family Psychology Review. 2008;11:75–113. doi: 10.1007/s10567-008-0036-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallo KP, Barlow DH. Factors involved in clinician adoption and nonadoption of evidence‐based interventions in mental health. Clinical Psychology: Science and Practice. 2012;19:93–106. [Google Scholar]
- Garland AF, Bickman L, Chorpita BF. Change what? Identifying quality improvement targets by investigating usual mental health care. Administration and Policy in Mental Health and Mental Health Services Research. 2010;37:15–26. doi: 10.1007/s10488-010-0279-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland AF, Hawley KM, Brookman-Frazee LI, Hurlburt M. Identifying common, core elements of evidence-based practice for children with disruptive behavior disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:505–514. doi: 10.1097/CHI.0b013e31816765c2. [DOI] [PubMed] [Google Scholar]
- Garland AF, Hurlburt MS, Hawley KM. Examining psychotherapy process in a services research context. Clinical Psychology: Science and Practice. 2006;13:30–46. [Google Scholar]
- Garland AF, Schoenwald SK. Use of effective and efficient quality control methods to implement psychosocial interventions. Clinical Psychology: Science and Practice. 2013;20:33–43. [Google Scholar]
- Gifford EV, Tavakoli S, Weingardt KR, Finney JW, Pierson HM, et al. How do components of evidence-based psychological treatment cluster in practice?: A survey and cluster analysis. Journal of Substance Abuse Treatment. 2012;42:45–55. doi: 10.1016/j.jsat.2011.07.008. [DOI] [PubMed] [Google Scholar]
- Glisson C. The organizational context of children’s mental health services. Clinical Child and Family Psychology Review. 2002;5:233–253. doi: 10.1023/a:1020972906177. [DOI] [PubMed] [Google Scholar]
- Godley SH, Garner BR, Smith JE, Meyers RJ, Godley MD. A large scale dissemination and implementation model for evidence-based treatment and continuing care. Clinical Psychology: Science and Practice. 2011;18:67–83. doi: 10.1111/j.1468-2850.2011.01236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins EH. A tale of two systems: Co-occurring mental health and substance abuse disorders treatment for adolescents. Annual Review of Psychology. 2009;60:197–227. doi: 10.1146/annurev.psych.60.110707.163456. [DOI] [PubMed] [Google Scholar]
- Hayes SC. Getting to dissemination. Clinical Psychology: Science and Practice. 2002;9:410–415. [Google Scholar]
- Henggeler SW, Pickrel SG, Brondino MJ. Multisystemic treatment of substance abusing and dependent delinquents: Outcomes, treatment fidelity, and transportability. Mental Health Services Research. 1999;1:171–184. doi: 10.1023/a:1022373813261. [DOI] [PubMed] [Google Scholar]
- Henggeler SW, Sheidow AJ. Empirically supported family‐based treatments for conduct disorder and delinquency in adolescents. Journal of Marital and Family Therapy. 2012;38:30–58. doi: 10.1111/j.1752-0606.2011.00244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hervis OE, Robbins MS. Brief Strategic Family Therapy Videotape Rating Checklist. Family Therapy Training Institute of Miami; 2015. [Google Scholar]
- Hoagwood K. Family-based services in children’s mental health: A research review and synthesis. Journal of Child Psychology and Psychiatry. 2005;46:690–713. doi: 10.1111/j.1469-7610.2005.01451.x. [DOI] [PubMed] [Google Scholar]
- Hoagwood KE. Don’t mourn: Organize. Reviving mental health services research for healthcare quality improvement. Clinical Psychology: Science and Practice. 2013;20:120–126. [Google Scholar]
- Hogue A. When technology fails: Getting back to nature. Clinical Psychology: Science and Practice. 2010;17:77–81. doi: 10.1111/j.1468-2850.2009.01196.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Dauber S, Henderson CE. Therapist self-report of evidence-based practices in usual care for adolescent behavior problems: Factor and construct validity. Administration and Policy in Mental Health and Mental Health Services Research. 2014;41:126–139. doi: 10.1007/s10488-012-0442-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Dauber S, Henderson CE. Benchmarking family therapy for adolescent behavior problems in usual care: Fidelity, outcomes, and therapist performance differences. Administration and Policy in Mental Health and Mental Health Services Research. 2016 doi: 10.1007/s10488-016-0769-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Dauber S, Henderson CE, Bobek M, Johnson C, Lichvar E, Morgenstern J. Randomized trial of family therapy versus non-family treatment for adolescent behavior problems in usual care. Journal of Clinical Child and Adolescent Psychology. 2015;44:954–969. doi: 10.1080/15374416.2014.963857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Dauber S, Lichvar E, Bobek M, Henderson CE. Validity of therapist self-report ratings of fidelity to evidence-based practices for adolescent behavior problems: Correspondence between therapists and observers. Administration and Policy in Mental Health and Mental Health Services Research. 2015;42:229–243. doi: 10.1007/s10488-014-0548-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Dauber S, Samuolis J, Liddle HA. Treatment techniques and outcomes in multidimensional family therapy for adolescent behavior problems. Journal of Family Psychology. 2006;20:535–543. doi: 10.1037/0893-3200.20.4.535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Henderson CE, Dauber S, Barajas PC, Fried A, Liddle HA. Treatment adherence, competence, and outcome in individual and family therapy for adolescent behavior problems. Journal of Consulting and Clinical Psychology. 2008;76:544–555. doi: 10.1037/0022-006X.76.4.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Henderson CE, Ozechowski TJ, Robbins MS. Evidence base on outpatient behavioral treatments for adolescent substance use: Updates and recommendations 2007-2013. Journal of Clinical Child and Adolescent Psychology. 2014;43:697–720. doi: 10.1080/15374416.2014.915550. [DOI] [PubMed] [Google Scholar]
- Hogue A, Liddle H. Family-based treatment for adolescent substance abuse: Controlled trials and new horizons in services research. Journal of Family Therapy. 2009;31:126–154. doi: 10.1111/j.1467-6427.2009.00459.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Liddle HA, Dauber S, Samuolis J. Linking session focus to treatment outcome in evidence-based treatments for adolescent substance abuse. Psychotherapy: Theory, Research, Practice, & Training. 2004;41:83–96. doi: 10.1037/0033-3204.41.2.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Liddle HA, Rowe CL. Treatment adherence process research in family therapy: A rationale and some practical guidelines. Psychotherapy: Theory, Research, Practice, & Training. 1996;33:332–345. [Google Scholar]
- Hogue A, Liddle HA, Rowe CL, Turner RM, Dakof GA, LaPann K. Treatment adherence and differentiation in individual versus family therapy for adolescent substance abuse. Journal of Counseling Psychology. 1998;45:104–114. [Google Scholar]
- Hogue A, Ozechowski TJ, Robbins MS, Waldron HB. Making fidelity an intramural game: Localizing quality assurance procedures to promote sustainability of evidence-based practices in usual care. Clinical Psychology: Science and Practice. 2013;20:60–77. [Google Scholar]
- Hurlburt MS, Garland AF, Nguyen K, Brookman-Frazee L. Child and family therapy process: Concordance of therapist and observational perspectives. Administration and Policy in Mental Health and Mental Health Services Research. 2010;37:230–244. doi: 10.1007/s10488-009-0251-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Psychosocial interventons for mental and substance use disorders: A framework for establishing evidence-based standards. Washington, DC: National Academies Press; 2015. [PubMed] [Google Scholar]
- Institute of Medicine. The looming expansion and transformation of public substance abuse treatment under the Affordable Care Act. Health Affairs. 2011;30:1402–1410. doi: 10.1377/hlthaff.2011.0480. [DOI] [PubMed] [Google Scholar]
- Jensen-Doss A. Practical, evidence-based clinical decision making: Introduction to the Special Section on Evidence-based Assessment. Cognitive & Behavioral Practice. 2015;22:1–4. [Google Scholar]
- Kaslow NJ, Broth MR, Smith CO, Collins MH. Family-based interventions for child and adolescent disorders. Journal of Marital and Family Therapy. 2012;38:82–100. doi: 10.1111/j.1752-0606.2011.00257.x. [DOI] [PubMed] [Google Scholar]
- Kazak AE, Hoagwood K, Weisz JR, Hood K, Kratochwill TR, Vargas LA, Banez GA. A meta-systems approach to evidence-based practice for children and adolescents. American Psychologist. 2010;65:85–97. doi: 10.1037/a0017784. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Current (lack of) status of theory in child and adolescent psychotherapy research. Journal of Child Clinical Psychology. 1999;28:533–543. doi: 10.1207/S15374424JCCP2804_13. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendations. Journal of Child Psychology and Psychiatry. 2003;44:1116–1129. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- Knudsen H, Ducharme L, Roman P. Clinical supervision, emotional exhaustion, and turnover intention: A study of substance abuse treatment counselors in the Clinical Trials Network of the National Institute on Drug Abuse. Journal of Substance Abuse Treatment. 2008;35:387–95. doi: 10.1016/j.jsat.2008.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberman RP, Corrigan PW. Implementing and Maintaining Behavior Therapy Programs: Behavior Therapy in Psychiatric Hospitals. New York: Springer; 1994. [Google Scholar]
- Liddle HA. Conceptual and clinical dimensions of a multidimensional, multisystems engagement strategy in family-based adolescent treatment. Psychotherapy: Theory, Research, and Training. 1995;32:39–58. [Google Scholar]
- Linehan MM. DBT® skills training manual. Guilford Publications; 2014. [Google Scholar]
- Lyon AR, Bruns EJ, Weathers ES, Canavas N, Ludwig K, Vander Stoep A, McCauley E. Taking evidence-based practices to school: Using expert opinion to develop a brief, evidence-informed school-based mental health intervention. Advances in School Mental Health Promotion. 2014;7:42–61. [Google Scholar]
- Lyon AR, Koerner K. User‐centered design for psychosocial intervention development and implementation. Clinical Psychology: Science and Practice. 2016;23:180–200. doi: 10.1111/cpsp.12154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill M, Apodaca TR, Walthers J, Gaume J, Durst A, Longabaugh R, Carroll KM. The Alcohol Intervention Mechanisms Scale (AIMS): Preliminary reliability and validity of a common factor observational rating measure. Journal of Substance Abuse Treatment. 2016;70:28–34. doi: 10.1016/j.jsat.2016.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCart MR, Sheidow AJ. Evidence-based psychosocial treatments for adolescents with disruptive behavior. Journal of Clinical Child & Adolescent Psychology. 2016;45:529–563. doi: 10.1080/15374416.2016.1146990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh R, Barlow DH. The dissemination and implementation of evidence-based psychological treatment: A review of current efforts. American Psychologist. 2010;65:73–84. doi: 10.1037/a0018121. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Murray HW, Barlow DH. Balancing fidelity and adaptation in the dissemination of empirically-supported treatments: The promise of transdiagnostic interventions. Behaviour Research and Therapy. 2009;47:946–953. doi: 10.1016/j.brat.2009.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay MM, Bannon WM. Engaging families in child mental health services. Child and Adolescent Psychiatric Clinics of North America. 2004;13:905–921. doi: 10.1016/j.chc.2004.04.001. [DOI] [PubMed] [Google Scholar]
- McLeod BD, Southam‐Gerow MA, Tully CB, Rodríguez A, Smith MM. Making a case for treatment integrity as a psychosocial treatment quality indicator for youth mental health care. Clinical Psychology: Science and Practice. 2013;20:14–32. doi: 10.1111/cpsp.12020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod BD, Sutherland KS, Martinez RG, Conroy MA, Snyder PA, Southam-Gerow MA. Prevention Science. Advanced online publication; 2016. Identifying common practice elements to improve social, emotional, and behavioral outcomes of young children in early childhood classrooms. [DOI] [PubMed] [Google Scholar]
- Minuchin S. Families and family therapy. Camridge, MA: Harvard University Press; 1974. [Google Scholar]
- Minuchin S, Fishman HC. Family therapy techniques. Cambridge, MA: Harvard University Press; 1981. [Google Scholar]
- Nakamura BJ, Chorpita BF, Hirsch M, Daleiden EL, Slavin L, Amundson M, et al. Large‐scale implementation of evidence‐based treatments for children 10 years later: Hawaii’s evidence‐based services initiative in children’s mental health. Clinical Psychology: Science and Practice. 2011;18:24–35. [Google Scholar]
- Nichols MP, Schwartz RC. Family therapy: Cocnepts and methods. 2nd. Boston: Allyn and Bacon; 1991. [Google Scholar]
- NIDA. Principles of adolescent substance use disorder treatment: A research-based guide. Bethesda, MD: NIH; 2014. (National Institute on Drug Abuse, National institutes of Health; NIH publication Number 14-7953). [Google Scholar]
- Ozechowski TJ, Waldron HB. Functional Family Therapy Therapist Adherence Rating Scale. Oregon Research Institute; 2016. Instrument available from the authors. [Google Scholar]
- Oxford. Clinical Policy, Behavioral Health Services. United Healthcare; 2013. [Google Scholar]
- Pincus HA, Spaeth-Rublee B, Watkins KE. Analysis & commentary: The case for measuring quality in mental health and substance abuse care. Health Affairs. 2011;30:730–736. doi: 10.1377/hlthaff.2011.0268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proctor EK, Landsverk J, Aarons G, Chambers D, Glisson C, Mittman B. Implementation research in mental health services: An emerging science with conceptual, methodological, and training challenges. Administration and Policy in Mental Health and Mental Health Services Research. 2009;36:24–34. doi: 10.1007/s10488-008-0197-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramchand R, Griffin BA, Suttorp M, Harris KM, Morral A. Using a cross-study design to assess the efficacy of motivational enhancement therapy-cognitive behavioral therapy 5 (MET/CBT5) in treating adolescents with cannabis-related disorders. Journal of Studies on Alcohol and Drugs. 2011;72:380–389. doi: 10.15288/jsad.2011.72.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robbins MS, Alexander JF, Newell RM, Turner CW. The immediate effect of reframing on client attitude in family therapy. Journal of Family Psychology. 1996;10:28–34. [Google Scholar]
- Robbins MS, Alexander JF, Turner CW. Disrupting defensive interactions in family therapy with delinquent adolescents. Journal of Family Psychology. 2000;14:688–701. doi: 10.1037//0893-3200.14.4.688. [DOI] [PubMed] [Google Scholar]
- Robbins MS, Feaster D, Horigian V, Puccinelli M, Henderson CE, Szapocznik J. Therapist adherence in Brief Strategic Family Therapy for adolescent drug abusers. Journal of Consulting & Clinical Psychology. 2011;79:43–53. doi: 10.1037/a0022146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Swendeman D, Chorpita BF. Disruptive innovations for designing and diffusing evidence-based interventions. American Psychologist. 2012;67:463. doi: 10.1037/a0028180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe CL. Family therapy for drug abuse: review and updates 2003–2010. Journal of Marital and Family Therapy. 2012;38:59–81. doi: 10.1111/j.1752-0606.2011.00280.x. [DOI] [PubMed] [Google Scholar]
- Rowe CL, Rigter H, Henderson CE, Gantner A, Mos K, Nielsen P, Phan O. Implementation fidelity of Multidimensional Family Therapy in an international trial. Journal of Substance Abuse Treatment. 2013;44:391–399. doi: 10.1016/j.jsat.2012.08.225. [DOI] [PubMed] [Google Scholar]
- Santisteban DA, Szapocznik J, Perez-Vidal A, Kurtines WM, Murray EJ, LaPerriere A. Efficacy of intervention for engaging youth and families into treatment and some variables that may contribute to differential effectiveness. Journal of Family Psychology. 1996;10:35–44. [Google Scholar]
- Schoenwald SK, Chapman JE, Kelleher K, Hoagwood KE, Landsverk J, Stevens J, Research Network on Youth Mental Health A survey of the infrastructure for children’s mental health services: Implications for the implementation of empirically supported treatments (ESTs) Administration and Policy in Mental Health and Mental Health Services Research. 2008;35:84–97. doi: 10.1007/s10488-007-0147-6. [DOI] [PubMed] [Google Scholar]
- Schoenwald SK, Sheidow AJ, Letourneau EJ. Toward effective quality assurance in evidence-based practice: Link between expert consultation, therapist fidelity, and child outcomes. Journal of Clinical Child and Adolescent Psychology. 2004;33:94–104. doi: 10.1207/S15374424JCCP3301_10. [DOI] [PubMed] [Google Scholar]
- Southam-Gerow MA, Daleiden EL, Chorpita BF, Bae C, Mitchell C, Faye M, Alba M. MAPping Los Angeles County: Taking an evidence-informed model of mental health care to scale. Journal of Clinical Child & Adolescent Psychology. 2014;43:190–200. doi: 10.1080/15374416.2013.833098. [DOI] [PubMed] [Google Scholar]
- Starin AC, Atkins MS, Wehrmann KC, Mehta T, Hesson-McInnis MS, Marinez-Lora A, Mehlinger R. Moving science into state child and adolescent mental health systems: Illinois’ evidence-informed practice initiative. Journal of Clinical Child & Adolescent Psychology. 2014;43:169–178. doi: 10.1080/15374416.2013.848772. [DOI] [PubMed] [Google Scholar]
- State of New York. New York State Office of Alcoholism and Substance Abuse Services (OASAS) Statewide Comprehensive Service Plan: 2010-2014 2010 [Google Scholar]
- State of Pennsylvania. Supporting the Journey: Transforming Pennsylvania’s Behavioral Health System Office of Mental Health and Substance Abuse Services, Pennsylvania Department of Public Welfare 2010 [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Intervention summaries: Multisystemic Therapy for Juvenile Offenders, Brief Strategic Family Therapy, & Multidimensional Family Therapy. Rockville, MD: Govt Printing Office (SAMHSA); 2012. National Registry of Evidence-based Programs and Practices (NREPP) [Google Scholar]
- Tanner-Smith EE, Wilson SJ, Lipsey MW. The comparative effectiveness of outpatient treatment for adolescent substance abuse: a meta-analysis. Journal of Substance Abuse Treatment. 2013;44:145–158. doi: 10.1016/j.jsat.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward AM, Regan J, Chorpita BF, Starace N, Rodriguez A, Okamura K, Daleiden EL, Bearman S, Weisz JR. Tracking evidence based practice with youth: Validity of MATCH and standard manual consultation records. Journal of Clinical Child and Adolescent Psychology. 2013;42:44–55. doi: 10.1080/15374416.2012.700505. [DOI] [PubMed] [Google Scholar]
- Watzlawick P, Weakland JH. The interactional view. New York: Norton; 1977. [Google Scholar]
- Weingardt KR. The role of instructional design and technology in the dissemination of empirically supported, manual-based therapies. Clinical Psychology: Science and Practice. 2004;11:313–331. [Google Scholar]
- Weisz JR, Chorpita BF, Palinkas LA, Schoenwald SK, Miranda J, Bearman SK, et al. Testing standard and modular designs for psychotherapy treating depression, anxiety, and conduct problems in youth: A randomized effectiveness trial. Archives of General Psychiatry. 2012;69:274–282. doi: 10.1001/archgenpsychiatry.2011.147. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Ugueto AM, Herren J, Afienko SR, Rutt C. Kernels vs. ears, and other questions for a science of treatment dissemination. Clinical Psychology: Science and Practice. 2011;18:41–46. doi: 10.1111/j.1468-2850.2010.01233.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Westen D, Novotny CM, Thompson-Brenner H. EBP does not equal EST: Reply to Crits-Cristoph et al. (2005) and Weisz et al. (2005) Psychological Bulletin. 2005;131:427–433. [Google Scholar]
- Zima BT, Murphy JM, Scholle SH, Hoagwood KE, Sachdeva RC, Mangione-Smith R, Jellinek M. National quality measures for child mental health care: background, progress, and next steps. Pediatrics. 2013;131(Supplement 1):S38–S49. doi: 10.1542/peds.2012-1427e. [DOI] [PMC free article] [PubMed] [Google Scholar]


