Abstract
Objective:
The aim of this study was to systematically review the literature on gendered implications of incarceration for HIV outcomes and engagement in care for women living with HIV (WLWH).
Design:
We systematically searched seven bibliographic databases, for peer-reviewed English-language studies, published between 2007 and 2017 reporting on incarceration, women (transgender inclusive) and HIV.
Methods:
Articles were included for evaluation if they reported outcomes for at least one of three measures of interest: viral load, antiretroviral therapy (ART) adherence or engagement in care among WLWH along incarceration trajectories.
Results:
Out of 1119 studies, 24 (2%) met the inclusion criteria. Of these 24 studies, the majority (n = 23) were conducted in the USA, 19 included samples of women and men and seven studies were transgender inclusive. Our review did not reveal clear sex differences in HIV outcomes during periods of incarceration; however, studies reporting postincarceration outcomes demonstrated significant sex disparities in all three outcomes of interest.
Following incarceration, women were less likely to be virally suppressed, less likely to achieve optimal ART adherence and less likely to be engaged in care.
Conclusion:
Despite growing numbers of incarcerated WLWH globally, there is a substantial gap in research examining the impact of incarceration on HIV outcomes for WLWH. Significant sex disparities in HIV outcomes and engagement in care exist along incarceration trajectories for WLWH, especially postincarceration. For improved health outcomes, research is needed to examine the experiences of WLWH throughout incarceration trajectories to develop interventions tailored to the specific needs of WLWH both during and following incarceration.
BACKGROUND
In the last decade, there have been significant advances in HIV treatment and care for people living with HIV (PLWH) [1,2]. Improved outcomes are frequently attributed to engagement in the HIV ‘cascade of care’, which includes timely HIV testing and diagnosis, linkage to care and support, retention in care, adherence and viral suppression [3,4]. This approach promotes improved health outcomes, such as lower mortality and morbidity, and reduced transmission of HIV [1,5,6]. However, not all PLWH have equally benefited from advances in HIV treatment and care; this is especially true for PLWH with a history of incarceration and criminal justice involvement [7–9]. Globally, PLWH are disproportionately represented among incarcerated populations [10,11], with the global HIV burden among incarcerated persons estimated between two and 10 times higher than the general adult population [12]. Racialized represent a rapidly increasing proportion of incarcerated people globally [13–15], and women living with HIV (WLWH) make up an ever-growing proportion of incarcerated women worldwide [16,17]. Within correctional facilities globally, women are more likely to be identified as living with HIV than men [18,19].
Although global research is limited, findings from the United States indicate that correctional facilities can provide an opportunity to connect with marginalized populations, subsequently creating an opportunity to engage PLWH in HIV treatment and care during incarceration [20]. However, overall optimal HIV treatment outcomes for incarcerated populations remain a challenge [21], and for many PLWH, arrest and detention often leads to interruptions and gaps in ART access and adherence [7–9,22].
WLWH experience intersecting structural vulnerabilities that create additional obstacles to receiving high-quality HIV care, including experiencing sex-based violence [23] and trauma [24], increased intersectional stigma due to racialization and sex [25], as well as high rates of unstable housing, poverty, illicit substance use and lack of access to high-quality HIV healthcare [26,27]. For WLWH, who in some settings including Canada and the USA, already experience suboptimal HIV treatment outcomes compared with men [27–30], incarceration is an added obstacle towards achieving optimal health [31]. For transgender women, and especially racialized transgender women, incarceration is associated with mistreatment and increased marginalization within a context of racism and transphobia, resulting in a disproportionate burden of social, mental and physical health disparities [32].
A lack of appropriate programming and supports for WLWH during and after incarceration, including limited supports for accessing healthcare, housing, addiction treatments and employment opportunities [33], has been linked to recidivism [34]. In addition, women are also more commonly tasked with additional responsibilities of taking care of their families [35], which can take precedent over their own health, including HIV care for some WLWH [36,37]. Barriers facing postincarceration add to the challenges for achieving viral suppression [38] and a loss of the potential health benefits from the provision of HIV care during incarceration [39]. There is currently limited understanding of the specific impacts of incarceration on HIV outcomes and continuity of care among WLWH on a global scale. Amidst a call for action and better interventions for incarcerated populations living with HIV [40], we conducted a systematic review to summarize the existing knowledge concerning how incarceration shapes HIV treatment adherence, viral suppression and continuity of care across incarceration trajectories (the pathways that characterize the carceral experience, including pretrial detention, incarceration and post release) among WLWH. A better understanding of the current state of knowledge will guide future research priorities and inform the development of interventions for WLWH who experience incarceration.
MATERIALS AND METHODS
Our systematic review was conducted and reported on the basis of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [41].
Search strategy
Seven databases (OVID Medline, Web of Science, PsycINFO, Cumulative Index to Nursing and Allied Health Literature, Sociological abstracts, Cochrane Library and EMBASE) were searched to reflect the following three distinct search term
domains: Incarceration, Women (transgender women) and HIV. The terms used in our literature search were ‘incarceration’ OR ‘incarcerated’ OR ‘prison*’ OR ‘jail*’ OR ‘detention centre*’ OR ‘detention center*’ AND ‘women’ OR ‘female*’ OR ‘trans’ OR ‘transgender’ OR ‘transsexual’ ‘woman’ AND ‘HIV’ OR ‘AIDS’ OR ‘human immunodeficiency virus’ OR ‘acquired immunodeficiency syndrome’ OR ‘acquired immune deficiency syndrome’ OR ‘HIV infections’. We used the following medical subject heading (MeSH) terms: for the Incarceration search domain: ‘Prisoners’, ‘Prisons’, ‘Legal Detention’, ‘Recidivism’, ‘Correctional Facilities’; for the sex and sexual identity search domain - ‘Transgender Persons’, ‘Transgender’, ‘Women’; and for the HIV domain - ‘HIV infections’. We developed search strategies with the assistance of a qualified librarian. Studies were restricted to the English language research, published between 1 January 2007 and 15 February 2017.
Our initial search amounted to 1119 unique English-language. Three reviewers (A.S., M.E., A.K.) evaluated the articles in three distinct stages to assess the relevance of each record.
Inclusion
Articles were included in the initial review process if they were peer-reviewed quantitative and/or qualitative studies, matched at least one term within each of the three search term domains and were published in English between January 2007 and February 2017.
Studies were included if the sample population involved HIV-seropositive women (transgender inclusive) with a history of incarceration, defined as involvement in the criminal justice system that resulted in one or more nights in either jail or prison, or those currently incarcerated. Studies that did not focus exclusively on women (i.e. inclusive of both men, women and transgender participants) were only included if they contained analysis of our outcomes of interest stratified by sex/gender. Of these studies, articles were included for evaluation if they provided data specific to WLWH during or following periods of incarceration that related to one of the following three HIV-related outcomes: HIV viral load, adherence to ART and engagement in care. Please see Table 1 for a detailed description of the outcomes definition, inclusion criteria and rationale [31,39,42,43]. To be included in the final review, studies had to report outcomes with the above-mentioned criteria through either appropriate statistical tests or the estimation of effect measures and confidence intervals (CIs), or through qualitative methods.
Table 1.
Summary of definitions for main outcomes of interests for women living with HIV who experience incarceration.
| Outcome | Definition and inclusion criteria | Additional definition or rational |
|---|---|---|
| HIV viral load (VL) | Serology data that examined HIV viral load | Viral suppression was defined as having a VL ≤400 copies/ml, as defined by the majority of studies that reported this outcome [31,39,42,43] |
| Adherence to ART | Self-reported ART adherence, or other measures (i.e. pharmacy data) that confirmed achieving a predefined threshold of adherence whenever possible | Optimal adherence referred to ≥90, ≥95 or 100% |
| Engagement in care | Any HIV-related care reported along the incarceration trajectorya. | Examples include accessing HIV-related healthcare either in the context of primary care or HIV specialist care, having a regular HIV care provider, being prescribed ART, postrelease HIV care discharge planning, referrals to HIV-specific services and so on |
ART, antiretroviral therapy.
No requirement for a longitudinal component (i.e. more than one follow-up visit).
Search protocol and data extraction
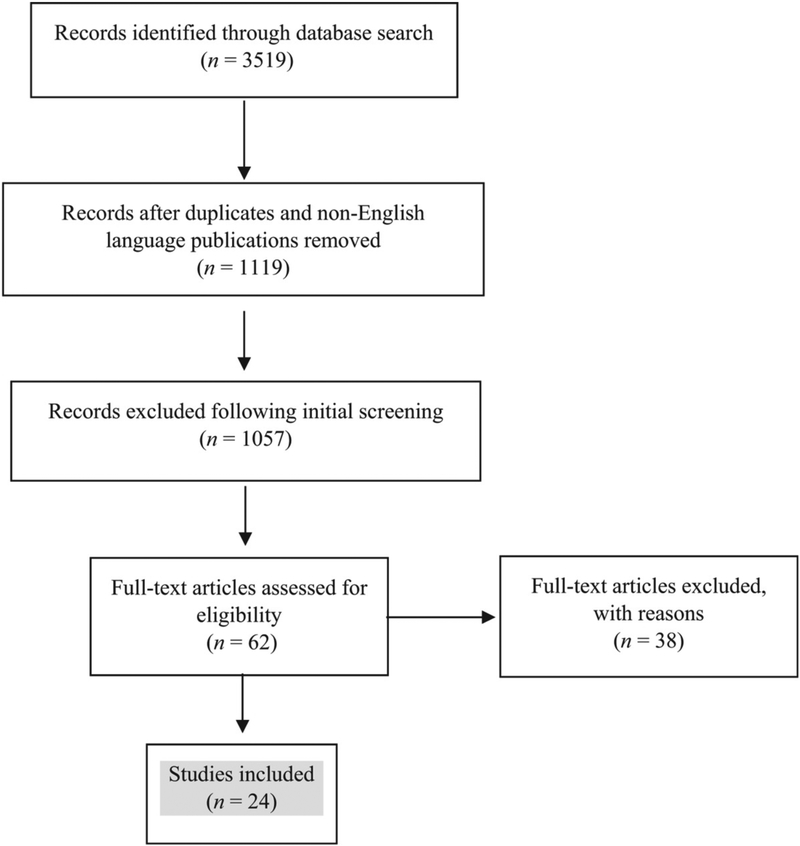
One author conducted the database search and compiled studies matching one or more terms for each of the search criteria groups. After removing duplicates, at least two authors reviewed titles and abstracts and excluded studies that did not meet the inclusion criteria. Full-text versions of all remaining potentially eligible articles were retrieved and independently reviewed, by two or three authors, to determine eligibility; 24 full-text peer-reviewed published articles met our inclusion criteria and were included in this systematic review. See Fig. 1 for flowchart of search strategy and data extraction process.
Figure 1.
Search strategy and data extraction process
RESULTS
As outlined in Fig. 1, of the identified 1119 unique publications from our original search, 24 studies (2%) met the full inclusion criteria and are included in this report [31,32,39,42–62]. Characteristics for the included studies are described in Table 2. Notably, all included publications were conducted in the USA, with the exception of one study set in Spain [59]. The studies include cross-sectional and longitudinal design, including 22 quantitative and two qualitative studies [56,57]. A significant number of studies (n = 6, 25%) utilized data from the Enhancing Linkages to HIV Primary Care in Jail Settings Initiative (EnhanceLink), a multisite study of 20 prisons across the United States evaluating HIV testing and linkages to care postrelease, which included 8056 PLWH [42]. In order to highlight findings across the incarceration trajectory, we separated results in two distinct tables. Table 3 includes outcomes of interest reflecting periods of incarceration (i.e. access to ART or viral suppression during incarceration and so on). Table 4 outlines findings captured following release from prison or postincarceration (i.e. engagement in care, adherence and viral suppression following release from prison). Studies that specifically captured findings related to individuals who experienced reincarceration were also included in Table 3. Tables 3 and 4 are further subdivided to include each of our outcomes of interest (i.e. viral load, adherence, engagement in care).
Table 2.
Summary of study characteristics and outcome measures on HIV treatment access, continuity of care and health outcomes across incarceration trajectories.
| Ref. | Study design and data source | Facilityb, Setting | Population of PLWH [n,(% of total sample)] | Reported HIV outcome for WLWH | ||
|---|---|---|---|---|---|---|
| VL | Adherence | Engagement in care | ||||
| Althoff et al. [44] | Prospective cohort study enhancing linkages to HIV Primary Care and Services in Jail Setting Initiative (EnhanceLink) | Jail, Multi-Site, USA | Women: 281 (32%) Men: 586 (68%) |
✓ | ||
| Baillargeon et al. [46] | Retrospective cohort study Texas Department of Criminal Justice (TDCJ) EMR, Centralized Patient Care Data Management System (CPCDMS) | Prison, Texas, USA | Women: 353 (17%) Men: 1762 (83%) |
✓ | ✓ | |
| Baillargeon et al. [45] | Retrospective cohort study TDCJ EMR and CPCDMS | Prison, Texas, USA | Women: 386 (22%) Men: 1364 (78%) |
✓ | ✓ | |
| Beckwith et al. [47] | Cross-sectional CARE+ Corrections Study, DC Department of Corrections | Jail, multisite, USA | Women: 26 (24%) Transgender Women: 20 (18%) Men: 64 (58%) |
✓ | ✓ | |
| Booker et al. [63] | Prospective cohort study EnhanceLink | Jail, multisite, USA | Women: 301 (29%) Transgender Women: 17 (2%) Men: 703 (69%) |
✓ | ||
| Boyd et al. [48] | Prospective cohort study EnhanceLink | Jail, Connecticut, USA | Women: 33 (30%) Men: 76 (70%) |
✓ | ||
| Clements-Noelle et al. [49] | Cross-sectional The San Francisco Department of Public Health’s Forensic AIDS Project | Jail, San Francisco, USA | Women (Transgendera): 32 (18%) M: 145 (82%) | ✓ | ||
| Jaffer et al. [50] | Cross-sectional The New York City (NYC) Department of Health and Mental Hygiene’s Correctional Health Services (CHS) | Jail, New York, USA | Women: 132 (22.3%) Men: 461 (77.7%) |
✓ | ||
| Lavanbakht et al. [51] | Cross-sectional Los Angeles County Sheriff’s Department and LA County Department of Public Health | Jail, Los Angeles, USA | Women: 84 (1.1% incarcerated women being tested for HIV) | ✓ | ||
| Meyer et al. [53] | Prospective cohort study Project CONNECT, Connecticut Department of Corrections (CTDOC) | Jail, Connecticut, USA | Women: 28(19%) Men: 123 (81%) |
✓ | ||
| Meyer et al. [43] | Prospective cohort study EnhanceLink | Jail, multisite, USA | Women: 277 (32%) Men: 590 (68%) |
✓ | ✓ | ✓ |
| Meyer et al. [40] | Retrospective cohort study CTDOC | Jail/Prison, Connecticut, USA | Women: 168 (19%) Men: 714(81%) |
✓ | ||
| Meyer et al. [47] | Retrospective cohort study CTDOC | Jail/Prison, Connecticut, USA | Women: 163 (18%) Men: 696 (79%) | ✓ | ✓ | |
| Meyer et al. [54] | Retrospective cohort study CTDOC | JaiI/Prison, Connecticut, USA | Women: 223 (21%) Men: 866 (79%) |
✓ | ||
| Pai et al. [55] | Retrospective cohort study The San Francisco City and Country jail’s Forensic AIDS Project (FAP) | Jail, San Francisco, USA | Women: 63 (12%) Transgender: 8 (2%) Men: 441 (86%) |
✓ | ||
| Reisner et al. [33] | Cross-sectional The National Transgender Discrimination Survey (NTDS); cross-sectional | Jail/Prison, multisite, USA | Transgender WLWH: 88 (12% of transgender women with a history of incarceration) | ✓ | ||
| Roberson et al. [59] (2008) | Secondary analysis of qualitative data | Prison, North Carolina, USA | Women: 12 (100%) | ✓ | ✓ | |
| Roberson et al. [57] (2012) | Secondary analysis of qualitative data | Prison, North Carolina, USA | Women: 12 (100%) | ✓ | ||
| Seth et al. [58] | Cross-sectionala National HIV Prevention Program Monitoring and Evaluation (NHM&E) | Jail/Prison, multisite, USA | Women: 165 (20%) Men: 676 (80%) |
✓ | ||
| Spaulding et al. [39] | Prospective cohort study EnhanceLink | Jail, multisite, USA | Women: 328 (30%) Men (Transgendera): 754 (70%) | ✓ | ||
| Sordo et al. [59] | Cross-sectional Medical Outcomes Study (MOS) | Prison, multisite, Spain | Women: 49 (8%) Men: 536 (92%) |
✓ | ||
| Teixeira et al. [60] | Prospective cohort study New York City Department of Health and Mental Hygiene (DOHMH) | Jail, New York, USA | Women: 87 (20%) Transgender women: 9 (2%) Men: 338 (78%) |
✓ | ||
| Williams et al. [32] | Prospective cohort study EnhanceLink | Jail, multisite, USA | Women: 350 (28%) Men: 920 (72%) |
✓ | ✓ | ✓ |
| Youmans et al. [61] | Retrospective cohort study South Carolina HIV/AIDS Reporting System (eHARS), the SC Department of Corrections and the SC Law Enforcement Division Computerized Criminal History Database | Jail/Prison, South Carolina, USA | WLWH with a history of criminal justice involvement: 678 (74%) | ✓ | ||
PLWH, people living with HIV; WLWH, women living with HIV.
Transgender = Inclusive of transgender participants.
Of note, Jails are typically designed to hold individuals awaiting trial, or those with shorter sentences, whereby Prisons are characterized by longer sentences.
Table 3.
Summary of studies reporting on viral suppression, adherence or engagement in care during incarceration.
| Ref. | Viral suppression | Adherence | Engagement in care |
|---|---|---|---|
| Baillargeon et al. [46] | - | - | 41% of women vs. 49% of men received ART while incarcerated 25% of women vs. 33% of men received enhanced HIV discharge planning |
| Beckwith et al. [47] | - | - | 67% of women vs. 95% of transgender women vs. 96% of men received ART during incarceration |
| Jaffer et al. [50] | - | - | 65% of known status women vs. 77% of known status men continued ART treatment at intake or initiated ART within 2 weeks of intake; 35% of women vs. 23% of men were not on treatment |
| Javanbakht et al. [51] | - | - | 100% HIV-positive cases received ART and were successfully referred to case manager to ensure linkages to healthcare following release |
| Meyer et al. [54] | 30% of women vs. 34% of men had viral suppression upon entry; 80% of women vs. 69% of men had viral suppression upon release | - | - |
| Meyer et al. [40] | 79% of women vs. 68% of men achieved viral suppression upon release | - | - |
| Pai et al. [55] | VL not significant based on sex in multivariate model | - | 71% of women vs. 63% of transgender participants vs. 76% of men took ART during incarceration 18% of women vs. 13% of transgender participants vs. 7% of men refused ART |
| Reisner et al. [33] | - | - | Transgender WLWH not at an increased risk of denial of healthcare in jail/prison (RR: 1.57; 95% Cl: 0.85–2.91, P = 0.15) |
| Roberson et al. [57] | - | ART adherence determined by medication line, stigma, access to medication, administration choice, relationships with healthcare team, prison policies, receiving education and counselling about the disease and medical privacy | - |
| Roberson et al. [56] | - | Medications line and lack of medical privacy seen as a barrier to adherence Relationships with healthcare providers both hindered and helped adherence | - |
| Sordo et al. [59] | - | - | 11% of women vs. 7.8% of men did not receive ART treatment |
| Williams et al. [32] | 69% of women vs. 72% of men had VL suppression at release | - | - |
CI, confidence interval; RR, risk ratio.
Table 4.
Summary of studies reporting on viral suppression, adherence or engagement in care postincarceration.
| Ref. | VL suppression | Adherence | Engagement in care |
|---|---|---|---|
| Althoff et al. [44] | - | - | Women (referent) are less likely than men to be retained in care in both early and late retention stages postrelease to be retained in care in early and late retention post release (AOR = 2.10, P≤0.01) |
| Baillargcon et al. [46] | 52% of women vs. 56% of men had an undetectable VL at baseline | - | 23% of women (RR: 0.9; Cl: 0.7–1.1, P = 0.20) vs. 31% of men had an ART prescription filled ≤ 60 days postrelease |
| Baillargeon et al. [45] | 31% of women vs. 38% of men had undetectable VL at baseline | - | 18% of women (OR: 1.0; Cl: 0.7–1.3) vs. 21% of men initiated in HIV outpatient care≤30 days postrelease. |
| 24% of (OR: 0.8; Cl: 0.6–1.1) vs. 29% of men initiated in HIV outpatient care ≤ 90 days postrelease | |||
| Beckwith et al. [47] | 48% of women vs. 80% transgender women vs. 69% of men had VL suppression (<200copies/ml) at baseline following release | 77% of women vs. 100% of transgender women vs. 75% of men had an HIV care provider in community postrelease | |
| 85% of women vs. 90% of transgender women vs. 86% of men reported currently taking HIV treatment | |||
| Booker et al. [63] | - | - | 26% of women (OR: 1.1; Cl: 0.6–2.0) vs. 24% of transgender women (OR: 0.7; Cl: 0.2–1.9) vs. 19% of men (referent) were not linked to care within 30 days postrelease |
| Boyd et al. [48] | - | - | More women vs. men frequently accessed the emergency department postrelease (IRR: 2.4; Cl: 1.4–4.4) |
| Clements-Noelle et al. [49] | - | - | 67% of women and transgender participants vs. 57% of men with a history of ART were engaged in care in the month proceeding reincarceration |
| Meyer et al. [53] | - | - | Women were more likely than men to have two or more Emergency Department visits (OR: 2.07; Cl: 0.65–6.6) within 12 months postrelease |
| Meyer et al. [40] | VL upon reincarceration not significant by sex | - | 71% of women vs. 45% of men experienced recidivism (compared with 362 nonrecidivists, the 497 recidivists were more likely to be women), P = 0.0003 |
| Meyer et al. [54] | 26% of women (referent) vs. 25% of men (AOR:2.0; Cl: 1.3.6, P = 0.02) had achieved viral suppression at baseline | 18% of women vs. 29% of men had optimal ART adherence at baseline; | 65% of women vs. 73% of men had a usual HIV provider at baseline |
| 18% of women vs. 30% of men achieved viral suppression at 6-month follow up (AOR: 2.88; Cl: 1.4–5.8, P≤ 0.001) | 28% of women vs. 44% of men had optimal ART adherence at 6-month follow-up | 50% of women vs. 63% of men had a usual HIV provider at 6-month follow-up | |
| Pai et al. [55] | - | - | 10% of women vs. 13% of transgender women vs. 16% of men had continuous use of ART (following release) |
| 18% of women vs. 13% of transgender women vs. 7% of men refused ART | |||
| Seth et al. [58] | - | - | 36% of women vs. 38% of men linked to HIV care within 90 days; |
| 67% of women vs. 68% of men linked to care at any time frame (within 90 days and >90 days) | |||
| Hispanic/Latina women more likely to be linked to care than black women and white women (70 vs. 35 vs. 28%) after 90 days | |||
| Spaulding et al. [39] | Men (trans*) more likely to be virally supressed at 6-month follow up compared to women (OR: 1.66; Cl: 1.09–2.53) | - | - |
| Teixeira et al. [60] | - | - | 62% of women vs. 78% of transgender women vs. 38% of men lost to follow-up ay 6-month postincarceration |
| Williams et al. [32] | - | - | 49% of women vs. 35% of men reported needing case management; 46% of women vs. 34% of men reported needing HIV medical services. |
| Women who expressed more needs were significantly less likely than men to engage and stay in care (OR: 0.90; Cl: 0.84–0.97) | |||
| Youmans et al. [61] | - | - | Women who were arrested |
| (HR: 1.92, 95% Cl: 1.43–2.58) and women who went to prison (HR: 2.27, 95% Cl: 1.52–3.39) had an increased risk of developing AIDS when compared with women without criminal justice-involvement |
ART, antiretroviral therapy; confidence interval; HR, hazard ratio; IRR, incidence rate ratio; OR, odds ratio; RR, risk ratio; VL, viral load.
During incarceration
Twelve studies reported on HIV outcomes and engagement in care among WLWH during incarceration (see Table 3). With regards to sex disparities in HIV outcomes during incarceration, five studies found that a smaller proportion of women received ART while incarcerated compared with men [45,47,50,55,59]. When reasons for sex disparities in ART access were discussed at all, the authors mainly attributed it to shorter sentences among women. Although only a small amount of research compiled data for transgender women, Pai et al. [55] found that transgender women were slightly less likely than cisgender women to receive ART while incarcerated (63 vs. 71%), while Beckwith et al. [47] found that transgender women were significantly more likely to receive ART while incarcerated compared with ciswomen (95 vs. 67%) in their sample.
Of the analyses measuring viral suppression at release from incarceration, two studies found that women were slightly more likely to achieve viral suppression during incarceration within Connecticut correctional facilities in the United States [39,54], yet slightly less likely to achieve viral suppression compared with men from multisite data with the EnhanceLink Study [31]. No studies reported quantitative measures of ART adherence during incarceration. In qualitative studies, WLWH reported that adherence to ART was shaped by a variety of factors, including privacy concerns, experience of stigma, and quality of relationships with healthcare and prison staff. WLWH also reported that access to medications and types of administration affected adherence (i.e. WLWH reported concerns regarding loss of privacy with directly observed therapy as well as with keeping medications in their sleeping quarters due to fear of inadvertent disclosure to cell mates) [56,57].
Postincarceration
Sixteen studies reported outcomes for periods postincarceration (see Table 4). Overall, the majority of these studies reported worse HIV outcomes postincarceration for women compared with men.
Although a limited number of studies reported on viral load postincarceration (n = 6), women were overall less likely to achieve viral suppression in the months following release from prison [38,45–47,53], with the exception of one study that found no sex differences in viral suppression [43]. The one study that reported on ART adherence postincarceration indicated that women were significantly less likely to report optimal adherence 6 months postincarceration compared with men (28 vs. 44%) [53].
The majority of studies exploring periods of postincarceration reported on factors related to engagement in care in the period following release from prison. An overwhelming amount of these studies indicated that women experienced worse outcomes compared with men concerning engagement in care postincarceration [31,38,44–46,48,49,52,53,55,60,62]. One study demonstrated that men were twice as likely (AOR = 2.10; CI 1.42–3.11; P < 0.01) to be retained in care postincarceration compared with women [44]. Women were also less likely to fill ART prescriptions [46], less likely to have a regular HIV care provider postincarceration [53] and significantly more likely to be lost to follow-up following incarceration (62% of women vs. 78% of transgender women vs. 38% of men) [60]. Two separate studies found that WLWH were over twice as likely to access hospital emergency departments compared with men postincarceration [IRR: 2.4; CI: 1.4–4.4 and odds ratio (OR): 2.07; CI: 0.65–6.6, respectively] [48,52].
Women also expressed different needs postincarceration compared with men. Although men commonly reported needing assistance with employment, job training and legal services, women’s needs focused on basic sustenance needs, including securing cash, food, clothing and transportation, along with the added need for case management and both HIV and general medical services [31]. Women who expressed more needs were significantly less likely than men to engage and stay in care postincarceration [31].
DISCUSSION
A systematic review of the literature revealed a concerning scarcity of global research surrounding the impact of incarceration on HIV outcomes among WLWH in the last decade. Of the limited research that exists, our review of the literature identified significant sex disparities in HIV outcomes and engagement in care following release from correctional facilities, suggesting substantial gaps in care for WLWH after incarceration.
Results from our review show inconsistencies in delivery of ART and viral suppression during incarceration for WLWH; research using data from four different US-based cohorts demonstrated that the percentage of WLWH who received ART during incarceration was below 50% [50,55] and of those provided treatment under 70% achieved viral suppression by the time of their release [31,39]. One study revealed that women with a history of incarceration were over twice as likely to develop AIDS compared with women who were never incarcerated [61].
The most pronounced and significant sex differences in HIV outcomes for women were observed in the period following incarceration. Release from correctional facilities is often complex and disruptive for individuals reintegrating into their communities [63]; our findings highlight barriers to optimal HIV outcomes for WLWH and point to potentially unique challenges faced by WLWH postincarceration. For example, although in one study 77% of cisgender women had an HIV care provider in the community after release, only 48% of these women achieved viral suppression in the same period [64]. In another study, 65% of women had an HIV provider at release, yet at the 6-month follow-up, this number dropped to 50% [53]. Another analysis found that 26% of women had not been linked to any HIV care within 30 days postrelease [62].
Outcomes for transgender women
This study also highlights the lack of research and visibility for transgender WLWH who experience incarceration. The one study that examined the unique experiences of transgender women with a history of incarceration, of whom 11.7% were living with HIV, highlighted the overall lack of robust research surrounding the impact of incarceration for transgender women, often related to small sample sized and limitations in research design [32]. With the exception of the above study, no mention of sex identity affirming practices, in regards to what type of correctional facility (i.e. male or female) transgender participants were imprisoned within, existed within any of the studies. This adds a level of complexity when analysing findings for this population.
Structural vulnerabilities and intersecting factors for women living with HIV
Alongside sex disparities, many studies highlighted intersecting factors that increased poor HIV outcomes for women. Compared with men, WLWH who were incarcerated were significantly more likely to experience homelessness and illicit substance use prior to and following periods of incarceration [53]. WLWH also experienced higher rates of both mental and physical illness than their male counterparts [31]. Age and race also constituted significant barriers to optimal health, whereby younger age [43,45,54,62] and being black [31,52] were consistently associated with gaps in linkages to care and adherence to ART. This is particularly concerning given the vast overrepresentation of racialized and marginalized WLWH in correctional systems globally [16]. In Canada for example, indigenous WLWH reported the highest HIV rates among the incarcerated population [65]. As the majority of research complied in this analysis was conducted in the United States, it is important to highlight the vast overrepresentation of black people in the United States correctional system due to various structural vulnerabilities, including institutionalized racism, economic marginalization and the overpolicing and criminalization of black communities in the United States [66]. Consequently, black and other racialized WLWH face unique intersectional vulnerabilities that are not well captured in the current literature on HIV outcomes and incarceration experiences. WLWH also face disproportionate rates of trauma [67], with gendered power dynamics and violence linked to poor HIV health outcomes for WLWH [24,68,69], including disengagement from HIV care following release from correctional facilities [53]. Historically, correctional facilities were designed for men [70], yet with the increasing rates of incarcerated women worldwide, little has been done to adjust for how the needs of women may differ within carceral settings. Incarcerated women are unique in comparison to incarcerated men, with women’s criminal justice involvement being predominantly related to poverty, mental health issues and illicit substance use, rather than violent crime [70]. This translates to shorter sentences, which can lead to more frequent interruptions in HIV treatment, and poorer HIV outcomes for WLWH [54]. In addition, as previously described, research found that women’s needs postincarceration were more focused on basic needs of health and social services, whereby men expressed needs surrounding employment, job training and legal services [31]. Consequently, women’s unmet needs postrelease were associated with poorer HIV health outcomes overall [31]. Unfortunately, despite varying needs and increased structural vulnerabilities for women, there is an overall lack of support given to WLWH upon release to community; one study in our review reported only 25% of women received HIV discharge planning upon release from prison [45].
Recommendations and suggested interventions
For WLWH, incarceration is a compounding structural vulnerability that adds to an existing list of barriers undermining the potential to achieve optimal health. The findings of this systematic review expose the significant sex disparities and negative impact of incarceration for WLWH, and highlight the need for enhanced discharge planning and specific sex-informed interventions, including trauma-informed care [71], during and following incarceration to address the sex-specific needs of incarcerated WLWH. An increase in robust longitudinal research is needed to identify the sex-specific needs of incarcerated WLWH. Future studies need to focus on the effects of incarceration among various subgroups of WLWH, including those who are racialized, live in poverty, suffer from mental health conditions or are criminalized due to illicit substance use. This will help to elucidate the constitutive and intersectional relationships between social and structural factors that intersect to shape HIV outcomes and continuity of care along incarceration trajectories. Future research should include consistent HIV viral load monitoring upon entry into correctional facilities coupled with research surrounding the health and wellbeing of WLWH during times of arrest in order to gain a better sense of the impact of incarceration for WLWH. Finally, given the dearth in data on transgender PLWH who experience incarceration, more research is needed to respond to the specific needs of this population.
Limitations
There are several limitations that should be noted in this study. First, as the overwhelming majority of studies were conducted in the United States, findings cannot be generalized to inform global perspective on the impact of incarceration for WLWH. Many studies utilized data from the same study samples; notably, six studies included in this review drew from the EnhanceLink project. Although the EnhanceLink sample is extensive and includes over 8000 participants, this narrows the generalizability of our findings. In addition, many studies did not identify the HIV treatment guidelines that pertained to their study population and location at the time of the study thus limiting conclusions regarding how HIV care differed between community and carceral settings. As most studies did not stratify structural vulnerabilities (i.e. race, substance use, homelessness and so on) based on sex, we were unable to draw conclusions on how sex intersects with various structural vulnerabilities incarcerated WLWH face to shape HIV outcomes and engagement in care. Furthermore, not all studies distinguished transgender participants from cisgender participants and most were limited by small sample sizes of transgender participants [55,60]. Therefore, conclusions about the unique impacts of incarceration among transgender PLWH are limited.
Conclusion
This systematic review demonstrates that despite growing numbers of incarcerated WLWH globally, there remain substantial gaps in research examining the impact of incarceration on health and HIV outcomes for women. In the period of postincarceration, our review revealed significant sex disparities in women’s needs, HIV outcomes and continuity of care for WLWH. Following release from correctional facilities, women are less likely to be virally suppressed, less likely to achieve optimal ART adherence and less likely to be engaged and retained in care. This review highlights the critical need to better understand the experiences of WLWH throughout incarceration trajectories, and the need to develop cisgender and transgender women-centred interventions. In order to improve postrelease engagement in healthcare and HIV outcomes for WLWH, and address the overcriminalization of WLWH, efforts addressing the intersectional structural vulnerabilities faced by WLWH are urgently needed.
Acknowledgements
A.S. completed the initial database search, M.E., A.S. and A.K. screened the research for eligible studies and finalized the included studies. M.E. wrote the drafts and final versions of the manuscripts with extensive input from A.S., A.K., N.P., F.R., R.E.M. and K.S. K.S. and A.K. obtained the funding for this study. Funding for this study was provided by Canadian Institute of Health Research: (CBR151184, FDN143349).
Footnotes
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Montaner JSG, Lima VD, Harrigan PR, Lourenco L, Yip B, Nosyk B, et al. Expansion of HAART coverage is associated with sustained decreases in HIV/AIDS morbidity, mortality and HIV transmission: the ‘HIV Treatment as Prevention’ experience in a Canadian setting. PLoS One 2014; 9:e87872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UNAIDS. Global AIDS update 2016. Geneva: UNAIDS; 2016. http://www.unaids.org/sites/default/files/media_asset/global-AIDS-update-2016_en.pdf. [Google Scholar]
- 3.Hull MW, Wu Z, Montaner JSG. Optimizing the engagement of care cascade. Curr Opin HIV AIDS 2012; 7:579–586. [DOI] [PubMed] [Google Scholar]
- 4.McNairy ML, El-Sadr WM. The HIV care continuum. AIDS 2012; 26:1735–1738. [DOI] [PubMed] [Google Scholar]
- 5.Montaner JS, Lima VD, Barrios R, Yip B, Wood E, Kerr T, et al. Association of highly active antiretroviral therapy coverage, population viral load, and yearly new HIV diagnoses in British Columbia, Canada: a population-based study. Lancet 2010; 376:532–539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Das M, Chu PL, Santos GM, Scheer S, Vittinghoff E, McFarland W, et al. Decreases in community viral load are accompanied by reductions in new HIV infections in San Francisco. PLoS One 2010; 5:e11068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goldenberg SM, Montaner J, Duff P, Nguyen P, Dobrer S, Guillemi S, et al. Structural barriers to antiretroviral therapy among sex workers living with HIV: findings of a longitudinal study in Vancouver, Canada. AIDS Behav 2016; 20:977–986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Milloy MJ, Kerr T, Buxton J, Rhodes T, Guillemi S, Hogg R, et al. Dose-response effect of incarceration events on nonadherence to HIV antiretroviral therapy among injection drug users. J Infect Dis 2011; 203:1215–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Belenko S, Dembo R, Copenhaver M, Hiller M, Swan H, Albizu Garcia C, et al. HIV stigma in prisons and jails: results from a staff survey. AIDS Behav 2016; 20:71–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jurgens R, Nowak M, Day M. HIV and incarceration: prisons and detention. J Int AIDS Soc 2011; 14:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rubenstein LS, Amon JJ, McLemore M, Eba P, Dolan K, Lines R, et al. HIV, prisoners, and human rights. Lancet 2016; 388:1202–1214. [DOI] [PubMed] [Google Scholar]
- 12.UNAIDS. The gap report 2014 Geneva: Joint United Nations Programme on HIV/AIDS. Geneva; 2014. [Google Scholar]
- 13.United Nations Department of Public Information. State of the world’s indigenous peoples press release. 2010. www.un.org/indigenous. [Google Scholar]
- 14.Braithwaite RL, Treadwell HM, Arriola KRJ. Health disparities and incarcerated women: a population ignored. Am J Public Health 2008; 98:S173–S175 Suppl 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walmsley R World Female Imprisonment List Women and girls in penal institutions, including pretrial detainees/remand prisoners. Inst Crim Policy Res 2015:1–13. [Google Scholar]
- 16.United Nations Office on Drugs and Crime; Joint United Nations Programme on HIV/AIDS. Women and HIV in prison settings. Vienna, Austria: United Nations Office on Drugs and Crime; 2008. [Google Scholar]
- 17.Beyrer C, Kamarulzaman A, McKee M. Prisoners, prisons, and HIV: time for reform. Lancet 2016; 388:1033–1035. [DOI] [PubMed] [Google Scholar]
- 18.Dolan K, Kite B, Black E, Aceijas C, Stimson GV. HIV in prison in low-income and middle-income countries. Lancet Infect Dis 2007; 7:32–41. [DOI] [PubMed] [Google Scholar]
- 19.Poulin C, Alary M, Lambert G, Godin G, Landry S, Gagnon H, et al. Prevalence of HIV and hepatitis C virus infections among inmates of Quebec provincial prisons. Can Med Assoc J 2007; 177:252–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Avery AK, Ciomcia RW, Lincoln T, Desbrais M, Jordan AO, Rana AI, et al. Jails as an opportunity to increase engagement in HIV care: findings from an observational cross-sectional study. AIDS Behav 2013; 17:137–144. [DOI] [PubMed] [Google Scholar]
- 21.Uthman OA, Oladimeji O, Nduka C. Adherence to antiretroviral therapy among HIV-infected prisoners: a systematic review and meta-analysis. AIDS Care 2017; 29:489–497. [DOI] [PubMed] [Google Scholar]
- 22.Small W, Wood E, Betteridge G, Montaner J, Kerr T. The impact of incarceration upon adherence to HIV treatment among HIV- positive injection drug users: a qualitative study. AIDS Care 2009; 21:708–714. [DOI] [PubMed] [Google Scholar]
- 23.Smith LR, Yore J, Triplett DP, Urada L, Nemoto T, Raj A. Impact of sexual violence across the lifespan on HIV risk behaviors among transgender women and cisgender people living with HIV. JAIDS J Acquir Immune Defic Syndr 2017; 75:408–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lichtenstein B Domestic violence in barriers to healthcare for HIV-positive women. AIDS Patient Care STDs 2006; 20:122–132. [DOI] [PubMed] [Google Scholar]
- 25.Logie CH, James L, Tharao W, Loutfy MR. HIV, gender, race, sexual orientation, and sex work: a qualitative study of inter- sectional stigma experienced by HIV-positive women in Ontario, Canada. PLoS Med 2011; 8:e1001124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aziz M, Smith KY. Challenges and successes in linking HIV- infected women to care in the United States. Clin Infect Dis 2011; 52 (Suppl 2):231–237. [DOI] [PubMed] [Google Scholar]
- 27.Carter A, Eun Min J, Chau W, Lima VD, Kestler M, Pick N, et al. Gender inequities in quality of care among HIV-positive individuals initiating antiretroviral treatment in British Columbia, Canada (2000–2010). PLoS One 2014; 9: e92334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hogg RS, Milloy M-J, Kerr T, Zhang R, Guillemi S, Hogg RS, et al. Rates of disease progression by baseline CD4 cell count and viral load after initiating triple-drug therapy. JAMA 2001; 286:2568–2577. [DOI] [PubMed] [Google Scholar]
- 29.Sohler NL, Li X, Cunningham CO. Gender disparities in HIV healthcare utilization among the severely disadvantaged: can we determine the reasons? AIDS Patient Care STDS 2009; 23:775–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Puskas CM, Kaida A, Miller CL, Zhang W, Yip B, Pick N, et al. The gender gap: a longitudinal examination of men’s and women’s art adherence in British Columbia, 2000–2014. AIDS 2017; 31:827–833. [DOI] [PubMed] [Google Scholar]
- 31.Williams CT, Kim S, Meyer J, Spaulding A, Teixeira P, Avery A, et al. Gender differences in baseline health, needs at release, and predictors of care engagement among HIV-positive clients leaving jail. AIDS Behav 2013; 17 (Suppl 2):S195–S202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Reisner SL, Bailey Z, Sevelius J. Racial/ethnic disparities in history of incarceration, experiences of victimization, and associated health indicators among transgender women in the U.S. Women Health 2014; 54:750–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Martin R, Buxton J, Smith M, Hislop G. The scope of the problem: the health of incarcerated women in BC. BC Med J 2012; 54:10. [Google Scholar]
- 34.Fu JJ, Herme M, Wickersham JA, Zelenev A, Althoff A, Zaller ND, et al. Understanding the revolving door: individual and structural-level predictors of recidivism among individuals with HIV leaving jail. AIDS Behav 2013; 17 (Suppl 2):S145–S155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kruttschnitt C The paradox of women’s imprisonment. Daedalus 2010; 139:32–42. [DOI] [PubMed] [Google Scholar]
- 36.UNAIDS. Gender and HIV /AIDS: UNAIDS technical update. Geneva: UNAIDS; 1998. https://www.popline.org/node/530050. [Google Scholar]
- 37.Murphy DA, Roberts KJ, Herbeck DM. HIV disease impact on mothers: what they miss during their children’s developmental years. J Child Fam Stud 2011; 20:361–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spaulding AC, Messina LC, Kim BI, Chung KW, Lincoln T, Teixeira P, et al. Planning for success predicts virus suppressed: results of a non-controlled, observational study of factors associated with viral suppression among HIV-positive persons following jail release. AIDS Behav 2013; 17:203–211. [DOI] [PubMed] [Google Scholar]
- 39.Meyer JP, Cepeda J, Wu J, Trestman RL, Altice FL, Springer SA. Optimization of human immunodeficiency virus treatment during incarceration: viral suppression at the prison gate. JAMA Intern Med 2014; 174:721–729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.UNODC, ILO, UNDP, WHO, UNAIDS. HIV prevention, treatment and care in prisons and other closed settings: a comprehensive package of interventions. Vienna, Austria: United Nations Office on Drugs and Crime; 2013. [Google Scholar]
- 41.Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Spaulding AC, Booker CA, Freeman SH, Ball SW, Stein MS, Jordan AO, et al. Jails, HIV testing, and linkage to care services: an overview of the EnhanceLink initiative. AIDS Behav 2013; 17:100–107. [DOI] [PubMed] [Google Scholar]
- 43.Meyer JP, Cepeda J, Springer SA, Wu J, Trestman RL, Altice FL. HIV in people reincarcerated in Connecticut prisons and jails: An observational cohort study. Lancet HIV 2014; 1:e77–e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Althoff AL, Zelenev A, Meyer JP, Fu J, Brown S-E, Vagenas P, et al. Correlates of retention in HIV care after release from jail: results from a multisite study. AIDS Behav 2013; 17 (Suppl 2):S156–S170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Baillargeon JG, Giordano TP, Harzke AJ, Baillargeon G, Rich JD, Paar DP. Enrollment in outpatient care among newly released prison inmates with HIV infection. Public Health Rep 2010; 125:64–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Baillargeon J, Giordano TP, Rich JD, Wu ZH, Wells K, Pollock BH, et al. Accessing antiretroviral therapy following release from prison. J Am Med Assoc 2009; 301:848–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Beckwith C, Castonguay BU, Trezza C, Bazerman L, Patrick R, Cates A, et al. Gender differences in HIV care among criminal justice-involved persons: baseline data from the CARER correction study. PLoS One 2017; 12:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Boyd AT, Song DL, Meyer JP, Altice FL. Emergency department use among HIV-infected released jail detainees. J Urban Health 2015; 92:108–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Clements-Nolle K, Marx R, Pendo M, Loughran E, Estes M, Katz M. Highly active antiretroviral therapy use and HIV transmission risk behaviors among individuals who are HIV infected and were recently released from jail. Am J Public Health 2008; 98:661–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jaffer M, Kimura C, Venters H. Improving medical care for patients with HIV in New York City jails. J Correct Heal Care 2012; 18:246–250. [DOI] [PubMed] [Google Scholar]
- 51.Javanbakht M, Boudov M, Anderson LJ, Malek M, Smith LV, Chien M, et al. Sexually transmitted infections among incar- cerated women: findings from a decade of screening in a Los Angeles county jail, 2002–2012. Am J Public Health 2014; 104:e103–e109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Meyer JP, Qiu J, Chen NE, Larkin GL, Altice FL, Mello MJ. Frequent emergency department use among released prisoners with human immunodeficiency virus: characterization including a novel multimorbidity index. Acad Emerg Med 2013; 20:79–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Meyer JP, Zelenev A, Wickersham JA, Williams CT, Teixeira PA, Altice FL. Gender disparities in HIV treatment outcomes following release from jail: results from a multicenter study. Am J Public Health 2014; 104:434–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Meyer JP, Cepeda J, Taxman FS, Altice FL. Sex-related disparities in criminal justice and HIV treatment outcomes: a retrospective cohort study of HIV-infected inmates. Am J Public Health 2015; 105:1901–1910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pai NP, Estes M, Moodie EE, Reingold AL, Tulsky JP. The impact of antiretroviral therapy in a cohort of HIV infected patients going in and out of the San Francisco county jail. PLoS One 2009; 4:e7115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Roberson DW, White BL, Fogel CI. Factors influencing adherence to antiretroviral therapy for HIV-infected female inmates. J Assoc Nurses AIDS Care 2009; 20:50–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Roberson DW. Medical privacy and antiretroviral therapy among HIV-infected female inmates. J Nurs Law 2012; 15:3–8. [Google Scholar]
- 58.Seth P, Figueroa A, Guoshen W, Reid L, Belcher L, Wang G. HIV testing, HIV positivity, and linkage and referral services in correctional facilities in the United States, 2009–2013. Sex Transm Dis 2015; 42:643–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sordo Del Castillo L, Ruiz-Perez I, Olry De Labry-Lima A, Soto-Blanco JM, Girela-Lopez E, Castro-Recio JM, et al. Influence of antiretroviral treatment on quality of life in seropositive inmates. Int J STD AIDS 2008; 19:172–177. [DOI] [PubMed] [Google Scholar]
- 60.Teixeira PA, Jordan AO, Zaller N, Shah D, Venters H. Health outcomes for HIV-infected persons released from the New York City Jail System with a transitional care-coordination plan. Am J Public Health 2015; 105:351–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Youmans E, Burch J, Moran R, Smith L, Duffus WA. Disease progression and characteristics of HIV-infected women with and without a history of criminal justice involvement. AIDS Behav 2013; 17:2644–2653. [DOI] [PubMed] [Google Scholar]
- 62.Booker CA, Flygare CT, Solomon L, Ball SW, Pustell MR, Bazerman LB, et al. Linkage to HIV care for jail detainees: findings from detention to the first 30 days after release. AIDS Behav 2013; 17 (Suppl 2):128–136. [DOI] [PubMed] [Google Scholar]
- 63.Lincoln T, Kennedy S, Tuthill R, Roberts C, Conklin TJ, Hammett TM. Facilitators and barriers to continuing healthcare after jail: a community-integrated program. J Ambul Care manage 2006; 29:2–16. [DOI] [PubMed] [Google Scholar]
- 64.Beckwith C, Bazerman L, Gillani F, Tran L, Larson B, Rivard S, et al. The feasibility of implementing the HIV seek, test, and treat strategy in jails. AIDS Patient Care STDS 2014; 28:183–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Correctional Service of Canada. Summary of emerging findings from the 2007 National Inmate Infectious Diseases and Risk-Behaviours Survey. 2010. http://publications.gc.ca/collections/collection_2010/scc-csc/PS83-3-211-eng.pdf.
- 66.Christian J, Thomas SS. Examining the intersections of race, gender, and mass imprisonment. J Ethn Crim Justice 2009; 7:69–84. [Google Scholar]
- 67.Machtinger EL, Wilson TC, Haberer JE, Weiss DS. Psychological trauma and PTSD in HIV-positive women: a meta-analysis. AIDS Behav 2012; 16:2091–2100. [DOI] [PubMed] [Google Scholar]
- 68.Machtinger EL, Haberer JE, Wilson TC, Weiss DS. Recent trauma is associated with antiretroviral failure and HIV trans- mission risk behavior among HIV-positive women and female-identified transgenders. AIDS Behav 2012; 16:2160–2170. [DOI] [PubMed] [Google Scholar]
- 69.Hatcher AM, Smout EM, Turan JM, Christofides N, Stockl H. Intimate partner violence and engagement in HIV care and treatment among women. AIDS 2015; 29:2183–2194. [DOI] [PubMed] [Google Scholar]
- 70.Penal Reform International. Women in prison: incarcerated in a man’s world [Internet]. Penal Reform Briefing No 3. London: Penal Reform International; 2008. https://www.penalreform.org/wp-content/uploads/2013/06/brf-03-2008-women-in-prison-en.pdf. [Accessed 1 March 2018] [Google Scholar]
- 71.Harner H, Burgess AW. Using a trauma-informed framework to care for incarcerated women. J Obstet Gynecol Neonatal Nurs 2011; 40:469–476. [DOI] [PubMed] [Google Scholar]