Abstract
Objective:
The aim of this study is to evaluate, through a systematic review of hospital based studies, the proportion of road traffic injuries and fatalities in SSA.
Methods:
In accordance with PRISMA and MOOSE guidelines we searched the following electronic databases: PubMed, Embase, Africa-Wide Information, Global Health, and Web of Science. Articles were eligible if they measured proportion of RTIs in SSA by using hospital based studies. In addition, a reference and citation analysis was conducted as well as a data quality assessment.
Results:
Until to 2015 there were a total of 83 hospital based epidemiologic studies including 310,660 trauma patients and 99,751 RTI cases, in 13 SSA countries. The median proportion of RTI among trauma patients was 32% (4% to 91%), of those the median proportion of death for the included articles was 5% (0.3% to 41%).
Conclusion:
The number of studies evaluating RTI proportion and fatalities in SSA countries is increasing but without the exponential rise expected from WHO calls for research during the “Decade of Action for Road Traffic Injuries.” Further research infrastructure including standardization of taxonomy, definitions, and data reporting measures, as well as funding, would allow for improved cross-country comparisons.
Keywords: proportion, Road Traffic Injury, Sub Saharan Africa
INTRODUCTION
As of 2010, road traffic injuries (RTIs) were the eighth leading cause of death (Lozano et al. 2012), and by 2020, they are predicted to become the third leading cause of death.(Peden et al. 2004) Between 1990 and 2010 there was a 46% rise in worldwide deaths due to road traffic crashes (RTCs).(Peden et al. 2004) A disproportionate burden of RTIs rests on low- and middle-income countries (LMIC), which have seen a precipitous increase, while high-income countries have actually seen a decrease.(Peden et al. 2004) This disparity is expected to widen, and by 2020, it is predicted that road traffic deaths in LMIC will increase by 83% while decreasing by 27% in high-income countries.(Peden et al. 2004) Africa has the highest RTI death rate in the world; here, RTIs are expected to become the number one cause of death for children 5 −15 years of age in the near future and the number two leading cause of premature death in young men after HIV/AIDS.(Marquez et al. 2013) The endemic problem of RTIs disproportionately affecting the socioeconomically disadvantaged in sub-Saharan Africa (SSA) is exacerbated by the limited access to healthcare and limited resources and infrastructure to adequately respond to this problem.(Peden et al. 2004) Moreover, the loss of the main wage earner due to a RTI can be crippling to an entire family, and thus also represents a serious social and economic crisis.
In order to appropriately address and attempt to lessen the burden of RTIs in SSA, it is important to first systematically study the proportion, number and economic burden of road traffic injuries and fatalities. However, the most complete reporting and data sets on RTIs come from high-income countries, whereas in SSA, there is a paucity of comprehensive datasets.(Ameratunga et al. 2006)(Chokotho et al. 2013)(Labinjo et al. 2009)(Salifu et al. 2012)(Murray et al. 1996)(Peden et al. 2004)(Samuel et al. 2012) Recently, the burden of road traffic injury and death was found to be concerningly high in African countries (Davies et al. 2016), however, the registry-based data sets available from SSA and other low-income countries do not accurately reflect the true incidence and proportion of RTIs due to systematic under-reporting, which is estimated to be as high as 50% in some LMIC.(Ameratunga et al. 2006)(Jacobs et al. 2000)(Labinjo et al. 2009)(Murray et al. 1996)(Peden et al. 2004)(Salifu et al. 2012)(Samuel et al. 2012).
The aim of this study is to evaluate, through a systematic review and summary, the proportion of hospital based data road traffic fatalities and injuries in SSA. In so doing, we hope to describe the current literature and publication trends on the proportion of RTI and fatalities in SSA.
METHODS
Protocol
This systematic review is reported in accordance with the Meta-analysis of Observational Studies in Epidemiology (MOOSE) and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and is registered in the Prospero (International Prospective Register of Systematic Reviews) database (CRD42014014091).(Stroup, 2000)(Liberati, 2009)
Eligibility Criteria
The following inclusion criteria were utilized: (i) studies conducted in LMIC SSA countries; (ii) articles that measured the incidence and/or proportion of RTIs; (iii) hospital-based studies. Study designs considered included primary observational research or secondary data analysis; these observational hospital-based studies must describe the burden of RTIs and fatalities on the healthcare system. The following were used as exclusion criteria: (i) articles in languages other than English, Spanish, Portuguese, and French; (ii) literature reviews; (iii) non hospital based studies. The rationale for inclusion and exclusion criteria were based on the goal of developing models to estimate a pooled proportion of RTIs and RTI fatalities in SSA countries presenting to the hospital, therefore seeking data on proportion or incidence among hospital-based observational studies. Potential sources of bias were coded considering average age of the sample, time of data collection (year of publication), country, and the reason for admission (RTI, trauma, other types of injury).
Information Sources
We searched the following electronic databases: MEDLINE, Embase, Africa-Wide information, Global Health, and Web of Science. In addition, we manually searched the references of the included articles, and we performed citation analysis of the included studies using Google Scholar. Database searches were performed by qualified investigators with significant experience in systematic review methodology (JV).
Search
The search strategy used for PubMed is shown in Table A2. We did not use limits for languages and included all studies from 1990 until the present. Searches were conducted on the official website for each electronic database and the results were gathered using MyEndnote Web.
Study Selection
Titles and abstracts of the retrieved articles were independently evaluated by two reviewers (EK, DS). Abstracts which did not provide enough information regarding the eligibility criteria were saved for full-text evaluation. Reviewers independently evaluated full-text articles to determine study eligibility. We attempted to evaluate all articles including contacting authors for manuscripts if the articles were not readily available. Only published manuscripts were included in this review; abstracts without accompanying manuscripts were not included. Only those studies independently agreed upon by both reviewers were included. Disagreements were solved by consensus, and if disagreement persisted, we sought a third reviewer’s opinion (CS). Articles published in other than English (Spanish, Portuguese, French) were evaluated by bilingual investigators. A list of citations (titles and abstracts) and selected studies are published as appendix to this paper and also on our research group’s website (https://sites.google.com/site/rtisubsaharanafrica/).
Assessment of Risk of Bias
Risk of bias was evaluated according to an association between the Guidelines for critically appraising studies of proportion or incidence of a health problem scoring system (Loney et al. 1998) and the checklist from the STROBE statement.(Moher et al. 2009) Study quality assessment included (i) design and sampling adequacy; (ii) sample size; (iii) measurement method; (iv) assessment bias; (v) response rate and missing data; (vi) statistical methods, estimates, and confidence intervals; (vii) sample description. Quality assessment was independently performed by two blinded reviewers (EK and DS) and disagreements were solved by consensus or by a third reviewer (CS). Quality of studies was categorized as “Low risk of bias” and “High risk of bias”. A study was categorized as “Low risk of bias” when it showed less than two indicators of the quality assessment present but with ‘unclear’ specification, which were not directly related risk in providing raw data or calculating proportions. Any studies with more than three items with ‘unclear’ classifications and/or one or more low quality indicators were classified as “High risk of bias”.
Data Extraction
Two reviewers (EK and DS) independently conducted article data extraction. Disagreements or discrepancies in the data extraction process were reviewed again by both reviewers, and if they persisted, these disagreements were resolved by a third reviewer (CS). General characteristics of the studies were collected, such as year of publication, country, aim of the study, study design, setting and population description, data collection time range, age, and gender. We also collected total sample size, total number of RTIs, total number of trauma patients, and total number of RTI deaths from each study.
Data Analysis
We opted to conduct qualitative and descriptive approaches for proportion of both the number of RTIs among trauma patients and RTI deaths among RTI patients. Quantitative pooling data in meta-analysis models was not possible because heterogeneity estimates were too high (I2>85% and Cochrane Q<0.05). Heterogeneity was assessed Cochrane’s Q (considering p-values lower than 0.05 to indicators of heterogeneity) and I statistics (Higgins et al. 2002). High I2 values indicate high heterogeneity, with a proposed categorization of 25% (low), 45% (moderate) and 75% (high).. We anticipated high heterogeneity due to the diversified cultural characteristics of SSA countries and different health systems (i.e. prehospital care or emergency care) that would affect the proportion of mortality. Meta-regression was applied to evaluate influence of patient’s age, time of publication, country and reason for admission on our proportion of RTI and fatality estimation. Patient’s age, time of publication and country showed impact, so subgroup analysis were conducted and discussed separately. Several models were tested considering possible confounders such as country of study, study population (ie pediatric, adult), study design, and time period of the study. However, heterogeneity was still high in subgroup analysis or meta-regression models, which is expected in observational systematic reviews. To summarize the main proportion, we report forest plots with proportion of RTI deaths in RTI patients and proportion of RTIs in trauma patients in SSA countries by type of population. Median of proportions was calculated to separate summary reports by country and year of publication. All analysis and figures were conducted with R Language Software for Statistical Computing.(R Core Team, 2013).
RESULTS
Study Selection
As shown in Figure 1, a total of 2697 citations from 5 databases (PubMed, EMBASE, Africa-Wide Information, Global Health and Web of Science) were screened for eligibility. Reference and citation analysis introduced 100 articles and finally a total of 83 studies were included for the final analysis. A total of 69 studies reported the number of RTIs among trauma patients, with sample size ranging from 94 to 88,822. Another 43 studies reported the number of RTI deaths in RTI patients with sample size ranging from 66 to 23,454 (Table A1).
Figure 1:
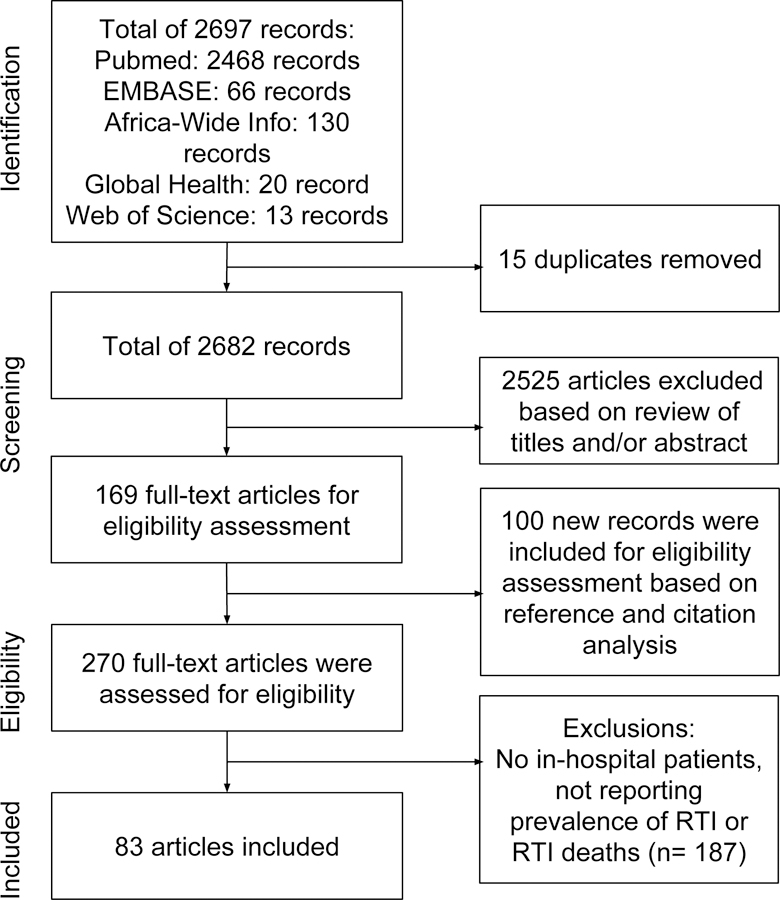
Study flow diagram
Studies Characteristics
Study characteristics for the 83 articles are included in Table A1. Our sample consists of studies among Emergency Department patients–based data in SSA countries. Nigeria had the largest number of studies (29), followed by South Africa with 12, Kenya with 11, and Uganda with 19. Ethiopia, Ghana, and Tanzania had 6, 7, and 5, respectively. Other countries represented were Malawi (3 studies), Rwanda (2), Cameroon (2), Mozambique (1), Namibia (1), and Senegal (1).
Considering study design, 45% were prospective and 53% retrospective, with only one study combining both prospective and retrospective methods. Trauma patients were the population type most frequent (38%) while RTI patients and overall injury patients had the same proportion (32%). Mostly, the studies did not differentiate age groups, discussing results of all ages of patients (53%), but 25% were pediatric-based data and 4% adults only; the rest were non-specified. Specific associations between proportion of RTI and RTI deaths and study characteristics will be presented. All countries with proportions and study numbers are represented in Figure 2. An increase in the number of studies is observed throughout the years, with only 2 studies before 1990 and a peak of 36 studies in the interval 2011–2015 (Figure 2).
Figure 2:
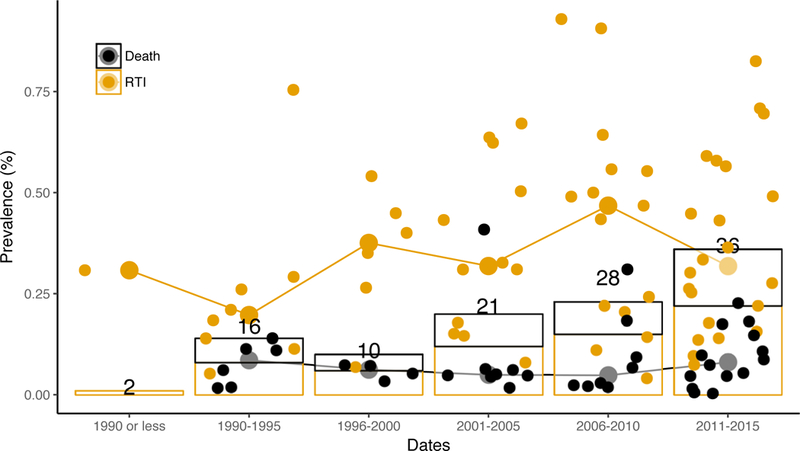
Time Series displaying manuscript per time period and proportion of RTI or death
Quality of Studies
Since we wanted to describe proportions, we chose data quality instruments focused on the adequacy and representativeness of samples within the studies. Our quality of studies evaluation indicated that 3 studies had indication of bias for proportion calculation (Adeolu et al. 2013)(Butchart et al. 1991)(Souza, 1968). Specifically, the main risk of bias common among the studies was the lack of appropriate sample description, selection or size (Table A1).
Most studies reported low risk of bias in relation to the proportion measures, although overall confidence intervals for proportions were not reported. Based on these results and the heterogeneity of study characteristics, we chose to report our results descriptively. Given our goal of qualitatively and descriptively summarizing the literature, we chose not to exclude studies based on quality issues. Quality classifications by study are displayed in Table A1.
Synthesis of Results
The proportion of RTI victims and fatal RTI were analyzed and descriptively summarized in the appendix (Figure A1 and A2). Our review included 310,660 trauma patients and 99,751 RTI cases across 13 SSA countries. Overall the median proportion of RTI among trauma patients was 32%, ranging from 4% to 91%. Studies reported a median of 22% with variation from 8% to 47% in pediatric RTI while adult-only population studies showed higher indicators with a median of 35% and values ranging from 26% to 64%. Studies with no age restrictions showed ranges from 5% to 91%, with median RTI proportion of 32%.
The median proportion of patients who died among all RTI patients for the included articles was 5%, ranging from 0.3% to 41%. For pediatric patients, RTI deaths varied from 0.3% to 18% with median of 3%, while all-age studies had 6% of median and a variation from 0.3% to 41%, and adults died in a proportion from 2% to 11% with median of 4% (Figure A2).
proportion by type of road user.
Studies reporting proportion of RTI within injury patients showed a median of 31.4% with variation from 11.1% to 92.9% for vehicle road users, while pedestrian-only population studies showed higher indicators with median of 43.2% and values ranging from 9.7% to 69.6%. Studies aggregating all RTI types regardless of type of vehicle had a median proportion of 31% ranging from 5.3% to 90.6% (Figure 3). Vulnerable road users (studies that did not differentiate motorcycle drivers, bicyclists and pedestrians) RTI proportion was 42.4% with ranges from 40% to 44.9%.
Figure 3:
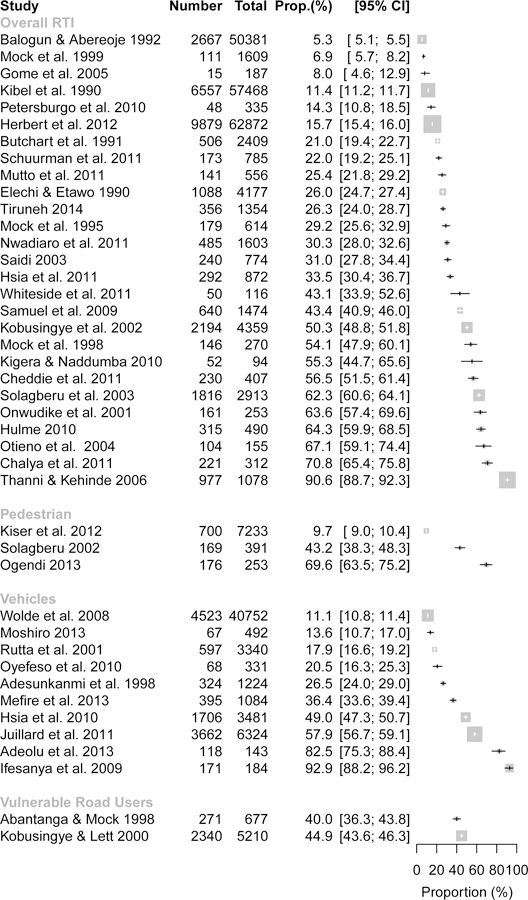
Summary of the proportion of Road Traffic Injuries among All Injuries by type of vehicle
The median proportion of patients who died among all RTI patients who reported to be motorcycle drivers was 9.8%, ranging from 8.8% to 10.8%. For vehicle drivers, RTI deaths varied from 2.4% to 31% with median of 7.4% while vulnerable road users had a proportion from 7.4% to 22.7% with median of 15%. Studies with all RTI regardless of type of vehicle (Overall RTI) had 5.6% of median and a variation from 0.3% to 40.8%. Finally, pedestrian RTI death proportion was 1.7% with ranges from 0.5% to 9.8% (Figure 4).
Figure 4:
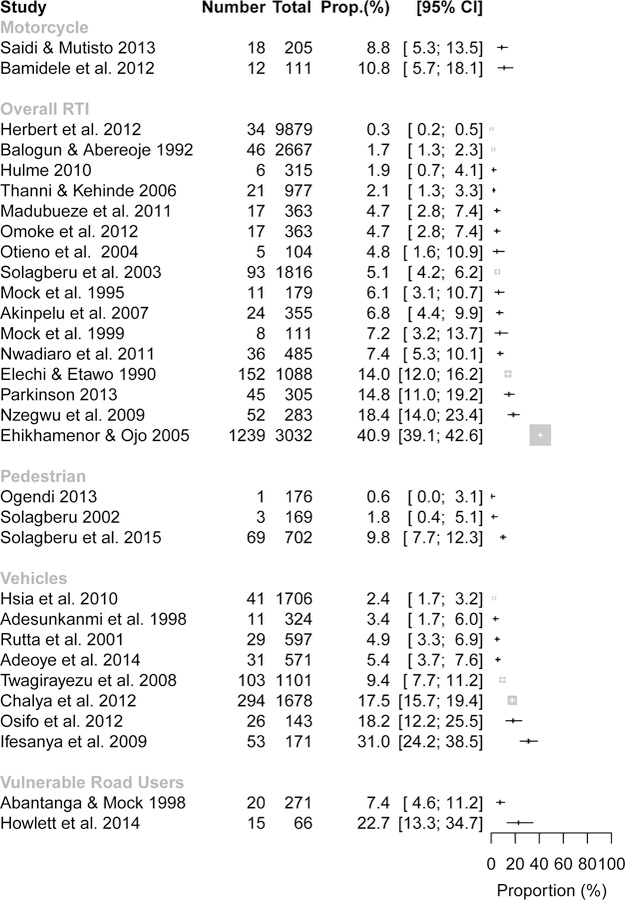
Summary of the proportion of Road Traffic Injury Fatalities among All Road Traffic Injury Victims by type of vehicle
proportion by SSA countries
Nigeria and Rwanda had the highest median (51%) but Rwanda had only one study while Nigeria had a range of proportion of RTI (5% to 91%). Highest median results of RTI among trauma patients was in Cameroon (47%, 36% to 58%), Ghana (40%, 32% to 54%), and Uganda (47%, 25% to 64%). Smaller proportion was observed in South Africa (15%, 7% to 56%), Tanzania (16%, 13% to 71%), Ethiopia (19%, 11% to 49%), and Malawi (22%, 10% to 43%). Kenya had 30% of median RTI (4% to 69%) while Mozambique (14%) and Namibia (20%) had only one study reporting RTI proportion among trauma patients (Figure 5).
Figure 5:
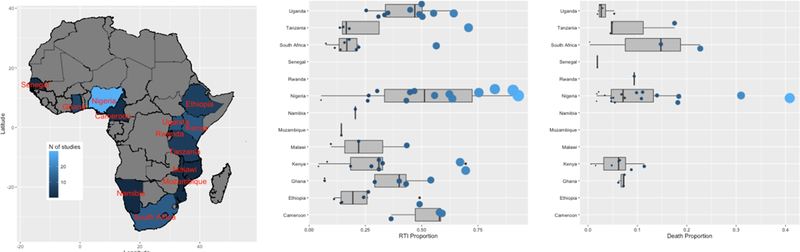
Map of Locations of Data Collection among articles as well as the proportion of deaths and proportion of RTI among all injury patients.
For deaths among RTI patients, not all countries reporting RTI proportion reported deaths as well. Deaths were most frequent in Rwanda (9%) although Rwanda only had one study. South Africa (7%, 0.3% to 15%), Ghana (7%, 6% to 7%), and Kenya (6%, 0.5% to 8%) had the next largest proportion. Nigeria showed a median proportion of RTI deaths of 5% (1% to 40%) and also the largest maximum proportion reported. The smallest values were found for Tanzania (4%, 4% to 17%) and Uganda (3%, 2% to 5%), Senegal (2%) and Ethiopia each had one paper (0.3%).
proportion by year of publication
Figure 2 shows the number of publications has been increasing (2 to 36), especially between 2011–2015. Median values show an increased trend in RTI among trauma patients and a small variation in median proportion of deaths. In the last period of time (2011–2015), the medium value of RTIs among injury patients decreased; however, this value must be interpreted carefully because for all time periods there is a wide variability in the proportion data, represented by the points scattered in the graph, for both outcome measures (Figure 2).
DISCUSSION
On March 2, 2010, with resolution 64/2551, the United Nations General Assembly declared 2011–2020 The Decade of Action for Road Safety. The goal of this resolution is to help develop the framework and support for coordinated local, national and global efforts to abate the pandemic of RTIs and fatalities. To our knowledge, we conducted the first systematic review and meta-analysis of RTI proportion over 20 years in sub-Saharan Africa; a region with rapidly increasing RTIs along with motorization and urbanization. We found a median proportion of RTI among trauma patients was 32% (4% to 91%) and the median proportion of patients who died among all RTI patients was 5% (0.3% to 41%).While according to our Global Burden of Disease data, it is well established that the burden of RTI and fatalities are increasing, our data found only a slightly increasing proportion of RTI among injury patients and a steady proportion of fatalities. Over the last two decades, the literature describing the RTI epidemiology in SSA grew. We feel the difference between our findings and the Global Burden of Disease highlights the limitations in RTI research in SSA: first, the limitations and challenges of injury research in a LMIC setting; and second, the limited road safety regulation environment leading to high numbers of immediate fatalities.
Limitations of data sources pose a significant challenge to injury research in an LMIC setting. Given the multi-sectoral nature of RTI, there are few complete and quality data sources for injury. Legal death registries are expensive, at times poor quality and do not describe the morbidity due to injuries which is a more burdensome challenge while hospital-based registries have selection biases limited by access to care and immediately fatal injuries.(Chandran A et al. 2010) Upwards of 50% of trauma deaths in LMIC occur in the prehospital setting.(Mock et al. 1998) In a LMIC, prehospital services are disastrously underdeveloped, leading directly to more immediate RTI deaths that would be otherwise occurring if prehospital services were available. Here, prehospital services are provided by bystanders and transport is usually by private vehicle with considerable transport delays.(Nilsen et al. 2014) In a 1998, study in Kumasi, Ghana, showed only 9% of trauma patients requiring admission were transported by ambulance, and most of those were intrahospital transfers, while the major source of transport to the hospital was via commercial vehicles.(Mock et al. 1998)
As such, a considerable proportion of RTI patients are never even seen in a hospital and those that are are likely have substantial delays in care worsening their morbidity and mortality.(Mock et al. 1998) In our data, made up of 32 studies and a total of 46,897 patients, the median proportion of patients who died among all RTI patients for the included articles was 5%, ranging from 0.3% to 41%. This significantly low mortality rate is likely due to a large proportion of mortalities occurring in prehospitally.
While the UN declared the current decade to be the one of action for road safety, specifically citing research in each of the pillars of the Global Plan, between 2011–2015 the number of published hospital-based RTI manuscripts in SSA have not exponentially escalated as hoped. With the UN declaration, a marked increase in road traffic research could be expected, but this rise in manuscripts appears comparable to the pre-declaration increase. As such, RTIs in SSA remain a strikingly understudied field; in 2013, the Lancet Global Health issued a call for increased data collection from the health sector.(Mullan et al. 2013) Insufficient road traffic injury research is likely driven by several factors. First, the combination of insufficient healthcare funding and limited resources and organizational mechanisms makes it difficult to conduct small-, medium-, or large-scale RTI epidemiology. On average, SSA governments pay for an estimated one-third of total health expenditures and how these funds (along with private funding) are allocated is extremely variable. Second, there is very limited funding for electronic health records (EHR) and data systems is very limited. While there has been an increase in the use of EHRs in SSA, their use is still exceedingly low and cost-prohibitive. Furthermore, the use of EHRs in SSA is fraught with challenges, including dependence on international funding and partnerships, high set-up and maintenance costs, and the need for parallel entry of data to paper and computer.(Akanbi et al. 2012) Lastly, despite the aforementioned calls for further research on the burden caused by road traffic crashes and the Decade of Action for Road Safety, the knowledge and recognition of the global burden of RTI on international platforms remains limited.
The strengths of this study include the multi-decade, multi-language inclusive nature of this systematic review. We included all languages likely to publish data about the countries of interest based on local languages (English, Portuguese, French, and Spanish). The main limitations in this study include those cited during the discussion about the quality and variability of the data as well as the publication biases inherent in this research. Publication bias on data from LMIC is impacted by financial difficulty obtaining funds to both conduct and then to publish data as well as limited research infrastructure and capacity to conduct and produce publishable research. Similarly, these results should not be generalized to discuss overall incidence or proportion of RTI in SSA as there is a large access to care bias in this unique setting for this unique population. We also acknowledge a limitation regarding information on specific of each hospital where the data was gathered. We understand that hospitals in LMIC manage data differently and have different levels of infrastructure. However, given our goal to be the most inclusive to describe the situation in SSA we choose to include all these different study methods- which while a limitation for any metanalytic results helps us with our aim of understand current literature on the burden of RTIs at hospitals
Through a systematic review and summary of road traffic injury and road traffic fatalities from hospital-based studies in SSA countries, we found a median proportion of RTI of 32% among hospitalized injury patients and a median of 5% mortality among hospitalized RTI patients. Over the last 20 years, while the number of manuscripts has increased, the taxonomy and methods used varied so broadly that there are significant challenges in performing comparisons and meta-analyses. Further funding focused on research infrastructure should be allocated in order to improve RTI-related research.
Supplementary Material
Acknowledgments
FUNDING
Dr. Staton and Dr. Krebs would like to acknowledge salary support funding from the Fogarty International Center (Staton, K01 TW010000–01A1), (VECD, Fogarty Fellowship).
Contributor Information
João Ricardo N. Vissoci, Division of Emergency Medicine, Department of Surgery, Division of Neurosurgery and Neurology, Department of Neurosurgery, Duke University, Durham USA, jnv4@duke.edu.
Daniel J. Shogilev, Duke School of Medicine, Duke University, Durham USA, daniel.shogilev@dm.duke.edu.
Elizabeth Krebs, Duke Global Health Institute, Duke University, Durham USA, krebse@gmail.com.
Luciano de Andrade, State University of Maringá, Maringá, Brazil, luc.and1973@gmail.com.
Igor Fiorese Vieira, UniCesumar, Maringa, Brazil, medigorvieira@gmail.com.
Nicole Toomey, Duke Global Health Institute, Duke University, Durham, USA, nicole.toomey@duke.edu.
Adelia Portero Batilana, IC-FUC, Porto Alegre, Brazil, adeliabatilana@gmail.com.
Michael Haglund, Duke School of Medicine, Duke Global Health Institute, Duke University, Durham USA, michael.haglund@dm.duke.edu.
Catherine A. Staton, Section of Emergency Medicine Global Health., Surgery and Global Health..
REFERENCES
- 1.Abantanga F, Mock C. Childhood injuries in an urban area of Ghana A hospital-based study of 677 cases. Pediatric Surgery International 1998;13(7):515–518. [DOI] [PubMed] [Google Scholar]
- 2.Adeloye D, Thompson J, Akanbi M, Azuh D, Samuel V, Omoregbe N, Ayo C. The burden of road traffic crashes, injuries and deaths in Africa: a systematic review and meta-analysis. Bull World Health Organ 2016. July;1(7):510–521A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adeolu A, Abiona T, Komolafe E, Adeolu J, Adegbehingbe O. Epidemiology of Neurotrauma in Ife-Ijesha Zone of Nigeria. World Neurosurgery 2013;80(3–4):251–254. [DOI] [PubMed] [Google Scholar]
- 4.Adeoye P, Kadri D, Bello J, Pascal C, Abdur-Rahman L, Adekanye A, Solagberu B. Host, vehicular and environmental factors responsible for road traffic crashes in a nigerian city: identifiable issues for road traffic injury control. Pan African Medical Journal 2014;19. [DOI] [PMC free article] [PubMed]
- 5.Adesunkanmi A, Oginni L, Oyelami A, Badru O. Epidemiology of Childhood Injury. The Journal of Trauma: Injury, Infection, and Critical Care 1998;44(3):506–511. [DOI] [PubMed] [Google Scholar]
- 6.Akanbi M, Ocheke A, Agaba P, Daniyam C, Agaba E, Okeke E, Ukoli C. Use of Electronic Health Records in sub-Saharan Africa: Progress and challenges. J Med Trop 2012;14(1):1–6. [PMC free article] [PubMed] [Google Scholar]
- 7.Akinpelu O, Oladele A, Amusa Y, Ogundipe O, Adeolu A, Komolafe E. Review of Road Traffic Accident Admissions in a Nigerian Tertiary Hospital. East and Central African Journal of Surgery 2007;12(1). [Google Scholar]
- 8.Ameratunga S, Hijar M, Norton R. Road-traffic injuries: confronting disparities to address a global-health problem. Lancet 2006;367(9521):1533–1540. [DOI] [PubMed] [Google Scholar]
- 9.Andrews C, Kobusingye O, Lett R. Road traffic accident injuries in Kampala. East Afr Med J 1999;76(4):189–94. [PubMed] [Google Scholar]
- 10.Ayana B, Mekonen B, Lollino N. The ‘hit by a stick’ disease: an epidemiologic study of the causes of trauma in a non-profit hospital in rural Ethiopia. Tropical Doctor 2011;42(1):1–4. [DOI] [PubMed] [Google Scholar]
- 11.Balogun J, Abereoje O. Pattern of road traffic accident cases in a Nigerian University teaching hospital between 1987 and 1990. Journal of Tropical Medicine and Hygiene 1992;95(1):23–29. [PubMed] [Google Scholar]
- 12.Bamidele J, Adebimpe W, Adeoye O. Morbidity and Mortality Pattern Among Commercial Motorcyclists In Osogbo Metropolis In South Western Nigeria. Journal of Contemporary Medicine 2012;2(1):13–16. [Google Scholar]
- 13.Brysiewicz P Pedestrian road traffic collisions in South Africa. Accident and Emergency Nursing 2001;9(3):194–197. [DOI] [PubMed] [Google Scholar]
- 14.Butchart A, Brown D. Non-fatal injuries due to interpersonal violence in Johannesburg — Soweto: Incidence, determinants and consequences. Forensic Science International 1991;52(1):35–51. [DOI] [PubMed] [Google Scholar]
- 15.Chalya P, Mabula J, Dass R, Mbelenge N, Ngayomela I, Chandika A, Gilyoma J. Injury characteristics and Outcome of Road traffic crash victims at Bugando Medical Centre in Northwestern Tanzania. J Trauma Manage Outcomes 2012;6(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chalya P, Gilyoma J, Dass R, Mchembe M, Matasha M, Mabula J, Mbelenge N, Mahalu W. Trauma admissions to the Intensive care unit at a reference hospital in Northwestern Tanzania. Scand J Trauma Resusc Emerg Med 2011;19(1):61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chandran A, Hyder A, Peek-Asa C. The Global Burden of Unintentional Injuries and an Agenda for Progress. Epidemiologic Reviews 2010;32(1):110–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cheddie S, Muckart D, Hardcastle T, Den Hollander D, Cassimjee H, Moodley S. Direct admission versus inter-hospital transfer to a level I trauma unit improves survival: An audit of the new Inkosi Albert Luthuli Central Hospital trauma unit. S Afr Med J 2011;101(3):176. [DOI] [PubMed] [Google Scholar]
- 19.Chichom Mefire A, Etoundi Mballa G, Azabji Kenfack M, Juillard C, Stevens K. Hospital-based injury data from level III institution in Cameroon: Retrospective analysis of the present registration system. Injury 2013;44(1):139–143. [DOI] [PubMed] [Google Scholar]
- 20.Chokotho L, Matzopoulos R, Myers J. Assessing quality of existing data sources on road traffic injuries (RTIs) and their utility in informing injury prevention in the Western Cape Province, South Africa. Traffic injury prevention 2013;14(3):267–273. [DOI] [PubMed] [Google Scholar]
- 21.Demyttenaere SV, Nansamba C, Nganwa A, Mutto M, Lett R, Razek T. Injury in Kampala, Uganda: 6 years later. J can chir 2009;52(5). [PMC free article] [PubMed] [Google Scholar]
- 22.Ehikhamenor E, Ojo M. Comparative Analysis of Traumatic Deaths in Nigeria. Prehosp Disast Med 2002;20(3):197–201. [DOI] [PubMed] [Google Scholar]
- 23.Ekenze S, Anyanwu K, Chukwumam D. Childhood trauma in Owerri (south eastern) Nigeria. Niger J Med 2009;18(1):79–83. [PubMed] [Google Scholar]
- 24.Elechi E Pilot study of injured patients seen in the University of Port Harcourt Teaching Hospital, Nigeria. Injury 1990;21(4):234–238. [DOI] [PubMed] [Google Scholar]
- 25.GBD 2013 Risk Factors Collaborators. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380(9859):2095–2128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gome D, Mutiso V, Kimende K. Paediatric Trauma at Kenyatta National Hospital, Nairobi Kenya. East and Central African Journal of Surgery 2005;10(2). [Google Scholar]
- 27.Govender I, Matzopoulos R, Makanga P, Corrigall J. Piloting a trauma surveillance tool for primary healthcare emergency centers. S Afr Med J 2002;102(5):303–306. [DOI] [PubMed] [Google Scholar]
- 28.Herbert H, Van A, Bachani A, Mtambeka P, Stevens K, Millar A, Hyder A. Patterns of pediatric injury in South Africa. Journal of Trauma and Acute Care Surgery 2012;73(1):168–174. [DOI] [PubMed] [Google Scholar]
- 29.Howlett J, Aldous C, Clarke D. Injuries sustained by passengers travelling in the cargo area of light delivery vehicles. S Afr J Surg 2014;52(2):49. [DOI] [PubMed] [Google Scholar]
- 30.Hsia R, Ozgediz D, Jayaraman S, Kyamanywa P, Mutto M, Kobusingye O. Epidemiology of child injuries in Uganda: challenges for health policy. Journal of Public Health in Africa 2011;2(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hsia R, Ozgediz D, Mutto M, Jayaraman S, Kyamanywa P, Kobusingye O. Epidemiology of injuries presenting to the national hospital in Kampala, Uganda: implications for research and policy. Int J Emerg Med 2010;3(3):165–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hulme P Mechanisms of trauma at a rural hospital in Uganda. Pan African Medical Journal 2011;7(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ifesanya A, Afuwape D, Okoje V, Agunloye A, Odole O, Okolo C, Alonge T. Unintentional Injury Outcomes Secondary to Pedestrian Traffic Crashes: A Descriptive Analysis from a Major Medical Center. Prehospital and Disaster Medicine 2009;24(5):443–446. [DOI] [PubMed] [Google Scholar]
- 34.Jacobs G, Thomas A. Estimating Global Road Fatalities Crowthorne: Transport Research Laboratory; 2000. [Google Scholar]
- 35.Juillard C, Mballa G, Nyemb N, Stevens K, Hyder A. Patterns of injury and violence in Yaound Cameroon: an analysis of hospital data. Injury Prevention 2010;16(Supplement1):A166–A166. [Google Scholar]
- 36.Juillard C, Stevens K, Monono M, Mballa G, Ngamby M, McGreevy J, Cryer G, Hyder A. Analysis of Prospective Trauma Registry Data in Francophone Africa: A Pilot Study from Cameroon. World J Surg 2014;38(10):2534–2542. [DOI] [PubMed] [Google Scholar]
- 37.Kebede T, Mekonene T, Bartolemes K, Taye M, Munie T, Meleses M. Injury surveillance in six hospitals of Addis Ababa, Ethiopia. Ethiop Med J 2008;46(4):383–90. [PubMed] [Google Scholar]
- 38.Kibel S, Bass D, Cywes S. Five years’ experience of injured children. S Air Med J 1990;78(1)387–391. [PubMed] [Google Scholar]
- 39.Kigera J. Is the pedestrian an endangered group of road users? A descriptive account of pedestrian injuries. E Af Orth Jnl 2011;4(2). [Google Scholar]
- 40.Kiser M, Samuel J, Mclean S, Muyco A, Cairns B, Charles A. Epidemiology of pediatric injury in Malawi: Burden of disease and implications for prevention. International Journal of Surgery 2012;10(10):611–617. [DOI] [PubMed] [Google Scholar]
- 41.Kobusingye O Citywide trauma experience in Kampala, Uganda: a call for intervention. Injury Prevention 2002;8(2):133–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kobusingye O, Lett R. Hospital-Based Trauma Registries in Uganda. The Journal of Trauma: Injury, Infection, and Critical Care 2000;48(3):498–502. [DOI] [PubMed] [Google Scholar]
- 43.Labinjo M, Juillard C, Kobusingye O, Hyder A. The burden of road traffic injuries in Nigeria: results of a population-based survey. Inj. Prev 2009;15(3):157–162. [DOI] [PubMed] [Google Scholar]
- 44.Liberati A The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. Annals of Internal Medicine 2009;151(4):W. [DOI] [PubMed] [Google Scholar]
- 45.Loney P, Chambers L, Bennett K, Roberts J, Stratford P. Critical appraisal of the health research literature: proportion or incidence of a health problem. Chronic Dis Can 1998;19(4):170–176. [PubMed] [Google Scholar]
- 46.Madubueze C, Chukwu C, Omoke N, Oyakhilome O, Ozo C. Road traffic injuries as seen in a Nigerian teaching hospital. International Orthopaedics (SICOT) 2010;35(5):743–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Makubi A, Mugusi F, Magesa P, Roberts D. Risk factors for anaemia among HIV infected children attending care and treatment clinic at Muhimbili National Hospital in Dar es Salaam, Tanzania. Tanzania Journal of Health Research 2012;14(1). [PubMed] [Google Scholar]
- 48.Marquez P, Farrington J. The challenge of non-communicable diseases and road traffic injuries in Sub-Saharan Africa : an overview Washington DC: 2013/07/12 2013. [Google Scholar]
- 49.Masiira-Mukasa N, Nombito B. Surgical admissions to the Rift Valley provincial general hospital, Kenya. E Af Med Jrnl 2002;79(7). [DOI] [PubMed] [Google Scholar]
- 50.Mengistu Z, Azaj A. Trauma severities scores and their prediction of outcome among trauma patients in two hospitals of Addis Ababa, Ethiopia. Ethiop Med J 2012;50(3):231–7. [PubMed] [Google Scholar]
- 51.Mock CN, Abantanga F, Cummings P, Koepsell T. Incidence and outcome of injry in Ghana: a community based survey. Bulletin of the World Health Organization 1999. [PMC free article] [PubMed] [Google Scholar]
- 52.Mock C, Adzotor E, Denno D, Conklin E, Rivara F. Admissions for injury at a rural hospital in Ghana: implications for prevention in the developing world. Am J Public Health 1995;85(7):927–931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mock C, Jurkovich G, nii-Amon-Kotei D, Arreola-Risa C, Maier R. Trauma Mortality Patterns in Three Nations at Different Economic Levels. The Journal of Trauma: Injury, Infection, and Critical Care 1998;44(5):804–814. [DOI] [PubMed] [Google Scholar]
- 54.Moher D Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Annals of Internal Medicine 2009;151(4):264. [DOI] [PubMed] [Google Scholar]
- 55.Mullan Z, Horton R. The Lancet Global Health: a call for papers. The Lancet 2013;381(9871):979. [DOI] [PubMed] [Google Scholar]
- 56.Murray C, Lopez A. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet 1997;349(9061):1269–1276. [DOI] [PubMed] [Google Scholar]
- 57.Mutto M, Lawoko S, Nansamba C, Ovuga E, Svanstrom L. Unintentional Childhood Injury Patterns, Odds, and Outcomes in Kampala City: an analysis of surveillance data from the National Pediatric Emergency Unit. Journal of Injury and Violence Research 2011;3(1):13–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ndiaye A, Camara S, Ndoye A, Dansokho A, Sow C, Ndiaye P, Bassenne N. Mortality caused by traffic accidents at the Traumatology and Orthopedics Center of Grand-Yoff. A 2-year study. Apropos of 156 cases. Med Trop (Mars) 1993;53(4):487–91. [PubMed] [Google Scholar]
- 59.Nilsen C, Østbye T, Daltveit A, Mmbaga B, Sandøy I. Trends in and socio-demographic factors associated with caesarean section at a Tanzanian referral hospital, 2000 to 2013. International Journal for Equity in Health 2014;13(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nwadiaro H, Akpayak I, Ekwe K, Shitta H. Motorcycle injuries in north-central Nigeria. Nigerian Journal of Clinical Practice 2011;14(2):186. [DOI] [PubMed] [Google Scholar]
- 61.Nzegwu M, Banjo A, Akhiwu W, Aligbe J, Nzegwu C. Morbidity and mortality among road users in Benin-city, Nigeria. Ann Afr Med 2008;7(3):102. [DOI] [PubMed] [Google Scholar]
- 62.Oboirien M Pattern of paediatric trauma in Sokoto, North West Nigeria. African Journal of Paediatric Surgery 2013;10(2):172. [DOI] [PubMed] [Google Scholar]
- 63.Odero W, Kibosia J. Incidence and characteristics of injuries in Eldoret, Kenya. East Afr Med J 1995;72(11):706–10. [PubMed] [Google Scholar]
- 64.Odero W Road traffic accidents in Kenya: an epidemiological appraisal. East Afr Med J 1995;72(5):299–305. [PubMed] [Google Scholar]
- 65.Odero W, Polsky S, Urbane D, Carel R, Tierney W. Characterists of injuries presenting to a rural health centre in western Kenya. E Af Med Jrnl 2008;84(8). [DOI] [PubMed] [Google Scholar]
- 66.Ogendi J, Odero W, Mitullah W, Khayesi M. Pattern of Pedestrian Injuries in the City of Nairobi: Implications for Urban Safety Planning. Journal of Urban Health 2013;90(5):849–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ogendi J, Ayisi J. Causes of injuries resulting in a visit to the emergency department of a Provincial General Hospital, Nyanza, western Kenya. Afr Health Sci 2011;11(2):255–261. [PMC free article] [PubMed] [Google Scholar]
- 68.Oluwadiya K, Kolawole I, Adegbehingbe O, Olasinde A, Agodirin O, Uwaezuoke S. Motorcycle crash characteristics in Nigeria: Implication for control. Accident Analysis & Prevention 2009;41(2):294–298. [DOI] [PubMed] [Google Scholar]
- 69.Omoke N, Chukwu C, Madubueze C, Oyakhiolme O. Outcome of road traffic injuries received in the emergency room of a teaching hospital, Southeast Nigeria. Tropical Doctor 2012;42(1):18–22. [DOI] [PubMed] [Google Scholar]
- 70.Onah I, Okwesili I. Presentation of trauma at the National Orthopaedic Hospital Enugu: a pilot study. Tropical Doctor 2009;39(2):80–83. [DOI] [PubMed] [Google Scholar]
- 71.Onwudike M, Olaloye O, Oni O. Teaching Hospital Perspective of the Quality of Trauma Care in Lagos, Nigeria. World Journal of Surgery 2001;25(1):112–115. [DOI] [PubMed] [Google Scholar]
- 72.Osifo O, Osagie T, Iribhogbe P. Pediatric Road Traffic Accident Deaths Presenting to a Nigerian Referral Center. Prehospital and Disaster Medicine 2012;27(02):136–141. [DOI] [PubMed] [Google Scholar]
- 73.Osman M, Kebede Y, Anberbir S. Magnitude and pattern of injuries in north Gondar administrative zone, northwest Ethiopia. Ethiop Med J 2003;41(3):213–20. [PubMed] [Google Scholar]
- 74.Otieno T, Woodfield J, Bird P, Hill A. Trauma in rural Kenya. Injury 2004;35(12):1228–1233. [DOI] [PubMed] [Google Scholar]
- 75.Oyefeso O, Madiba S, Hoque M. proportion and profile of injuries in Khorixas District Hospital, Namibia. South Afr J Epidemiol Infect 2011;26(2):83–87. [Google Scholar]
- 76.Parkinson F, Kent S, Aldous C, Oosthuizen G, Clarke D. Patterns of injury seen in road crash victims in a South African trauma centre. S Afr J Surg 2013;51(4):131. [DOI] [PubMed] [Google Scholar]
- 77.Peden M, Scurfiled R, Sleet D, Mohan D, Hyder A, Jarawan E. World report on road traffic injury prevention Geneva: World Health Organization; 2004. [Google Scholar]
- 78.Petersburgo D, Keyes C, Wright D, Click L, Macleod J, Sasser S. The epidemiology of childhood injury in Maputo, Mozambique. Int J Emerg Med 2010;3(3):157–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Rutta E, Mutasingwa D, Ngallaba S, Berege Z. Epidemiology of injury patients at Bugando Medical centre, Tanzania. E Af Med Jrnl 2001;78(3). [DOI] [PubMed] [Google Scholar]
- 80.Saidi H Initial injury care in Nairobi, Kenya: A call for trauma care regionalisation. E Af Med Jrnl 2004;80(9). [DOI] [PubMed] [Google Scholar]
- 81.Saidi H, Macharia W, Atinga J. Crash and road-user characteristics in non-fatal motor vehicle collisions in Nairobi, Kenya Afr. Safety Promotion Journal 2006;4:50–58. [Google Scholar]
- 82.Saidi H, Mutisto B. Motorcycle injuries at a tertiary referral hospital in Kenya: injury patterns and outcome. Eur J Trauma Emerg Surg 2013;39(5):481–485. [DOI] [PubMed] [Google Scholar]
- 83.Salifu M, Ackaah W. Under-reporting of road traffic crash data in Ghana. International journal of injury control and safety promotion 2012;19(4):331–339. [DOI] [PubMed] [Google Scholar]
- 84.Samuel J, Sankhulani E, Qureshi J, Baloyi P, Thupi C, Lee C, Miller W, Cairns B, Charles A. Under-reporting of road traffic mortality in developing countries: application of a capture-recapture statistical model to refine mortality estimates. PloS one 2012;7(2):e31091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Samuel J, Akinkuotu A, Villaveces A, Charles A, Lee C, Hoffman I, Miller WC, Baloyi P, Hoffman M, Brown L, Muyco A. Epidemiology of Injuries at a Tertiary Care Center in Malawi. World J Surg 2009;33(9):1836–1841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Schuurman N, Cinnamon J, Matzopoulos R, Fawcett V, Nicol A, Hameed S. Collecting injury surveillance data in low- and middle-income countries: The Cape Town Trauma Registry pilot. Global Public Health 2011;6(8):874–889. [DOI] [PubMed] [Google Scholar]
- 87.Solagberu B Trauma deaths in children: a preliminary report. Nigerian Journal of Surgical Research 2002;4(3). [Google Scholar]
- 88.Solagberu B Motorcycle injuries in a developing country and the vulnerability of riders, passengers, and pedestrians. Injury Prevention 2006;12(4):266–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Solagberu B, Adekanye A, Ofoegbu C, Udoffa U. Epidemiology of trauma deaths. West African Journal of Medicine 2004;22(2). [DOI] [PubMed] [Google Scholar]
- 90.Solagberu B, Balogun R, Mustafa I, Ibrahim N, Oludara M, Ajani A, Idowu O, Osuoji R. Pedestrian Injuries in the Most Densely Populated City in Nigeria-An Epidemic Calling for Control. Traffic Injury Prevention 2014;16(2):184–189. [DOI] [PubMed] [Google Scholar]
- 91.Stroup D Meta-analysis of Observational Studies in Epidemiology:A Proposal for Reporting. JAMA 2000;283(15):2008. [DOI] [PubMed] [Google Scholar]
- 92.Souza L The pattern of trauma at Mulago hospital, Kampala. East Afr Med J 1968;45(7):523–31. [PubMed] [Google Scholar]
- 93.Thanni L, Kehinde O. Trauma at a Nigerian teaching hospital: pattern and documentation of presentation. African Health Sciences 2006;6(2):104–107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Tiruneh B, Dachew B, Bifftu B. Incidence of Road Traffic Injury and Associated Factors among Patients Visiting the Emergency Department of Tikur Anbessa Specialized Teaching Hospital, Addis Ababa, Ethiopia. Emergency Medicine International 2014:1–6. [DOI] [PMC free article] [PubMed]
- 95.Twagirayezu E, Teteli R, Bonane A, Rugwizangoga E. Road Traffic Injuries at Kigali University Central Teaching Hospital, Rwanda. East and Central African Journal of Surgery 2008;13(1) [Google Scholar]
- 96.Whiteside L, Oteng R, Carter P, Amuasi J, Abban E, Rominski S, Nypaver M, Cunningham R. Non-fatal injuries among pediatric patients seeking care in an urban Ghanaian emergency department. International Journal of Emergency Medicine 2012;5(36). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wolde A, Abdella K, Ahmed E, Tsegaye F, Babaniyi O, Kobusingye O. Pattern of Injuries in Addis Ababa, Ethiopia: A One-year Descriptive Study. East and Central African Journal of Surgery 2008.
- 98.Yu K, Bong C, Huang M, Chen C, Ko Y, Chang P, Chen T, Chiang H. The use of hospital medical records for child injury surveillance in northern Malawi. Tropical Doctor 2009;39(3):170–172. [DOI] [PubMed] [Google Scholar]
- 99.Zwi K, Zwi A, Smettanikov E, Soderlund N, Logan S. Patterns of injury in children and adolescents presenting to a South African township health centre. Injury Prevention 1995;1(1):26–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


