Abstract
Background:
The Institute for Healthcare Improvement defines an adverse event (AE) as an “unintended physical injury resulting from or contributed to by medical care that requires additional monitoring, treatment, or hospitalization, or that results in death”. The majority of research has focused on AE’s from the provider’s perspective.
Objective:
The objective of this qualitative study is to describe patient perceptions on AEs following surgery for pelvic floor disorders (PFD).
Study Design:
Women representing 3 separate surgical populations: 1) preoperative (women ≤12 weeks prior to surgery); 2) short-term postoperative (women up to 12 weeks post-surgery); and 3) long-term postoperative (women 1–5 years post-surgery) participated in focus groups. De-identified transcripts of audio recordings were coded and analyzed with NVivo 10 software to identify themes, concepts and AEs. Women were asked to rank patient-identified and surgeon-identified AEs in order of perceived severity.
Results:
81 women participated in 12 focus groups. Group demographics were similar between groups and all groups shared similar perspectives regarding surgical expectations. Women commonly reported an unclear understanding of their surgery and categorized AEs such as incontinence, constipation, nocturia, and lack of improvement in sexual function as “very severe”, ranking these comparably to Intensive Care Unit (ICU) admissions or other major surgical complications. Women also expressed a sense of personal failure and shame if symptoms recurred.
Conclusion:
Women consider functional outcomes such as incontinence, sexual dysfunction, and recurrence of symptoms as severe AEs, and rate them as similar in severity to ICU admissions and death.
Keywords: Funciton outcomes, Pelvic floor disorders, Qualitative study, Surgical adverse events
CONDENSATION:
Women consider adverse functional outcomes, such as incontinence, sexual dysfunction, and symptom recurrence as serious adverse events after surgery for pelvic floor disorders.
Introduction:
Surgical adverse events (AE) are common and range from life threatening complications to deviations from the usual clinical course that are distressing, but not dangerous. AE events following urogynecologic surgery are not uncommon. In review of recent surgical studies conducted by the Pelvic Floor Disorders Network (PFDN), the incidence of any AEs ranged from 30% - 76.3% and SAEs ranged from 3% - 17%.1–4
Institutional monitoring agencies and boards such as the U.S Food and Drug Administration (FDA), the National Institute of Health (NIH), and Institutional Review Boards (IRBs) use established definitions and guidelines to rank and evaluate adverse events (AE). The FDA defines an AE as “any undesirable experience associated with the use of a medical product in a patient”5, this could include a range of events from a urinary tract infection to the return to the operating room. Most IRBs, which provide oversight for surgical trials, implement and use similar language as that used by the FDA for AEs.6–7 In routine clinical care, established classifications of perioperative complications are used, such as the Clavien-Dindo scale8,9, which was validated in the general surgical population and the Pelvic Floor Complication Scale10 (PFCS), which is a more condition-specific classification system for AEs from pelvic reconstructive surgery. Neither of these scales were designed to include patient-identified AEs, such as functional problems that women undergoing PFD surgery may consider important. Patients’ perceptions of AEs may be different than those of the medical or regulatory communities.
In urogynecology there is increased focus on patient goal achievement and expectations, which have been shown to be linked with patient satisfaction.11–13 Patient satisfaction has also been linked to the patient’s experience of what they felt was a complication.14 Recently, a retrospective qualitative study of women who had undergone uterovaginal prolapse surgery found that besides symptom relief, several other factors influenced whether or not patients considered their surgery a success.15 These included a feeling of being normal, sense of independence, sexuality issues and length of recovery. The authors also reported that women received a variety of conflicting information from providers and family that led to confusion regarding their recovery.15 These findings demonstrate that patient expectations and experience of AEs vary from what surgeons typically consider complications16, and may also vary based on their disease process and what counseling they receive. Therefore, the counseling about AEs may influence not only a woman’s decision to have surgery but her satisfaction with her surgical outcome. As increased value is placed on outcomes such as patient experience and satisfaction, it is imperative that surgeons understand the patient perspective on surgical outcomes and harms associated with surgery. Shared decision-making between patients and providers is especially important for women considering surgery for pelvic floor disorders (PFD) as these surgeries are elective, aim to improve function and can be associated with serious complications. Patient-centered care and shared decision-making may be improved with a better understanding of patient perceived impact of specific AEs.
Objectives:
The primary aim of this study was to identify concepts important to patients that are not currently represented in guidelines regarding AEs associated with pelvic reconstructive surgery. We utilized a conceptual framework of the relative importance, from the patient perspective, of surgical AEs, including functional limitations that may result from pelvic reconstructive surgery, to describe what women consider AEs following surgery, and to gain insight as to how women rank the severity of AEs, compared to AEs identified by surgeons. A conceptual framework in qualitative research can be thought of as a network of linked concepts that can be modified as more information is obtained.17, 18
Methods:
We conducted a multi-center qualitative study through the NICHD Pelvic Floor Disorders Network (PFDN). An initial conceptual framework (Figure 1) was developed based on existing AE definitions and scales, prior studies that have explored what patients consider AEs, and expert pelvic surgeon opinion, defined as board certified Female Pelvic Medicine and Reconstructive Surgeon members of the Pelvic Floor Disorders Network, who routinely perform the surgeries to be discussed by the focus groups. In addition, we reviewed studies that have explored what patients consider as complications. Examples of such are anesthesia complications, constipation, fatigue, discharge home with a catheter and continued urgency and urgency urinary incontinence.14, 15, 19 This preliminary framework was developed to provide an opportunity to synthesize the current literature and experience of pelvic surgeons regarding known views of AEs. This preliminary conceptual framework served as the foundation from which to develop questions for an initial interview guide was developed to explore how patients think about risks, complications, and adverse events (Appendix 1).
Figure 1:

Preliminary Patient Conceptual Framework
The preliminary conceptual framework serves as a way to define major concepts of interest based on a literature review and expert opinion and was developed prior to the conduct of the focus groups.
Prior to beginning the study IRB approval was obtained from all sites. We selected an exploratory focus group design, as focus groups would create a dynamic interaction for participants to share perspective on AEs after surgery for PFD. Adult women (≥ 21 years of age) who were able to speak, read, and comprehend English and who had bothersome urinary incontinence (UI) or pelvic organ prolapse (POP) or history of at least one of these disorders that were going to be or were treated with surgery were recruited for the study. As the length of time that has elapsed since surgery may influence perceptions, focus groups were conducted with three separate patient populations: 1) women planning to undergo surgery (≤ 12 weeks from surgery), 2) short-term postoperative women (up to 12 weeks after surgery) and 3) a longer term postoperative group (1–5 years after surgery). Based on qualitative methodology20 and the experience of the research team, we anticipated that a total of 4 focus groups in each of the three patient populations would be sufficient to achieve thematic saturation for a total of 12 focus groups.
Women were recruited from one of four sites in the PFDN (Brown, Cleveland Clinic, Duke, UNM). Site coordinators facilitated recruitment at their respective clinics. At each site, women who were within the study window of planned surgery for a pelvic floor disorders were called to see if they were interested in participating. Similarly, women who had previously undergone a surgery within the two postoperative time windows (up to 12 weeks postoperative or 1–5 years postoperative) and met inclusion criteria were contacted by each sites’ coordinators. One female moderator, experienced in qualitative data collection techniques and employed by the University of New Mexico Community Engagement and Research Core (CERC), led all focus group sessions with co-moderators from the individual sites and ensured equal participation. Prior to the start of the focus groups, women were consented and provided basic demographic information and their Pelvic Floor Disorder (PFD) treated or to be treated with surgery. All women completed the Pelvic Floor Distress Inventory Questionnaire – Short Form 20 (PFDI 20)21 and the Life Orientation Test-Revised (LOT-R)22 an assessment of optimism. Women in the postoperative groups also completed the Patient Global Impression of Improvement (PGI-I)23, the Satisfaction with Decision Scale-Pelvic Floor Disorders (SDS-PFD) as well as the Decision Regret Scale-Pelvic Floor Disorders (DRS-PFD)24. These questionnaires were given to provide a descriptive summary of the focus group sample.
Following the focus group interview guide (see Appendix 1), the moderator began each session by engaging participants in open-ended discussions about their anticipated concerns (preoperative groups) as well as adverse events experienced (postoperative groups). Later in the session, the moderator recorded a running list of adverse events identified during each session (Focus Group Identified AEs) and prior to the end of the discussion asked all participants to characterize these AEs as either “very severe,” “moderately to somewhat severe,” or “not severe.” Following this process, women then reviewed a list of AEs that had been previously generated by the authors (Provider Identified AEs) which included urogynecologic surgeons, as a way to further compare/contrast the Focus Group Identified AEs and reflect on the severity categorizations. The moderator then asked each group to add any AEs from the Provider Identified AEs to the focus groups original list that they felt were important and to change their initial severity ranking of AEs if needed. All focus groups were digitally audio recorded, de-identified and transcribed by Rev.com, a transcription service very familiar with qualitative protocols. Women received a $50 gift card at the conclusion of their session.
Members of the core research team (GD, AS, CERC moderator) independently reviewed the full set of transcripts and made observational notes regarding common themes guided by the conceptual framework after each site’s focus groups were completed. During regular core research team meetings, these initial reviews were synthesized and a preliminary coding template was created. This process continued following the completion of the focus groups at each site and the template was continually modified to reflect emergent themes; reorganization of subthemes occurred based on further review of the transcripts. Iterative data collection was performed until data saturation was achieved.
Following the completion of data collection, the coding template was finalized and all transcripts were imported into NVivo10, a qualitative data analysis software program. The primary analyst conducted queries to generate reports on each thematic category and to explore cross-sectional relationships (e.g., long-term postoperative responses in all sites) as well as selected queries to further understand experiences of stigma and/or surgical expectations. Lastly, summary reports were created and reviewed by the core research team members prior to finalizing the interpretive schema.25–27
Process for Developing a conceptual framework
We developed a conceptual framework prior to data collection activities as a way to define major concepts of interest and their relationships. The framework was intended to serve as an initial guide to visualize factors along a pathway that might influence perceptions of adverse events and that would be modified as data analysis concluded. We did not design the interview guides to “test” the concepts included in the framework but rather to facilitate our exploratory goals and remain open to unanticipated factors raised during data collection. Our initial literature review, complemented by expert pelvic surgeon input, indicated that aspects of the patient-provider interaction, patient characteristics and attributes of the patients’ condition should serve as foundational elements of the framework. As illustrated in Figure 1, we then outlined a pathway to identify factors that influence patient experience both prior to and following surgery. The conceptual framework is reviewed periodically throughout the data collection and analytic process and once data interpretation was complete the preliminary framework is revised to best reflect the content and sequence of concepts of our final results.
Results:
A total of 81 women participated in 12 focus groups across four different sites. Groups averaged 6–8 women each. The mean (± standard deviation, SD) age of women was 58.4 ± 12 years in the preoperative group, 60.4 ± 9.9 years in the short-term post-operative group and 60.2 ± 12.3 years in the long-term post-operative group. Greater than 80% of participants were White, and 74% had at least some college education. Women were severely impacted by their pelvic floor disorders as illustrated in Table 1. Results were organized under three major thematic groupings: surgical expectations and understandings, unanticipated AEs in the postoperative period, and personal failure/shame.
Table 1:
Patient characteristics
| Preoperative Group |
Intermediate Postoperative (Up to 12 weeks) |
Long-term Postoperative (1–5 years) |
|
|---|---|---|---|
| Pt Characteristics | Mean ± SD N (%) |
Mean ± SD N (%) |
Mean ± SD N (%) |
| Age (years) | 58.4 ± 12 | 60.4 ± 10 | 60.2 ± 12 |
| BMI (kg/m2) | 30.9 ± 8 | 28.1 ± 7 | 29.8 ± 6 |
| PFDI-20 scores • UDI-6 • POPDI-6 • CRADI-8 • Total |
48.5 ± 23 35.7 ± 14 26.3 ± 23 110.5 ± 38 |
22.5 ± 23 25.7 ± 23 20.7 ± 20 68.9 ± 50 |
16.3 ± 21 15.8 ± 20 16.7 ± 20 48.8 ± 49 |
| LOT-R total scores | 16.0 ± 7 | 18.9 ± 3 | 19.2 ± 4 |
| PGI-I | - | 2.5 ± 2 | 2.0 ± 1 |
| SDS-PFD total score | - | 1.2 ± 0.3 | 1.4 ± 1 |
| DRS-PFD total score | - | 1.3 ± 0.4 | 1.4 ± 1 |
| Caucasian | 21 (84) | 27 (96) | 23 (82) |
| Some college or beyond | 18 (72) | 21 (75) | 21 (75) |
Surgical Expectations and Understandings
Women in the preoperative and postoperative groups shared similar perspectives regarding surgical expectations. They anticipated that surgery would reduce the severity/frequency of symptoms and lead to functional improvements and quality of life. Many expressed reaching a “tipping point” in terms of the impact of symptom frequency and interference with daily, leisure, sexual and employment activities that influenced the decision to undergo surgery. Women, especially those in the preoperative group, described these varied experiences,
“Pads all the time that cause—I have sensitive skin so it causes rashes all the time, the constant changing of them out, every little cough, sneeze, bend, no matter what I do, it’s out. It drips, it leaks, it just pours.”
“Cathing becomes a problem when you’re out in public. It’s hard to go in a stall and try to cath.”
“I have nine grandkids and just keeping up with them, the pads and everything, it’s hard.”
“Not realizing that you’re peeing, that would be embarrassing or having sex with my husband and you’re in a position and you start leaking everywhere.”
Anesthesia complications, such as memory loss, a general sense of loss of control, and vulnerability with surgery were also frequently mentioned by the preoperative group. Concerns were voiced about the recovery period included fear of gaining weight, not being able to work, and healing emotionally.
We also identified a pervasive view of misaligned expectations among both short and long term postoperative focus group participants. Women expressed that they anticipated, “getting back to normal” and resuming tasks of daily living in the time period specified by their surgeon. In situations where either the immediate post-surgical recovery process deviated from the usual course or the surgery was not successful in alleviating symptoms, participants felt unprepared. As women in these groups reflected on their experiences following surgery, they expressed varying degrees of disappointment and regret regarding their current status as well as a desire to have more “honest” communication with their surgeons in terms of realistic expectations, This was observed in both short and long term postoperative groups.
“I have to wear big old granny panties and three maxi-pads, two to three maxi-pads. That sucks.” I have pain as well in my rectum. It feels like it gets pinched or something, so if I do a lot of physical exercise or I’m standing a lot, when I go to sit down it is excruciating. That was why I chose the surgery… What else? I would just say that overall the way that my nethers came back together, it’s just different. It just wasn’t what I had expected. I feel like … I needed … that conversation like, ‘No, honey. It is not like your level 4 episiotomy at all.’ You know, like honesty. Hardcore, we’re not going to like this conversation honesty, because it’s my body and I have to walk with it until I die.”
“I wasn’t expecting—how do I say it in a nice way—t he sex part of it. I wasn’t expecting that. Yeah, because me and the mister, we had a really healthy relationship and everything was good. Then right after I had the procedure, after I had the operation, after the healing process went and stuff, he was the one that was, like, ‘There’s something weird in there.’ Now it’s kind of like I would say obsolete. That part I wasn’t expecting. If I were to do it all over again, I would probably ask would it affect or how bad it would affect it, and maybe had just done the hysterectomy without the mesh with it.”
We also asked all focus group participants to talk in general about their planned (or previous) urogynecological surgical procedures and describe their level of understanding. They commonly reported a general lack of knowledge about their specific surgery and expressed interest in having surgeons provide more information, particularly regarding functional outcomes,
“I feel like it was on me to ask more questions. I should have just asked more. Instead, I just blindly trusted.”
“They (the doctors) didn’t really explain a lot of things to me and my surgery is coming up. I’m hoping that before then they will sit down and tell me more of what’s going on. I would like to know how this is going to affect my job.”
Lastly, when all participants were asked about their concerns prior to having the surgery, women identified a range of fears pertaining to clinical complications such as infection, pain, needing a catheter and problems associated with anesthesia. However, women most notably identified their primary concern as not fixing the underlying problem,
Moderator: “If a friend asked you what you were most worried about having surgery for your pelvic floor condition, what would you say?”
Participant: “That I went through with it and it didn’t work.”
Unanticipated AEs in the Post-Operative period
As depicted in Table 2, and consistent with a major theme across all participant groups, AEs that diminished function and quality of life were consistently categorized as equivalent to AEs that surgeons typically rank as “very severe., during the focus group discussion. Women ranked AEs such as death, Intensive Care Unit (ICU) admissions and other major complications as severe but also consistently endorsed functional AEs such incontinence, constipation, nocturia and lack of improvement in sexual function as “very severe.” For example, one woman described complications from incontinence as follows,
Table 2:
Focus Group Ranking of AEs
| Preoperative Group Ranking of AEs | |||
|---|---|---|---|
| Very Severe | Moderately to Somewhat Severe |
Not Severe | |
| N = 26 | • Infection • Surgery failure* • Death • Recovery: Lack of mobility* • Multiple surgeries* • Causing more problems* • Nicking something • Anesthesia Related |
• Catheter: unable to void • Pain • Sexual function • Unwelcome surprises: discovering another disease • Recovery time • Blood clots |
• Mesh related complications • Financial |
| AEs Added After Physician Generated AE List Reviewed | |||
| • Everything on list • Sepsis |
• Inability to jump/exercise |
• No additions | |
| Immediate Post-Operative Group Ranking of AEs | |||
| Very Severe |
Moderately to Somewhat Severe |
Not Severe | |
| N = 27 | • Incontinence* • Infection • Death • Pain at surgical site • Blood loss/blood transfusion • Constipation* • Nicked bladder • Anesthesia during surgery • Recurrence of problem* • Mesh complication • Scar tissue at surgical site causing pain • Sexual function* • Dehydration during/after surgery |
• Pain • Financial recovery • Numbness in limbs • Unpleasant smell • Limited mobility • Stitches • Sexual function • Weight gain • Double voiding |
• Blood clots • Weight loss |
| AEs Added After Physician Generated AE List Reviewed | |||
| • Up more than 2 times per night to urinate* • Mesh pain |
• No additions | • Spraying of urine • Painful intercourse |
|
| Long Term Post-Operative Group Ranking of AEs | |||
| Very Severe |
Moderately to Somewhat Severe |
Not Severe | |
| N = 28 | • Sexual Function* • Repeat Surgery* • Surgery failure* • Chronic pain • Death • Lifelong treatment*: Stool softener, Catheterization • Continue incontinence* • Pulmonary edema • MI/CHF • Mesh complication • Anal incontinence* • Burn after surgery • Catheter • Recovery time* • ICU admission • Stiches too tight • Constipation* |
• UTI • Pain • Recovery with limited mobility • Neurologic injury |
• Bleeding during surgery • Blood clots • Mesh complications |
| AEs Added After Physician Generated AE List Reviewed | |||
| • No additions | • No additions | • No additions | |
These adverse events marked to signify those that are further discussed in the Results section and represent a significant departure from adverse events that would be typically considered as “very severe” by surgeons
I think incontinence covers the whole situation because you can’t travel. You can’t have a job where you’re running constantly to a bathroom. Your quality of life is just not good.
The focus of concerns varied across the patient populations. In the preoperative groups, women ranked issues such as “surgery failure,” “need for multiple surgeries,” and “causing more [functional] problems” as “very s evere” adverse events. At this stage, the women were thinking less about specific symptoms and more about whether they would experience favorable surgical outcomes. Another “very severe” adverse event identified by these women was related to fears about “recovery—lack of mobility” as many women were fearful that the surgery would not improve ease of movement with regard to work, household and child care responsibilities.
In the short-term postoperative population, women were still actively recovering and cited symptoms such as incontinence, constipation, nocturia as “very severe.” In the long term postoperative groups, women continued to identify these types of adverse events as “very severe”; in addition to this list they included outcomes that paralleled women’s growing concerns that anticipated improvements in their underlying condition would not be realized. For example, participants indicated that “lifelong treatment,” which may include the use of daily stool softeners and the need for self-catheterization, constitute very severe adverse events.
Personal Failure and Shame
Lastly, perspectives were elicited about how the women viewed AEs such as a lack of reduction in symptoms or recurrent prolapse. Women commonly expressed a sense of personal failure and shame in these situations. In many cases, women were unaware that such outcomes were possible, they assumed responsibility. Women indicated that prior to the surgery, they would routinely hide their daily struggles from family members and friends but noted that it was “devastating” to undergo surgery and have the problem return,
“I would say that for all of the investment, financial, emotional, physical, the problems that I was dealing with were uncomfortable but they were my own. Once I had the surgery then other people were now involved. My children were put out for several months while mom was recovering, a lot of pressure was added to my husband while I recovered. To have it fail, it’s going to make me cry, it feels like a failure to more than myself.”
Women also expressed an implicit obligation to their family and social networks that provided care for them during the recovery period. Recognizing their inability to maintain an active role in terms of work and/or daily supportive activities in the family setting, women felt like a suboptimal surgical outcome was somehow a “let down” and this led to feelings of shame in terms of feelings relating to loss of respect and esteem pertaining to one’s circumstances.
“Right, because as we’ve experienced when it fails, it doesn’t just feel like a failure of the surgery. It feels personal, and then I felt the responsibility of letting everyone that helped me for six months, I let you down. I failed.”
Across the three populations, women in our study had high expectations for the outcome of their surgery; they wanted their problem fixed and the surgery to be effective. They reported that they wanted to more easily engage in routine daily activities including leisure, work, childcare, and have improved sexual function; if preoperative expectations were not met, women felt that their suboptimal outcome was a serious AE. For example, if women expected sexual function to improve following surgery and it did not, they felt that this was a serious AE.
Results of the conceptual framework refer to Fig 1 and 2.
Figure 2:
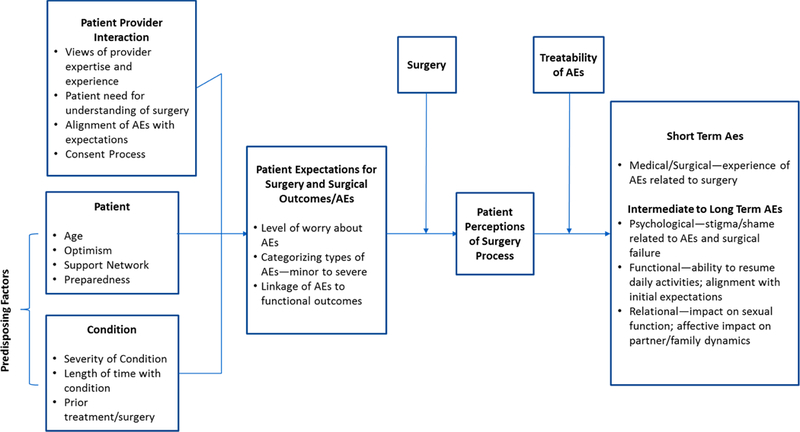
Revised Patient Conceptual Framework
The revised conceptual framework is the culmination of final data interpretation.
Given these findings, our preliminary conceptual framework was revised (Figure 2). The main revisions were to the patient/provider interaction, patient expectations for surgery, and short and long term AEs. Of particular clinical relevance is AE ranking and the importance to women of adverse function outcomes. From the patient perspective, short term AEs focused on the medical/surgical arena and the patient experience of more traditional AEs related to surgery. For intermediate to long term AEs we added the following to our conceptual framework:
Psychological—stigma/shame related to AEs and surgical failure
Functional—ability to resume daily activities; alignment with initial expectations
Relational—impact on sexual function; affective impact on partner/family dynamics
Comment:
In this qualitative study we found that women consider adverse functional outcomes to be severe AEs, that there are misalignments between patient and traditional views of AEs and that women internalize negative surgical outcomes as reflective of personal failure. Interestingly, we found that in the preoperative period women were concerned about AEs such as pain, catheter issues, and bleeding. In the postoperative period, AEs identified by women evolved into concerns related to function. If their preoperative expectations were not met, women felt that their suboptimal outcome was a serious AE. For example, if a woman expected sexual function to improve following surgery, and it did not, this was considered a serious AE. It is interesting to note that the preoperative group did not view mesh complications as serious AEs. This may be because the majority of the preoperative group had already undergone preoperative counseling with their surgeons prior to the focus group.
Postoperatively, AEs identified by women were not aligned with traditional AEs and focused on function including constipation, fatigue, pain, need for a catheter and infection issues. Women do not perceive PFDs as chronic conditions; likely because providers do a poor job explaining them as such. This misconception creates an environment in which a woman will view both the surgery and herself as a failure if some symptoms continue.
Limitations of this study include those inherent with a qualitative design, including that the findings in this work are descriptive and hypothesis generating, and no hypotheses were tested. It is possible that bias could have been introduced as the participants completed the questionnaires prior to the focus group, however, this is unlikely as many of the questionnaires utilized are routinely administered in Urogynecologic clinics before and after surgery and should not have skewed the subsequent interaction. In addition, despite efforts to reruit ethno-racially diverse patients, the majority of participants were non-Hispanic White and college educated. Further, focus groups were conducted with women undergoing or who had undergone different procedures for a variety of pelvic floor disorders, and our findings may not be generalizable to individuals undergoing other types of surgery. Strengths include a multi-center study with a geographically diverse group of patients following rigorous qualitative methods. Generation of a conceptual framework and interview guide was performed with the guidance of experts in qualitative work and with the same experienced moderator (CERC) conducting all focus groups.
Our results indicate that traditional AE collection does not include adverse outcomes important to women, and that women blame themselves for surgical failures. Functional AEs that are collected routinely following surgery, such as constipation, and have traditionally been thought to be minor, are classified by women as moderate to severe. This is likely related to outcome expectations; patients view the restoration of function status as paramount and therefore if it is not achieved patients perceive this as an AE. Altering the perception of PFDs to a condition similar to a chronic disease may help with the misalignment of expectations and outcomes women currently experience. This work will help clarify and lead to a better understanding of how patients and providers think about and perceive AEs. Inclusion of these functional AEs in surgical counseling may help to better align patient and provider expectations and may lead to improved satisfaction with outcomes.
Supplementary Material
IMPLICATIONS AND CONTRIBUTIONS:
- Why was this study conducted?
- • Little is known on how patients perceive adverse events. Although there are scales created to rate surgical adverse events; most were created without patient input.
- What are the key findings?
- • Although patients recognize bleeding or hospital readmission as adverse events, women also consider poor functional outcomes, such as recurrent symptoms or sexual dysfunction as adverse events.
- What does this study add to what is already known?
- • Patients think about adverse events differently than surgeons. Patients view lack of functional improvement as adverse events.
- • Appropriate expectation settings regarding surgery for pelvic floor dysfunction along with inclusion of these functional AEs in surgical counseling may help to better align patient and provider expectations and may lead to improved satisfaction with outcomes.
ACKOWLEDGMENTS:
The authors would like to thank the CERC moderator Venita Wolfe, the Coordinators, and all those who made this work possible, including:
DISCLOSURES: Gena C Dunivan, MD received research funding from Pelvalon. J. Eric Jelovsek, MD MMEd: royalties UpToDate. Christopher J. Chermansky, MD receives research funding from Allergen. Rebecca G Rogers, MD was DSMB chair for the TRANSFORM trial sponsored by American Medical Systems and receives royalties from UptoDate. All other authors report no disclosures.
FUNDING: Eunice Kennedy Shriver National Institute of Child Health and Human Development; (U10 HD041261, U10 HD069013, U10 HD054214, U10 HD054215, U10 HD041267, U10 HD069025, U10 HD069010, U10 HD069006, U01 HD069031) National Institute of Health Office of Research on Women’s Health. University of New Mexico Clinical and Translational Science Center; (UL1TR001449)
PRESENTATION INFORMATION: Oral Poster presentation at the American Urogynecologic Society 38th Annual Scientific Meeting in Providence, RI. October 3–7th, 2017
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Gena C. DUNIVAN, Division of Urogynecology, Department of OBGYN, University of New Mexico, Albuquerque, NM
Andrew L. SUSSMAN, Department of Family and Community Medicine, University of New Mexico, Albuquerque, NM.
J. Eric JELOVSEK, Department of OBGYN, Duke University, Durham, NC.
Vivian SUNG, Department of OBGYN, Brown University Providence, RI.
Uduak U. ANDY, Department of OBGYN, University of Pennsylvania.
Alicia BALLARD, Department of OBGYN, University of Alabama, Birmingham, AL.
Sharon JAKUS-WALDMAN, Department of OBGYN, Bellflower Medical Center, Bellflower, CA.
Cindy L. AMUNDSEN, Department of OBGYN, Duke University, Durham, NC.
Christopher J. CHERMANSKY, Division of Urology, University of Pittsburgh, Pittsburgh, PA.
Carla M. BANN, Division of Statistical and Data Sciences, RTI International, Research Triangle Park, NC.
Donna MAZLOOMDOOST, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health, Bethesda, MD.
Rebecca G ROGERS, Dell Medical School, Department of Women’ Health, University of Texas at Austin, Austin, TX.
References:
- 1.Brubaker L, Cundiff G, Fine P, et al. Abdominal Sacrocolpopexy with Burch Colposuspension to Reduce Urinary Stress Incontinence. N Engl J Med 2006: 354:1557–1566. [DOI] [PubMed] [Google Scholar]
- 2.Visco AG, Brubaker L, Richter HE, et al. Anticholinergic Therapy versus OnabotulinumtoxinA for Urgency Urinary Incontinence. N Engl J Med 2012; 367:1803–1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wei JT, Nygaard I, Richter HE, et al. A Midurethral Sling to Reduce Incontinence after Vaginal Prolapse Repair. N Engl J Med 2012; 366:2358–2367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barber MD, Brubaker L, Menefee S, et al. Sacrospinous Ligament Suspension versus Uterosacral Ligament Suspension for Pelvic Organ Prolapse: A Randomized Trial. JAMA [in press] [DOI] [PMC free article] [PubMed]
- 5.U.S. Food and Drug Administration. http://www.fda.gov/safety/medwatch/howtoreport/ucm053087.htm Accessed September 14, 2013.
- 6. http://www.umass.edu/research/irb-guidelines-adverse-events.
- 7. http://hsc.unm.edu/som/research/hrrc/docs/ru/RU_S1_HRPO_Fundamentals.pdf.
- 8.Dindo D, Demartines N, Clavien P. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240(2):205–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clavien P, Barkun J, de Oliveira M, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009;250(2):187–196 [DOI] [PubMed] [Google Scholar]
- 10.Gutman RE, Nygaard IE, Ye W, et al. The Pelvic Floor Complication Scale: a new instrument for reconstructive pelvic surgery. Am J Obstet Gynecol 2013;208:81.e1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Srikrishna S, Robinson D, Cardozo L, Cartwright R. Experiences and expectations of women with urogenital prolapse: a quantitative and qualitative exploration. BJOG 2008;115(11):1362–8 [DOI] [PubMed] [Google Scholar]
- 12.Lawndy SS, Withagen MI, Kluivers KB, Vierhout ME. Between hope and fear: patient’s expectations prior to pelvic organ prolapse surgery. Int Urogynecol J 2011;22(9):1159–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mamik MM, Rogers RG, Qualls CR, Komesu YM. Goal attainment after treatment in patients with symptomatic pelvic organ prolapse. Am J Obstet Gynecol 2013;June 13 [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 14.Elkadry EA, Kenton KS, FitzGerald MP, Shott S, Brubaker L. Patient-selected goals: A new perspective on surgical outcomes. Am J Obstet Gynecol 2003; 189(6):1551–1557 15574. [DOI] [PubMed] [Google Scholar]
- 15.Schmidt M, Jacobs K, Ramm O, Kenton K. The way they see it: patients’ perspective of perioperative events. Female Pelvic Med Reconstr Surg 2013;19(2) Mar-Apr 2013 ABSTRACT [Google Scholar]
- 16.Schmidt M, Ramm O, Kenton K The way we see it: surgeons’ perceptions of perioperative events. J Gyn Surg 2012;28(4):270–27417. [Google Scholar]
- 17.Jabareen Y; Building a conceptual framework: philosophy, definitions and procedure. International Journal of qualitative Methods 2009; 8(4):49–62 [Google Scholar]
- 18.Sung Vivian W.; Rogers Rebecca G.; Bann Carla M.; More. Symptom Outcomes Important to Women With Anal Incontinence: A Conceptual Framework. Obstetrics & Gynecology 123(5):1023–1030, May 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baskayne K, Willars J, Pitchforth E, Tincello D. Women’s expectations of prolapse surgery: a retrospective qualitative study. Neurourol Urodynam 2014;33:85–89. [DOI] [PubMed] [Google Scholar]
- 20.Guest G, Bunce A, & Johnson L (2006). How many interviews are enough? An experiment with data saturation and variability. Field Methods, 18(1), 59–82. doi: 10.1177/1525822X05279903 [DOI] [Google Scholar]
- 21.Barber MD, Kuchibhatla MN, Pieper CF, Bump RC. Psychometric evaluation of 2 comprehensive condition-specific quality of life instruments for women with pelvic floor disorders. Am J Obstet Gynecol 2001. December;185(6):1388–95. [DOI] [PubMed] [Google Scholar]
- 22.Wren P, Janz N, FitzGerald M, et al. Optimism in women undergoing abdominal sacrocolpopexy for pelvic organ prolapse. J Am Coll Surg 2008;207:240–245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Srikrishna S, Robinson D, Cardozo L. Validation of the patient global impression of improvement (PGI-I) for urogenital prolapse. Int Urogynecol J May;21(5):523–8. [DOI] [PubMed] [Google Scholar]
- 24.Sung V, Kauffman N, Raker C, et al. Validation of decision-making outcomes for female pelvic floor disorders. Am J Obstet Gynecol 2008;198:575.e1–575.e6. [DOI] [PubMed] [Google Scholar]
- 25.Corbin J, Strauss A. Basics of qualitative research: techniques and procedures for developing grounded theory Thousand Oaks, CA: Sage Publications, 2008 [Google Scholar]
- 26.Krueger R Focus groups: A practical guide for applied research (4th edition). Thousand Oaks, CA: Sage Publications, 2008 [Google Scholar]
- 27.Morse JM, Barrett M, Mayan M, et al. Verification strategies for establishing reliability and validity in qualitative research. International Journal of Qualitative Methods 2002;1:1–19. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


