Abstract
Despite the existence of a safe and effective vaccine, human papillomavirus (HPV) remains prevalent in the United States, with late adolescence and early adulthood being periods of increased risk. Thus, targeting college-aged individuals for HPV prevention and vaccination promotion is critical—particularly in regions such as the Deep South where vaccination rates remain low. This study sought to examine awareness and knowledge of HPV as well as experiences and attitudes regarding HPV vaccination among college students in the Deep South. Specifically, we completed a cross-sectional survey of 256 undergraduate students from a large public university in South Carolina. Although a majority of participants were aware of HPV, significant knowledge gaps existed, particularly regarding prevention, symptoms, and consequences of HPV infection. Participants were also largely unaware of men’s susceptibility for negative HPV outcomes. Multivariate regression modeling was used to identify predictors of HPV knowledge, with results indicating that participants who were female and white, as well as those who were vaccinated, had higher levels of HPV knowledge. Findings highlight the need for comprehensive HPV education on college campuses and offer insights to priority populations that may be appropriate focuses of efforts to increase HPV knowledge and vaccination rates.
Keywords: Human papillomavirus, papillomavirus infections, vaccination, health knowledge, adolescent health, student health, surveys and questionnaires
Introduction
Around 79 million Americans are estimated to be infected with genital human papillomavirus (HPV), the most common sexually transmitted infection in the world.1,2 Human papillomaviruses are a family of viruses that infect epithelial tissue; while most types are low-risk and resolve spontaneously or become undetectable, certain high-risk types—most notably HPV 16 and 18—are oncogenic, causing a wide range of cancers that affect women (eg, cervical, vaginal, and vulvar cancers), men (eg, penile cancer), and both sexes (eg, oropharyngeal and anal cancers).2 HPV is prevalent among college-aged individuals (eg, aged 18-22) due to increased rates of high-risk sexual behaviors, including multiple sexual partners and engagement in unprotected sex.3 Such behavioral risks yield high rates of HPV, with data from 2007 to 2010 indicating an HPV prevalence of 59.8% among young women aged 20 to 24.4 Other potential causes for increased HPV risk during this period have been suggested and include a lack of engagement in preventive care and limited HPV knowledge.5
Beginning in 2006, vaccination against the main types of high-risk HPV has been available in the United States, with 3 vaccines (ie, Cervarix, Gardasil, Gardasil 9) currently approved for use.2 Routine vaccination is recommended for male and female adolescents at ages 11 to 12, though vaccination can begin as early as age 9.2 Despite this recommendation, uptake of the HPV vaccine has been slow and uneven in the United States, with many youth remaining un- or under-vaccinated.2 Currently, only 60% of US adolescents between the ages of 13 and 17 have received at least one dose of the HPV vaccine, with 2 or 3 doses needed for full coverage depending on the selected vaccine.6 HPV vaccination coverage among female adolescents increased gradually following the vaccine’s approval for girls in 2006; in contrast, coverage among male adolescents has risen rapidly since its approval for boys in 2011, resulting in a shrinking “gender-gap” in vaccination uptake.6 However, several interesting racial and ethnic differences in HPV vaccination coverage remain. Currently, African American and Hispanic youth in the United States are significantly more likely to receive the HPV vaccine than white, non-Hispanic youth, with 65.9% of African American adolescents and 69.8% of Hispanic adolescents receiving at least one dose of the HPV vaccine, compared to 54.7% of white, non-Hispanic youth.6
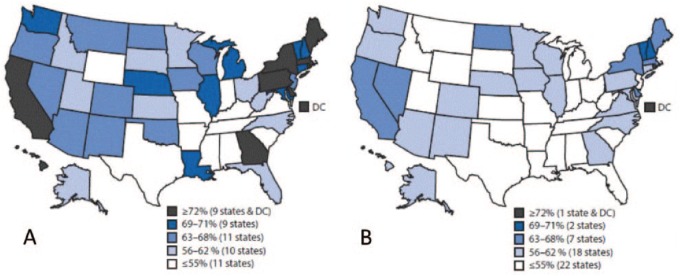
In addition, significant geographic disparities in HPV vaccination persist, with several states in the “Deep South” region (eg, Mississippi, Alabama, South Carolina) falling significantly below the national average and far below recommended Healthy People 2020 goals of 80% coverage (see Figure 1).6,7 South Carolina is representative of these regional challenges, with only 30.8% of females and 27.4% of males aged 13 to 17 years currently “up-to-date” with the HPV vaccination series.6 This low uptake is particularly alarming given the estimated 30 000 new cases of anogenital cancer and 4000 deaths from cervical cancer that are estimated to occur yearly in the United States due to HPV.8 Regional differences in HPV vaccine uptake are likely to stem from complex and intersecting factors including policy-related and socio-cultural factors, as well as factors related to health care services and infrastructure. In the United States, youth residing in rural areas (ie, non-Metropolitan Statistical Areas) are less likely to receive the HPV vaccine than non-rural peers, possibly due to fewer pediatric primary care providers in these areas.6,9 These urban-rural disparities are not present for Tdap coverage, suggesting that a lack of access to vaccines is not a likely reason for low HPV vaccination among rural adolescents.6 Regional and state variation in HPV vaccination may also be due to lower levels of HPV knowledge and awareness among residents and unwillingness or discomfort of providers to initiate discussions about HPV with families.5 Some Southern states such as Georgia have had success in rapidly increasing adolescent HPV vaccination rates through a variety of initiatives, including statewide health promotion campaigns, policy-related efforts, and the development of vaccination partnerships with local health departments and health care providers.10
Figure 1.
Estimated vaccination coverage with ⩾1 HPV vaccine among female (A) and male (B) adolescents aged 13 to 17 years—National Immunization Survey-Teen, United States, 2016. HPV indicates human papillomavirus.
Reproduced from Walker et al.6
Because HPV vaccination is recommended through age 21 for males and through age 26 for females and other priority populations (eg, men who have sex with men, transgender individuals), college and university health systems have an important role to play in comprehensive, public health approaches to reducing the burden of HPV. College health professionals may work to raise awareness and knowledge of HPV, encourage the adoption of healthy sexual practices, and provide vaccination to willing students. College may be a particularly important window of opportunity for late HPV vaccination as it is a time when individuals assume greater responsibility for their medical care and frequently begin to make medical decisions, including receiving vaccination, without parental knowledge or consent. Although much research on attitudes and beliefs of HPV vaccination has focused on parents,11–14 an emerging body of literature is beginning to explore how college students make decisions about HPV vaccination. This literature suggests a positive association between students’ HPV knowledge, perceptions of HPV vaccine acceptability, and actual uptake of the vaccine.15,16
Given the need to target college-aged individuals in the South for “catch-up” HPV vaccination, it is important to gain a deeper understanding of factors that may increase their likelihood to be vaccinated and/or engage in other preventive behaviors (eg, routine condom use). The Health Belief Model17 provides a theoretical framework to investigate key factors that may influence HPV-related behaviors, and suggests that an individual’s awareness and knowledge of HPV, including perceived severity and risk, are likely to influence HPV-related behaviors. Understanding college students’ HPV-related knowledge, attitudes, and perceived risk may help to inform future interventions and policies aimed at HPV-preventive behaviors, including “catch-up” vaccination among college students. Thus, the purpose of this study was to explore awareness and knowledge of HPV, as well as experiences and attitudes regarding HPV vaccination among college students in South Carolina, as well as to identify current sources of HPV information. This information may serve as a starting place to identify effective strategies and interventions to increase HPV vaccination and thus reduce the prevalence of high-risk strains of HPV among a key target population (ie, college-aged individuals).
Method
Participants
A non-probability, purposive sample of college students from South Carolina were recruited for this study from undergraduate courses in the College of Arts & Sciences and School of Public Health at a large public university. The study protocol was approved by the Institutional Review Board at the University of South Carolina, which waived requirement for written documentation of informed consent due to the study’s minimal risk of harm. Interested students were provided with a research information sheet that described study goals and included potential benefits and risks of participation. This sheet was reviewed with interested students, and in total, 256 participants consented to participate. All then individually completed a paper-pencil survey in a classroom setting, with data collection occurring between September and October of 2017. Students who participated were eligible to be entered into a drawing for 1 of 6 US $25 incentives.
Measures
Demographic characteristics
Participants provided information about demographics including age, gender, sexual orientation, race, ethnicity, year in college, undergraduate major, and state of home residence. Participants also reported whether they had ever engaged in sexual contact with others.
HPV awareness, perceptions, and experiences
To assess awareness, participants were asked to report if they had “ever heard” of HPV and the HPV vaccine, with response options including “yes,” “no,” and “I don’t know.” Participants were asked if a health care provider had ever recommended that they receive the HPV vaccine and if they had received at least one dose of the HPV vaccine (“yes,” “no,” “I don’t know”). Participants rated their perceived risk for HPV infection using a 5-point Likert scale, as well as the level of shame they would feel if they found out they had HPV. Higher scores indicate greater perceived risk and more shame. Finally, participants were asked to endorse any encountered sources of information of HPV (eg, health care providers, friends, family, health classes, Internet).
HPV-Knowledge 18
For this study, we created an 18-item HPV knowledge scale to assess participants’ accurate knowledge of HPV infection, HPV-related outcomes, HPV screening, and HPV prevention, with all items adapted from existing published measures.16,18–21 Participants read a series of 18 statements on HPV and responded by endorsing “True,” “False,” or “I don’t know.” Participants received one point for each correct response; points were summed to create a total knowledge score (ie, range of 0-18). The HPV-Knowledge 18 (HPV-K18) yielded strong internal consistency (α = .79).
Statistical analysis
We conducted statistical analysis using STATA. Initially, we tabulated descriptive statistics for all variables. Chi-square tests were calculated to examine differences in HPV awareness, vaccine awareness, vaccination status, and sources of HPV information by gender, race, and ethnicity. t Tests were used to compare gender, race, and ethnicity differences in HPV knowledge; perceived risk for HPV; and HPV-associated shame. In addition, we used t tests to compare differences in HPV knowledge based on reported sources of information. We then ran a regression model with HPV knowledge as the outcome variable and predictor variables of age, gender (male, female), race (non-white, white), ethnicity (Hispanic/Latino, not Hispanic/Latino), history of sexual activity (no, yes), and HPV vaccination status (no/don’t know, yes).
Results
Demographic and behavioral characteristics of participants are shown in Table 1. The majority of the sample was female (80.9%), white (78.5%), and not of Hispanic or Latino ethnicity (88.7%). Participants ranged from 18 to 31 years of age (M = 19.7 SD = 1.7). About half of participants (50.7%) reported being from South Carolina, with 78.5% from the Southern United States. Most participants (96.1%) identified as heterosexual, with 84.8% reporting a history of sexual activity.
Table 1.
Demographic characteristics and HPV experiences of study participants (N = 256).a
| Variable | No. (%) | Mean (SD) |
|---|---|---|
| Gender | ||
| Female | 207 (80.9) | |
| Male | 49 (19.1) | |
| Age | 19.7 (1.7) | |
| Race | ||
| American Indian or Alaskan Native | 2 (0.8) | |
| Asian | 13 (5.1) | |
| Black or African American | 31 (12.1) | |
| White | 201 (78.5) | |
| Other | 2 (0.8) | |
| Not reported | 7 (2.7) | |
| Ethnicity | ||
| Hispanic or Latino | 8 (3.1) | |
| Not Hispanic or Latino | 227 (88.7) | |
| Other | 9 (3.5) | |
| Not reported | 12 (4.7) | |
| State of home residence | ||
| Northeast | 31 (12.1) | |
| Midwest | 15 (5.9) | |
| South | 201 (78.5) | |
| West | 8 (3.1) | |
| Other | 1 (0.4) | |
| Year in school | ||
| Freshman | 72 (28.1) | |
| Sophomore | 62 (24.2) | |
| Junior | 62 (24.2) | |
| Senior | 58 (22.7) | |
| Other | 1 (0.4) | |
| Not reported | 1 (0.4) | |
| Sexually active | ||
| No | 39 (15.2) | |
| Yes | 217 (84.8) | |
| Sexual orientation | ||
| Heterosexual (straight) | 246 (96.1) | |
| Gay or lesbian | 5 (2.0) | |
| Bisexual | 4 (1.6) | |
| Not sure | 1 (0.4) | |
| Ever heard of HPV? | ||
| Yes | 244 (95.3) | |
| No/Do not know | 12 (4.7) | |
| Ever heard of the HPV vaccine? | ||
| Yes | 232 (90.6) | |
| No/Do not know | 23 (9.0) | |
| Not reported | 1 (0.4) | |
| Has a health care provider recommended the HPV vaccine to you? | ||
| Yes | 186 (72.7) | |
| No/Do not know | 70 (27.3) | |
| Have you received at least one dose of the HPV vaccine? | ||
| Yes | 164 (64.1) | |
| No/Do not know | 91 (35.5) | |
| Perceived risk of HPV infection (on a 5-point scale)b | 2 (1.2) | |
| Perceived shame associated with HPV infection (on a 5-point scale)b | 4 (1.0) | |
| Total HPV knowledge (out of 18 total points)b | 8.9 (3.7) |
Abbreviation: HPV, human papillomavirus.
Missing values are not shown in the table but are listed here by number missing: age (4), perceived risk of HPV infection (2), total HPV knowledge score (6), and received one dose of HPV vaccine (1).
Higher scores indicate greater perceived risk for HPV, HPV-related shame, and HPV knowledge.
The vast majority of the participants reported being aware of HPV (95.3%) and the HPV vaccine (90.6%) prior to the day of the survey. Ethnicity was not significantly associated with awareness; however, some differences were observed by gender and race. Female participants were more likely than males to report HPV awareness (97% vs 88%, P = .005) and awareness of the HPV vaccine (95% vs 76%, P < .001). In addition, white participants were more likely than non-white participants (97% vs 90%, P = .04) to report awareness of HPV. Self-reported vaccination rates fell well below Healthy People 2020 targets, with 64.1% of participants reporting having received at least one dose of the HPV vaccine. A larger proportion (72.7%) indicated that a physician or other health care provider had previously recommended that they receive the vaccine. Those who were vaccinated did not differ significantly by gender, race, and ethnicity when compared with those who were not vaccinated.
A summary of participant responses on HPV-K18 items are presented in Table 2. Participants’ mean total knowledge score was 8.9 (SD = 3.7), indicating moderate levels of overall HPV knowledge (ie, potential range of 0-18). Significant differences in HPV knowledge existed between genders and races. Female participants displayed greater overall HPV knowledge (M = 9.2) than male participants (M = 7.2, P = .02), and white participants displayed higher levels of knowledge (M = 9.3) than non-white participants (M = 7.7, P = .01).
Table 2.
Number and percentage of participants correctly answering HPV-Knowledge 18 items and gender differences by item.a
| HPV-K18 item (Correct response) | No. (%) | P-value | ||
|---|---|---|---|---|
| Female | Male | Total | ||
|
174 (84) | 43 (88) | 217 (85) | .52 |
|
108 (52) | 17 (35) | 125 (49) | .03 |
|
145 (70) | 25 (51) | 170 (66) | .01 |
|
16 (8) | 1 (2) | 17 (7) | .15 |
|
149 (72) | 24 (49) | 173 (68) | .00 |
|
19 (9) | 5 (10) | 24 (9) | .80 |
|
112 (54) | 20 (41) | 132 (52) | .09 |
|
157 (76) | 29 (59) | 186 (73) | .02 |
|
113 (55) | 23 (47) | 136 (53) | .34 |
|
27 (13) | 5 (10) | 32 (13) | .59 |
|
170 (82) | 28 (57) | 198 (77) | .00 |
|
174 (84) | 33 (67) | 207 (81) | .01 |
|
163 (79) | 42 (86) | 205 (80) | .30 |
|
107 (52) | 25 (51) | 132 (52) | .93 |
|
41 (20) | 11 (22) | 52 (20) | .68 |
|
115 (56) | 30 (61) | 145 (57) | .47 |
|
75 (37) | 15 (31) | 90 (36) | .49 |
|
28 (14) | 9 (19) | 37 (15) | .36 |
Abbreviation: HPV, human papillomavirus.
Missing values are not shown in the table but are listed here by number missing: Item 6 (2), Item 12 (1), Item 13 (1), Item 17 (3), and Item 18 (2).
Gender difference in correct response = P < .05.
Item analysis revealed patterns of knowledge gaps regarding HPV. For instance, participants were largely incorrect in responding to items about men and HPV. Only 7% of participants correctly responded to an item that asked whether screening is commonly used to test men for HPV (ie, currently there is no approved test for HPV in men), and only 36% knew that HPV may cause penile cancer. Participants displayed confusion about the distinction between HPV and genital herpes, with only 13% of participants aware that HPV does not cause genital herpes. Participants underestimated the prevalence of HPV, with just 15% correctly indicating that at some point almost all sexually active women and men will contract HPV. Although a majority of participants (53%) understood that HPV can cause genital warts, a much smaller portion (9%) were familiar with the fact that most HPV infections will clear on their own. Moreover, more than half of the respondents (51%) were unaware that there is no cure for HPV. On the other hand, some aspects of HPV knowledge seemed well understood by the majority of participants, including that HPV is sexually transmitted (85%), that HPV can lay dormant in the body without symptoms (81%), and that having a greater number of sexual partners increases a person’s chance of acquiring HPV (80%).
Individual items were also analyzed to assess for gender differences (see Table 2). When compared with female participants, males were less likely to know that an abnormal Pap smear may indicate HPV for women (49% vs 72%, P < .01) and were also less likely to know about HPV’s association with cervical cancer (57% vs 82%, P < .01). Female participants were more likely than males to be aware that HPV infections may be asymptomatic (84% vs 67%, P = .01) and that it is possible for a person to acquire more than one type of HPV (70% vs 51%, P = .01). Females also were more knowledgeable that there is currently no cure for HPV (52% vs 35%, P = .03) and that HPV is a common virus (76% vs 59%, P = .02) as compared with their male counterparts.
Participants were also asked to indicate sources of knowledge of HPV, with the most reported sources being health care provider (68%), school health education class (64%), and the Internet (50%) (see Table 3). Female students were more likely than males to report that they had learned about HPV from a health care provider (73% vs 47%, P < .01), radio/TV (33% vs 12%, P < .01), and magazines/newspapers (19% vs 6%, P = .03). We next examined whether a particular source of information was associated with higher overall HPV knowledge scores. Participants who reported learning about HPV from health care providers (P = .03), school health education classes (P < .01), and the Internet (P = .05) had higher levels of HPV knowledge than those who did not endorse that particular source of knowledge.
Table 3.
Number and percentage of participants endorsing sources of HPV information and gender differences.
| Sources of HPV information | Female No. (%) |
Male No. (%) |
Total No. (%) |
P-value |
|---|---|---|---|---|
| Health care provider* | 151 (73) | 23 (47) | 174 (68) | .00 |
| School health education class | 131 (63) | 32 (65) | 163 (64) | .79 |
| Internet | 104 (50) | 24 (49) | 128 (50) | .87 |
| Radio/TV* | 69 (33) | 6 (12) | 75 (29) | .00 |
| Family member | 66 (32) | 9 (18) | 75 (29) | .06 |
| Friend | 49 (24) | 12 (24) | 61 (24) | .90 |
| Magazine/newspaper* | 40 (19) | 3 (6) | 43 (17) | .03 |
| Community health program | 16 (8) | 1 (2) | 17 (7) | .15 |
| Other | 6 (3) | 2 (4) | 8 (3) | .67 |
| Centers for Disease Control and Prevention (CDC) National Sexually Tranmitted Diseases (STD) hotline | 4 (2) | 0 (0) | 4 (2) | .33 |
Abbreviation: HPV, human papillomavirus.
Gender difference = P < .05.
Finally, multivariate regression analysis was used to test whether key demographic and behavioral variables significantly predicted higher HPV knowledge (see Table 4). Specifically, the variables of gender, age, race, ethnicity, HPV vaccination status, and history of sexual activity were included in the regression model. Results of the regression indicated that the predictors explained 8.2% of the variance (R2 = 0.08, F(6, 237.4) = 3.5, P ⩽ .01). Three variables in the model were significant predictors of total HPV knowledge: gender, HPV vaccination status, and race. Being female significantly predicted HPV knowledge (B = 1.20, SE = 0.59, P = .04), as did having received the HPV vaccine (B = 1.25, SE = 0.48, P = .01). Finally, being white also significantly predicted higher total HPV knowledge (B = 1.21, SE = 0.60, P = .04). Age (B = 0.12, SE = 0.14), ethnicity (B = 0.47, SE = 0.93), and sexual activity (B = 0.84, SE = 0.63) were not significant (P > .05) in the model.
Table 4.
Estimates from regression model predicting HPV knowledge (R2 = 0.08, F(6, 237.4) = 3.5, P ⩽ .01).
| Variable | b | SE | P |
|---|---|---|---|
| Intercept | 2.65 | 3.06 | |
| Gender | 1.20* | 0.59 | .04 |
| Age | 0.12 | 0.14 | >.05 |
| HPV vaccination status | 1.25* | 0.48 | .01 |
| Sexually active | 0.84 | 0.63 | >.05 |
| Race | 1.21* | 0.60 | .04 |
| Ethnicity | 0.47 | 0.93 | >.05 |
Abbreviation: HPV, human papillomavirus.
P ⩽ .05.
Discussion
This study aimed to explore knowledge and awareness of HPV and HPV vaccination among male and female college students in South Carolina. Results of our research are consistent with recent studies that have found a substantial increase in HPV awareness among college students over the past decade.21–24 In this study, more than 9 out of every 10 participants were aware of HPV and the HPV vaccine. Increasing awareness has been the focus of multiple recent public health campaigns designed to promote the benefits of HPV vaccination to parents and adolescents.25 Despite this high level of awareness, we found many gaps in actual knowledge of HPV, similar to much prior research.5,26,27 The majority of participants were uninformed about the high prevalence of HPV in the general population, as well as current options for screening and treatment. Furthermore, many had limited knowledge about the causal role of HPV in a variety of cancers and genital warts—information that may be key in prompting vaccination. This raises concerns that comprehensive information on HPV is not reaching key youth populations. There is an urgent need to better educate college-aged individuals on HPV. Student health and wellness programs should routinely evaluate the content and impact of current HPV-related services to ensure that comprehensive information on HPV, including the effectiveness of the HPV vaccine and opportunities for vaccination, reach their intended audience.25
A second key finding was that the majority of college students in this study perceived their own risk for HPV to be low. Although clinical HPV status was not evaluated in this study, previous research with college populations has found a large portion of women who believe themselves to be “not at risk” for HPV actually test positive, with Ramirez et al28 finding a 35% HPV prevalence rate among college women who perceived themselves to not be at risk. Students also underestimated overall prevalence, with only 15% of participants familiar with the fact that nearly all US adults will acquire HPV at some point in their lives. According to the Health Belief Model,17 low perceived risk for HPV is likely to decrease an individual’s willingness to engage in vaccination or other preventive behaviors, such as routine condom use.15,29 Among the sample, there was also widespread lack of awareness of the severity of HPV, including its causal links with penile cancer and cervical cancer (ie, particularly among male participants). Increasing college students’ understanding of the likelihood of HPV acquisition and the potential severity of the virus may promote important preventive health behaviors. Making college students more aware of how widespread HPV actually is may also serve to reduce the high levels of shame associated with infection.
Consistent with previous research,21,24,26,30,31 we found that young men were less aware of HPV and displayed poorer knowledge than young women. Moreover, in comparison to white students, non-white students were less likely to be aware of HPV, had lower levels of HPV knowledge, and reported lower perceived risk. These sex and racial differences are important, both for identifying priority populations for future college health promotion campaigns and for exploring potential socio-cultural and systemic factors that may underlie these disparities. Because many men do not develop visible symptoms of HPV and there continues to be no approved male HPV screening tool, men often remain unaware of their positive HPV status—potentially contributing to lower levels of HPV awareness and knowledge.32 In addition, numerous socio-cultural and psychological variables also likely contribute to these observed gender differences. Men have been dubbed “the forgotten fifty percent”33 due to a history of omission from many aspects of sexual and reproductive public health discourse. Societal beliefs regarding gender-based power and gender norms (eg, norms surrounding masculinity) contribute in complex ways to gendered behavioral health practices, and college-aged men have identified multiple barriers to seeking health information and services, including social stigma and concerns about perceived vulnerability.34 In addition to gender disparities, we also found that non-white college students had lower levels of awareness and knowledge than white individuals. This is concerning, particularly within the context of South Carolina, which has some of the largest racial health disparities in the nation and where African American women face significantly increased risk for death from cervical cancer when compared with white women.35 Reducing persistent disparities in HPV infection among African American women36 and promoting equity in the uptake of HPV vaccine is a public health priority, especially in the Southern United States. To achieve these aims, more research is needed to develop culturally specific frameworks of behavioral decision-making regarding HPV, as well as culturally tailored HPV prevention interventions.37,38
In our sample, the majority of students indicated that they would feel shame if they acquired HPV. This finding is concerning because shame associated with HPV may be a barrier for cervical cancer screening.39 Shame may also hinder individuals from disclosing a positive HPV status to their partners and/or families.40 Available literature suggests that the extent to which the acquisition of HPV infection is perceived as shameful is positively associated with awareness about the sexually transmitted nature of this virus and negatively associated with knowledge of the high prevalence of HPV.39,41 Within the current sample, the majority of college students knew about the sexual transmission of HPV and had limited knowledge about its high prevalence, which may have contributed to perceptions of HPV as “shameful.” Reducing the stigma associated with sexually transmitted infections and increasing open communication about sexual health must be foundations of health promotion campaigns designed to lower current rates of HPV and increase acceptability of vaccination.
Finally, this study found that the college students received information about HPV from a myriad of sources but overwhelmingly through health care providers, school health education classes, and the Internet. Health care providers who work in college and university health centers thus have a critical role to play in promoting HPV vaccination for the “catch-up” age rage (eg, through age 21 or 26), including assessing vaccination status, initiating discussions about vaccination (ie, for the un- or under-vaccinated), offering general HPV prevention messaging to all, and ensuring that routine screening for cervical cancer is completed when indicated. In addition, health outreach programs are needed campus-wide to increase HPV awareness and improve knowledge. The rapid increase in the consumption of online health information offers both advantages (eg, ease of access, reduction of common barriers to care such as stigma, transportation, and cost) and disadvantages (eg, potential for misinformation) for college populations. College and university health centers can take a lead in making sure that students can access accurate and supportive health information by ensuring that their websites contain reliable information on HPV and the benefits of vaccination. A recent study found video messaging to be an effective way to increase HPV knowledge as well as vaccination intentions among college-aged individuals,42 and incorporating brief, educational videos online or during patient visits may be a cost-effective strategy. In addition, social networking sites (eg, Facebook, Twitter, etc) may be effective mediums to deliver HPV vaccination messages though much more research is needed in this domain.43
Limitations
Results of this research must be considered in the context of its limitations. First, although the study’s findings on differences by gender and race for HPV awareness and knowledge are important, they must be considered within the context of the sample. The vast majority of individuals in this study were born in the mid-to-late 1990s. Thus, many female participants were in the first age cohort of girls eligible for HPV vaccination when the vaccine was introduced for females in 2006. The recommendation for male vaccination not made until 2011, by then many male participants were older than the recommended age range of 10 to 11 years. Considering cohort effects on HPV, awareness and knowledge is particularly important, given the major changes in recommendations and uptake over the past decade. Current data on HPV vaccination uptake in the United States indicate that the male-female coverage gap is rapidly shrinking and that racial and ethnic minorities are now vaccinated against HPV at higher rates than non-minorities.6 Thus, these findings are unlikely to generalize across age cohorts, and should, most importantly, be used to inform current policy and programs that aim to promote “catch-up” vaccination for college students in South Carolina who may have missed opportunities for education and vaccination during their adolescence.
In addition, the study relied on self-reported data, and we did not confirm participants’ HPV vaccination status or assess the total number of doses received. To reduce the potential for social desirability bias in responding, the survey was anonymous with no identifying data collected. Our sample presents several limitations as well. The sample consisted of students recruited from courses in public health, sociology, and other disciplines. Because we did not employ a probability sampling framework, our participants may not be representative of the broader college population in South Carolina.
Conclusions
HPV remains a critical issue in the United States, and increasing preventive health behaviors, most notably HPV vaccination, is a public health priority. College and university health services can play a key role in promoting sexual health and assisting in “catch up” vaccination efforts for the un- and under-vaccinated. However, low perceived risk for HPV, limited HPV knowledge, and high levels of HPV-associated shame may be barriers to efforts to prevent HPV infection and increase vaccination coverage among college populations. Results of this study confirm the need to accelerate efforts to improve HPV knowledge and increase vaccination among college-aged individuals, particularly in the Deep South. Future studies are needed to identify culturally appropriate frameworks that can speed the reduction of HPV disparities across both places and populations.
Author Contributions
CP and SH designed and implemented the original research study. SK led analysis of study results and drafted the initial manuscript. SH oversaw all aspects of the study, including analysis, manuscript development, and revisions. All authors provided feedback during manuscript development and approved the final manuscript.
Acknowledgments
The authors wish to thank Peyton Pretsch for her assistance with data collection, as well as Julie Morris for her strong support of undergraduate research efforts at the University of South Carolina.
Footnotes
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was supported by the University of South Carolina Magellan Scholars Program under award number 11540-17-45155.
Declaration of Conflicting Interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Informed Consent: Informed consent was provided by all individual participants included in the study, in accordance with study approval from the University of South Carolina Institutional Review Board (#00068790).
ORCID iD: Sayward E Harrison  https://orcid.org/0000-0002-7316-7640
https://orcid.org/0000-0002-7316-7640
References
- 1. World Health Organization. Human papillomavirus vaccines: WHO position paper, May 2017. Wkly Epidemiol Rec. 2017;19:241–268. [Google Scholar]
- 2. Centers for Disease Control and Prevention. HPV vaccine information for clinicians. https://www.cdc.gov/hpv/hcp/need-to-know.pdf. Published 2016. Accessed June 11, 2018.
- 3. American College Health Association. American College Health Association-National College Health Assessment Spring 2008 Reference Group Data Report (abridged): the American College Health Association. J Am Coll Health. 2009;57:477–488. [DOI] [PubMed] [Google Scholar]
- 4. Markowitz LE, Hariri S, Lin C, et al. Reduction in human papillomavirus (HPV) prevalence among young women following HPV vaccine introduction in the United States, National Health and Nutrition Examination Surveys, 2003–2010. J Infect Dis. 2013;208:385–393. [DOI] [PubMed] [Google Scholar]
- 5. Schmotzer GL, Reding KW. Knowledge and beliefs regarding human papillomavirus among college nursing students at a minority-serving institution. J Community Health. 2013;38:1106–1114. doi: 10.1007/s10900-013-9720-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Walker TY, Elam-Evans LD, Singleton JA, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2016. MMWR Morb Mortal Wkly Rep. 2017;66:874–882. doi: 10.15585/mmwr.mm6633a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Office of Disease Prevention and Health Promotion. Healthy People 2020 Topics and Objectives: Immunization and Infectious Diseases. Washington, DC: US Department of Health and Human Services; 2018. www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives. Accessed May 30, 2015. [Google Scholar]
- 8. Petrosky E, Bocchini JJ, Hariri S, et al. Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the advisory committee on immunization practices. MMWR Morb Mortal Wkly Rep. 2015;64:300–304. [PMC free article] [PubMed] [Google Scholar]
- 9. Shipman SA, Lan J, Chang CH, Goodman DC. Geographic maldistribution of primary care for children. Pediatrics. 2011;127:19–27. doi: 10.1542/peds.2010-0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Smith-Lindsey CF. Georgia recognized for increasing the rate of HPV vaccine among adolescent girls. Georgia Department of Public Health Blog; https://dph.georgia.gov/blog/2016-01-08/georgia-recognized-increasing-rate-hpv-vaccine-among-adolescent-girls. Published January 8, 2016. Accessed October 15, 2018. [Google Scholar]
- 11. Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr. 2014;168:76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Radisic G, Chapman J, Flight I, Wilson C. Factors associated with parents’ attitudes to the HPV vaccination of their adolescent sons: a systematic review. Prev Med. 2017;95:26–37. doi: 10.1016/j.ypmed.2016.11.019. [DOI] [PubMed] [Google Scholar]
- 13. VanWormer J, Bendixsen CG, Vickers ER, et al. Association between parent attitudes and receipt of human papillomavirus vaccine in adolescents. BMC Public Health. 2017;17:766. doi: 10.1186/s12889-017-4787-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fu LY, Zimet GD, Latkin CA, Joseph JG. Associations of trust and healthcare provider advice with HPV vaccinate acceptance among African American parents. Vaccine. 2017;35:802–807. doi: 10.1016/j.vaccine.2016.12.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Jones M, Cook R. Intent to receive an HPV vaccine among university men and women and implications for vaccine administration. J Am Coll Health. 2008;57:23–32. [DOI] [PubMed] [Google Scholar]
- 16. Licht AS, Murphy JM, Hyland AJ, Fix BV, Hawk LW, Mahoney MC. Is use of the HPV vaccine among female college students related to HPV knowledge and risk perception? Sex Transm Infect. 2009;86:74–78. [DOI] [PubMed] [Google Scholar]
- 17. Rosenstock IM. The health belief model: explaining health behavior through expectancies. In: Glanz K, Lewis FM, Rimer BK, eds. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, CA: Jossey-Bass; 1990:39–62. [Google Scholar]
- 18. Gerend MA, Shepherd JE. Correlates of HPV knowledge in the era of HPV vaccination: a study of unvaccinated young adult women. Women Health. 2011;51:25–40. doi: 10.1080/03630242.2011.540744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Colón-López V, Ortiz AP, Del Toro-Mejías LM, García H, Clatts MC, Palefsky J. Awareness and knowledge of human papillomavirus (HPV) infection among high-risk men of Hispanic origin attending a sexually transmitted infection (STI) clinic. BMC Infec Dis. 2012;12:346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ragin CC, Edwards RP, Jones J, et al. Knowledge about human papillomavirus and the HPV vaccine—a survey of the general population. Infect Agent Cancer. 2009;4:S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bertram CC, Niederhauser VP. Understanding human papillomavirus: an Internet survey of knowledge, risk, and experience among female and male college students in Hawaii. Am J Health Educ. 2008;39:15–24. [Google Scholar]
- 22. Gerend MA, Magloire ZF. Awareness, knowledge, and beliefs about human papillomavirus in a racially diverse sample of young adults. J Adolesc Health. 2008;42:237–242. doi: 10.1016/j.jadohealth.2007.08.022. [DOI] [PubMed] [Google Scholar]
- 23. Marchand E, Glenn BA, Bastani R. HPV vaccination and sexual behavior in a community college sample. J Community Health. 2013;38:1010-1014. doi: 10.1007/s10900-013-9710-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sandfort JR, Pleasant A. Knowledge, attitudes, and informational behaviors of college students in regard to the human papillomavirus. J Am Coll Health. 2009;58:141–149. doi: 10.1080/07448480903221368. [DOI] [PubMed] [Google Scholar]
- 25. Blasi PR, King D, Henrikson NB. HPV vaccine public awareness campaigns: an environmental scan. Health Promot Pract. 2015;16:897–905. [DOI] [PubMed] [Google Scholar]
- 26. Itty TL, Hodge FS, Poitra C, Cardoza B. HPV awareness among American Indian young adults: implications for health education. J Cult Divers. 2014;21:123–129. [PubMed] [Google Scholar]
- 27. Trad M, Reardon RF, Caraveo D. Understanding HPV and the future implications of contracting the virus. Radiol Technol. 2013;84:457–466. [PubMed] [Google Scholar]
- 28. Ramirez JE, Ramos DM, Clayton L, Kanowitz S, Moscicki AB. Genital human papillomavirus infections: knowledge, perception of risk, and actual risk in a nonclinic population of young women. J Women Health. 1997;6:113–121. [DOI] [PubMed] [Google Scholar]
- 29. Caron RM, Kispert E, McGrath RJ. Human papillomavirus (HPV) vaccine: attitudes, behaviors, and beliefs of at-risk women. Internet J Health. 2008;9:1–14. [Google Scholar]
- 30. Boakye EA, Tobo BB, Rojek RP, Osazuwa-Peters N. Racial and gender disparities in knowledge and awareness of HPV and HPV vaccine in a national sample of US adults. Cancer Epidemiol Biomarkers Prev. 2016;25(3 Suppl): Abstract nr A51. doi: 10.1158/1538-7755.DISP15-A51. [DOI] [Google Scholar]
- 31. Smith ML, Wilson KL, Pulczinski JC, Ory MG. Support for HPV vaccination mandates for both females and males. Am J Health Behav. 2014;38:831–838. doi: 10.5993/AJHB.38.6.5. [DOI] [PubMed] [Google Scholar]
- 32. Centers for Disease Control and Prevention. HPV and men—fact sheet. https://www.cdc.gov/std/hpv/stdfact-hpv-and-men.htm. Published 2017. Accessed May 15, 2018.
- 33. Varga CA. The forgotten fifty per cent: a review of sexual and reproductive health research and programs focused on boys and young men in sub-Saharan Africa. Afr J Reprod Health. 2001;5:175–195. [PubMed] [Google Scholar]
- 34. Davies J, McCrae BP, Frank J, et al. Identifying male college students’ perceived health needs, barriers to seeking help, and recommendations to help men adopt healthier lifestyles. J Am Coll Health. 2000;48:259–267. [DOI] [PubMed] [Google Scholar]
- 35. Adams SA, Fleming A, Brandt HM, et al. Racial disparities in cervical cancer mortality in an African American and European American cohort in South Carolina. J S C Med Assoc. 2009;105:237–244. [PMC free article] [PubMed] [Google Scholar]
- 36. Dunne EF, Unger ER, Sternberg M, et al. Prevalence of HPV infection among females in the United States. JAMA. 2007;297:813–819. [DOI] [PubMed] [Google Scholar]
- 37. Brawner BM, Baker JL, Voytek CD, et al. The development of a culturally relevant, theoretically driven HPV prevention intervention for urban adolescent females and their parents/guardians. Health Promot Pract. 2013;14:624–636. [DOI] [PubMed] [Google Scholar]
- 38. Bynum SA, Brandt HM, Sharpe PA, Williams MS, Kerr JC. Working to close the gap: identifying predictors of HPV vaccine uptake among young African American women. J Health Care Poor Underserved. 2011;22:549–561. [DOI] [PubMed] [Google Scholar]
- 39. Waller J, Marlow LA, Wardle J. The association between knowledge of HPV and feelings of stigma, shame and anxiety. Sex Transm Infect. 2007;83:155–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Tomás-Aragonés L, Castillo-Amores AB, Rodríguez-Cerdeira C, Marrón-Moya SE. Psychological aspects associated with the acquisition and development of HPV infection and its repercussion on quality of life. Open Dermatol J. 2009;3:133–136. doi: 10.2174/1874372200903010133. [DOI] [Google Scholar]
- 41. O’Connor M, Costello L, Murphy J, et al. “I don’t care whether it’s HPV or ABC, I just want to know if I have cancer”: factors influencing women’s emotional responses to undergoing human papillomavirus testing in routine management in cervical screening: a qualitative study. BJOG. 2014;121:1421–1430. doi: 10.1111/1471-0528.12741. [DOI] [PubMed] [Google Scholar]
- 42. Sheaves CG. Influence of education strategies on young women’s knowledge and attitudes about the HPV vaccine. Womens Healthcare. 2016;4:38–45. [Google Scholar]
- 43. Lee MJ, Cho J. Promoting HPV vaccination online: message design and media choice. Health Promot Pract. 2017;18:645–653. doi: 10.1177/1524839916688229. [DOI] [PubMed] [Google Scholar]