Abstract
A revised diagnostic algorithm provides guidelines for the diagnosis of patients with suspected pulmonary hypertension, both prior to and following referral to expert centres, and includes recommendations for expedited referral of high-risk or complicated patients and patients with confounding comorbidities. New recommendations for screening high-risk groups are given, and current diagnostic tools and emerging diagnostic technologies are reviewed.
Short abstract
State of the art and research perspectives in the diagnostic procedures of patients with pulmonary hypertension including a comprehensive diagnostic algorithm http://ow.ly/Ow9730mknM6
Introduction
There has been no meaningful decrease in the time from symptom onset to diagnosis of pulmonary hypertension (PH) in the past 20 years. Therefore, the diagnostic algorithm and guidelines for screening at-risk groups have been modified, balancing the benefits of earlier diagnosis and disease recognition against the economic healthcare burden of additional screening and increased referrals to PH centres.
Diagnostic approach in patients with clinical suspicion for PH/pulmonary arterial hypertension
PH due to parenchymal, cardiac, thromboembolic and other diseases (diagnostic groups 2, 3, 4 and 5, respectively) is associated with worse outcomes and limited treatment options, resulting in referral of these patients to PH centres. Guidelines for the diagnosis and management for these subgroups are addressed separately by the relevant 6th World Symposium on Pulmonary Hypertension (WSPH) Task Force articles in this issue of the European Respiratory Journal [1–3].
Clinical suspicion of PH
Symptoms
Symptoms of PH are non-specific: exertional dyspnoea, fatigue, weakness, chest pain, light-headedness/syncope and, less frequently, cough. Progressive right-sided heart failure (oedema, ascites, abdominal distension) occurs in later or more accelerated disease. Rarely, haemoptysis, Ortner's syndrome/hoarseness (unilateral vocal chord paralysis) and arrhythmias may characterise PH.
Physical findings
Physical findings include augmented second heart sound (P2 component), right ventricular lift, jugular venous distension, hepatojugular reflux, ascites, hepatomegaly and/or splenomegaly, oedema, tricuspid regurgitant or pulmonary regurgitant murmurs, and S3 gallop.
Diseases associated with PH can be suggested by history and physical exam.
Established diagnostic tools
Electrocardiography
Since the US National Institutes of Health (NIH) registry report on primary PH in 1987 [4], the ECG has been considered a reliable clue to the presence of PH. ECG features in patients with pulmonary arterial hypertension (PAH) have been demonstrated to be associated with worse prognosis [5, 6]. The derivative populations for these conclusions were patients with known PAH, predominantly World Health Organization Functional Class III and IV. The utility of the ECG as a screening tool in complicated patients or those early in the course of their disease is uncertain. A normal ECG does not exclude PH.
Blood tests and immunology
Blood tests are not useful for PH diagnosis, but distinguish some forms of PH and indicate end-organ compromise. Routine biochemistry, haematology and thyroid function tests are required in all patients. Liver function abnormalities may represent congestion, primary liver disease and/or consequences of therapy. Thyroid disease is common in PAH, may develop during the disease and should be considered in cases of abrupt deterioration. Elevations of brain natriuretic peptide (BNP) and N-terminal pro-BNP (NT-proBNP) are associated with right ventricular overload, and are predictors of worse outcome.
Routine screening for connective tissue disease (CTD), hepatitis and HIV is required. Elevated antinuclear antibodies (ANAs) occur frequently, although in low titres (1:80). Recommended serological testing for scleroderma includes ANAs (as ELISA can be associated with false-negative tests, ANA immunofluorescence is recommended and should be considered positive at ≥1:160). If there is a high index of suspicion, consider a panel that consists of anticentromere, antitopoisomerase, anti-RNA polymerase III, double-stranded DNA, anti-Ro, anti-La and U1-RNP antibodies.
Patients with CTD (associated with thombophilic states) and chronic thromboembolic PH (CTEPH) should undergo screening for coagulopathies and thrombophilia, including anticardiolipin antibodies, lupus anticoagulant and anti-β2-glycoprotein antibodies.
Pulmonary function tests and arterial blood gases
Pulmonary function tests are addressed in the PH lung disease Task Force article in this issue of the European Respiratory Journal [2], and should include total lung capacity and diffusing capacity of the lung for carbon monoxide (DLCO). In most patients with PAH there is a mild restrictive component. Marked reduction in DLCO (<60% of predicted) or severe exertional hypoxaemia can indicate pulmonary veno-occlusive disease/pulmonary capillary haemangiomatosis [7].
Cardiopulmonary exercise testing
Cardiopulmonary exercise testing (CPET) for diagnostic purposes can be done non-invasively or with haemodynamic testing [8]. CPET can quantify the degree of relative hypoperfusion of the lung and the systemic circulation that occurs during exercise in patients with PH [9], and can grade the severity of exercise limitation and assess responses to therapy [10].
Abnormalities in effort-independent ratio of minute ventilation to carbon dioxide production (V̇E/V̇CO2) and end-tidal carbon dioxide tension (PETCO2) obtained during CPET have been used to estimate the likelihood of PH (lower peak oxygen uptake (V̇O2) and/or higher V̇E/V̇CO2 signifying an increasing likelihood of pulmonary vascular disease) [11]. Several investigators have demonstrated the utility of CPET in defining abnormal exercise responses specific to PAH [12–15]. CPET can be particularly useful in helping identify the predominant underlying cardiopulmonary pathophysiology [13, 16–19]. A detailed description of the methodologies used in CPET for PH can be found in Sun et al. [9]. Submaximal exercise testing to evaluate PAH severity using a simplified gas exchange system has also been proposed [20].
Accurate utilisation of CPET requires performance by a competent facility and interpretation by a clinician with expertise in gas exchange in conjunction with the patient's history, physical and laboratory findings. CPET is useful for determining the nature of the exercise limitation in patients with unexplained dyspnoea, but should not be used as the sole screening tool for asymptomatic subjects at risk for developing PAH; CPET can help evaluate cardiopulmonary limitations and assess pulmonary vascular involvement in these patients; emerging evidence suggests that CPET may be useful for evaluating symptomatic patients at high risk for developing PAH [15]. In addition, CPET should be considered after diagnosis of PAH to quantify the severity of exercise impairment and to estimate prognosis.
Transthoracic echocardiography
The transthoracic echocardiogram (TTE) remains the most important non-invasive screening tool and right heart catheterisation (RHC) remains mandatory to establish the diagnosis.
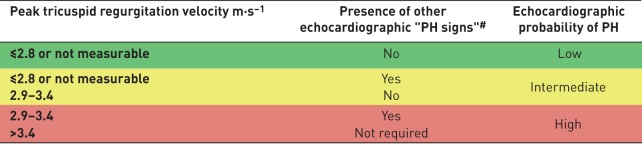
The echocardiographic probability of PH was derived from previously published data in normal adults [21–23], and consolidated by expert opinion using the combination of tricuspid regurgitant velocity, right ventricular size, interventricular septal function, inferior vena cava diameter fluctuations with respiratory cycle, systolic right atrial area, pattern of systolic flow velocity and early diastolic pulmonary regurgitant velocity, and diameter of the pulmonary artery (tables 1 and 2) [24–27].
TABLE 1.
Echocardiographic probability of pulmonary hypertension (PH) in symptomatic patients with a suspicion of PH
#: see table 2. Reproduced and modified from [24] with permission.
TABLE 2.
Echocardiographic signs suggesting pulmonary hypertension (PH) used to assess the probability of PH in addition to tricuspid regurgitation velocity measurement in table 1
| A: The ventricles | B: Pulmonary artery | C: Inferior vena cava and right atrium |
| Right ventricle/left ventricle basal diameter ratio >1.0 | Right ventricular outflow Doppler acceleration time <105 ms and/or mid-systolic notching | Inferior cava diameter >21 mm with decreased inspiratory collapse (<50% with a sniff or <20% with quiet inspiration) |
| Flattening of the interventricular septum (left ventricular eccentricity index >1.1 in systole and/or diastole) | Early diastolic pulmonary regurgitation velocity >2.2 m·s–1 | Right atrial area (end-systole) >18 cm2 |
| Pulmonary artery diameter >25 mm |
Echocardiographic signs from at least two different categories (A/B/C) from the list should be present to alter the level of echocardiographic probability of PH. Reproduced and modified from [24] with permission.
Ventilation/perfusion lung scanning
Ventilation/perfusion (V/Q) lung scanning is addressed in the CTEPH Task Force article in this issue of the European Respiratory Journal [3]. A normal V/Q scan remains the preferred diagnostic tool and rules out CTEPH. Nuclear medicine societies are recommending a transition of V/Q reporting to a binary interpretation [28, 29].
Chest computed tomography
Chest computed tomography (CT) demonstrating right ventricular dilation, right atrial dilation, enlarged main pulmonary artery (diameter ≥29 mm) or a main pulmonary artery/ascending aorta diameter ratio ≥1 is suggestive of PH [30]. High-resolution non-contrast examination can identify parenchymal lung disease and discriminate between PH lung disease and PAH (group 3 versus group 1).
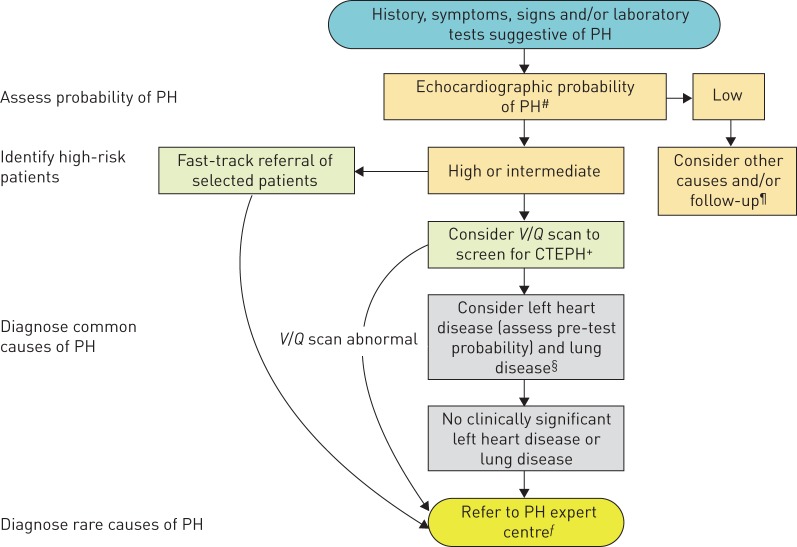
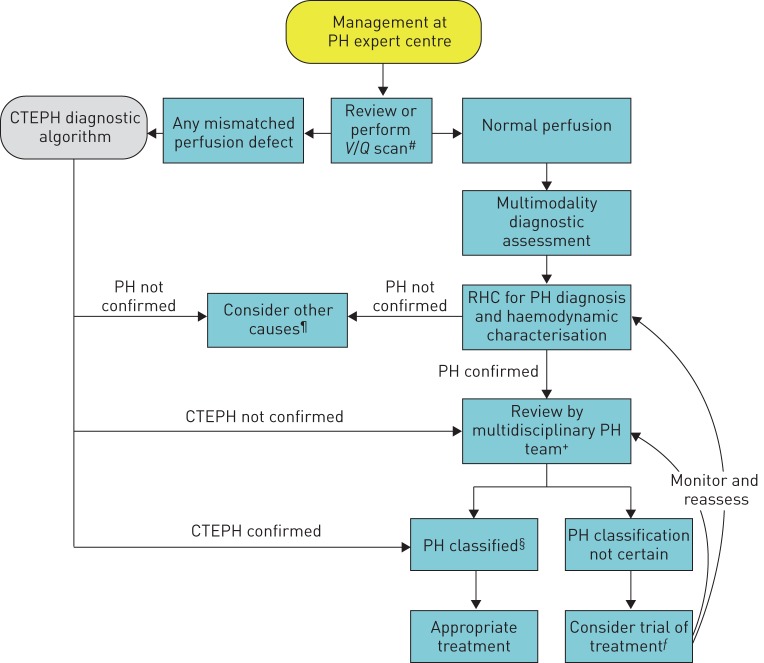
Current state-of-the-art diagnostic algorithm
The modified diagnostic algorithm divides the diagnostic approach into 1) that undertaken outside the PH expert centre, including recommendations for high-risk/accelerated disease requiring expedited triage to the expert centre (figure 1), and 2) that focusing on the diagnosis of PH once referred to a PH expert centre (figure 2).
FIGURE 1.
Algorithm for the diagnosis of pulmonary hypertension (PH) and its causes: triage of urgent cases and diagnosis of common conditions (for more details, see the accompanying text). V/Q: ventilation/perfusion; CTEPH: chronic thromboembolic PH. #: described in the 2015 European Society of Cardiology/European Respiratory Society PH guidelines [24]; ¶: these include chronic thromboembolic disease without PH, which should be considered in patients with risk factors and/or previous venous thromboembolism; +: single photon emission computed tomography or planar V/Q scan is acceptable (interpretation is binary: normal or abnormal); §: see algorithms for left heart disease and lung disease/hypoxia-related PH [1–3], which provide details of further management of these patients; ƒ: referral of a patient to be seen in person or for a teleconsultation.
FIGURE 2.
Algorithm for the diagnosis of pulmonary hypertension (PH) and its causes: role of the PH expert centre. CTEPH: chronic thromboembolic PH; V/Q: ventilation/perfusion; RHC: right heart catheterisation. #: single photon emission computed tomography or planar V/Q scan is acceptable; ¶: these include patients with chronic thromboembolic disease without PH; +: the composition of the multidisciplinary team may differ depending on the type of clinical problem; §: according to clinical classification of PH; ƒ: only in expert centres and only with a reassessment plan in place.
Practice recommendations (including high-risk population screening recommendations)
Patients with congenital heart disease (CHD), CTD, HIV and portopulmonary hypertension (POPH) are at increased risk for PH. As little or no progress has been made in earlier diagnosis, this Task Force recommends more aggressive assessment and screening of some of these high-risk populations.
Scleroderma (systemic sclerosis) and scleroderma spectrum
The 5th WSPH report, the 2015 European Society of Cardiology (ESC)/European Respiratory Society (ERS) PH guidelines and the NIH-supported 2013 CTD-PAH guidelines recommend annual screening in patients with systemic sclerosis (SSc) [24, 31, 32]. All guidelines recommend the DETECT algorithm (evidence-based detection of PAH in SSc) in patients with SSc spectrum disorders (SSc, mixed CTD or other CTDs with prominent scleroderma features (e.g. sclerodactyly, nail fold capillary abnormalities and SSc-specific autoantibodies)) associated with DLCO <60% of predicted and disease duration >3 years. The current diagnosis Task Force undertook a systematic review of the published literature for screening tools available for CTD-PAH [33]. The review supports incorporating TTE, DETECT (with preliminary data on its performance with those with DLCO <80% of predicted) or forced vital capacity (FVC)/DLCO ratio >1.6 and blood markers (such as NT-proBNP) in SSc spectrum disorders. Based on this data and on the published guidelines, this Task Force recommends the incorporation of DETECT, TTE or FVC/DLCO ratio with elevated NT-proBNP to screen for SSc spectrum disorders. Although the prevalence of PAH is lower in those with DLCO ≥80% of predicted, review of two large cohorts in the USA ([33] and Steve Mathai, Johns Hopkins, Baltimore, MD, USA; personal communication) suggested that PAH is present in these patients.
Recommendations
For patients with SSc and SSc spectrum with uncorrected DLCO <80% of predicted, annual screening should be considered. The appropriate screening tools include DETECT, the 2015 ESC/ERS recommendations for TTE or FVC/DLCO ratio >1.6 (assuming none-to-mild interstitial lung disease) and >2-fold upper limit of normal of NT-proBNP. If any of these screening tests are positive, these patients should be referred for RHC. For those with uncorrected DLCO ≥80% of predicted, screening may be considered with TTE.
HIV
Although the incidence of PAH in HIV is low, the large number of HIV-infected individuals worldwide makes HIV a major contributor to the worldwide incidence of PAH and a significant contributor to HIV-related death. Prior guidelines did not recommend PAH screening in HIV-infected patients, a conclusion derived from contemporary RHC-based studies in Europe [34] and the USA [35].
Preliminary data from an ongoing RHC-based study in Atlanta HIV clinics suggests a higher incidence of PH than previously reported in the USA (prevalence 2% in this US-based African-American population) (Marshaleen Henriques-Forsythe, Morehouse School of Medicine, Atlanta, GA, USA and Harrison W. Farber, Pulmonary Center, Boston University School of Medicine, Boston, MA, USA; personal communication). Risks for PAH in HIV include sex and i.v. drug use. Males are more frequently infected with HIV than females, but HIV-infected females are disproportionately diagnosed with PAH (around 2-fold). Intravenous drug use has been associated with HIV-PAH [36] in univariate analysis, although it dropped out in multivariate analysis; however, a biological rationale for this association has been demonstrated [37]. Data suggest that cocaine acts synergistically with the HIV-1 Tat (transactivator of transcription) protein [38] by suppressing bone morphogenetic protein receptor expression on pulmonary artery smooth muscle cells.
Other studies report an association between HIV-PAH and female sex [39], chronic hepatitis C virus infection (multivariate OR 3.01, 95% CI 1.2–8.2; p=0.02 [21, 40]) and origin from high-prevalence country [41].
The following higher-risk features are proposed for PAH screening in HIV to enrich the likelihood of earlier diagnosis of HIV-PAH in asymptomatic patients: female sex, i.v. drug use/cocaine use, hepatitis C virus infection, origin from high-prevalence country, known Nef (negative regulatory factor) or Tat HIV proteins and US African-American patients independent of symptoms.
Recommendations
Screen for PAH in HIV patients with symptoms or with more than one risk factor for HIV-PAH.
Heritable
Recommendations in the USA for PAH genetic screening are largely ignored, misunderstood or unfunded [42]. In contrast, genetic screening and counselling offered by French PH referral centres have identified PAH mutations in 16.9% of presumed sporadic PAH patients, in 89% of patients with a family history [43] and in asymptomatic first-degree relatives of mutation carriers pre-emptively screened. Recent longevity data indicates a lifelong risk of developing disease in 14% of male and 42% of female carriers, prompting our recommendation for annual echocardiography in asymptomatic carriers [44].
Recommendations
Genetic counselling of all idiopathic, anorexiant and familial PAH patients and first-generation asymptomatic family members of patients with known genetic mutations.
Subsequent evaluations for PAH should be offered (e.g. CPET and TTE), in mutation-positive individuals.
National databases for genotyping all PAH patients should be advocated by the WSPH. Biobanking of samples and/or genotyping should be mandated in future interventional studies in PAH patients and possibly in PH patients.
Other heritable PH
Hereditary haemorrhagic telangiectasia
The French hereditary haemorrhagic telangiectasia (HHT) registry [45] demonstrated the echocardiographic prevalence of PH in HHT as 4.23%, although this was usually associated with high-output left heart failure. However, the review indicated that while PAH was rare, it was associated with much poorer survival.
Recommendations
In symptomatic patients and those with heart failure or hepatic arteriovenous malformations, with HHT or family history of HHT, genetic testing and an echocardiogram should be undertaken. If TTE positive (tables 1 and 2) or suggestive of PH, RHC should be undertaken to distinguish the aetiology of PH.
Portopulmonary hypertension
The frequency of PH in patients with liver disease varies with disease severity and duration. By time of liver transplantation 10.3% of patients had RHC-proven mean pulmonary arterial pressure (mPAP) >35 mmHg [46]. A retrospective review of the UK National Registry of all incident treatment-naive patients with POPH suggested a prevalence of 0.85 cases per million population [47]. The prevalence of POPH in the portal hypertensive population has been previously estimated as 2–6%. Estimated median survival time was 3.75 years in this patient population, with 1-, 2-, 3- and 5-year survival of 85%, 73%, 60% and 35%, respectively.
Recommendations
Echocardiographic screening is recommended in all patients with portal hypertension. If a tricuspid regurgitant jet of >3.4 m·s−1 or right atrial or right ventricular enlargement or dysfunction is found, then further evaluation with RHC and referral to PH expert centre is recommended.
Congenital heart disease
In CHD, PAH can be identified in four distinct subgroups of patients: 1) Eisenmenger syndrome, 2) persistent systemic-to-pulmonary shunts, 3) those with small, coincidental defects, and 4) patients who have undergone defect correction. PAH is present by definition in subgroups 1 and 3. Thus, PAH screening in the CHD population should be undertaken in subgroup 2 and, importantly, subgroup 4.
Recommendations
Post-operative PAH screening in subgroup 4 should include clinical and echocardiographic and ECG screening during follow-up visits 3–6 months after correction and then throughout their planned long-term cardiological follow-up. Annual screening should be planned for corrected patients who presented with increased baseline pulmonary vascular resistance or with combinations of other predisposing factors.
Novel diagnostic modalities
Innovative imaging
V/Q single photon emission CT
V/Q single photon emission CT (SPECT) has higher sensitivity compared with planar imaging and outcome studies have confirmed a high negative predictive value in excluding pulmonary embolism [48, 49].
Dual-modality techniques with varying combinations of hybrid SPECT/CT pulmonary imaging can improve the specificity of V/Q SPECT by identifying lung diseases in patients with perfusion abnormalities. The addition of low-dose CT improves the specificity of V/Q SPECT from 88% to 100% while maintaining the same high sensitivity of 97% [50]. V/Q SPECT reduces radiation exposure relative to CT [51–53].
The three-dimensional aspects of V/Q SPECT allow for data objectification and facilitate automated analysis. The perfusion redistribution index as measured by V/Q SPECT showed perceptible reduction in the normal gravity-dependent redistribution of lung perfusion in PAH patients compared with the normal population [54] and hence can be a potential marker of pulmonary vascular disease.
V/Q SPECT and hybrid pulmonary imaging are not universally available.
Dual-energy CT: pulmonary perfusion
Dual-energy CT (DECT) offers visualisation of morphological and perfusion abnormalities in the pulmonary vasculature. Perfusion alterations were less common but more homogeneous in PAH and were mainly in the form of patchy defects [55]. In CTEPH, perfusion alterations were more frequent and heterogeneous with a high level of concordance with V/Q scintigraphy. The utility of DECT in the diagnosis and prognosis of PH, particularly CTEPH, requires further evaluation.
Three-dimensional dynamic contrast-enhanced magnetic resonance: lung perfusion
Dynamic contrast-enhanced magnetic resonance estimates of perfusion are based on quantification of tissue enhancement at serial time-points after injection of gadolinium and the technique has comparable sensitivity to perfusion scintigraphy for diagnosing CTEPH [56, 57]. Although the lack of ionising radiation makes this an attractive alternative, limited availability and higher costs preclude this technique from superseding V/Q scintigraphy.
Functional magnetic resonance imaging: ventilation
The ready availability and ease of inhaled oxygen as a contrast medium makes pulmonary magnetic resonance imaging (MRI) a promising tool for assessing ventilation. In a small study, oxygen-enhanced ventilation and contrast-enhanced perfusion MRI was concordant with scintigraphy [58]. Standardisation of analyses and reproducibility of oxygen-enhanced MRI metrics is needed before routine use in clinical practice.
Subclinical right ventricular dysfunction
Parametric mapping
A review of the magnetic resonance literature found 21 magnetic resonance metrics indicative of PH [59]. Of these, the ventricular mass index (VMI) was frequently used to assess right ventricular functional and structural changes compared with RHC. A meta-analysis of VMI revealed a positive likelihood ratio of 4.894, indicating a modest ability to differentiate PH patients from healthy controls.
Late gadolinium enhancement (LGE) at the right ventricular insertion points in PH due to delayed clearance of gadolinium correlates inversely with right ventricular performance [60]; however, its utility has been called into question in recent studies as a prognostic indicator in PH [61].
T1 mapping is a non-invasive technique for extracellular volume (ECV) quantification and facilitates early detection of myocardial involvement that is not detectable by LGE. PH has been shown in a small study to be independently associated with increased right ventricular ECV even after adjustment for right ventricular dilatation and dysfunction [62].
Larger studies are required to determine if right ventricular ECV reliably predicts adverse clinical outcomes, offering the potential for risk stratification, prognostication and therapeutic efficacy assessment.
Right ventricular strain
Cardiac magnetic resonance-based right ventricular strain imaging evaluates regional myocardial function by measuring the percentage change in myocardial deformation. Cardiac magnetic resonance feature tracking has shown a significant reduction in right ventricular strain in PH patients with normal right ventricular ejection fraction, predicting subsequent clinical deterioration [63]. Magnetic resonance strain indices are similar to echocardiographic indices, but longitudinal and circumferential strain measurements are more reliable.
Pulmonary artery four-dimensional flow imaging
Time-resolved three-dimensional phase-contrast MRI, also known as four-dimensional flow magnetic resonance, visualises and quantifies cardiovascular blood flow. The pulmonary artery flow patterns can be a non-invasive early marker in those at risk for developing PH.
Main pulmonary artery flow vortices are a marker of elevated mPAP. Vortical blood flow in the main pulmonary artery >14.3% of the cardiac interval corresponds to PH with 97% sensitivity and 96% specificity [64]. The duration of the vortical flow shows a linear increase with mPAP and can be used to estimate PAPs [65]. Early onset of retrograde flow in the dorsal aspect of the main pulmonary artery is another characteristic of PAH [66].
Wall shear stress is reduced in the proximal pulmonary arteries of PAH patients, and may contribute to pulmonary endothelial cell dysfunction and PAH progression [67]. Wall shear stress can be characterised by four-dimensional flow magnetic resonance with the ability to discriminate PAH patients from normal controls [68–70].
These metrics are not available from routine RHC and therefore have potential for non-invasive PH screening and monitoring. Data extraction is complex and clinical trials are necessary to explore the benefits of four-dimensional flow magnetic resonance over standard practices.
Intravascular ultrasound and optical coherence tomography in PAH
Intravascular ultrasound and optical coherence tomography (OCT) can demonstrate intimal fibrosis, a surrogate marker of pulmonary arterial remodelling that correlates negatively with pulmonary arterial compliance and is associated with unfavourable clinical outcomes during mid-term follow-up [71]. OCT has shown development of pulmonary arterial remodelling in patients with borderline PH and the occurrence of reverse remodelling following effective treatment [72].
Machine learning
Technological advances in cardiac imaging coupled with exceptional computing power and innovative analytical modelling offer an unprecedented amount of data that can contribute to the search for novel imaging biomarkers.
A recently published machine learning-based survival model had incremental prognostic power when compared with conventional parameters to more accurately predict outcomes in PH [73]. Such computational simulations can illuminate pathophysiological mechanisms of right ventricular failure, risk stratify different PH groups and identify imaging end-points following therapeutic interventions.
Future biomarkers
Numerous potential biomarkers (e.g. asymmetric dimethylarginine, cystatin C, volatile exhaled gases, exhaled nitric oxide (NO) fraction (FENO) and NOx derivates) [74] have been associated with endothelial cell dysfunction, inflammation, epigenetics, cardiac function, oxidative stress, metabolism, extracellular matrix and exhaled breath condensate [75, 76]; while novel, these have not yet demonstrated sensitivity and specificity for diagnosis, risk assessment or management of PH.
The future of laboratory biomarkers may hinge on the ability to use “deep phenotyping”, i.e. characteristic patterns in the genome, transcriptome, proteome and/or metabolome of the patient [77–81]. Currently metabolomics emerges as a potentially informative area of systems biology. In the future, a metabolomics fingerprint may inform treatment decisions, while changes may be considered “deep monitoring” of treatment results. Currently, however, abnormal responses versus normal responses to abnormal stimuli are indistinguishable and metabolic signatures have only been evaluated in well-defined, homogenous study populations. New research paradigms are necessary to prove their value for early detection and differential diagnosis of PAH in real life.
Footnotes
Number 5 in the series “Proceedings of the 6th World Symposium on Pulmonary Hypertension” Edited by N. Galiè, V.V. McLaughlin, L.J. Rubin and G. Simonneau
Conflict of interest: A. Frost reports personal fees and non-financial support (travel and lodging for attendance and participation in the 6th WSPH) from Actelion, Gilead, United Therapeutics and Bayer, honoraria for presentations from Gilead, and honoraria for participation in an end-point adjudication committee for an FDA-approved study from United Therapeutics, during the conduct of the study; and personal fees (honoraria and travel and lodging for presentations at meetings) from Actelion Pharmaceuticals, outside the submitted work.
Conflict of interest: D. Badesch reports grants and personal fees (as steering committee member and site investigator) from Acceleron, Complexa, Bellerophon and Liquidia, grants, personal fees and advisory board work from Actelion, is a long-term stock holder of Johnson and Johnson, grants and personal fees (as advisory board member and site investigator) from Arena, Gilead and United Therapeutics/Lung LLC, personal fees for consultancy from Respira, grants and personal fees (as site investigator, advisory board member and consultant) from Bayer, outside the submitted work.
Conflict of interest: J.S.R. Gibbs reports grants and personal fees from Actelion, GSK, MSD and Pfizer, personal fees from Arena, Bayer, Bellerophon, Complexa and Acceleron, and grants from United Therapeutics, during the conduct of the study.
Conflict of interest: D. Gopalan has nothing to disclose.
Conflict of interest: D. Khanna reports personal fees from Actelion, Bayer, Boehringer Ingelheim, Chemomab, Corbus, Covis, Cytori, EMD Sereno, Genentech/Roche, Gilead, GSK, Sanofi-Aventis and UCB Pharma; grants from Bayer, Boehringer Ingelheim, Genentech/Roche, Pfizer and Sanofi-Aventis; and has stock options with Eicos Sciences, Inc. He was also supported by the NIH/NIAMS (K24 AR063120).
Conflict of interest: A. Manes reports grants and personal fees from Actelion, and grants from Bayer and Pfizer, outside the submitted work.
Conflict of interest: R. Oudiz reports grants and consulting and speaker fees from Actelion, Gilead and United Therapeutics, grants from Aadi and GSK, consulting fees from Complexa, Acceleron and Medtronic, and grants and consulting fees from Arena and Reata, outside the submitted work.
Conflict of interest: T. Satoh has nothing to disclose.
Conflict of interest: F. Torres reports personal fees from Actelion, Bayer, Reata and Arena, and grants from Gilead, United Therapeutics, Medtronic, Eiger and Bellerophon, during the conduct of the study.
Conflict of interest: A. Torbicki reports personal fees from Actelion, AOP Orphan Pharmaceutics, Bayer and MSD, and non-financial support from Pfizer, outside the submitted work; and is also a chairperson of the Foundation for Pulmonary Hypertension, which receives donations from outside parties to support its activities. The chair receives no financial compensation for this function.
References
- 1.Vachiéry J-L, Tedford RJ, Rosenkranz S, et al. . Pulmonary hypertension due to left heart disease. Eur Respir J 2019; 53: 1801897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nathan SD, Barbera JA, Gaine SP, et al. . Pulmonary hypertension in chronic lung disease and hypoxia. Eur Respir J 2019; 53: 1801914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim NH, Delcroix M, Jais X, et al. . Chronic thromboembolic pulmonary hypertension. Eur Respir J 2019; 53: 1801915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rich S, Dantzker DR, Ayres SM, et al. . Primary pulmonary hypertension. A national prospective study. Ann Intern Med 1987; 107: 216–223. [DOI] [PubMed] [Google Scholar]
- 5.Bossone E, Paciocco G, Iarussi D, et al. . The prognostic role of the ECG in primary pulmonary hypertension. Chest 2002; 121: 513–518. [DOI] [PubMed] [Google Scholar]
- 6.Henkes IR, Gan CT, van Wolferen SA, et al. . ECG monitoring of treatment response in pulmonary arterial hypertension patients. Chest 2008; 134: 1250–1257. [DOI] [PubMed] [Google Scholar]
- 7.Hadinnapola C, Bleda M, Haimel M, et al. . Phenotypic characterization of EIF2AK4 mutation carrier in a large cohort of patients diagnosed clinically with pulmonary arterial hypertension. Circulation 2017; 136: 2022–2033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berry NC, Manyoo A, Oldham WM, et al. . Protocol for exercise hemodynamic assessment: performing an invasive cardiopulmonary exercise test in clinical practice. Pulm Cir 2015; 5: 610–618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sun XG, Hansen JE, Oudiz RJ, et al. . Exercise pathophysiology in patients with primary pulmonary hypertension. Circulation 2001; 104: 429–435. [DOI] [PubMed] [Google Scholar]
- 10.Oudiz RJ. The role of exercise testing in the management of pulmonary arterial hypertension. Semin Respir Crit Care Med 2005; 26: 379–384. [DOI] [PubMed] [Google Scholar]
- 11.Yasunobu Y, Oudiz RJ, Sun XG, et al. . End-tidal Pco2 abnormality and exercise limitation in patients with primary pulmonary hypertension. Chest 2005; 127: 1637–1646. [DOI] [PubMed] [Google Scholar]
- 12.Markowitz DH, Systrom DM. Diagnosis of pulmonary vascular limit to exercise by cardiopulmonary exercise testing. J Heart Lung Transplant 2004; 23: 88–95. [DOI] [PubMed] [Google Scholar]
- 13.Tolle JJ, Waxman AB, Van Horn TL, et al. . Exercise-induced pulmonary arterial hypertension. Circulation 2008; 118: 2183–2189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kovacs G, Maier R, Aberer E, et al. . Borderline pulmonary arterial pressure is associated with decreased exercise capacity in scleroderma. Am J Respir Crit Care Med 2009; 180: 881–886. [DOI] [PubMed] [Google Scholar]
- 15.Dumitrescu D, Nagel C, Kovacs G, et al. . Cardiopulmonary exercise testing for detecting pulmonary arterial hypertension in systemic sclerosis. Heart 2017; 103: 774–778. [DOI] [PubMed] [Google Scholar]
- 16.Hansen JE, Ulubay G, Chow BF, et al. . Mixed-expired and end-tidal CO2 distinguish between ventilation and perfusion defects during exercise testing in patients with lung and heart diseases. Chest 2007; 132: 977–983. [DOI] [PubMed] [Google Scholar]
- 17.Zhai Z, Murphy K, Tighe H, et al. . Differences in ventilatory inefficiency between pulmonary arterial hypertension and chronic thromboembolic pulmonary hypertension. Chest 2011; 140: 1284–1129. [DOI] [PubMed] [Google Scholar]
- 18.Ramos RP, Ferreira EVM, Valois FM, et al. . Clinical usefulness of end-tidal CO2 profiles during incremental exercise in patients with chronic thromboembolic pulmonary hypertension. Respir Med 2016; 120: 70–77. [DOI] [PubMed] [Google Scholar]
- 19.Deboeck G, Niset G, Lamotte M, et al. . Exercise testing in pulmonary arterial hypertension and in chronic heart failure. Eur Respir J 2004; 23: 747–751. [DOI] [PubMed] [Google Scholar]
- 20.Woods PR, Taylor BJ, Frantz RP, et al. . A pulmonary hypertension gas exchange severity (PH-GXS) score to assist with the assessment and monitoring of pulmonary arterial hypertension. Am J Cardiol 2012; 109: 1066–1072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rudski LG, Lai WW, Afilalo J, et al. . Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography. J Am Soc Echocardiogr 2010; 23: 685–713. [DOI] [PubMed] [Google Scholar]
- 22.Lang RM, Badano LP, Mor-Aviv V, et al. . Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2015; 16: 233–270. [DOI] [PubMed] [Google Scholar]
- 23.Foale R, Nihoyannopoulos P, McKenna W, et al. . Echocardiographic measurement of the normal adult right ventricle. Br Heart J 1986; 56: 33–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Galiè N, Humbert M, Vachiery J-L, et al. . 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J 2015; 46: 903–975. [DOI] [PubMed] [Google Scholar]
- 25.Hellenkamp K, Unsold B, Mushemi-Blake S, et al. . Echocardiographic estimation of mean pulmonary artery pressure: a comparison of different approaches to assign the likelihood of pulmonary hypertension. J Am Soc Echocardiogr 2018; 31: 89–98. [DOI] [PubMed] [Google Scholar]
- 26.Magnino C, Omede P, Avenatti E, et al. . Inaccuracy of right atrial pressure estimates through inferior vena cava indices. Am J Cardiol 2017; 120: 1667–1673. [DOI] [PubMed] [Google Scholar]
- 27.Focardi M, Cameli M, Carbone SF, et al. . Traditional and innovative echocardiographic parameters for the analysis of right ventricular performance in comparison with cardiac magnetic resonance. Eur Heart J Cardiovasc Imaging 2015; 16: 47–52. [DOI] [PubMed] [Google Scholar]
- 28.Bajc M, Neilly JV, Miniati N, et al. . EANM guidelines for ventilation/perfusion scintigraphy. Part 1. Pulmonary imaging with ventilation/perfusion single photon emission tomography. Eur J Nucl Med Mol Imaging 2009; 36: 1356–1370. [DOI] [PubMed] [Google Scholar]
- 29.Glaser J, Chamarthy M, Haramati LB, et al. . Successful and safe implementation of a trinary interpretation and reporting strategy for V/Q lung scintigraphy. J Nucl Med 2011; 52: 1508–1512. [DOI] [PubMed] [Google Scholar]
- 30.Shen Y, Wan C, Tian P, et al. . CT-Base pulmonary artery measurement in the detection of pulmonary hypertension: a meta-analysis and systematic review. Medicine 2014; 93: e256–e264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hoeper MM, Bogaard HJ, Condliffe R, et al. . Definitions and diagnosis of pulmonary hypertension. J Am Coll Cardiol 2013; 62: D42–D50. [DOI] [PubMed] [Google Scholar]
- 32.Khanna D, Gladue H, Channick R, et al. . Recommendations for screening and detection of connective tissue disease associated pulmonary arterial hypertension. Arthritis Rheum 2013; 65: 3194–3201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Young A, Nagaraja V, Basilious M, et al. . Update of screening and diagnostic modalities for connective tissue disease-associated pulmonary arterial hypertension. Semin Arthritis Rheum 2018; in press [ 10.1016/j.semarthrit.2018.10.010]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ten Freyhaus H, Vogel D, Lehmann C, et al. . Echocardiographic screening for pulmonary arterial hypertension in HIV-positive patients. Infection 2014; 42: 737–741. [DOI] [PubMed] [Google Scholar]
- 35.Henriques-Forsythe M, Annangi S, Farber HW. Prevalence and hospital discharge status of human immunodeficiency virus-associated pulmonary arterial hypertension in the United States. Pulm Circ 2015; 5: 506–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Quezada M, Martin-Carbonero L, Soriano V, et al. . Prevalence and risk factors associated with pulmonary hypertension in HIV-infected patients on regular follow up. AIDS 2012; 26: 1387–1392. [DOI] [PubMed] [Google Scholar]
- 37.Dhillon NK, Li F, Xue B, et al. . Effect of cocaine on human immunodeficiency virus-mediated pulmonary endothelial and smooth muscle dysfunction. Am J Respir Cell Mol Biol 2011; 45: 40–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Centers for Disease Control and Prevention. HIV among women. www.cdc.gov/hiv/group/gender/women/index.html Date last updated: July 5, 2018. Date last accessed: October 30, 2018.
- 39.Dalvi P, O'Brien-Ladner A, Dhillon NK. Down regulation of bone morphogenetic protein receptor axis during HIV-1 and cocaine-mediated pulmonary smooth muscle hyperplasia: implications for HIV-related pulmonary arterial hypertension. Arterioscler Thromb Vasc Biol 2013; 33: 2585–2295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sangal RB, Taylor LE, Gillai F, et al. . Risk of echocardiographic pulmonary hypertension in individuals with human immunodeficiency virus hepatitis C virus coinfection. Ann Am Thorac Soc 2014; 11: 1553–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Schwarze-Zander C, Pabst S, Hammerstingl C, et al. . Pulmonary hypertension in HIV infection: a prospective echocardiographic study. HIV Med 2015; 16: 578–582. [DOI] [PubMed] [Google Scholar]
- 42.Jacher JE, Martin LJ, Chung WK, et al. . Pulmonary arterial hypertension: specialists’ knowledge, practices, and attitudes of genetic counseling and genetic testing in the USA. Pulm Circ 2017; 7: 372–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Girerd B, Montani D, Jais X, et al. . Genetic counselling in a national referral centre for pulmonary hypertension. Eur Respir J 2016; 47: 541–552. [DOI] [PubMed] [Google Scholar]
- 44.Larkin EK, Newman JH, Austin ED, et al. . Longitudinal analysis casts doubt on the presence of genetic anticipation in heritable pulmonary arterial hypertension. Am J Respir Crit Care Med 2012; 186: 892–896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Revuz S, Decullier E, Ginon I, et al. . Pulmonary hypertension subtypes associated with hereditary haemorrhagic telangiectasia: haemodynamic profiles and survival probability. PLoS One 2017; 12: e0184227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.DeMartino ES, Cartin-Ceba R, Findlay JY, et al. . Frequency and outcomes of patients with increased mean pulmonary artery pressure at the time of liver transplantation. Transplantation 2017; 101: 101–106. [DOI] [PubMed] [Google Scholar]
- 47.Sithamparanathan S, Nair A, Thirugnanasothy L, et al. . Survival in portopulmonary hypertension: outcomes of the United Kingdom National Pulmonary Arterial Hypertension Registry. J Heart Lung Transplant 2017; 36: 770–779. [DOI] [PubMed] [Google Scholar]
- 48.Leblanc M, Leveillée F, Turcotte E. Prospective evaluation of the negative predictive value of V/Q SPECT using 99mTc-Technegas. Nucl Med Commun 2007; 28: 667–672. [DOI] [PubMed] [Google Scholar]
- 49.Grüning T, Drake BE, Farrell SL, et al. . Three-year clinical experience with VQ SPECT for diagnosing pulmonary embolism: diagnostic performance. Clin Imaging 2014; 38: 831–835. [DOI] [PubMed] [Google Scholar]
- 50.Gutte H, Mortensen J, Jensen CV, et al. . Detection of pulmonary embolism with combined ventilation–perfusion SPECT and low-dose CT: head-to-head comparison with multidetector CT angiography. J Nucl Med 2009; 50: 1987–1992. [DOI] [PubMed] [Google Scholar]
- 51.Hurwitz LM, Yoshizumi TT, Goodman PC, et al. . Radiation dose savings for adult pulmonary embolus 64-MDCT using bismuth breast shields, lower peak kilovoltage, and automatic tube current modulation. AJR Am J Roentgenol 2009; 192: 244–253. [DOI] [PubMed] [Google Scholar]
- 52.International Commission on Radiological Protection. Radiation dose to patients from radiopharmaceuticals (Addendum to ICRP 53). ICRP Publication 80. Ann ICRP 1998; 28: 1–126. [DOI] [PubMed] [Google Scholar]
- 53.International Commission on Radiation Protection. Managing patient dose in multi-detector computed tomography (MDCT). ICRP Publication 102. Ann ICRP 2007; 37: 1–79. [DOI] [PubMed] [Google Scholar]
- 54.Lau EM, Bailey DL, Bailey EA, et al. . Pulmonary hypertension leads to a loss of gravity dependent redistribution of regional lung perfusion: a SPECT/CT study. Heart 2014; 100: 47–53. [DOI] [PubMed] [Google Scholar]
- 55.Giordano J, Khung S, Duhamel A, et al. . Lung perfusion characteristics in pulmonary arterial hypertension (PAH) and peripheral forms of chronic thromboembolic pulmonary hypertension (pCTEPH): dual-energy CT experience in 31 patients. Eur Radiol 2017; 27: 1631–1639. [DOI] [PubMed] [Google Scholar]
- 56.Rajaram S, Swift AJ, Telfer A, et al. . 3D contrast-enhanced lung perfusion MRI is an effective screening tool for chronic thromboembolic pulmonary hypertension: results from the ASPIRE Registry. Thorax 2013; 68: 677–678. [DOI] [PubMed] [Google Scholar]
- 57.Johns CS, Swift AJ, Rajaram S, et al. . Lung perfusion: MRI vs. SPECT for screening in suspected chronic thromboembolic pulmonary hypertension. J Magn Reson Imaging 2017; 46: 1693–1697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nakagawa T, Sakuma H, Murashima S, et al. . Pulmonary ventilation-perfusion MR imaging in clinical patients. J Magn Reson Imaging 2001; 14: 419–424. [DOI] [PubMed] [Google Scholar]
- 59.Wang N, Hu X, Liu C, et al. . A systematic review of the diagnostic accuracy of cardiovascular magnetic resonance for pulmonary hypertension. Can J Cardiol 2014; 30: 455–463. [DOI] [PubMed] [Google Scholar]
- 60.Freed BH, Gomberg-Maitland M, Chandra S, et al. . Late gadolinium enhancement cardiovascular magnetic resonance predicts clinical worsening in patients with pulmonary hypertension. J Cardiovasc Magn Reson 2012; 14: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.El Abouelnour A, Doyle M, Thompson DV, et al. . Does late gadolinium enhancement still have value? Right ventricular internal mechanical work, Ea/Emax and late gadolinium enhancement as prognostic markers in patients with advanced pulmonary hypertension via cardiac MRI. Cardiol Res Cardiovasc Med 2017; 2017: CRCM-111. [PMC free article] [PubMed] [Google Scholar]
- 62.Mehta BB, Auger DA, Gonzalez JA, et al. . Detection of elevated right ventricular extracellular volume in pulmonary hypertension using Accelerated and Navigator-Gated Look-Locker Imaging for Cardiac T1 Estimation (ANGIE) cardiovascular magnetic resonance. J Cardiovasc Magn Reson 2015; 17: 110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.De Siqueira ME, Pozo E, Fernandes VR, et al. . Characterization and clinical significance of right ventricular mechanics in pulmonary hypertension evaluated with cardiovascular magnetic resonance feature tracking. J Cardiovasc Magn Reson 2016; 18: 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Reiter G, Reiter U, Kovacs G, et al. . Magnetic resonance-derived 3-dimensional blood flow patterns in the main pulmonary artery as a marker of pulmonary hypertension and a measure of elevated mean pulmonary arterial pressure. Circ Cardiovasc Imaging 2008; 1: 23–30. [DOI] [PubMed] [Google Scholar]
- 65.Reiter G, Reiter U, Kovacs G, et al. . Blood flow vortices along the main pulmonary artery measured with MR imaging for diagnosis of pulmonary hypertension. Radiology 2015; 275: 71–79. [DOI] [PubMed] [Google Scholar]
- 66.Helderman F, Mauritz GJ, Andringa KE, et al. . Early onset of retrograde flow in the main pulmonary artery is a characteristic of pulmonary arterial hypertension. J Magn Reson Imaging 2011; 33: 1362–1368. [DOI] [PubMed] [Google Scholar]
- 67.Tang BT, Pickard SS, Chan FP, et al. . Wall shear stress is decreased in the pulmonary arteries of patients with pulmonary arterial hypertension: an image based, computational fluid dynamics study. Pulm Circ 2012; 2: 470–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Odagiri K, Inui N, Miyakawa S, et al. . Abnormal hemodynamics in the pulmonary artery seen on time-resolved 3-dimensional phase-contrast magnetic resonance imaging (4D-flow) in a young patient with idiopathic pulmonary arterial hypertension. Circ J 2014; 78: 1770–1772. [DOI] [PubMed] [Google Scholar]
- 69.Odagiri K, Inui N, Hakamata A, et al. . Non-invasive evaluation of pulmonary arterial blood flow and wall shear stress in pulmonary arterial hypertension with 3D phase contrast magnetic resonance imaging. Springerplus 2016; 5: 1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Barker AJ, Roldan-Alzate A, Entezari P, et al. . Four-dimensional flow assessment of pulmonary artery flow and wall shear stress in adult pulmonary arterial hypertension: results from two institutions. Magn Reson Med 2015; 73: 1904–1913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Domingo E, Grignola JC, Aguilar R, et al. . In vivo assessment of pulmonary arterial wall fibrosis by intravascular optical coherence tomography in pulmonary arterial hypertension: a new prognostic marker of adverse clinical follow-up. Open Respir Med J 2013; 7: 26–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dai Z, Fukumoto Y, Tatebe S, et al. . OCT imaging for the management of pulmonary hypertension. JACC Cardiovasc Imaging 2014; 7: 843–845. [DOI] [PubMed] [Google Scholar]
- 73.Dawes TJW, de Marvao A, Shi W, et al. . Machine learning of three-dimensional right ventricular motion enables outcome prediction in pulmonary hypertension: a cardiac MR imaging study. Radiology 2017; 283: 381–390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.McMahon TJ, Bryan NS. Biomarkers in pulmonary vascular disease: gauging response to therapy. Am J Cardiol 2017; 120: S89–S95. [DOI] [PubMed] [Google Scholar]
- 75.Rameh V, Kossaify A. Role of biomarkers in the diagnosis, risk assessment, and management of pulmonary hypertension. Biomark Insights 2016; 11: 85–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Anwar A, Ruffenach G, Mahajan A, et al. . Novel biomarkers for pulmonary arterial hypertension. Respir Res 2016; 17: 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Austin ED, West J, Loyd JE, et al. . Translational advances in the field of pulmonary hypertension molecular medicine of pulmonary arterial hypertension. From population genetics to precision medicine and gene editing. Am J Respir Crit Care Med 2017; 195: 23–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Elinoff JM, Agarwal R, Barnett CF, et al. . Challenges in pulmonary hypertension: controversies in treating the tip of the iceberg. Am J Respir Crit Care Med 2018; 198: 166–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Maron BA, Abman SH. Translational advances in the field of pulmonary hypertension. focusing on developmental origins and disease inception for the prevention of pulmonary hypertension. Am J Respir Crit Care Med 2017; 195: 292–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nakhleh MK, Haick H, Humbert M, et al. . Volatolomics of breath as an emerging frontier in pulmonary arterial hypertension. Eur Respir J 2017; 49: 1601897. [DOI] [PubMed] [Google Scholar]
- 81.Newman JH, Rich S, Abman SH, et al. . Enhancing insights into pulmonary vascular disease through a precision medicine approach. A joint NHLBI–Cardiovascular Medical Research and Education Fund Workshop Report. Am J Respir Crit Care Med 2017; 195: 1661–1670. [DOI] [PMC free article] [PubMed] [Google Scholar]