Abstract
Introduction
Primary care patients with a suspected head and neck cancer are referred through the urgent suspicion of cancer referral pathway. Rates of cancer detection through this pathway are low. Evidence surrounding the pathway of these patients is lacking. This study aimed to determine the outcome of urgent suspicion of cancer referrals for head and neck cancer.
Methods and methods
All head and neck cancer urgent suspicion of cancer referrals in NHS Greater Glasgow and Clyde between June 2015 and May 2016 were analysed in regard to their clinical pathway.
Results
There were 2116 urgent suspicion of cancer referrals in the one-year period. The overall cancer rate was 235 (11.8%), compared with 152 (7.6%) that resulted in a primary head and neck cancer diagnosis. Of the total, 851 (42.6%) were reassured and discharged after one clinic appointment; 536 (26.8%) were followed up for suspected benign pathology and 436 (21.8%) were actively investigated for cancer.
Conclusion
A significant proportion of patients attending urgent suspicion of cancer clinic appointments can be seen and discharged in one clinic appointment, provided there is same day imaging available. Cancer identification rates through urgent suspicion of cancer pathways remain low.
Keywords: Outpatients, Referral and consultation, Secondary care, Head and neck neoplasms, Radiology
Introduction
The NHS cancer plan was introduced by the UK Department of Health after comparatively inferior cancer treatment and survival rates compared with those of Europe and North America were recorded. A range of targets were introduced which included a ‘two-week wait’ from general practitioner referral to specialist review in patients with suspected cancer.1 The Scottish Referral Guidelines for Suspected Cancer were introduced to assist general practitioners in their decision to refer as an urgent suspicion of cancer (USOC), by defining red flag symptoms that require urgent specialist assessment.2 Despite the introduction of these guidelines, cancer detection rates remain at 11%, with the majority of the 8000 new cases of head and neck cancer diagnosed in the UK each year being identified through more routine methods.3,4
There have been many studies focusing on USOC referrals, the detection rate, the specificity of the guidelines, compliance and patient demographics. However there is a lack of data regarding the patient pathway after referral. This audit reviews the outcomes of USOC head and neck cancer referrals at the initial outpatient appointment and their subsequent pathway.
Materials and methods
A total of 2116 consecutive USOC referrals to the ear, nose and throat (ENT) department of NHS Greater Glasgow and Clyde between June 2015 and May 2016 were assessed. Of these, 118 (6%) patients were excluded due to non-attendance, leaving 1998 patient referrals for analysis. A retrospective case record review was conducted. Demographics, clinic findings and outcomes were recorded anonymously. Each patient pathway was reviewed regarding investigations required to reach a diagnosis and definitive treatment. Data were collected and analysed using Microsoft Excel. This is an audit of clinical practice and formal ethical approval was not required.
Results
Demographics
Of the total referrals, 1195 (56.6%) were female. The mean age was 59.5 years (range 12–99 years); 58 (2.9%) had a previously known head and neck cancer. Of all referrals, 721 (34.3%) were non-compliant with the National Institute for Health and Care Excellence guidance, 366 (17.4%) were non-compliant with Scottish Referral Guidelines. Presenting complaints are summarised in Table 1. Twenty patients (1%) were seen as an emergency prior to their scheduled USOC appointment, of which 11 (0.55%) resulted in a cancer diagnosis. 152 (7.6%) had a diagnosis of head and neck cancer and an additional 83 patients (4.2%) had other types of cancer.
Table 1.
Summary of presenting complaints.
| Presenting complaint | Symptoms | |
| Intermittent (%) | Persistent (%) | |
| Hoarseness > 3 weeks | 183(9.2) | 558(27.9) |
| Cough > 3 weeks | 0 | 132(6.6) |
| Neck lump | 0 | 649(32.5) |
| Odynophagia > 3 weeks | 0 | 72(3.6) |
| Dysphagia > 3 weeks | 99(5.0) | 217(10.8) |
| Sore throat > 3 weeks | 56(2.8) | 197(9.9) |
| Unilateral sore throat | 0 | 56(2.8) |
| Haemoptysis | 0 | 16(0.8) |
| Globus pharyngeus | 0 | 198(9.9) |
| Oral mucosa or tongue swelling or ulceration | 0 | 83(4.2) |
| Oral mucosa or tongue white/red plaques | 0 | 20(1.0) |
USOC referral outcome
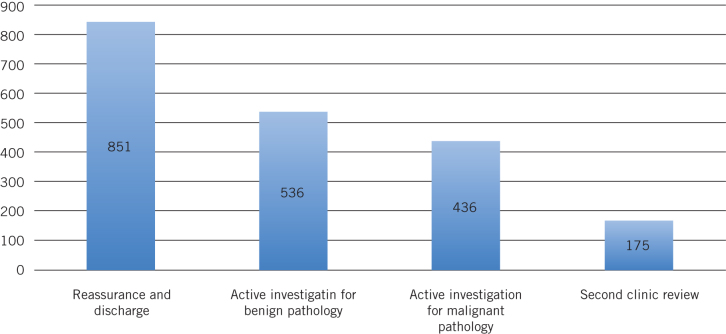
851 (42.6%) were reassured and discharged after one clinic appointment and 68 (8%) were discharged with speech and language input. A total of 171 patients (20.1%) were discharged with medication, the most common of which were proton pump inhibiters (n = 27; 3.2%) and nasal steroids (n = 25; 2.9%). An overview of outcomes after one clinic appointment are shown in Figure 1.
Figure 1.
Clinic outcomes after one urgent suspicion of cancer clinic appointment.
The top diagnoses of these patients were gastro-oesophageal reflux disease (n = 60; 7.1%), globus pharyngeus (n = 47; 5.5%), laryngitis (n = 28; 3.3%), rhinosinusitis (n = 28; 3.3%), presbyphonia (n = 24; 2.8%), reactive lymph nodes (n = 22; 2.6%), functional dysphonia (n = 20; 2.6%) and nasal symptoms (n = 33; 3.9%). 47 patients (5.5%) were asymptomatic with resolved symptoms at the time of review.
Same dame ultrasound was performed in 84 patients (4.2%) and an additional 473 (23.7%) required a separate appointment for ultrasound. Some 536 patients (26.8%) were investigated for suspected benign pathology: 374 (18.7%) required imaging, 62 (3.1%) required surgery and 78 (3.9%) had surgery and scanning to reach a definitive diagnosis. Of these, 25 (1.3%) resulted in a malignant pathology, most commonly a haematological malignancy (n = 10; 0.5%).
Of the total, 436 patients (21.8%) were actively investigated for suspected cancer. Of these patients, 208 (10.4%) were diagnosed with cancer. All required imaging and surgery to establish diagnosis.
One hundred and seventy-five patients (8.8%) were observed at variable intervals with trials of conservative management. Two of these patients were later found to have cancer: one pulmonary and one supraglottic. The pulmonary malignancy, alongside superior vena cava obstruction, was diagnosed on computed tomography (CT) previously arranged by the general practitioner but scheduled for after the initial USOC appointment. They had presented with facial swelling, neck and chest vein engorgement with a normal ENT examination. The supraglottic cancer initially appeared as a benign mucus retention cyst, but it became more painful and erythematous during follow-up and was found to be an atypical carcinoid (neuroendocrine carcinoma).
Diagnostic investigations
Ultrasound scan and ultrasound with fine-needle aspiration (FNA) with cytology was performed in 44 (2.2%) and 30 (1.5%) patients, respectively, prior to USOC appointment. Of the patients who had ultrasound, 28 (1.4%) required repeat investigation; 20 (1.0%) required ultrasound with FNA for cytological diagnosis to confirm findings. Eight patients required repeat ultrasound, which either confirmed or disputed the diagnosis. Similarly 13 patients (0.7%) who underwent ultrasound FNA required a repeat procedure (n = 7; 0.4%) or a further ultrasound scan alone (n = 6; 0.3%). The most prevalent reason for this was to confirm suspicions in non-diagnostic investigations.
Prior to their appointment, 461 patients (23.1%) received a chest x-ray. Of these, 238 (11.9%) were related to a presenting complaint of hoarseness, 70 (3.5%) related to a neck mass, 62 (3.1%) related to dysphagia and 64 (3.2%) related to persistent cough. CT was performed in 39 patients (1.95%) prior to referral.
Flexible nasendoscopy was performed in 1690 (84.6%) of the patients. Ultrasound was performed in 44 (2.25%) and ultrasound with FNA in 40 patients (2.0%) during the clinic; 45 (2.3%) of these resulted in a cancer diagnosis (Table 2).
Table 2.
Summary of procedures performed during clinic.
| Procedure | n (%) |
| Flexible nasendoscopy | 1690 (84.6) |
| Ultrasound | 44 (2.2) |
| Ultrasound with sampling (fine-needle aspiration/core) | 40 (2.0) |
| Incision and drainage | 11(0.5) |
| Audiometry | 15(0.7) |
| Excision and biopsy of lesion | 7(0.4) |
| Allergy testing | 4(0.2) |
| Microsuction | 5(0.3) |
| Nasal cautery | 5(0.3) |
| Tonsillolith removal | 1(0.05) |
| Salivary stone removal | 2(0.1) |
| Bloods | 53(2.7) |
| Other | 14(0.7) |
For those patients who did not receive ultrasound with or without FNA with cytology during clinic (n = 473; 23.7%), ultrasound was arranged as an outpatient. Of these scans, 40 (0.2%) resulted in a cancer diagnosis.
Investigations required to make a definitive diagnosis are summarised in Table 3. Barium swallow was performed in 153 (7.7%) patients. Only 16 patients were investigated for suspected cancer with barium swallow, with the most common presenting complaint as dysphagia (n = 127; 6.4%), hoarseness (n = 42; 2.1%) and globus (n = 23; 1.2%). No barium swallows performed resulted in diagnoses of cancer; 66 (3.3%) resulted in an entirely normal examination. The remaining examinations demonstrated benign pathology such as aspiration, reflux and hiatus hernia.
Table 3.
Investigations required for diagnosis.
| Investigation | Patients (%) |
| Radiological | |
| Ultrasound total | 557 (27.9) |
| Performed after USOC clinic appointment. | 473 (23.7) |
| Performed same-day as USOC appointment | 84 (4.2) |
| Barium swallow | 153(7.7) |
| Computed tomography | 368(18.4) |
| Magnetic resonance imaging | 60(3.1) |
| Surgical | |
| Panendoscopy | 262(13.1) |
| Malignant | 96(4.8) |
| oesophagogastroduodenoscopy | 37(1.9) |
The mean number of clinics attended was 1.88 (± 2.09). Most commonly, only one clinic appointment is required (n = 1204; 60.3%); 851 (42.6%) were reassured and discharged from initial clinic, a further 268 (13.4%) were investigated and discharged and 74 (3.7%) were actively investigated and referred to a different specialty.
Discussion
Referral outcomes
The USOC and the two-week wait pathway do not identify significant rates of cancer in an ENT clinic.3–4 In NHS Greater Glasgow and Clyde, 364 patients are diagnosed with head and neck cancer per year.5 In the year analysed, 152 patients (42%) came through the USOC pathway, which means that the majority present through less emergent pathways. Twenty patients (1%) presented as emergencies before their USOC clinic appointment and eleven (0.55%) of these patients were found to have head and neck cancer.
The USOC clinic setting does enable rapid clinical decision making. A significant proportion of these (n = 851; 42.6%) were assessed and discharged after the initial appointment. Globus pharyngeus is a common USOC referral reason despite not being a red flag symptom. Globus pharyngeus in this group is frequently referred as dysphagia (which is a red flag symptoms in the Scottish Referral Guidelines). Another local issue is that USOC referrals cannot be downgraded by ENT surgeons and require rejection of the referral. In this large group of patients, globus is not associated with any serious pathology and should not be a reason for referral for a two-week urgent appointment unless it is associated with other more significant symptoms.
Diagnostic investigations
Given that the most common presenting symptom in the above cohort was a lump in the neck (n = 649; 32.5%), ultrasound with or without FNA is the primary investigation required. Investigation with ultrasound prior to clinic, which may help the general practitioner in deciding upon a referral, is of limited use in the USOC setting, as these procedures were often repeated or the patient required further ultrasound and FNA. This represents wasted resources and a potential delay in waiting time for patients attending clinic. Since the observation period began, NHS Greater Glasgow and Clyde has now stopped neck ultrasound requests originating in primary care. Ultrasound and ultrasound FNA during the clinic have shown benefit for immediate reassurance and discharge from clinic, which benefits both clinician and patient. Additionally, these procedures can lead to immediate initiation of active treatment.
Clinical implications
It is possible to determine that the majority of these patients can be managed in one outpatient clinic. In NHS Greater Glasgow and Clyde, there is now increased availability of same-day ultrasound. In this group of patients, investigation in primary care leads to repetition of scan requests and is not recommended.
Strengths and limitations
This is a large audit looking at over 2000 patient records in a 12-month period. It assesses a patient pathway that has been only infrequently analysed.
As this is a retrospective study of the patient journey, there are issues surrounding missing data from the clinical letters, such as clinical impression and findings.
Conclusion
This audit has demonstrated that the majority of USOC referrals for head and neck cancer can be managed in one clinic appointment and has advocated the need for increased same-day scanning. Pre-clinic imaging (chest x-ray and ultrasound) is of limited use in the context of USOC referrals.
References
- 1.Department of Health The NHS Cancer Plan: A Plan for Investment, a Plan for Reform. London: DoH; 2000. [Google Scholar]
- 2.Health Improvement Scotland Scottish Referral Guidelines for Suspected Cancer. Edinburgh: Health Improvement Scotland; 2014. [Google Scholar]
- 3.McKie C, Ahmad UA, Fellows S et al. . The 2-week rule for suspected head and neck cancer in the United Kingdom: referral patterns, diagnostic efficacy of the guidelines and compliance. Oral Oncol 2008; (9): 851–856. [DOI] [PubMed] [Google Scholar]
- 4.Lyons M, Philpott J, Hore I, Watters G. Audit of referrals for head and neck cancer: the effect of the 2-week, fast track referral system. Clin Otolaryngol Allied Sci 2004; (2): 143–145. [DOI] [PubMed] [Google Scholar]
- 5.ISD Scotland Cancer Statistics. Head and Neck Cancer. www.isdscotland.org/Health-topics/Cancer/Cancer-statistics/Head-and-neck (cited August 2018).