Abstract
Introduction
Extended intralesional curettage, together with bone grafting/cementing, is considered as a surgical treatment option for giant cell tumour of the bone. This study aimed to discover the efficacy and recurrence rate with the use of bone cement in giant cell tumour and to compare it with that of bone grafting.
Material and methods
The present systemic review is derived from the publications in the past 10 years (2009–2018). A literature search was performed via PubMed, using suitable keywords and Boolean operators database (‘Giant cell tumor,’ ‘osteoclastoma,’ ‘bone,’ ‘bone cement,’ ‘bone graft’ and ‘curettage’). A detailed statistical analysis of the data derived from the published literature was done.
Results
The patients who underwent bone graft only exhibited significantly higher recurrence rates than those treated with polymethyl methacrylate only (risk ratio 1.90; 95% confidence interval 1.14, 3.16; overall effect Z = 2.488; P-value 0.012). The observational analysis was done in rest of the seven studies; three studies showed no recurrence rate. Only one study reported the highest recurrence rate of 42% and the remaining six had an overall recurrence rate of 20.4%.
Conclusion
The use of bone cement was associated with a statistically significantly lower recurrence rate than bone grafting in giant cell tumour of bones. We therefore recommend the use of bone cement with extensive intralesional curettage. Adjuvant therapy like electrocautery, phenol irrigation and the use of intravenous denosumab or bisphosphonates may help in decreasing the incidence of recurrence in giant cell tumour of bone.
Keywords: Giant cell tumour, Polymethyl methacrylate, Bone graft, Bone cement, Curettage
Introduction
Giant cell tumour of bone is a known locally aggressive tumour, mostly involving the ends of long bones. It commonly affects people aged 20–40 years, with a female preponderance. The disease accounts for approximately 20% of all benign bone tumours.1 The most common sites (in decreasing order) are a distal femur, proximal tibia and distal radius. The reported recurrence rates after various surgical procedures for giant cell tumour is as high as 50%.2,3 It has been observed that there is a strong correlation between surgical margins and the rate of recurrence, dependent on whether intralesional curettage, marginal or wide resection is used.4 Owing to the frequent meta-epiphyseal location, wide resection may result in a significant functional deficit. Hence, intralesional curettage has become the most recommended treatment.5,6 After curettage, filling the cavity with bone graft or bone cement is commonly performed to provide structural support and to prevent collapse.7,8
Bone cement has been proposed to reduce local recurrence resulting in disease-free survival rates as high as 85%.9 Cementing after curettage immediately stabilises the affected limb and releases heat during polymerisation that kills remaining tumour cell.10 Bone grafting has also been used extensively in the past, but recurrence rate is much higher compared with cement.11 However, the downside of using bone cement in the subchondral region is that it may damage the adjacent articular cartilage. Bone cement, once incorporated, gives a better overall functional outcome.
The present systemic review is derived from the publications in the past 10 years. This study aimed to discover the present status of the efficacy of the use of bone cement in giant cell tumour and to compare the recurrence rate with that of bone grafts.
Material and methods
A literature search was performed via PubMed, using suitable keywords and Boolean operator’s database (‘Giant cell tumour’, ‘osteoclastoma’, ‘bone graft’, ‘bone cement’ and ‘curettage’) from January 2009 to January 2018. These electronic literature databases provided us with a systematic and objective means of evaluating the emerging scientific literature in any field critically. The search resulted in 150 papers. Articles were subtyped as one of: clinical study, clinical trial, clinical trial phase 1, clinical trial phase 2, clinical trial phase 3, clinical trial phase 4, comparative study, controlled clinical trial, meta-analysis, multicentre study, observational study, randomised controlled trial, review article, systemic review. For each clinical article, the level of evidence was determined, resulting in 82 papers.
Publications were then analysed and filtered to remove publications older than 10 years . One paper written in Chinese was excluded from the study. Publication trends and most cited paper in the field were then analysed. Additionally, bibliographies from selected articles and pertinent journals were searched for additional relevant citations, leaving 20 papers. We also studied the citation trends of these articles, checked the search strategy and the number of citations received by these papers in Google, which is a free citation database with very broad coverage. Eventually, all the papers that were not relevant to the present study were excluded, leaving us with 10 papers for the study.
Results
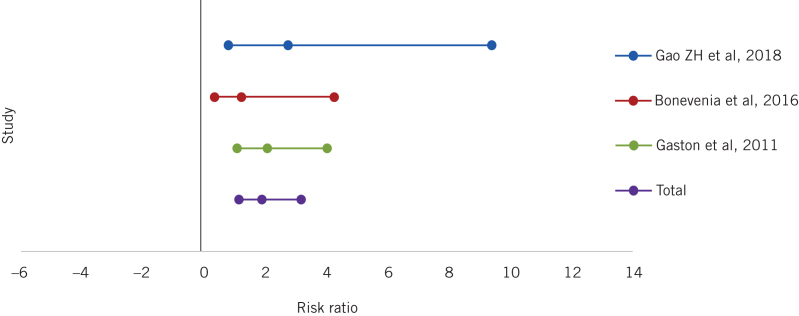
A comparative analysis between curettage with bone graft and curettage with cement was performed for three studies (Table 1). We analysed the risk ratio (RR) and P-value for each study. A forest plot was then created. Local recurrence rates differed significantly between patients treated with polymethyl methacrylate only and those treated with bone graft only, with patients who had bone graft only exhibiting significantly higher recurrence rates than with polymethyl methacrylate or bone cement only (RR 1.90, 95% confidence interval, CI, 1.14, 3.16; overall effect: Z = 2.488; P-value 0.012; Table 2).
Table 1.
Comparative analysis of bone cement and bone graft in giant cell tumour.
| Study | Curettage with bone graft (n) | Curettage with cement (n) | Risk ratio (95% confidence interval) | P-value | ||
| Event | Total | Event | Total | |||
| Gao et al (2014)12 | 12 | 34 | 4 | 31 | 2.73 (0.79, 9.37) | 0.109 |
| Benevenia et al (2016)15 | 7 | 21 | 6 | 22 | 1.22 (0.35, 4.23) | 0.751 |
| Gaston et al (2011)19 | 73 | 246 | 12 | 84 | 2.07 (1.07, 4.01) | 0.029 |
| Total | 92 | 301 | 22 | 137 | 1.9 (1.14, 3.16) | 0.012 |
Table 2.
Overall recurrence rates in giant cell tumour.
| Study | Curettage with bone graft | Curettage with cement | Overall recurrence rate (%) | ||||
| Recurrence (n) | Total (n) | Recurrence rate (%) | Recurrence (n) | Total (n) | Recurrence rate (%) | ||
| Gao et al (2014)12 | 12 | 34 | 35.3 | 4 | 31 | 13 | 25 |
| Benevenia et al (2017)15 | 7 | 21 | 32.0 | 6 | 22 | 29 | 30 |
| Gaston et al (2011)19 | 73 | 246 | 29.7 | 12 | 84 | 14 | 26 |
| Caubere et al (2017)13 | 8 | 19 | 42.1 | – | – | – | 42 |
| Karmakar et al (2017)14 | 0 | 18 | 0.0 | – | – | – | 0 |
| Moon et al (2013)16 | – | – | – | 0 | 23 | 0 | 0 |
| Yu et al (2012)17 | – | – | – | 0 | 16 | 0 | 0 |
| Saikia et al (2011)18 | 11 | 34 | 32.4 | – | – | – | 32 |
| Fraquet et al (2009)20 | 9 | 30 | 30.0 | – | – | – | 30 |
| Kivioja et al (2009)21 | 56 | 294 | 19.0 | – | – | – | 19 |
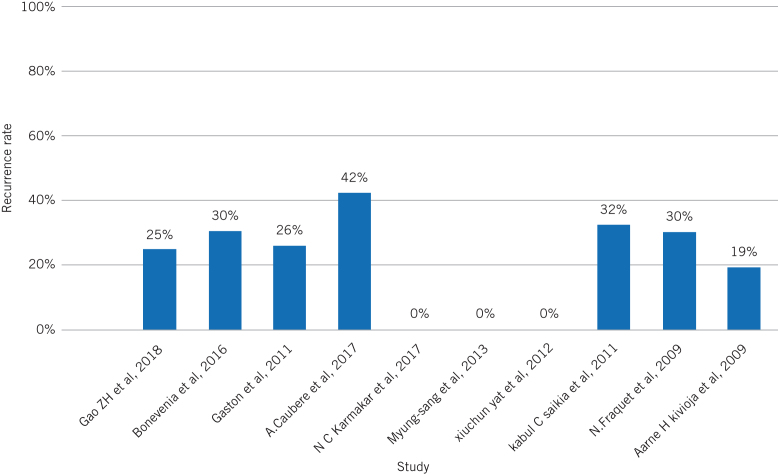
We applied the observational analysis to the remaining studies and the recurrence rate for each study was extracted. We noticed that Caubere et al had an overall recurrence rate of 42% in their 19 cases,13 whereas Karmakar et al,14 Moon et al16 and Yu et al17 enrolled 18, 23 and 16 cases, respectively, in their studies and reported zero recurrence rate. Saikia et al observed a 32% overall recurrence rate (32 cases),18 Fraquet et al reported a 30% overall recurrence rate (30 cases),20 and Kivioja et al only a 19% overall recurrence rate (294 cases).21 In all these studies, only bone cement was used (Fig 1).
Figure 1.
Forest plot showing a comparative analysis of bone cement and bone graft in giant cell tumours.
An observational analysis was done in seven studies; three studies showed no recurrence rate (Fig 2). One study13 showed the highest recurrence rate of 42% and the remaining studies reported an overall recurrence rate of 20.4%, from all 10 studies (Table 3). When all the cases of bone grafting alone and bone cement alone were pooled, we found that in 696 bone graft alone cases (from 8 studies) there was an average recurrence rate of 27.56%, whereas in 176 bone cement alone cases (from 5 studies) an average recurrence rate was significantly lower (11.20%) than the bone graft alone cases.
Figure 2.
Overall recurrence rates in various studies.
Table 3.
Demographics of the studies included in the present paper.
| Study | Type | Patients (n) | Surgical treatment | Score used/evaluated analysis | Follow-up | Recurrence rate (%) | Conclusion |
| Gao et al (2014)12 | Retrospective | 65 | 34 curettage and BG 31 curettage and BC |
x-ray, MRI, MSTS score Curettage and BG 91.1% Curettage and BC 94.7% |
37.7 months 46.5 months |
35.3 12.9 |
Curettage and BC have low recurrence rate than BG |
| A.Caubere et al (2017)13 | Retrospective | 19 | curettage and BC | Radiographical analysis 4 patients (21%) KL-3 1 patients (5%) KL-4 (to evaluate OA knee) |
120 months | 42 | Good functional outcome and no development of osteoarthritis |
| Karmakar et al (2017)14 | Prospective | 18 | curettage and BC | Schatzker and Lambert criteria: excellent 38.9%, good 44.4%, fair 11.1%, poor 5.6% | 18 months | 0 | Excellent relief of pain and good functional outcome |
| Benevenia et al (2017)15 | Retrospective | 43 | 21 BG and BC 22 BC only |
92% (no significant difference) MSTS score 93% |
59 months | 29 32 |
BG and BC reduces postoperative complications, decreases tumour recurrence and has good functional outcome than cement alone |
| Moon et al (2013)16 | Retrospective | 23 | curettage, electrocautery, burring, phenol irrigation and cement | Radiographical analysis, histology | 10 years | 0 | combined treatment with curettage, electrocautery, burring, phenol irrigation and cementation was more effective |
| Yu et al (2013)17 | Retrospective | 16 | curettage, cement, internal fixation and oral bisphosphonates | Enneking limb function score 24–29 | 25 months | 0 | curettage, cement, internal fixation and oral bisphosphonates exhibit solid fixation without fracture |
| Saikia et al (2011)18 | Retrospective | 32 | curettage and BC | x-ray, MRI, CT (Campanacci grade 2 and 3) | 2.5–12 years | 34.4 | high rate of local recurrence with Campanacci grade 3 |
| Gaston et al (2011)19 | Retrospective | 330 | curettage alone curettage with BC |
Kaplan–Meier survival curve x-ray, MRI | 76.5 months | 29.7 14.3 |
curettage with cement is associated with low risk of recurrence than curettage alone |
| Fraquet et al (2009)20 | Retrospective | 30 | curettage and BC | x-ray, CT, MRI, MSTS score 93.33% | 6 years 4 months | 30 | curettage and bone cement is a treatment of choice with low rate of recurrence |
| Kivioja et al (2009)21 | Prospective | 294 | Intralesional surgery filling with BC or BG | MRI, x-ray, Kaplan–Meier method | 5 years | 19 | cement is recommended in intralesional surgery of GCT, with low recurrence rate |
BC, bone cement; BG, bone graft; CT, computed tomography; KL, Kellgren and Lawrence system score; MRI, magnetic resonance; MSTS, musculoskeletal tumour staging; OA, osteoarthritis.
Discussion
Giant cell tumours of bone can be managed by multiple treatment modalities. There is a consensus that in a contained lesion with no cortical break and no articular involvement, extensive curettage is the treatment of choice.5,6 The management of the defect left in the bone after extended curettage has been a point of major discussion in the literature. An ideal filler for the defect should have the ability to fill the gap completely, minimum donor site morbidity, the ability to provide support to the bony architecture to allow early rehabilitation, ease of detection of recurrence and ease of removal in case of recurrence. Based on these criteria, various options have been used in the past. These include bone grafting alone, bone grafting mixed with cement and cement alone. The use of bone graft alone has the advantages of providing a biological background for bone healing. However, there are several disadvantages to using bone graft alone in the management of cavity after extended curettage. There is significant donor site morbidity, the graft may not be ideal to fill up extensive cavities and the strength of the bone is not immediately restored. The bone cement has claimed to have a tumouricidal effect by its exothermic reaction, which produces more than 60 degrees of heat.14 Moreover, bone cement can fill the large cavities and provides immediate stability, with no donor site morbidity (Table 4).22
Table 4.
Advantages and disadvantages of bone graft and bone cement in giant cell tumours.
| Method of treatment | Advantages | Disadvantages |
| Bone graft | Provides biological background for bone healing | Donor site morbidity |
| Provides structural support | May not be ideal to fill up large cavities | |
| Strength of the bone is not immediately restored | ||
| Bone cement | Provides structural support | May cause bone cement implantation syndrome |
| No donor site morbidity | Being nonbiological, there is no incorporation with the host bone | |
| Can fill up the large cavities | Being a foreign body, may lead to various complications such as infection | |
| May cause adjacent cartilage damage and osteoarthritis |
The current systemic analysis of 10 studies was carried out to evaluate recurrence rates after the use of bone cement and bone graft in giant cell tumour, and encompasses 870 cases. All these cases were treated with intralesional curettage followed by the use of bone cement or bone graft (in three studies) and cement only in the remaining seven studies. In three studies where both modalities were used, a comparative analysis using Forest plot revealed that local recurrence rates differed significantly between bone cement only cases and bone graft only cases, with patients having a bone graft only exhibiting statistically significantly higher recurrence rates than those who had bone cement only. An observational analysis was done in the remaining seven studies and, of these, three studies showed no recurrence rate. One study reported the highest recurrence rate of 42%, whereas the overall recurrence rate from all these studies pooled together in this study was 20.4%. The current study provides novel and compelling evidence in intralesional curettage for giant cell tumour of bone.
In the currently available literature, a consensus has not been reached for preferential use of bone cement in giant cell tumour. In a retrospective study of 65 patients, 34 underwent curettage and bone grafting and 31 underwent curettage and bone cement.12 X-ray, magnetic resonance imaging for recurrence and musculoskeletal tumour staging score was used for functional analysis. The recurrence rate for curettage and bone graft was 35.3% (at 37.7 months of follow-up) and curettage and bone cementing was 12.9% (at 46.5 months). The study demonstrated that curettage and bone cement has a lower recurrence rates than bone grafting, with good functional outcomes. Caubere et al studied 19 patients in a retrospective series, with an average follow up of 120 months.13 All their patients underwent curettage and were treated with bone cement. Radiological analysis, MSTS and Knee injury and Osteoarthritis Outcome score was used to evaluate osteoarthritis and functional outcome, respectively. The authors reported a recurrence rate was 42% but did not find any case of osteoarthritis.
Karmakar et al analysed 18 patients treated with curettage and bone cement in a prospective study.14 They used Schatzker and Lambert criteria and found that the majority of their patients had favourable outcomes, with excellent results in 38.9% and good results in 44.4%. Only 11.1% had fair and 5.6% poor results. At the end of 18 months of follow-up, they did not encounter any recurrence. They concluded that the majority of their patients had excellent pain relief and good functional outcome after curettage and bone grafting. However, Benevenia et al did not find any significant difference between bone cement and bone cement mixed with bone graft in their retrospective study of 43 patients, at an average follow-up of 59 months.15 The authors concluded that curettage with bone graft and cement reduces postoperative complication, decreases tumour recurrence and provide excellent functional outcomes than if bone cement is used alone.
Moon et al performed a retrospective study that included 23 patients who underwent curettage, electrocautery, burring, phenol irrigation and cement.16 Radiographical analysis and histology were done. The patients were followed up for 10 years and there were no recurrences. The authors concluded that combined treatment with curettage, electrocautery, burring, phenol irrigation and cementation was a highly effective treatment for giant cell tumour of bone.
Yu et al analysed 16 patients who underwent curettage, cement, internal fixation and oral bisphosphonates in a retrospective study.17 Enneking limb function score was used. The patients were followed-up for 25 months and no recurrences were found. The authors concluded that curettage, cement, internal fixation and oral bisphosphonates exhibit stable fixation without fracture and recurrence.
In a retrospective study,18 32 patients were treated with curettage and bone cement. X-ray, magnetic resonance imaging and computed tomography were used to analyse the rate of recurrence. At follow-up of 2.5–12 years, the overall recurrence rate was found to be 34.4% for patients with Campanacci grade II and III giant cell tumour. Gaston et al performed a retrospective study in 330 patients.19 These patients were divided into two groups: curettage only and curettage with cement. Kaplan–Meier survival curve, x-ray and magnetic resonance imaging were used to check for recurrence rate. At follow-up to 76.5 months, the recurrence rate was 29.7% in only curettage group and 14.3% in curettage with cement group. The authors concluded that the curettage with cement was associated with lower risk of recurrence than curettage alone.
Fraquet et al conducted a retrospective study in 2009, which comprised 30 patients with giant cell tumour of bones.20 All patients underwent curettage and bone cement, musculoskeletal tumour staging score was 93.33%, defining a good functional outcome. The authors found a 30% recurrence rate at six years and four months of follow-up and concluded that curettage and bone cement is the treatment of choice with a low rate of recurrence.
Kivioja et al conducted a prospective study in 294 patients in whom intralesional surgery was performed, and the cavity was filled with cement or bone graft. Magnetic resonance imaging, x-ray and the Kaplan–Meier method were used, with a follow-up of five years. The overall recurrence rate was 19%, and the authors recommended the use of bone cement in intralesional surgery of giant cell tumour, with a low recurrence rate.
In the present survey of 10 studies, we noticed that, in two studies,16,17 extensive intralesional curettage was followed by bone cementation. Moon et al used electrocautery, burring and phenol irrigation16 and Yu et al 17 used internal fixation and bisphosphonates. These additional adjuvant therapies might have been responsible for their excellent results and are worth exploring in future studies. Karmakar et al also reported zero recurrence after the use of bone graft alone, but did not mention or discuss the reasons for their outstanding success.14 This paper was published in a local medical college journal rather than an indexed journal. In contrast to these studies with a zero recurrence rate, Caubere et al reported the maximum recurrence rate of 42% in their study of 19 cases, where bone cement was used.13 The reasons for this high incidence could be related to higher number of cases (25%) lost to follow-up and a smaller number of patients in this retrospective study.
We found that local recurrence rates differed significantly between treatment with polymethyl methacrylate or bone cement only and bone graft only, with the last exhibiting significantly higher recurrence rates (Table 2), with a statistically significant difference (RR 1.90, 95% CI 1.14, 3.16; overall effect Z = 2.488; P-value 0.012) in favour of bone cement only. From our analysis of the pooled data, it was evident that 176 bone cement cases (in five studies) had a much lower recurrence rates of 11.2%, compared with 696 bone graft cases (in eight studies) where there was an average recurrence rate of 27.56%. Hence, it became evident by analysing the current literature of 10 selected studies that the bone cementation alone with extensive intralesional curettage and preferably some adjuvant therapy such as electrocautery, phenol irrigation and the use of denosumab23 or bisphosphonates may help in decreasing the incidence of recurrence in giant cell tumour of bone.
Limitations of study
Because of the paucity of excellent and comparative studies on the management of giant cell tumour of bone, we could not find enough comparative studies of different modalities of treatment. From a critical survey of the recently published studies (in the past 10 years) for the management of giant cell tumour of bone, we found only three studies where comparative analysis could be done, and the remaining seven were observational analysis.
Conclusions
Although giant cell tumour is a commonly occurring bone tumour, there is a paucity of good studies in the literature on the management of this tumour. We found that the use of bone cement was associated with a statistically significantly lower recurrence rate than bone grafting in giant cell tumour of bones. We therefore recommend that bone cementation alone with extensive intralesional curettage and preferably some adjuvant therapy such as electrocautery, phenol irrigation and the use of denosumab or bisphosphonates, may help in decreasing the incidence of recurrence in giant cell tumour of bone. We suggest that more comparative, prospective and multicentre studies are required for better results, which could guide us convincingly about the management of giant cell tumour of bone.
References
- 1.Egbert RC, Folsom R, Bell J, Rajani R. Denosumab therapy for giant cell tumor of bone pulmonary metastasis. Case Rep Orthop 2017; : 230–259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McDonald DJ, Sim FH, McLeod RA, Dahlin DC. Giant-cell tumor of bone. J Bone Joint Surg (Am) 1986; : 235–242. [PubMed] [Google Scholar]
- 3.Sung HW, Kuo DP, Shu WP et al. Giant cell tumor of bone: analysis of two hundred and eight cases in Chinese patients. J Bone Joint Surg (Am) 1982; : 755–761. [PubMed] [Google Scholar]
- 4.Campanacci M, Baldini N, Boriani S, Sudanese A. Giant-cell tumor of bone. J Bone Joint Surg (Am) 1987; : 106–114. [PubMed] [Google Scholar]
- 5.Eckardt JJ, Grogan TJ. Giant cell tumor of bone. Clin Orthop 1986; : 45–58. [PubMed] [Google Scholar]
- 6.Mendenhall WM, Zlotecki RA, Scarborough MT et al. Giant cell tumor. Am J Clin Oncol 2006; : 96–99. [DOI] [PubMed] [Google Scholar]
- 7.Raskin KA, Schwal JH, Mankin HJ et al. Giant cell tumor of bone. J Am Acad Orthop Surg 2013; : 118–126. [DOI] [PubMed] [Google Scholar]
- 8.Campanacci M, Capanna R, Fabbri N, Bettelli G. Curettage of giant cell tumor of bone and reconstruction with subchondral grafts and cement. Chir Organi Mov 1990; : 212–213. [PubMed] [Google Scholar]
- 9.Klenke FM, Wenger DE, Inwards CY et al. Giant cell tumor of bone: risk factor for recurrence. Clin Orthop Relat Res 2011; : 591–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frassica FJ, Gorski JP, Pritchard DJ et al. A comparative analysis of subchondral replacement with polymethylmethacrylate or autogenous bone graft in dogs. Clin Orthop Relat Res 1993; : 378–390. [PubMed] [Google Scholar]
- 11.Nelson D, Barker M, Hamlin B. Thermal effect of acrylic cementation of bone tumor sites. Int J Hyperthermia 1997; : 287–306. [DOI] [PubMed] [Google Scholar]
- 12.Gao ZH, Yin JQ, Xie XB et al. Local control of giant cell tumors of the long bone after aggressive curettage with and without bone cement. BMC Musculoskelet Disord 2014; : 330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Caubere A, Harrosch S, Fioravanti M et al. Does curettage-cement packing for treating giant cell tumour at the knee lead to osteoarthritis? Orthop Traumatol Surg Res 2017; : 1,075–1,079. [DOI] [PubMed] [Google Scholar]
- 14.Karmakar NC, Uddin MM, Rahman MM et al. Management of giant cell tumour by curettage and bone cement in weight bearing bone: a study done in DMCH & NITOR. Faridpur Med Coll J 2017; (1): 9–13. [Google Scholar]
- 15.Benevenia J, Rivero SM, Moore J et al. Supplemental bone grafting in giant cell tumor of the extremity reduces nononcologic complications. Clin Orthop Relat Res 2017; (3): 776–783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moon MS, Kim SS, Moon JL et al. Treating giant cell tumours with curettage, electrocautery, burring, phenol irrigation, and cementation. J Orthop Surg (Hong Kong) 2013; : 209–212. [DOI] [PubMed] [Google Scholar]
- 17.Yu X, Xu M, Xu S, Su Q. Clinical outcome of gaint cell tumour of bone treated with bone cement filling and internal fixation, and oral bisphosphonates. Oncol Lett 2013; : 447–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Saikia KC, Bhattacharyya TD, Bhuyan SK et al. Local recurrences after curettage and cementing in long bone giant cell tumor. Indian J Orthop 2011; (2): 168–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gaston CL, Bhumbra R, Watanuki M et al. Does the addition of cement improve the rate of local recurrence after curettage of giant cell tumours in bone? J Bone Joint Surg Br 2011; (12): 1,665–1,669. [DOI] [PubMed] [Google Scholar]
- 20.Fraquet N, Faizon G, Rosset P et al. Long bones giant cells tumors: treatment by curettage and cavity filling cementation. Orthop Traum Surg Res 2009; : 402–406. [DOI] [PubMed] [Google Scholar]
- 21.Kivioja AH, Blomqvist C, Hietaniemi K et al. Cement is recommended in intralesional surgery of giant cell tumors: a Scandinavian Sarcoma Group study of 294 patients followed for a median time of 5 years. Acta Orthop 2009; : 86–93. [DOI] [PubMed] [Google Scholar]
- 22.Vaishya R, Chauhan M, Vaish A. Bone cement. J Clin Orthop Trauma 2013; : 157–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vaishya R, Agarwal A, Vijay V. Salvage treatment' of aggressive giant cell tumor of bones with denosumab. Cureus July; (7): e291. [DOI] [PMC free article] [PubMed] [Google Scholar]